Abstract
Introduction
In patients with severe head trauma, endotracheal suctioning can result in adverse reactions including cough, systemic hypertension, increased intracranial pressure, and reduced cerebral perfusion pressure. The aim of this prospective, blinded clinical trial in mechanically ventilated patients with severe head trauma whose cough reflexes were still intact was to assess the effectiveness of endotracheally instilled lidocaine in preventing endotracheal suctioning-induced changes in cerebral hemodynamics (increase in intracranial pressure and reduced cerebral perfusion pressure) after a single endotracheal suctioning.
Methods and Results
Ten minutes after lidocaine instillation into the endotracheal tube, secretions were suctioned for <30 s through a standard closed endotracheal suctioning circuit. Heart rate, arterial pressure, intracranial pressure, and cerebral perfusion pressure were continuously monitored. The first patient studied received an endotracheal lidocaine dose of 2.0 mg/kg. The dose for the next study patient was titrated upwards or downwards in 0.5 mg/kg steps according to, whether the intracranial pressure reached the predefined threshold of ≥20 mmHg. A total of 41 patients were studied. Lidocaine instillation into the endotracheal tube had no effect on hemodynamic and ventilatory variables. In 21 patients lidocaine dose instilled into the endotracheal tube effectively prevented the endotracheal suctioning-induced intracranial pressure increase behind the predefined threshold of ≥20 mmHg and cerebral perfusion pressure remained unchanged. In the remaining 20, although intracranial pressure rose significantly cerebral perfusion pressure remained constant.
Conclusions
In mechanically ventilated patients with severe head trauma endotracheal lidocaine instillation effectively and dose-dependently prevents the endotracheal suctioning-induced intracranial pressure increase and cerebral perfusion pressure reduction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary goals in managing severe head trauma are to prevent cerebral ischemia and acute intracranial hypertension [1–3]. Endotracheal suctioning is a nursing procedure that needs to be frequently repeated in intubated and mechanically ventilated patients to optimize gas exchange in the lungs and to minimize the risk of ventilator associated pneumonia [4]. Some studies including severe head trauma patients with and without cough reflexes disagree on whether coughing needs to be prevented in patients with severe head trauma [5, 6]. Nevertheless, in patients with severe head trauma, who move or cough during endotracheal suctioning the intracranial pressure (ICP) increases, while cerebral perfusion pressure (CPP) and jugular oxygen saturation decrease [7]. These adverse cerebral hemodynamic events can have catastrophic consequences, especially, when cerebral auto-regulation is lost because of head trauma [8, 9]. Although several techniques or pharmacological agents have been proposed to prevent increased ICP during endotracheal suctioning in patients with severe head trauma, including hyperventilation [10], muscle relaxants [1] and topical, and systemic use of local anesthetics including lidocaine [1, 11, 12] and more recently infusion of the sedative opioid remifentanil [13], all have adverse effects that limit their clinical application. Hyperventilation, for example, abruptly reduces carbon dioxide tension, and thereby, reducing cerebral perfusion thus increasing the risk of cerebral ischemia [14] and causes hyperinflation thus worsening ICP [15]. The use of muscle relaxants lengthens patients’ stay in the intensive care unit and increases the incidence of sepsis, pneumonia and neuropathy [16]. Sedation alters systemic and cerebral hemodynamics (possibly reducing CPP) and precludes neurological examination [13, 17]. Earlier clinical trials did not resolve the clinical problem of endotracheal suctioning-induced changes in cerebral hemodynamics.
Lidocaine-injected intravenously blunts the cough reflex in awake and anesthetized patients [1], and has potential neuroprotective effects [18], an advantage in patients with severe head trauma. More recent evidence demonstrates that lidocaine sprayed down the endotracheal tube attenuates the airway-circulatory reflexes during emergence and extubation after general anesthesia [19]. These evidences prompted us to reappraise the issue of endotracheal lidocaine instillation for blunting endotracheal suctioning-induced cerebral hemodynamic changes in patients undergoing intensive care after severe head trauma.
Our primary objective of this prospective, blinded clinical trial in mechanically ventilated patients with severe head trauma whose cough reflexes were still intact was to assess the effectiveness of endotracheally instilled lidocaine in preventing the endotracheal suctioning-induced cerebral hemodynamic changes (ICP increase and CPP reduction) after a single endotracheal suctioning. Systemic and cerebral hemodynamics was assessed in patients in whom endotracheal lidocaine instillation failed or succeeded in preventing ICP from increasing to ≥20 mmHg during endotracheal suctioning. We also determined the lidocaine dose that prevents the ICP increase during endotracheal suctioning in 50% of these patients.
Materials and Methods
After obtaining approval from the hospital ethics committee, an informed consent was obtained from patients’ next of kin. In this study, we prospectively enrolled consecutive patients older than 18 years, admitted to the neurointensive care unit with severe closed-head injury (Glasgow Coma Scale score of ≤8 and ICP monitoring). Patients were studied 3 days after admission within the first week after head trauma and were all intubated and mechanically ventilated. Patients were sedated with continuous infusion of propofol (3–5 mg/kg/h). No muscle relaxants were used. According to our standard practice, patients with a CPP below 70 mmHg received a continuous infusion of dopamine titrated to achieve this target. Patients were suitable for inclusion only if they had stable hemodynamics (CPP >70 mmHg and ICP ≤20 mmHg for 24 h or more). In this study, we have enrolled only patients who moved or coughed during endotracheal suctioning with transient acute increase of ICP (i.e. ICP >20 mmHg) [7]. Patients with intracranial hypertension (ICP >20 mmHg), those in whom endotracheal suctioning did not increase ICP to more than 20 mmHg, and patients with severe pulmonary failure (acute lung injury, PaO2 /FiO2 <300) were excluded.
Data Collection
Heart rate (HR) with 3-lead ECG, invasive mean arterial pressure (MAP), arterial oxygen saturation (SpO2) by pulse oximetry and end-tidal CO2 (ETCO2), were continuously monitored (Siemens SC 7000, Sweden). Ventilation (tidal volume and respiratory rate) was adjusted to maintain PaCO2 between 33 and 37 mmHg. The ICP, and the derived CPP value, were continuously monitored with an intraparenchymal catheter (Rehau System, Switzerland). During the study period, the blood flow velocity in the mid cerebral artery (VMCA, cm/sec) was measured with a 2-MHz pulsed Doppler ultrasound device (Computer Medics, DWL, Multi Dop, Germany), after identifying the middle cerebral artery, and adjusting the focus by 2-mm increments to obtain peak VMCA signals from the proximal (M1) segment.
The threshold value for acute intracranial hypertension was defined to be endotracheal suctioning-induced changes leading to ICP ≥20 mmHg during and within 1 min after endotracheal suctioning (peak ICP value). The systemic and cerebral hemodynamic values were recorded by an observer blinded to the lidocaine dose instilled. Only routine endotracheal suctioning procedures, planned as part of the nursing procedure, were analyzed; unplanned endotracheal suctioning procedures were not considered for this study.
Study Design
The dose at which endotracheally instilled lidocaine prevents endotracheal suctioning-induced ICP increase to ≥20 mmHg during endotracheal suctioning in 50% of the patients (ED50) was determined using Dixon’s up-and-down method [2, 20]. Each patient was tested once, the study continued until lidocaine failed to prevent the endotracheal suctioning-induced ICP increase to ≥20 mmHg in 20 patients (crossovers). Lidocaine was instilled at body temperature through a four French tube inserted within the endotracheal tube at 1 ml/s rate. The first patient studied received a dose of 2.0 mg/kg (2% lidocaine solution), the dose for the next patient was titrated upward (crossover) or downward with 0.5 mg/kg steps according to whether the ICP increased behind the predefined threshold of ≥20 mmHg. In order to avoid leaving patients untreated, the minimal dose was defined as 0.5 mg/kg. During the study, patients were in the supine position, with the head elevated 30° in the midline position (Fowler position). After endotracheal lidocaine instillation a 10 min interval was allowed before endotracheal suctioning, no additional muscle relaxants or systemic sedation were given. After 60 s of ventilation at 100% FiO2, endotracheal secretions were suctioned in a single pass using a closed endotracheal suctioning circuit (with a 16-F catheter, negative pressure of 100 mmHg, and total duration of 30 s), FiO2 was maintained at 100% for 30 s after completing the endotracheal suctioning maneuver then restored to the procedural (baseline) value.
The systemic and cerebral hemodynamic and ventilatory effects of endotracheal lidocaine instillation were assessed by recording HR, MAP, CPP, ICP, EtCO2, SpO2, and VMCA at 5 time points: in baseline conditions, before (T1), 5 min (T2), and 10 min after endotracheal lidocaine instillation (T3). The systemic and cerebral hemodynamic and ventilatory effects of endotracheal suctioning were assessed by measuring the same seven variables immediately before (T3), and within 1 min (at peak ICP, T4), and 5 min after endotracheal suctioning (T5).
Statistical Analysis
According to our previous experience, we determined that a sample size of 20 patients in whom lidocaine failed to prevent the endotracheal suctioning-induced cerebral hemodynamic changes after a single suctioning (using alpha and beta values of 0.05 and 0.2) would be required to detect a clinically significant difference in the ICP increase (≥30%) among the groups in whom lidocaine instillation failed or succeeded. Data were entered into a database and checked by double entry and visual inspection. Differences in distribution were tested by the Student’s t-test for paired values and by the Kruskal–Wallis test. The chi-squared test or Fisher exact test was used for comparison between categorical data. Unless otherwise indicated, results are expressed as means and SD. P values ≤0.05 were considered statistically significant.
Results
A total of 41 patients with severe head trauma admitted to the neurointensive care unit met an entry criteria and were prospectively and consecutively enrolled, no patient was excluded. Eighteen out of 41 patients enrolled in this study had been associated to the head trauma and a chest trauma, this might account for the limited increase in the Sp02 even during 100% O2 ventilation. The associated brain injuries included the following: cerebral contusions, epidural hematoma, subdural hematoma and subarachnoid hemorrhage (Table 1). Of the 41 patients enrolled, 15 patients were receiving dopamine in continuous infusion to maintain the CPP above the threshold of 70 mmHg.
In all enrolled patients endotracheal-suctioning before lidocaine instillation—pre-enrollment test- lead to a significant ICP increase, behind the threshold of 20 mmHg, associated to a reduction of CPP (mean ICP and CPP baseline versus endotracheal suctioning 16.9 ± 1.5 vs. 29.7 ± 1.5 mmHg, p < 0.05; 74 ± 6 vs. 63 ± 8 mmHg, p < 0.05).
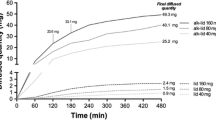
Lidocaine instilled into the endotracheal tube did not affect hemodynamic and ventilatory variables (Table 2, time points 1–3), in 12 patients lidocaine instillation lead to movements or cough but it was not associated ICP values >20 mmHg. Neither arrhythmias nor ventilation abnormalities developed after endotracheal lidocaine instillation or during the study period. Overall endotracheal suctioning led to a significant increase in the mean HR, ICP and VMCA, while MAP and CPP remained constant (Table 2, time points 3 and 4). In the subgroup of 21 patients in whom lidocaine effectively prevented endotracheal suctioning-induced cerebral hemodynamic changes (ICP remained below the threshold of 20 mmHg), both ICP and CPP remained unchanged (Table 3, time points 3 vs. 4). In the subgroup of 20 patients in whom lidocaine instillation failed to prevent the ICP increase to the threshold value of ≥20 mmHg, the ICP was significantly higher during endotracheal suctioning than before, but the CPP remained constant (17.2 vs. 25.8 mmHg; P < 0.05, and 73 vs. 70 mmHg, P = NS, by paired Student’s t-test) (Table 3, time points 3 vs. 4). Accordingly, the Dixon’s up-and-down test with the 20 crossovers yielded an ED 50 of 1.7 ± 0.3 mg/kg as lidocaine dose to instill in the endotracheal tube to prevent a endotracheal suctioning ICP increase (Fig. 1).
Discussion
In this prospective, blinded clinical trial we originally report the dose of lidocaine to be instilled into the endotracheal tube to prevent ICP increase and to blunt cerebral hemodynamic reactions related to endotracheal suctioning. We have measured it in mechanically ventilated patients after severe traumatic brain injury, whose cough reflexes were still intact.
The prevention and treatment of ICP increase in patients who have suffered severe traumatic brain injury is a corner stone of neurocritical management [20]. Since all the patients included in this prospective, blinded clinical trial had an intact cough reflexes, we used a minimum dose of 0.5 mg/kg of lidocaine for ethical reasons. The overall HR and ICP increases, and the ICP increased by more than 30% in the 20 patients in whom lidocaine failed to prevent endotracheal suctioning-induced reactions, is new evidence strongly supporting the advantages of preventing these untoward reactions in mechanically ventilated patients after severe head trauma whose cough reflexes are intact [7, 15, 16]. Owing to the relatively small ED 50 dose (1.7 ± 0.3 mg/kg) of lidocaine to be instilled into the endotracheal tube, we hypothesize that the effectiveness of endotracheal lidocaine in preventing endotracheal suctioning-induced cerebral hemodynamic changes primarily depends not on the plasma concentration but on the direct anesthetic effect on the tracheobronchial mucosa.
Study Limitations
In the clinical setting it is more useful to know the ED90 (the dose that would effectively prevents endotracheal suctioning-related ICP increase in 90% of the patients), rather than the ED50. We chose the Dixon’s up-and-down test because it allows to reliably calculate the ED50 in the clinical setting and with a relatively small sample size [21, 22]. By determining the ED50 for lidocaine our results helps to standardize the first dose of lidocaine to be instilled (we suggest starting with the ED50 dose of 1.7 mg/kg) to prevent endotracheal suctioning-induced ICP increase in mechanically ventilated patients after severe head trauma. The individual dose can be titrated by adding the SD dose of 0.3 mg/kg. (statistical inference would lead to an ED95 by adding 2SD to the ED50). An another limitation of this study is that lidocaine instillation itself sometime causes movements or cough, nevertheless this reaction in our study was not associated to ICP increase >20 mmHg. In order to minimize this reaction it is recommend to instill lidocaine at body temperature, slowly (1 ml/s), and through a fine tube advanced into the endotracheal tube within its length (avoid direct contact with the mucosa at the tip of endotracheal tube).
Although none of our patients had adverse reactions to a single instillation of lidocaine, whether this procedure could be safely and advantageously used over a period of days with the dose regimen needed to ensure adequate prevention of endotracheal suctioning-induced cerebral hemodynamic changes deserve further studies. Repeated lidocane endotracheal instillation has the potential for local and systemic toxicity, also these features should be monitored. In our experience no evidence for local or systemic toxicity arised from endotracheal lidocaine instillation.
Since lidocaine blunts cough reflexes it is possible that it has some effects also on the clearance of secretion. We have studied patients in the early phase after severe traumatic brain injury and have considered that an optimal control of the ICP and CPP is the clinical priority. We consider unlike that lidocaine might have increased the risk of pneumonia because in these patient the presence of the intratracheal tube “per se,” the use of mechanical ventilation, and sedation are far more active in reducing clearance of secretion. Furthermore, according to our previously published experience the rate of infection in our patients is relatively low and was further reduced over time by the use of various intervention that included endotratracheal lidocaine instillation [23].
In our experience lidocaine instillation into the endotracheal tube in patients with severe head trauma also reduce the need for sedatives and improve adaptation to mechanical-ventilation by reducing airway reactivity but a dedicated and quantitative evaluation of this effect deserves future studies.
Conclusion
Our study suggests that in patients with severe head trauma, who are mechanically ventilated, lidocaine instilled in the endotracheal tube effectively and safely prevents endotracheal suctioning-related systemic and cerebral hemodynamic changes and in particular the associated increase in ICP and CPP reduction. The ED50 for lidocaine that prevents endotracheal suctioning-reactions is 1.7 ± 0.3 mg/kg. We suggest an endotracheally instilled lidocaine as the first line therapy for preventing endotracheal suctioning-induced changes in systemic and cerebral hemodynamics in intubated patients, who have suffered severe traumatic brain injury.
References
Guidelines for the Management of Severe Traumatic Head Injury. Brain Trauma Foundation. American association of neurological surgeon, joint section on neurotrauma and critical care. J Neurotrauma 1996;13:641–734.
Fletcher S, Lam AM. Improving outcome for the injured brain and spinal cord. Curr Opin Anaesthesiol 2000;13(2):155–60.
Balestreri M, Czosnyka M, Hutchinson P, Steiner LA, Hiler M, Smielewski P, Pickard JD. Impact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injury. Neurocrit Care 2006;4(1):8–13.
Young PJ, Ridley SA. Ventilator-associated pneumonia. Diagnosis, pathogenesis and prevention. Anaesthesia 1999; 54:1183–97.
Carhuapoma J, Williams M. Endotracheal suctioning and cerebral ischemia in traumatic brain injury: the “phantom menace”? Crit Care Med 1999;27:2843–4.
Kerr ME, Weber BB, Sereika SM, Darby J, Marion DW, Orndoff PA. Effects of endotracheal suctioning on cerebral oxygenation in traumatic brain-injured patients. Crit Care Med 1999; 27(12):2776–81.
Gemma M, Tommasino C, Cerri M, Giannotti A, Piazzi B, Borghi T. Intracranial effects of endotracheal suctioning in the acute phase of head injury. J Neurosurg Anesthesiol 2002;14:50–4.
Miller JD, Pickard JD. Intracranial volume pressure studies in patients with head injury. Injury 1974;5:265–8.
Cremer OL, Van Dijk GW, Amelink GJ, De Smet AM, Moons KG, Kalkman CJ. Cerebral hemodynamic response to blood pressure manipulation in severely head-injured patients in the presence or absence of intracranial hypertension. Anesth Analg 2004;99:1211–7.
Kerr ME, Rudy EB, Weber BB, Stone KS, Turner BS, Orndoff PA, Sereika SM, Marion DW. Effect of short duration hyperventilation during endotracheal suctioning on intracranial pressure in severe head injured adults. Nurs Res 1997;46:195–201.
Yano M, Nishiyama H, Yokota H, Kato K, Yamamoto Y, Otsuka T. Effect of lidocaine on ICP response to endotracheal suctioning. Anesthesiology 1986;64:651–3.
White PF. IV vs LTA lidocaine: does it make any difference? Anesthesiology 1982;57:242–4.
Leone M, Albanese J, Viviand X, Garnier F, Bourgoin A, Barrau K, Martin C. The effects of remifentanil on endotracheal suctioning-induced increase in intracranial pressure in head-injured patients. Anesth Analg 2004;99:1193–8.
Menon DK. Brain ischaemia after traumatic brain injury: lessons from 15O2 positron emission tomography. Curr Opin Crit Care 2006;12(2):85–9.
Rudy EB, Turner BS, Baun M, Stone KS, Brucia J. Endotracheal suctioning in head-injured patients. Heart Lung 1991;20:667–74.
Hsiang JK, Chesnut RM, Crisp CB, Klauber MR, Blunt BA, Marshall LF. Early, routine paralysis for intracranial pressure control in severe head injury: is it necessary? Crit Care Med 1994;22:1471–6.
Tipps LB, Coplin WM, Murry KR, Rhoney DH. Safety and feasibility of continuous infusion of remifentanil in the neurosurgical intensive care unit. Neurosurgery 2000;46:596–601.
Wang D, Wu X, Li J, Xiao F, Liu X, Meng M. The effect of lidocaine on early postoperative cognitive dysfunction after coronary artery bypass surgery. Anesth Analg 2002;95:1134–41.
Jee D, Park SY. Lidocaine sprayed down the endotracheal tube attenuates the airway-circulatory reflexes by local anesthesia during emergence and extubation. Anesth Analg 2003;96:293–7.
Treggiari MM, Schutz N, Yanez ND, Romand JA. Role of intracranial pressure values and patterns in predicting outcome in traumatic brain injury: a systematic review. Neurocrit Care 2007;6(2):104–12.
Dixon WJ. Staircase bioassay: the up-and-down method. Neurosci Biobehav Rev 1991;15:47–50.
Stapelfeldt C, Lobo EP, Brown R, Talke PO. Intraoperative clonidine administration to neurosurgical patients. Anesth Analg 2005;100(1):226–32.
Orsi GB, Scorzolini L, Franchi C, Mondillo V, Rosa G, Venditti M. Hospital-acquired infection surveillance in a neurosurgical intensive care unit. J Hosp Infect 2006;64(1):23–9.
Acknowledgments
We are indebted to all the intensive care nurses staff for their active cooperation. We also thank Drs. Fabio Araimo, Floriana Baisi, Donato Colagiovanni, Nicola DeBlasiis, Carmela Imperiale, Giuseppina Magni, Filomena Musolino, Marina Pennacchia, Letizia Pennacchiotti, Francesca Rinaldi, and Paolo Tordiglione for continuous patients care.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bilotta, F., Branca, G., Lam, A. et al. Endotracheal Lidocaine in Preventing Endotracheal Suctioning-induced Changes in Cerebral Hemodynamics in Patients with Severe Head Trauma. Neurocrit Care 8, 241–246 (2008). https://doi.org/10.1007/s12028-007-9012-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-007-9012-4