Abstract
Introduction
Tight glycemic control (TGC) after ischemic stroke may improve clinical outcome but previous studies failed to establish TGC, principally because of postprandial glucose surges. The aim of the present study was to investigate if safe, effective and feasible TGC can be achieved with continuous tube feeding and a computerized treatment protocol.
Methods
We subjected ten acute ischemic stroke patients with admission hyperglycemia (glucose >7.0 mmol/l (126.0 mg/dl)) to continuous tube feeding and a computerized intensive protocol with insulin adjustments every 1–2 h. Two groups of regularly fed patients from a previous study with a similar design served as controls. These groups comprised hyperglycemic patients treated according to an intermediate protocol with insulin adjustments at standard intervals (N = 13), and normoglycemic controls treated according to standard care (N = 15). The primary outcome was the percentage of time within target (4.4–6.1 mmol/l (79.2–109.8 mg/dl)). Secondary outcome was the number of patients with hypoglycemic episodes (glucose <3.0 mmol/l (54.0 mg/dl)).
Results
Median time within target was 55% in the continuously fed intensive group compared to 19% in the regularly fed intermediate group, and 58% in normoglycemic controls. Hypoglycemic episodes occurred in 20% of patients in the continuously fed group—lowest glucose level 2.4 mmol/l (43.2 mg/dl). In contrast, in the regularly fed group, this was 31%—lowest glucose level 1.6 mmol/l (28.8 mg/dl).
Conclusions
TGC after acute ischemic stroke is feasible with continuous tube feeding and a computerized intensive treatment protocol. Although glycemic control is associated with hypoglycemia, no severe hypoglycemia occurred in the continuous tube feeding group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In acute ischemic stroke, hyperglycemia on admission and during the clinical course is associated with increased infarct expansion, worse clinical outcome and increased case-fatality [1–6]. Tight glycemic control (TGC) was shown to improve clinical outcome in critically ill patients [7–9], and has been implemented worldwide on intensive care units (ICU).
Recently, TGC has become the subject of debate. Several clinical trials demonstrated that TGC increases the risk of severe hypoglycemia and was not associated with an overall mortality benefit [10, 11]. It remains unclear why these recent and earlier trials showed different results. Further post hoc analyses, more closely exploring subgroups of patients and the role of (severe) hypoglycemia, are awaited.
Various subgroups of patients could still benefit from TGC [12], and recently, TGC was associated with improved outcome in aneurysmal subarachnoid hemorrhage [13]. In experimental studies, several mechanisms could account for an adverse outcome of hyperglycemia after acute ischemic stroke [14, 15]. Therefore, high levels of blood glucose might also be targeted to improve clinical outcome in patient with ischemic stroke. Until now, only one clinical trial has investigated this, but no beneficial effect of glycemic control on clinical outcome was demonstrated [16]. In this trial, however, glycemic control was short lasting and poorly regulated. Treatment lasted for just 24 h and resulted in only a small contrast in the mean glucose levels (0.57 mmol/l (10.26 mg/dl)) between treated patients and controls.
To attain a clinical benefit from TGC on clinical outcome, it is important that blood glucose levels are maintained in the lower physiological range (below 6.1 mmol/l (109.8 mg/dl)), without (severe) hypoglycemia [17, 18]. It is, however, difficult to establish TGC, especially outside the ICU setting [19–22]. This seems particularly true for ischemic stroke patients. Various TGC protocols have been investigated in stroke patients, but hitherto none has managed to establish TGC, maintaining blood glucose levels in the lower physiological range (4.4–6.1 mmol/l (79.2–109.8 mg/dl)) or even within the predefined target range [19, 23–25]. Possible explanations for this are a relatively high rate of (previously unrecognized) insulin resistance or diabetes mellitus, high levels of stress inflicted by the stroke and a high rate of in-hospital infections accompanying stroke [26–30]. Another, potentially modifiable factor, is the feeding pattern of stroke patients. In contrast to patients admitted to an ICU, patients on a stroke unit often resume oral intake after an initial phase of starvation, rendering nutritional intake unpredictable. Indeed, we [22] and others [19] reported previously that strict glucose control is hampered by postprandial glucose surges. Besides unpredictable feeding patterns, less intensive care with a lower frequency of blood glucose assessments could also hamper TGC on a stroke unit as compared to the ICU setting. The use of a computer supported treatment protocol and increasing the rate of insulin adjustments has the potential to enhance TGC [31, 32].
The aim of the present study was therefore to investigate if safe, effective and feasible TGC can be established on a stroke unit by subjecting patients to continuous tube feeding that is guided by treatment with an intensive, computer supported algorithm.
Methods
Patients
Ischemic stroke patients from a continuing cohort of ischemic stroke patients were consecutively recruited from two university hospitals and one large regional hospital in the Netherlands. All patients had a supra-tentorial infarct within the last 24 h and gave written informed consent. Exclusion criteria were insulin use before admission (i.e. patients with oral hypoglycemic agents or non insulin dependent diabetics were included), admission Glasgow coma scale below 8, renal deficiency (creatinine >150 μmol/l), HIV positivity, age below 18 years and pregnancy.
For the present study, ten consecutive patients with hyperglycemia on admission (blood glucose exceeding 7.0 mmol/l (126.0 mg/dl)) were subjected to continuous tube feeding and an intensive, computer supported treatment algorithm (the continuously fed intensive group). Since we did not want to subject non-dysphagic patients with minor neurological deficit to continuous tube feeding, we excluded patients without a substantial neurological deficit defined as a National Institutes of Health Stroke Scale (NIHSS) of at least four.
Regularly fed ischemic stroke patients from a recent randomized study [22], also aiming to improve glycemic control, served as reference groups. These groups comprised regularly fed patients with admission hyperglycemia treated according to an intermediate intensive insulin infusion protocol (the regularly fed intermediate group), and regularly fed patients with normoglycemia on admission treated according to routine practice.
Interventions
Patients included in the continuously fed intensive group received 1.5 l of continuous tube feeding per 24 h, aiming at 2000 kcal/day. Insulin infusions in this group were adjusted based on fingerpick glucose assessments every hour until glucose levels remained on target for two consecutive hours, and every 2 h thereafter. Adjustments to the insulin infusion rate were made according to a sliding scale regime and calculated from the previous glucose level, the actual glucose level and the actual insulin infusion rate. Insulin infusion adjustments were performed with the aid of a web-based computerized algorithm that was modified from a previously used predefined paper written algorithm [22] with the aim of maintaining glucose levels between 4.4 and 6.1 mmol/l (79.2 and 109.8 mg/dl). Execution of the protocol was left to the nursing staff with the possibility of consulting the principal investigator at all times. A coordinating nurse was allocated to each center to register possible difficulties arising during the study period.
Patients included in the regularly fed intermediate group received a predominantly basal intravenous insulin algorithm also with the aim to maintain glucose levels between 4.4 and 6.1 mmol/l (79.2 and 109.8 mg/dl) for 5 consecutive days. In this protocol, glucose levels were assessed with fingerpicks every hour till target levels were reached. After this, insulin infusion was adjusted at standard intervals by a physician experienced in diabetes care: immediately before, 2 h after each meal and around 22:30 (i.e. each 2–3 h, 7 times in 14 h). Insulin infusion rate was adjusted with the aid of a predefined paper written treatment protocol according to a sliding scale regimen. Adjustment of infusion rate was calculated from the previous glucose level, the actual glucose level and the actual insulin infusion rate. Meal-related insulin was intravenously administered as bolus insulin in a dose equal to the newly calculated hourly insulin infusion rate.
For regularly fed normoglycemic controls, glucose levels were monitored with fingerpicks at the same intervals as in the regularly fed intermediate group. Glycemic control in this group was left to the treating physician. In practice, this consisted of subcutaneous short acting insulin administered if glucose values exceeded 16.6 mmol/l (298.8 mg/dl).
Patients in the regularly fed hyperglycemic group and normoglycemic controls were encouraged to eat standard meals (a balanced diet of approximately 2000 kcal/day). Dysphagic patients received intermittent enteral feeding gradually increasing over the first 2 or 3 days, aiming at 2000 kcal/day.
For patients in all groups, glucose levels below 3.5 mmol/l (63.0 mg/dl) were treated by interrupting insulin administration and by intravenous administration of 50 ml glucose 20%. After this, glucose levels were monitored each 30 min until levels returned within range.
The study protocol was approved by the local ethics committee of all institutions.
Outcomes
The primary efficacy outcome was defined as the time spent within the target range (4.4–6.1 mmol/l (79.2–109.8 mg/dl)) during days 1–5. Day 1 started at the first measurement on the day after inclusion. In addition, we calculated the mean glucose levels over the study period.
Secondary safety outcomes were the number of patients with a hypoglycemic episode (glucose <3.0 mmol/l (54.0 mg/dl)). We chose a higher cut-off to define hypoglycemia than used in previous ICU based studies (2.2 mmol/l (39.6 mg/dl)) as the deleterious effects of hypoglycemia are potentially more harmful to the ischemic brain. As there exists no universally accepted definition of hypoglycemia in hospitalized patients with ischemic stroke treated with TGC, we further defined serious hypoglycemia (glucose <2.5 mmol/l (45.0 mg/dl)) and registered the lowest glucose value in each group. Other secondary safety outcomes were the number of hypoglycemic episodes per group divided by the total number of glucose assessments in that group (we anticipated that the number of glucose assessments would be larger in the continuously fed intensive group), and the number of symptomatic hypoglycemic episodes (i.e. hypoglycemia accompanied by perspiration, tachycardia, tremor, confusion or coma). Because we were particularly interested in the effect of feeding interval on glycemic control, we used daytime glucose assessments (08:30–22:30 h) for analyses.
To explore how the nursing staff experienced the execution of the protocol in the continuously fed intensive group, we recorded the number, and the reasons for consultation of the principal investigator. In addition, we held structured interviews with the coordinating nurse of each center after the study had ended to gain more insight into subjective experiences related to the execution of the protocol.
Statistical Analysis
Baseline characteristics were presented as means or medians as appropriate. Baseline and outcome between-group differences of continuous variables were calculated with the Students t-test or the Mann–Whitney U-test as appropriate. Dichotomous variables were analyzed with the χ2 or Fisher’s exact test as appropriate. To calculate the mean time spent within the target range, we linearly interpolated glucose values for each 30 min.
All analyses were performed according to the intention-to-treat principle. Therefore, if patients discontinued the study protocol between day 1 and 5, glucose measurements till then were included in the analysis.
Results
Patient Inclusion
One patient in the regularly fed normoglycemic group had to be excluded because informed consent was withdrawn before day 1. Ten patients discontinued the study between day 1 and 5: two patients in the continuously fed intensive group (imminent death and withdrawal of informed consent), two patients in the regularly fed intermediate group (logistic failure and withdrawal of informed consent) and six patients in the regularly fed normoglycemic group (imminent death [2], withdrawal of informed consent [2], early discharge because of rapid clinical improvement and transfer to another hospital).
Baseline Characteristics
Baseline characteristics are summarized in Table 1. Patients in the continuously fed intensive group had more severe strokes because of the requirement of a NIHSS score of at least four for this group.
Primary Outcome
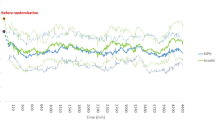
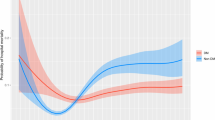
Figure 1 shows the distribution of the percentage of time spent within the target range during the treatment period. The median percentage of time spent within the target range was similar for the continuously fed intensive group (55%) and regularly fed normoglycemic controls (58%). These values were significantly higher when compared to the regularly fed intermediate group (19%) (P < 0.001, Mann–Whitney rank tests).
Table 2 shows that the mean glucose level during treatment in the continuously fed intensive group (5.8 ± 0.3 mmol/l (104.4 ± 5.4 mg/dl)) was significantly lower than that in the regularly fed intermediate group (7.6 ± 1.5 mmol/l (136.8 ± 27.0 mg/dl); P < 0.005) and similar to that in the regularly fed normoglycemic group (5.9 ± 1.2 mmol/l (106.2 ± 21.6 mg/dl)).
Secondary Outcomes
Table 2 also shows that in the continuously fed intensive group, two patients (20%) had a serious hypoglycemic episode, and the lowest glucose value was 2.4 mmol/l (43.2 mg/dl). In the regularly fed intermediate group, four patients (31%) had a hypoglycemic episode, two of which were serious (15%) with a lowest glucose value of 1.6 mmol/l (28.8 mg/dl). The total number of hypoglycemic episodes divided by the total number of glucose assessments did not differ between the groups. None of the (serious) hypoglycemic episodes was symptomatic.
For patients in the continuously fed intensive group, the principal investigator had to be consulted only once because of a failure to connect to the internet. The interviews with the coordinating nurse revealed that the execution of the protocol was laborious due to the high number of glucose assessments, but well appreciated as it appeared very straightforward. Also, the fact that the execution of the intensive protocol could be done without the intervention of a physician was well appreciated.
Discussion
This study demonstrates that by subjecting ischemic stroke patients with admission hyperglycemia to continuous tube feeding, glucose levels can be maintained in a low physiological range with the aid of a computer supported intensive protocol. Furthermore, this was established for 5 consecutive days with only minimal consultation of treating or consulting physicians. Glycemic control was accompanied by hypoglycemic episodes in both the intensive and the intermediate treatment protocol.
To our knowledge, this is the first study to achieve TGC for 5 consecutive days in acute ischemic stroke patients with admission hyperglycemia. Recently, a predominantly ICU-based trial in diabetic patients with ischemic stroke managed to lower blood glucose levels for 72 h, but the mean glucose level of 7.4 mmol/l (133.2 mg/dl) was much higher than what we achieved and still outside the predefined target range (<7.2 mmol/l (129.6 mg/dl)) [25]. The glucose profiles we established were similar to glucose profiles in critically ill patients treated with insulin infusions in ICU-based trials that demonstrated a beneficial effect of TGC on the clinical outcome [33–35]. Furthermore, the glucose profiles were similar as in the normoglycemic controls. Continuous feeding appears therefore crucial to establish TGC in acute ischemic stroke.
The major drawback of TGC, also in our study, is the accompanying increased risk of severe hypoglycemia. Recently, a clinical trial investigating TGC in patients with severe sepsis was stopped early because TGC-related hypoglycemia increased the risk of serious adverse events [36]. Moreover, in another recent large clinical ICU-based trial, 7% of TGC treated patients had at least one episode of severe hypoglycemia and this may have contributed to the increased mortality observed [11]. It is important to note that in this and most other ICU-based studies, the cut-off to define hypoglycemia (<2.2 mmol/l (39.6 mg/dl)) is much lower than ours (3.0 mmol/l (54.0 mg/dl)). In fact, if we had used the same cut-off, we would not have found any hypoglycemic episode in the continuously fed intensive group. Still, caution is warranted especially after ischemic stroke, as the effects of low glucose levels on the ischemic brain are potentially harmful, even if glucose levels are just slightly below normal. In experimental studies, low glucose levels were shown to increase infarct size and mortality [37], and the benefit of glucose lowering is lost when glucose levels fall below the level of 2 to 3 mmol/l (36 to 54 mg/dl) [38].
The intensive protocol we used demanded that non-dysphagic patients also are subjected to continuous tube feeding. By its invasive nature, this may have led to considerable patient discomfort. Despite this discomfort, none of the patients withdrew consent for this reason. One patient in the continuously fed intensive group withdrew consent because of the high frequency of fingerpicks. Nowadays, continuous glucose monitoring systems are available, which might be of benefit for both patients and caregivers, offering advantages to our intensive protocol [39, 40].
A limitation of our study is that we used historic controls for comparison. Furthermore, because of ethical considerations, the inclusion criteria differed somewhat, with the inclusion of more severe strokes in the continuously fed intensive group. However, all patient groups were treated on the same stroke units and standard stroke care was maintained in the period that separated the inclusion periods, minimizing a possible time effect. Moreover, the inclusion of more severe strokes in the continuously fed intensive group probably does not debilitate our results, as achieving TGC is presumed to be more difficult in a more severe stroke [27, 41].
In conclusion, effective and feasible TGC on a stroke unit can be achieved by subjecting patients to continuous tube feeding, a high rate of insulin adjustments (every 1–2 h) and by facilitating the nursing staff with a computer supported treatment algorithm. However, caution is warranted as TGC is also associated with hypoglycemia. Further studies should address this problem as low levels of blood glucose might be detrimental, especially for the ischemic brain.
References
Baird TA, Parsons MW, Phanh T, Butcher KS, Desmond PM, Tress BM, et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke. 2003;34:2208–14. doi:10.1161/01.STR.0000085087.41330.FF.
Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein HC. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–32. doi:10.1161/hs1001.096194.
Chalela JA, Merino JG, Warach S. Update on stroke. Curr Opin Neurol. 2004;17:447–51. doi:10.1097/01.wco.0000137536.06986.f9.
Els T, Klisch J, Orszagh M, Hetzel A, Schulte-Monting J, Schumacher M, et al. Hyperglycemia in patients with focal cerebral ischemia after intravenous thrombolysis: influence on clinical outcome and infarct size. Cerebrovasc Dis. 2002;13:89–94. doi:10.1159/000047756.
Parsons MW, Barber PA, Desmond PM, Baird TA, Darby DG, Byrnes G. Acute hyperglycemia adversely affects stroke outcome: a magnetic resonance imaging and spectroscopy study. Ann Neurol. 2002;52:20–8. doi:10.1002/ana.10241.
Yong M, Kaste M. Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke. 2008;39(10):2749–55. doi:10.1161/STROKEAHA.108.514307.
Krinsley JS. Effect of an intensive glucose management protocol on the mortality of critically ill adult patients. Mayo Clin Proc. 2004;79:992–1000. doi:10.4065/79.8.992.
van den Berghe WA, Hermans G, Meersseman W, Wouters PJ, Milants I. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61. doi:10.1056/NEJMoa052521.
van den Berghe WA, Milants I, Wouters PJ, Bouckaert B, Bruyninckx F. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55:3151–9. doi:10.2337/db06-0855.
Wiener RS, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008;300:933–44. doi:10.1001/jama.300.8.933.
Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97. doi:10.1056/NEJMoa0810625.
Griesdale DE, de Souza RJ, van Dam RM, Heyland DK, Cook DJ, Malhotra A. Intensive insulin therapy and mortality among critically ill patients: a meta-analysis including NICE-SUGAR study data. CMAJ. 2009.
Latorre JG, Chou SH, Nogueira RG, Singhal AB, Carter BS, Ogilvy CS. Effective glycemic control with aggressive hyperglycemia management is associated with improved outcome in aneurysmal subarachnoid hemorrhage. Stroke. 2009.
Garg R, Chaudhuri A, Munschauer F, Dandona P. Hyperglycemia, insulin, and acute ischemic stroke: a mechanistic justification for a trial of insulin infusion therapy. Stroke. 2006;37:267–73. doi:10.1161/01.STR.0000195175.29487.30.
Martini SR, Kent TA. Hyperglycemia in acute ischemic stroke: a vascular perspective. J Cereb Blood Flow Metab. 2007;27:435–51. doi:10.1038/sj.jcbfm.9600355.
Gray CS, Hildreth AJ, Sandercock PA, O’Connell JE, Johnston DE, Cartlidge NE. Glucose–potassium–insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007;6:397–406. doi:10.1016/S1474-4422(07)70080-7.
Langouche L, Vanhorebeek I, van den Berghe G. Therapy insight: the effect of tight glycemic control in acute illness. Nat Clin Pract Endocrinol Metab. 2007;3:270–8. doi:10.1038/ncpendmet0426.2004;114:1187-95.
van den Berghe G. How does blood glucose control with insulin save lives in intensive care? J Clin Invest. 2004;114:1187–95.
Bruno A, Saha C, Williams LS, Shankar R. IV insulin during acute cerebral infarction in diabetic patients. Neurology. 2004;62:1441–2.
Hassan E. Hyperglycemia management in the hospital setting. Am J Health Syst Pharm. 2007;64:S9–14. doi:10.2146/ajhp070102.
McCormick MT, Muir KW, Gray CS, Walters MR. Management of hyperglycemia in acute stroke: how, when, and for whom? Stroke. 2008;39:2177–85. doi:10.1161/STROKEAHA.107.496646.
Vriesendorp TM, Roos YBWEM, Kruyt ND, Biessels GJ, Kappelle LJ, Vermeulen M. Efficacy and safety of two 5-day insulin dosing regimens to achieve strict glycemic control in patients with acute ischemic stroke. J Neurol Neurosurg Psychiatry. 2009 (in press).
Walters MR, Weir CJ, Lees KR. A randomised, controlled pilot study to investigate the potential benefit of intervention with insulin in hyperglycaemic acute ischaemic stroke patients. Cerebrovasc Dis. 2006;22:116–22. doi:10.1159/000093239.
Kreisel SH, Berschin UM, Hammes HP, Leweling H, Bertsch T, Hennerici MG. Pragmatic management of hyperglycaemia in acute ischaemic stroke: safety and feasibility of intensive intravenous insulin treatment. Cerebrovasc Dis. 2009;27:167–75. doi:10.1159/000185608.
Bruno A, Kent TA, Coull BM, Shankar RR, Saha C, Becker KJ. Treatment of Hyperglycemia in Ischemic Stroke (THIS). A randomized pilot trial. Stroke. 2007.
Johnston KC, Li JY, Lyden PD, Hanson SK, Feasby TE, Adams RJ. Medical and neurological complications of ischemic stroke: experience from the RANTTAS trial. RANTTAS investigators. Stroke. 1998;29:447–53.
O’Neill PA, Davies I, Fullerton KJ, Bennett D. Stress hormone and blood glucose response following acute stroke in the elderly. Stroke. 1991;22:842–7.
Christensen H, Boysen G, Johannesen HH. Serum-cortisol reflects severity and mortality in acute stroke. J Neurol Sci. 2004;217:175–80. doi:10.1016/j.jns.2003.09.013.
Vancheri F, Curcio M, Burgio A, Salvaggio S, Gruttadauria G, Lunetta MC. Impaired glucose metabolism in patients with acute stroke and no previous diagnosis of diabetes mellitus. QJM. 2005;98:871–8. doi:10.1093/qjmed/hci134.
Kernan WN, Viscoli CM, Inzucchi SE, Brass LM, Bravata DM, Shulman GI. Prevalence of abnormal glucose tolerance following a transient ischemic attack or ischemic stroke. Arch Intern Med. 2005;165:227–33. doi:10.1001/archinte.165.2.227.
Braithwaite SS. Inpatient insulin therapy. Curr Opin Endocrinol Diabetes Obes. 2008;15:159–66.
Hermayer KL, Neal DE, Hushion TV, Irving MG, Arnold PC, Kozlowski L. Outcomes of a cardiothoracic intensive care web-based online intravenous insulin infusion calculator study at a Medical University Hospital. Diabetes Technol Ther. 2007;9:523–34.
Cordingley JJ, Vlasselaers D, Dormand NC, Wouters PJ, Squire SD, Chassin LJ. Intensive insulin therapy: enhanced model predictive control algorithm versus standard care. Intensive Care Med. 2009;35:123–8. doi:10.1007/s00134-008-1236-z.
Hovorka R, Kremen J, Blaha J, Matias M, Anderlova K, Bosanska L. Blood glucose control by a model predictive control algorithm with variable sampling rate versus a routine glucose management protocol in cardiac surgery patients: a randomized controlled trial. J Clin Endocrinol Metab. 2007;92:2960–4. doi:10.1210/jc.2007-0434.
Plank J, Blaha J, Cordingley J, Wilinska ME, Chassin LJ, Morgan C. Multicentric, randomized, controlled trial to evaluate blood glucose control by the model predictive control algorithm versus routine glucose management protocols in intensive care unit patients. Diabetes Care. 2006;29:271–6. doi:10.2337/diacare.29.02.06.dc05-1689.
Brunkhorst FM, Engel C, Bloos F, Meier-Hellmann A, Ragaller M, Weiler N. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39. doi:10.1056/NEJMoa070716.
de Courten-Meyers, Kleinholz M, Wagner KR, Myers RE. Normoglycemia (not hypoglycemia) optimizes outcome from middle cerebral artery occlusion. J Cereb Blood Flow Metab. 1994;14:227–36.
Zhu CZ, Auer RN. Optimal blood glucose levels while using insulin to minimize the size of infarction in focal cerebral ischemia. J Neurosurg. 2004;101:664–8.
Chase JG, Shaw GM. Is there more to glycaemic control than meets the eye? Crit Care. 2007;11:160. doi:10.1186/cc6099.
Hovorka R. The future of continuous glucose monitoring: closed loop. Curr Diabetes Rev. 2008;4:269–79. doi:10.2174/157339908785294479.
Wong AA, Schluter PJ, Henderson RD, O’Sullivan JD, Read SJ. Natural history of blood glucose within the first 48 hours after ischemic stroke. Neurology. 2008;70:1036–41. doi:10.1212/01.wnl.0000306635.08410.68.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kruyt, N.D., Biessels, G.J., Vriesendorp, T.M. et al. Subjecting Acute Ischemic Stroke Patients to Continuous Tube Feeding and an Intensive Computerized Protocol Establishes Tight Glycemic Control. Neurocrit Care 12, 62–68 (2010). https://doi.org/10.1007/s12028-009-9230-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-009-9230-z