Abstract
Background
To investigate the hemodynamic response of the cerebral bridging veins to increased intracranial pressure (ICP) during normo- and hyperventilation.
Methods
Flow velocity (FVm), diameter (D), and pulsatility index (PI) were measured and calculated in the cerebral bridging veins using Color Doppler Ultrasound in seven pigs, and cerebral blood flow (CBF) was measured using 133Xe clearance in nine pigs, both during normo- and hyperventilation. ICP was increased stepwise from baseline (about 10 mmHg) to 20 and 30 mmHg by infusion of mock CSF into the cisterna magna.
Results
Moderate elevations of ICP caused venous relative stasis as evidenced by a decrease in FVm and increase in diameter and PI, but no change of volume flow in the veins. CBF was stable indicating autoregulation at ICP of 20 and 30 mmHg. Parallel observations were made during normo- and hyperventilation, but at two different levels of CBF.
Conclusions
The cerebral bridging veins dilation and blood flow velocity decrease indicate the venous relative stasis in response to the elevated ICP. This response is proposed to be caused by an ICP-dependent increase in resistance to the outflow from the cerebral bridging veins.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pressure–volume relationship between intracranial pressure (ICP), cerebrospinal fluid (CSF), blood, and brain tissue is known as the Monro-Kellie doctrine which states that the cranial compartment is incompressible, and the volume inside the cranium is a fixed volume [1]. The cranium and its constituents create a state of volume equilibrium, such that any increase in volume of one of the cranial constituents must be compensated by a decrease in volume of another. For example, an increase in lesion volume (e.g., epidural hematoma or tumor) will be compensated by the downward displacement. This study focuses on the hemodynamic response of the cerebral venous system especially the bridging veins to increased ICP. Plausibly, an elastic tube (e.g., brain veins) will be collapsed if the surrounding pressure increases. It may not be true. Some previous reports have indicated that the venous outflow from a compartment of higher pressure to a compartment of lower pressure can be described as a “waterfall” outflow [2]. In the brain as in other encapsulated organs, this “waterfall” phenomenon actually implies that the resistance to venous outflow increases by increasing organ pressure preventing the veins from collapsing. This concept has been evidenced from studies of mechanical models [3, 4] and some vascular systems [5–7]. Furthermore, a few in vivo studies of the cerebral veins have indicated dilatation of the cerebral bridging veins in response to increased ICP [8]. The mechanism behind these interesting issues remains unexplained completely. In this study, we investigated the hemodynamics response of the cerebral venous system and the bridging veins to increased ICP both during normo- and hyperventilation.
Materials and Methods
Yorkshire landrace pigs of both sexes with a mean weight of 53.9 ± 0.6 kg (mean ± SE) were deprived of food for 12 h before the experiment but had free access to water. Pigs were studied in two different groups: “Doppler” group has seven pigs subjected to both normo- and hyperventilation; “133Xe-CBF” group has nine pigs subjected to both normo- and hyperventilation. All the protocols in this study have been approved by the Institutional Review Board of Shandong University (Jinan, China).
Anesthetic and Surgical Methods
Premedication using Sedaperone (2 mg/kg i.m.) and Dormicum® (Midazolam, 0.1 mg/kg i.m.) was administered before transportation to the laboratory. Upon arrival to the laboratory 13–15-ml Hypnomidate® (Etomidate) was given intravenously in an ear vein for induction of anesthesia. After endotracheal intubation, the pigs were continuous anaesthetized with halothane (1–2%), pancuronium (0.05 mg/kg/h. iv.), and fentanyl (0.10 mg/kg/h reduced to 0.04 mg/kg/h. iv. after completion of surgery).
Respiratory rate was set around 12 breaths/min with 4.5-l O2 and 4-l air (Servo Ventilator 900, Siemens-Elema, Sweden). Normo- and hyperventilation were ensured by blood gas analysis after adjustment of the respiratory minute volume. Surgery was performed under clean conditions with the animal in the supine position. A burr hole simulating an artificial anterior fontanel with the diameter of 10 mm was made in the midline over the superior sagittal sinus (SSS) for placement of the ultrasound transducer. Another burr hole was placed on the right side for positioning of a subarachnoid screw for monitoring of ICP. Furthermore, an indwelling catheter was placed in the cisterna magna for infusion of mock CSF (lactated Ringer solution: 1.4-mM Ca, 4.0-mM K, 130-mM Na, 109-mM Cl, 28-mM lactate). Indwelling catheters were also placed into the femoral arteries for arterial blood sampling (intermittent blood gas analysis, Radiometer ABL 510, Denmark) and monitoring of mean arterial blood pressure (MABP), and into the inferior vena cava via the femoral vein for monitoring of CVP in the “Doppler” experiment. ICP, cisterna magna pressure, arterial blood pressure, and central venous pressure were continuously monitored. Catheters were placed in the vena cava superior via the jugular vein for intravenous injection of 133Xe in “133Xe-CBF” experiment. The animals were placed on a thermostatically controlled heating blanket to maintain the rectal temperature at normothermia (38°–39°). Continuous intravenous infusion of 0.9% saline-balanced intraoperative blood loss and substituted fluid consumed during the experiment. Flushing of the arterial catheter with Heparin SAD® 5000I.E./l was applied. Elevations of ICP from baseline (about 10 mmHg) up to 20 and 30 mmHg were obtained and maintained by stepwise elevation of a reservoir (bottle) of mock CSF connected to the needle placed in the cisterna magna.
The same experimental time schedule (Fig. 1) was used for both the groups. ICP was elevated at 30-min intervals to allow for steady-state and specific measurements. Blood flow velocity and diameter of the cerebral bridging vein were measured in the same cerebral bridging vein both during normo- and hyperventilation.
133Xe-CBF Measurement
Cerebral blood flow (CBF) was measured in nine pigs during normo- and hyperventilation using the i.v. 133Xe injection method. For injection of 133Xe a catheter was placed through the right jugular vein into the vena cava superior. The tip of the catheter was to be located proximal to the right auricle during image control.
Brain clearance of 133Xe was monitored using an extracranial lead-shielded NaI scintillation detector placed over one hemisphere. For each measurement of CBF, 110–150 kBq (3–4 mCi) of 133Xe was injected through the catheter followed by a rapid injection of l0-ml saline. CBF was computed using a Novo Cerebrograph l0a CBF system (B Simonsen Medical AS, Randers, Denmark). CBF was calculated as the initial slope index (ISI) using 11-min clearance curve. The ISI value represents primarily estimates of gray matter flow of the region below the detector. Due to the effect of the white matter, the ISI tends to underestimate the true gray matter flow as pointed out by Lassen and Ingvar [9]. This study was primarily concerned with relative changes of CBF during ICP and PaCO2 changes. Correction for residual activity was performed between the CBF measurements. In order to minimize counting of extracranial 133Xe, the scintillation detector of 17 mm in diameter was shielded using 5-mm lead and retraction of the detector by 22 mm to provide a 42° angled window.
Ultrasound Doppler Measurement
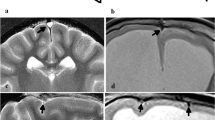
The experiments were carried out using a Color Doppler ultrasound system (Diagnostic Ultrasound System Type 3535, B&K Medical, Denmark) with a 7.5-MHz transducer. Flow velocity and diameter of the cerebral bridging veins were examined through the artificial anterior fontanel by a combination of sagittal and parasagittal scan planes. Using a mechanical holder the transducer was fixed into position a few millimeters above the dural surface to avoid compression of dura and the SSS. The bridging veins were identified according to their anatomical location and the direction of flow as structures with flow draining into the SSS in the midline (Fig. 2a). The image was then optimized for a bridging vein to measure its flow and diameter in relation to changes in ICP (Fig. 2b). To minimize the effect of the insonation angle on the flow velocity as given by cosinus of the angle, the insonation angle was kept below 30°. Possible changes of the ICP in the SSS could not be observed in this study. Doppler measurements were obtained within 3 min to minimize time-related changes in flow velocity. These measurements were performed within 30 min after the stepwise elevation of the mock CSF reservoir and when the new ICP level was obtained in a steady state. A velocity spectrum containing at least eight cardiac cycles was fixed on the display screen for measurements of mean velocities over this time interval. This procedure was repeated at least five times in each experimental interval.
a Midline sagittal Color Doppler sonography scan showing identification of a bridging vein (red) draining into the superior sagittal sinus (SSS, blue). The image was then optimized for measurements of the bridging vein, b the flow velocity in a bridging vein at ICP equals to 10, 20, and 30 mmHg (normoventilation). Flow velocity decreases markedly with increasing ICP. The calipers for measurements of venous diameter are indicated. The SSS is only incompletely or not imaged but its position is marked by “SSS” on the image for anatomical clarification. Distance of few millimeters is present between the transducer surface and the SSS to avoid compression. (Color figure online)
The diameter of the cerebral bridging veins was averaged from five measurements of the width of the colour band. Electronic calipers were placed over the closest pixel and the distance between two opposite calipers was used to estimate the diameter of the cerebral bridging veins as shown in Fig. 2.
The mean volume of cerebral bridging venous blood flow (VBF) per minute was calculated as:
where diameter (D) represents the bridging venous diameter and FVm represents the mean cerebral bridging venous blood flow velocity. The pulsatility index (PI) was calculated at each interval by means of the Pourcelot formula modified by Bada et al. [10]:
Statistics
Mean ± standard error (SE) was calculated. Paired t test (two-tailed) was used to analyze changes in FVm, D, PI, CBF, MABP, CPP, PaCO2, CVP, and VBF. Linear regression was used to analyze the ICP–FVm, ICP–D, and ICP–PI relations. Statistical significance was considered to be P < 0.05.
Results
Physiological variables and results during normo- and hyperventilation in the 133Xe-CBF and the Doppler groups are shown in Tables 1 and 2, respectively.
The 133Xe-CBF Experiment
As shown in Table 1 MABP and PaCO2 was rather unaffected by the applied increments in ICP. Correspondingly the cerebral perfusion pressure (CPP), which is calculated by MABP − ICP, fell from 82.1 ± 4.4 to 65.7 ± 4.1 mmHg (normoventilation) and from 71.4 ± 7.0 to 50.6 ± 5.8 mmHg (hyperventilation) with increased ICP. The CBF remained unaffected by increased ICP during normoventilation. During hyperventilation at ICP = 30 mmHg, however, CBF decreased significantly from 50.4 ± 2.6 to 38.8 ± 2.5 ml/100 g/min indicating a fall in CPP somewhere below the capacity of autoregulation as shown in Fig. 3. The applied variation in ICP during the Doppler measurements was within the capacity of autoregulation to maintain CBF stable.
The Doppler Experiment
These experiments were designed to measure corresponding values of FVm and D of a bridging vein during increments in ICP from baseline to 20 and 30 mmHg. The results are shown in Table 2 and in Figs. 4, 5. When ICP was increased, the FVm became slower (Fig. 4) and the venous diameter increased (Fig. 5) indicating venous system distension. These changes occurred in a balanced way so that the venous blood flow (VBF) calculated from FVm and D in terms of ml/min remained stable during both normo- and hyperventilation, as indicated in Fig. 6. Similar changes were observed during normo- and hyperventilation, but at a lower level of flow in the hyperventilated animals. No changes in CVP were observed.
Discussion
“Vascular Waterfall” and “Outflow Cuff Segment”
In a mechanical model of flow through collapsible tubes, Holt [3] observed that flow was maintained by the development of a partial local collapse of the site of the outlet segment when surrounding pressure was increased. This was supposed to provide a stenosis and resistance to outflow at the point of the outlet from the higher-pressure compartment. This phenomenon was termed the “vascular waterfall” by Permutt et al. [11] using a pulmonary venous model in dogs. Since its introduction, the concept has been applied to various vascular beds such as the hepatic circulation [12], the coronary circulation [13, 14], and human skeletal muscle [15]. Studies by Asgeirsson and Grände [16] using a model of perfused cat gastrocnemius muscle contained in a pressure chamber have indicated a similar response. They observed that an increase in the chamber pressure was associated with an increase in venous outflow resistance and this resistance was confined to the point of venous outlet. In addition, sagittal sinus pressure has been found to decrease or remain unchanged during rapid elevation of ICP in several reports. Nakagawa et al. concluded from their measurements of pressure in the bridging veins and SSS that pressure in the cerebral bridging veins varied in parallel with ICP, while pressure in the SSS remained lower. This observation was explained by assuming a pressure induced narrowing of the cerebral bridging vein at the site of junction with the SSS. Asgeirsson and Grände termed the narrowing point of venous outflow resistance the “outlet orifice”. By measurements of pressure, Nakagawa et al. [17] observed in a dog model that a gradual stenosis of the cerebral venous outflow pathway occurred 1–2-mm proximal to the junction between the vein and the sinus. All these studies including this study imply that there is a site of anatomical narrowing which vary according to ICP in such a way that a balanced resistance to venous outflow is provided. As described in a parallel study of morphology and biomechanics of the cerebral bridging veins in pigs, we have identified an “outflow cuff segment” located in the sinus-near end of the veins [18].
Blood Flow in the Bridging Veins Independent of ICP and Role of “Outflow Cuff Segment”
The corresponding values of FVm and D in a single bridging vein during increments of ICP to 20 and 30 mmHg show that flow in the vein remained constant and independent of ICP as did CBF measured by the 133Xe method and hence total venous outflow from the brain. It is remarkable that flow in the bridging vein remains constant even though the pressure gradient to the CVP. This phenomenon that venous outflow from an encapsulated organ continues at a constant rate independent of the pressure gradient is consistent with the aforementioned “waterfall flow phenomenon”. Only by being independent of pressure is the venous outflow able to match the arterial inflow into brain, at least theoretically.
To become independent of pressure the venous outflow must be regulated by a pressure variable resistance, outflow cuff segment, interpositioned between the bridging vein (high pressure) and the SSS (low pressure equal to CVP). Otherwise the bridging veins would drain empty and collapse without hindrance. The cuff structure is supposed to occur gradually as ICP is elevated which protected the cortical veins from collapse during increased ICP. This implies that there is a progressive increase in resistance to the cerebral venous outflow with increasing ICP. The biomechanical measurements in our parallel study [19] have shown that the diameter of the “outflow cuff segment” is about one-third of the cerebral bridging venous diameter. According to the Poiseuille’s law, the resistance to flow through the outflow cuff segment is about 25 times higher than through the regular part of the cerebral bridging vein. These observations were made at an intraluminal pressure of 4 mmHg that is considered close to physiological values. In this connection, the outflow cuff segment may be regarded as a valve that provides stabilization of the venous outflow from the brain otherwise challenged by variations in the ICP and in the SSS pressure conditioned by postural changes or moderate valsalva exercises.
PI is defined as the blood flow velocity pulse amplitude divided by the mean flow velocity. The PI reflects the degree of pulsatile flow and increases with an increase in peripheral vascular resistance. Accordingly, the observed progressive increases in PI in the cerebral bridging veins during the elevations of ICP indicate that the vascular resistance to venous outflow increases (Fig. 7).
ICP as the Only Variable
This study indicates the hemodynamic response of the cerebral bridging veins and other variables to moderate elevations in ICP. No significant changes in physiological variables including MABP or PaCO2 occurred. CVP remained very stable indicating no central resistance to obstruct venous outflow from the intracranial cavity. At the same time, CBF remained stable and independent of ICP due to autoregulation of blood flow within the changes in ICP and CPP that occurred in this study. This is indicated by the 133Xe measurements of CBF with the exception of a slight fall in CBF during hyperventilation and ICP = 30 mmHg during which CPP dropped to 50.6 ± 5.8 mmHg. Accordingly, the venous relative stasis during increased ICP is neither caused by central venous resistance nor by changes in CBF. As intended, CBF was reduced to a lower level by hyperventilation to provide observations of the venous response at two different levels of CBF. Essentially the same type of response was observed during hyperventilation, however, at a lower level of venous flow and CBF. The response occurred at two different levels of CBF and was not related to other variables such as CVP, MABP, or PaCO2. The results clearly indicate relative stasis of the cerebral bridging veins as a response to ICP, as the only variable.
Another important finding of this study is that hyperventilation had little effect on venous blood volume. The hemodynamic response of cerebral venous system is actually balanced by decreased velocity and dilated veins so that total volume flow in the veins remains stable. Since hyperventilation is still used for reducing ICP clinically or operationally, this finding drop a hint that venous volume does not play a role in hyperventilation-induced ICP change. Considering 80% even more of the total brain blood volume is in the venous side of the circuit, it could be an explanation that hyperventilation is not very efficient to release ICP due to maintained drainage of venous blood.
This study corroborates previous studies of the cerebral bridging veins and venous outflow from the brain [20]. The results illustrate the general physiological problem of venous outflow from an encapsulated organ having a higher intracapsular tissue pressure than the surroundings, i.e., the problem of maintaining flow through collapsible tubes like the veins passing from a compartment of higher pressure to a compartment of lower pressure. In conclusion, moderate elevation of ICP is associated with the balanced increase of the venous outflow resistance which causing relative stasis with dilatation and slowing of flow velocity in the cerebral bridging veins. This response occurred at two different levels of CBF during normo- and hyperventilation, and was not related to other factors such as CVP, MABP, or PaCO2. Hence, the cerebral venous blood volume cannot be considered as a volume buffer, which may be reduced by therapeutical strategies in conditions of increased ICP.
References
Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56(12):1746–8.
Luce JM, Huseby JS, Kirk W, Butler J. A Starling resistor regulates cerebral venous outflow in dogs. J Appl Physiol. 1982;53(6):1496–503.
Holt JP. Flow through collapsible tubes and through in situ veins. IEEE Trans Biomed Eng. 1969;16(4):274–83.
Cirovic S, Walsh C, Fraser WD. Mathematical study of the role of non-linear venous compliance in the cranial volume-pressure test. Med Biol Eng Comput. 2003;41(5):579–88.
Piechnik SK, Czosnyka M, Richards HK, Whitfield PC, Pickard JD. Cerebral venous blood outflow: a theoretical model based on laboratory simulation. Neurosurgery. 2001;49(5):1214–22.
Pranevicius M, Pranevicius O. Cerebral venous steal: blood flow diversion with increased tissue pressure. Neurosurgery. 2002;51(5):1267–73. (discussion 1273–1274).
Monson KL, Goldsmith W, Barbaro NM, et al. Significance of source and size in the mechanical response of human cerebral blood vessels. J Biomech. 2005;38(4):737–44.
Rosengarten B, Ruskes D, Mendes I, et al. A sudden arterial blood pressure decrease is compensated by an increase in intracranial blood volume. J Neurol. 2002;249(5):538–41.
Lassen NA, Ingvar DH. Radioisotopic assessment of regional cerebral blood flow. Prog Nucl Med. 1972;1:376–1409.
Bada HS, Miller JE, Menke JA, et al. Intracranial pressure and cerebral arterial pulsatile flow measurement in neonatal intraventricular hemorrhage. J Pediatr. 1982;100(2):291–6.
Permutt S, Bromberger-Barnea B, Bane HN. Alveolar pressure, pulmonary venous pressure, and the vascular waterfall. Med Thorac. 1962;19:239–60.
Beloucif S, Brienza N, Andreoni K, et al. Distinct behavior of portal venous and arterial vascular waterfalls in porcine liver. J Crit Care. 1995;10(3):104–14.
Gosselin RE, Kaplow SM. Venous waterfalls in coronary circulation. Theor Biol. 1991;149(2):265–79.
Versluis JP, Heslinga JW, Sipkema P, et al. Microvascular pressure measurement reveals a coronary vascular waterfall in arterioles larger than 110 micron. Am J Physiol Heart Circ Physiol. 2001;281(5):H1913–8.
van Donkelaar CC, Huyghe JM, Vankan WJ, et al. Spatial interaction between tissue pressure and skeletal muscle perfusion during contraction. J Biomech. 2001;34(5):631–7.
Asgeirsson B, Grande PO. Effects of arterial and venous pressure alterations on transcapillary fluid exchange during raised tissue pressure. Intensive Care Med. 1994;20(8):567–72.
Nakagawa Y, Tsuru M, Yada K. Site and mechanism for compression of the venous system during experimental intracranial hypertension. J Neurosurg. 1974;41(4):427–34.
Si Z, Luan L, Kong D, et al. MRI-based investigation on outflow segment of cerebral venous system under increased ICP condition. Eur J Med Res. 2008;13(3):121–6.
Pang Q, Lu X, Gregersen H, Oettingen Gv, Astrup J. Biomechanical properties of porcine cerebral bridging veins with reference to the zero-stress state. J Vasc Res. 2001;38(1):83–90.
Doepp F, Schreiber SJ, von Munster T, et al. How does the blood leave the brain? A systematic ultrasound analysis of cerebral venous drainage patterns. Neuroradiology. 2004;46(7):565–70.
Acknowledgments
This work was funded by the National Natural Science Foundation of China No. 30571917. We thank Shandong Provincial Medical Imaging Research Institute in China for their support in MRI technique.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yanbing Yu and Jie Chen contributed equally to this work.
Rights and permissions
About this article
Cite this article
Yu, Y., Chen, J., Si, Z. et al. The Hemodynamic Response of the Cerebral Bridging Veins to Changes in ICP. Neurocrit Care 12, 117–123 (2010). https://doi.org/10.1007/s12028-009-9299-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9299-4