Abstract
Dengue virus is a worldwide health problem, with billions of people at risk annually. Dengue virus causes a spectrum of diseases, namely dengue fever, dengue hemorrhagic fever and dengue shock syndrome with the latter two being linked to death. Understanding how dengue is able to evade the immune system and cause enhanced severity of disease is the main topics of interest in the Fernandez-Sesma laboratory at Mount Sinai School of Medicine. Using primary human immune cells, our group investigates the contribution of dengue virus-specific proteins to the evasion of innate immunity by this virus and the host factors that the virus interacts with in order to evade immune recognition and to establish infection in humans. Here, we review recent findings from our group as well as published data from other groups regarding immune modulation by dengue virus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dengue virus (DENV) is the leading cause of arthropod-borne human disease worldwide, with an estimated 50–100 million individuals infected annually and with 2.5 billion people at risk. The virus is endemic to over 100 countries, mostly in tropical and subtropical urban areas, where the primary vector Aedes aegypti is found [1]. The virus is spread to a lesser extent by Aedes albopictus mosquito (which has a broader temperature and geographical range than Aedes aegypti). Members of the family Flaviviridae, dengue viruses are comprised of four genetically related serotypes of viruses, DENV 1–4. The viral genome is approximately 10 kB in length and is composed of 10 genes, three that encode the structural proteins capsid (C), premembrane (prM) that is later cleaved during viral development to membrane (M) and envelope (E). The remaining seven genes code for the nonstructural proteins NS1, NS2A, NS2B, NS3, NS4A, NS4B and NS5. Asymptomatic in most infected individuals, dengue can present as dengue fever (DF), the more severe dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). The World Health Organization (WHO) is currently working to recategorize the spectrum of dengue disease to dengue with or without warning signs and severe dengue to facilitate easier clinical diagnosis [1]. This recategorization has not been fully adopted by the scientists performing basic research [2, 3], and as the majority of the literature uses the older classification system, we will be using DF, DHF and DSS in this review. DF is a febrile illness characterized by high fever, rash, severe joint paint, retro-orbital pain and nausea [4], comprising the vast majority of dengue infection-related disease. DHF and DSS usually present in a secondary infection and are characterized by more severe manifestations including hemorrhage, thrombocytopenia and/or shock [4] and can result in death in approximately 2.5 % of the cases according to the WHO [5].
DENV has been shown to infect many cells of immune system (mainly of myeloid origin) and related organs and is introduced to the human body upon a blood meal by an infected mosquito. The first cells to encounter the virus are believed to be Langerhans cell in the skin [6], macrophages [7] and dendritic cells (DCs) [8] and causes viremia in the patients, allowing transmission to the next host by mosquitoes. We have data showing that all PBMCs are capable of being productively infected by DENV and produce infectious particles, but show different kinetics of infection, suggesting a specific hierarchy and chronology of infection for different cells in humans (unpublished data).
DENV blocks the type I IFN system
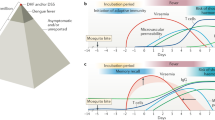
The signaling system of type I interferon (IFN) is integral to the innate immune system’s ability to create an antiviral state. Viral pathogen-associated molecular patterns (PAMPs) are recognized by intracellular molecules including Toll-like receptors (TLRs), NOD-like receptors (NLRs) and RIG-I like receptors (RLRs), leading to a downward signal transduction cascade that results in the transport of NFκB, IRF3 and ATF2/JUN to the nucleus to activate the gene of IFN beta (Fig. 1a). Type I IFN is able to signal in an autocrine and paracrine manner. IFNα/β binds to the IFNα receptor leading to the activation of the Janus kinases, Jak1 and Tyk2, through tyrosine phosphorylation. These kinases then phosphorylate STAT1 and STAT2 that dimerize to form a transcription factor that turns IFN-stimulated genes (ISGs) by binding to ISREs (IFN-stimulated response elements; Fig. 1b). ISGs are responsible for turning on many antiviral properties (as reviewed in [9]). Treatment of cells with IFN alpha, beta or gamma before infection with dengue virus protects the cells from infection, though IFN gamma’s protective abilities were variable [10]. Thus, in order to mount a successful infection, dengue virus must circumvent the type I interferon system. At MSSM, our group is focused on looking at prevention of interferon production in primary cells and the García-Sastre group, also in the department of Microbiology, investigates dengue suppression of IFN signaling.
DENV blocks type I IFN production and signaling in infected cells. a Type I IFN production. In MDDCs dsRNA, a replication product of DENV, is detected either by TLR3 present in the endosomal membrane or by RIG-I or MDA5, helicases present in the cytoplasm. The detection of dsRNA activates of signal transduction pathways that lead to the translocation of NFκB, IRF3, p38 and JNK to the nucleus where they form a transcription factor complex that activates the transcription of IFNβ. Work from the Fernandez-Sesma laboratory suggests that DENV NS2B3 blocks IFN production at the level of IRF3 phosphorylation. b Type I IFN signaling. IFNα/β binds to the receptors IFNaR1 and IFNaR2 on the surface of cells that activate the Janus kinases Jak1 and Tyk2 which in turn phosphorylate STAT1 and STAT2. Phosphorylated STAT1 and STAT2 form a transcription factor complex with IRF9, which travels to the nucleus where it binds to an ISRE to turn on the transcription of ISGs. Dengue NS5 causes the degradation of STAT2, which prevents the formation of the complex, transcription of ISGs and establishment of an antiviral state
Antagonism of type I interferon production
Upon infection with dengue virus, monocyte-derived dendritic cells (MDDCs) express many proinflammatory cytokines including IFI56K, IL-8, MIP-1 beta, RIG-I, TNF alpha, CD86 and STAT-1 [8]. The Fernandez-Sesma laboratory was the first to show that type I IFN is not induced during infection by DENV in MDDCs [8]. Interestingly, our group also showed that even plasmacytoid dendritic cells (pDCs), an exquisitely sensitive cell type to viruses that produce large quantities of IFN alpha upon stimulation, do not express IFN alpha when infected with DENV [8]. Furthermore, we showed that once infected by DENV, DCs are also unable to produce IFN upon stimulation by strong inducers of type I IFN such as infections by Newcastle disease virus, Semliki Forrest virus, and Sendai virus as well as treatment with PolyI:C (an inducer of Toll-like receptor) suggesting that DENV is a strong inhibitor of IFN. We also showed that the inhibition of type I IFN production by DENV in DCs makes them very inefficient at priming T cells to a Th1 type cell (as measured by IFN gamma ELISA) [8]. These data from our laboratory strongly suggest that early events induced in human DCs by DENV may be determinant for the cross-reactive and inefficient adaptive immunity observed in DENV infected patients. Co-expressing individual dengue proteins and protein complexes in 293-T cells that express luciferase behind an IFN alpha/beta promoter, our group also demonstrated that the DENV protease (NS2B3) is required for the inhibition of type I IFN production in infected cells [11]. We are currently investigating the targets of the NS2B3 protease, paying specific attention to molecules involved in the IFN pathway that could possibly be involved in the antagonism of IFN (Fig. 1a).
In addition to DENV actively inhibiting IFN production, our laboratory is interested in how dengue can passively evade the immune system. DENV induces intracellular membrane structures such as vesicle pockets (VP), which are bound to the ER and have a pore through to the cytoplasm [12–14]. The interior of the VPs contain products of replication including nonstructural dengue proteins, de novo synthesized RNA and double-stranded RNA. Not only do these membrane compartments concentrate viral products, they may also allow for sufficient amounts of replication to occur before any PAMPs are detected by the host cells PRRs. Other flaviviruses also utilize this process for immune evasion [12, 14]. Our laboratory is currently investigating how much of the inhibition of the IFN production is through active inhibition by the NS2B3 complex or through passive inhibition by hiding replication products in membrane vesicles.
Dengue inhibits type I interferon signaling
In addition to antagonizing the production of type I IFN, DENV also inhibits its signaling. A report by Ho et al. [15] demonstrated that DENV can block signaling of IFNα/β, but it cannot block IFNγ signaling through STAT2 down-regulation. Treatment with type I IFN prior to infection with DENV prevents infection with the virus [10, 16], suggesting that IFNs are very efficient at controlling this pathogen and that the virus is likely to dedicate some of its proteins to antagonize this important innate immune system. Extensive work has been done by the García-Sastre group at Mount Sinai School of Medicine to elucidate how DENV is able to thwart the host IFN signaling. They have identified NS2A, NS4A, NS4B and NS5 as able to block IFN signaling (Fig. 1b); expression of these proteins in cells that were then infected with IFN-sensitive viruses rescued replication of those viruses, showing that these nonstructural proteins were responsible for preventing IFN signaling [17]. Interestingly, expression of NS4B alone resulted in down-regulation in the expression of interferon-stimulated genes (ISG), suggesting that this protein by itself is a potent IFN antagonist [17, 18]. They went on to show that NS4B is able to block IFN signaling by down-regulating STAT1 expression [18].
Additionally, the Garcia-Sastre group investigated the IFN antagonistic properties of some of the other DENV nonstructural proteins identified in their earlier screenings, such as the NS5. It was shown by another group that IFN alpha signaling is decreased in DENV infected cells through down-regulation of STAT2 [19], indicating that another protein, different from NS4B, may act on STAT2. The Garcia-Sastre group showed that binding of NS5 to STAT2 is required for the observed decreased levels of STAT2 in an ubiquitin and proteasome-dependent process (Fig. 1b) [20]. Interestingly, they showed in a subsequent study that dengue NS5 is unable to degrade mouse STAT2 and can only degrade human STAT2, strongly suggesting that STAT2 could be a restriction factor for DENV infection in mice [21]. This may explain why establishing a dengue mouse model has been so difficult for the DENV research community. If NS5 is unable to cause the degradation of STAT2, then IFN signaling is able to take place, creating an antiviral state and preventing the replication of dengue virus. Currently, the majority of dengue mouse models, such as the AG129, used are immunocompromised, many with the type I IFN system knocked out [22]. Using transgenic technology, a better, immunocompetent mouse model might be created with by replacing mouse STAT2 with human STAT2 [21].
Severity of dengue disease
Our laboratory is also very interested in finding out what causes severe dengue disease manifestation in humans. DENV is unique in that the virus can induce a more severe disease upon subsequent infections, implying that the patient’s own immune response to the first infection may determine the severity of subsequent secondary infections by other serotypes of DENV. While many infections with DENV are asymptomatic [23, 24], patients can also develop DF, DHF or DSS. DF is characterized by arthralgia, rash, high fever, nausea, retro-orbital pain and headache [1, 4]. Severe DENV usually manifests upon a secondary infection of the virus, though there are exceptions. Ten percent of DHF infections are primary infections, and almost all of these cases are infants born to mothers who previously had dengue [25]. DHF is characterized as an extremely severe febrile illness with thrombocytopenia, petechiae and bruising, and dengue shock syndrome is even more severe with shock manifestations due to vasculature leakage [1, 4, 26]. Patients with DHF also have a 10–100 times higher viremia than patients with DF [27–29] as well as other markers of enhanced disease.
There are several different theories to explain how severe cases of DENV can arise including antibody-dependent enhancement and T-cell-mediated immunity and these will be discussed in this section.
Antibody-dependent enhancement
The phenomenon of antibody-dependent enhancement was first described by Sabin on work performed on the virus during World War II [30] and extensively studied by Halstead in the 1960 and 1970s in a group of small children in Bangkok [31]. Currently, many studies are being performed in vitro to fully elucidate this occurrence. During a primary infection, antibodies are generated against that particular serotype. After a brief period of time when these antibodies are able to neutralize the viruses, these antibodies remain cross-reactive for other serotypes and facilitate entry into the cell. In vitro work has demonstrated that heterotypic antibodies are able to neutralize at high titers, but as concentrations decrease, the neutralization threshold has been lost and entry is enhanced [32–34]. Cross-reactive antibodies are able to bind to the virus and also bind to Fcγ I and II receptors [32, 35], and Fc receptor-mediated endocytosis is faster and more efficient than normal entry into the host cell via the yet undescribed viral entry receptor. Faster entry into the cell allows for more rapid replication and higher production of infectious particles. Several cell types that are primary targets for DENV support enhanced entry including monocytes, macrophages and mature dendritic cells [36]. Other cells such as immature dendritic cells do not have enhanced entry in the presence of antibodies but demonstrate high infectivity by DENV without antibodies [36]. Many of the antibodies generated against DENV antigens are against the E protein, the most outwardly exposed protein in the virion, and there is mounting evidence that the antibodies involved ADE are mostly against the prM protein of immature virions that have failed to mature as they exit the host cell [37]. In vitro studies have demonstrated that anti-prM antibodies facilitate binding and entry of immature virions, and these virions are able to replicate [38]. To complicate matters, it has been proposed that neutralizing antibodies, when titers decrease, could become enhancing [39, 40]. This ADE phenomenon makes it very challenging to develop efficient vaccines against DENV, since the generation of the wrong type of antibodies in the vaccines may make them more susceptible to sever dengue disease. Several ongoing trials for vaccine development are trying to address this issue by using different strategies of vaccination [41]. The Fernandez-Sesma laboratory is currently exploring the influence of human antibodies to different DENV in the ability of other serotypes of the virus to infect primary human cells (such as monocytes, MDDCs and MDDM) and to antagonize the IFN response in those cells.
T-cell-mediated immunity
Another immune factor contributing to disease severity is the T-cell response. There is some evidence in dengue patients indicating that T cells react quickly and most likely enhance severity of disease; DHF patients have high levels of soluble IL-2R, soluble CD8 and soluble CD4 [29, 42, 43] and as well as higher levels of activated T cells and some cytokines compared with patients with other febrile illnesses and patients with dengue fever in the case of elevated cytokine levels [44, 45]. After an infection with DENV of a particular serotype, mice and human patients have been reported to produce cross-reactive CD4+ and CD8+ T cells against the other serotypes [46–48]. Cross-reactive murine T cells were shown to be against nonstructural DENV proteins, while serotype-specific T cells were against structural DENV proteins [48–51], suggesting a role for cross-reactive T-cell responses in severity of dengue disease. T-cell epitopes have been identified in both mice and humans against almost all of the DENV proteins; however, the majority of these epitopes are against either the E protein and more abundantly against NS1, NS2A and NS3 [48–50, 52, 53]. The NS3 epitopes have been identified to be important target of CD8+ T cells in DHF patients [52]. More studies need to be performed in order to identify what epitopes are important for protective responses in DENV infections, but limitations due to the lack of an immunocompetent small animal model have made this kind of research very difficult.
Intrinsic viral properties
There is also mounting evidence suggesting that distinct viral properties can influence the severity of dengue disease; however, it can be difficult to fully ascertain specific strain properties when most areas that have endemic DENV have multiple co-circulating serotypes. Studies by Rico-Hesse et al. have demonstrated that in the US, the circulating DENV-2 American genotype, which had no link to DHF and DSS, was replaced with a Southeast Asian (SEA), which was associated with DHF [54–56]. Recent work in Cambodia demonstrates that clinical isolates from children with DSS were phenotypically distinct and replicated less efficiently in mammalian cell culture than isolates from patients presenting with DF or DHF from the same outbreak [57]. In Sri Lanka, DHF was extremely uncommon before 1989; however, in 1989, DHF emerged. At the time of the onset of DHF, there had been neither an increase in transmission of the virus nor a change in the circulating serotypes [58]. Phylogenetic analysis of clinical isolates revealed a clade replacement in the circulating DENV-3 viruses from a subtype group A virus to a group B virus, which accounted for change in disease severity [58, 59]. Our laboratory is currently working with viruses from Sri Lanka from patients with DF (before 1989) or DHF (after 1989) in collaboration with the de Silva laboratory at the University of North Carolina, Chapel Hill. We are investigating if viruses associated with DHF will induce stronger immune responses in a primary infection conditions with monocytes and MDDCs that could suggest that intrinsic viral properties can induce severe disease. Our preliminary data show that in a primary infection of MDDCs, the DHF-associated viruses induce higher levels of cytokines and chemokines (unpublished data, Fig. 2).
Proposed model of how intrinsic DENV properties may induce different immune responses in MDDCs, leading to more severe disease manifestation. a MDDCs infected with DF-associated DENV do not produce type I IFN but do express cytokines and chemokines. b MDDCs infected with a DHF-associated DENV produce type I IFN as well as increased cytokines and chemokines
Host genetic determinants
Additionally, there are host factors that also play a role in disease severity. There are several genetic factors that have been correlated with more severe disease including HLA alleles [60–63], polymorphisms in TNF alpha [64], LT alpha [64] and the promoter of CD209 [65]. These facts may explain the differences in distribution of DHF cases in different areas of the world where all serotypes of DENV co-circulate, like the low incidence of sever dengue disease reported in Africa as compared to Asia or Central and South America [66].
Conclusions
DENV is an important pathogen to study based on the wide distribution of the disease worldwide and in addition to the spectrum of disease severity it causes. Dengue disease is multifactorial, and it has been difficult to study due to the lack of tools and immune competent small animal models. Currently, several groups, including ours, are focusing on primary human cells to try to identify the specific viral and host factors that contribute to the severity of dengue disease. Identifying such factors will facilitate the development of efficient antivirals and vaccines for DENV.
Considerations for enhanced severity of disease have been vital in the creation of a tetravalent DENV virus vaccine. If the vaccine does not provide complete, lifelong immunity to all four serotypes of the virus, the vaccine could then potentially enhance infection of the waning serotype. Thus, ongoing research is being performed by several groups to create a strong vaccine and several candidates are in different phases of clinical trials.
References
Dengue, guidelines for diagnosis, treatment, prevention and control. Geneva: World Health Organization; 2009.
Narvaez F, Gutierrez G, Perez MA, Elizondo D, Nunez A, Balmaseda A, et al. Evaluation of the traditional and revised WHO classifications of dengue disease severity. PLoS Negl Trop Dis. 2011;5(11):e1397. doi:10.1371/journal.pntd.0001397.
Srikiatkhachorn A, Rothman AL, Gibbons RV, Sittisombut N, Malasit P, Ennis FA, et al. Dengue—how best to classify it. Clin Infect Dis. 2011;53(6):563–7. doi:10.1093/cid/cir451.
Dengue haemorrhagic fever: diagnosis, treatment, prevention and control. Geneva: World Health Organization; 1997.
Dengue and dengue haemorrhagic fever. In: WHO Media Center. 2009. http://www.who.int/mediacentre/factsheets/fs117/en/. Accessed 9 Jan 2012.
Limon-Flores AY, Perez-Tapia M, Estrada-Garcia I, Vaughan G, Escobar-Gutierrez A, Calderon-Amador J, et al. Dengue virus inoculation to human skin explants: an effective approach to assess in situ the early infection and the effects on cutaneous dendritic cells. Int J Exp Pathol. 2005;86(5):323–34. doi:10.1111/j.0959-9673.2005.00445.x.
Jessie K, Fong MY, Devi S, Lam SK, Wong KT. Localization of dengue virus in naturally infected human tissues, by immunohistochemistry and in situ hybridization. J Infect Dis. 2004;189(8):1411–8. doi:10.1086/383043.
Rodriguez-Madoz JR, Bernal-Rubio D, Kaminski D, Boyd K, Fernandez-Sesma A. Dengue virus inhibits the production of type I interferon in primary human dendritic cells. J Virol. 2010;84(9):4845–50. doi:10.1128/JVI.02514-09.
Borden EC, Sen GC, Uze G, Silverman RH, Ransohoff RM, Foster GR, et al. Interferons at age 50: past, current and future impact on biomedicine. Nat Rev Drug Discov. 2007;6(12):975–90. doi:10.1038/nrd2422.
Diamond MS, Roberts TG, Edgil D, Lu B, Ernst J, Harris E. Modulation of Dengue virus infection in human cells by alpha, beta, and gamma interferons. J Virol. 2000;74(11):4957–66.
Rodriguez-Madoz JR, Belicha-Villanueva A, Bernal-Rubio D, Ashour J, Ayllon J, Fernandez-Sesma A. Inhibition of the type I interferon response in human dendritic cells by dengue virus infection requires a catalytically active NS2B3 complex. J Virol. 2010;84(19):9760–74. doi:10.1128/JVI.01051-10.
Fredericksen BL, Gale M Jr. West Nile virus evades activation of interferon regulatory factor 3 through RIG-I-dependent and -independent pathways without antagonizing host defense signaling. J Virol. 2006;80(6):2913–23. doi:10.1128/JVI.80.6.2913-2923.2006.
Mackenzie JM, Jones MK, Young PR. Immunolocalization of the dengue virus nonstructural glycoprotein NS1 suggests a role in viral RNA replication. Virology. 1996;220(1):232–40. doi:10.1006/viro.1996.0307.
Welsch C, Zeuzem S. RNA-binding activity of hepatitis C virus NS4B: a novel target for small molecule inhibitors. Gastroenterology. 2009;137(6):2170–2. doi:10.1053/j.gastro.2009.10.024.
Ho LJ, Hung LF, Weng CY, Wu WL, Chou P, Lin YL, et al. Dengue virus type 2 antagonizes IFN-alpha but not IFN-gamma antiviral effect via down-regulating Tyk2-STAT signaling in the human dendritic cell. J Immunol. 2005;174(12):8163–72.
Diamond MS, Harris E. Interferon inhibits dengue virus infection by preventing translation of viral RNA through a PKR-independent mechanism. Virology. 2001;289(2):297–311. doi:10.1006/viro.2001.1114.
Munoz-Jordan JL, Sanchez-Burgos GG, Laurent-Rolle M, Garcia-Sastre A. Inhibition of interferon signaling by dengue virus. Proc Natl Acad Sci USA. 2003;100(24):14333–8. doi:10.1073/pnas.2335168100.
Munoz-Jordan JL, Laurent-Rolle M, Ashour J, Martinez-Sobrido L, Ashok M, Lipkin WI, et al. Inhibition of alpha/beta interferon signaling by the NS4B protein of flaviviruses. J Virol. 2005;79(13):8004–13. doi:10.1128/JVI.79.13.8004-8013.2005.
Jones M, Davidson A, Hibbert L, Gruenwald P, Schlaak J, Ball S, et al. Dengue virus inhibits alpha interferon signaling by reducing STAT2 expression. J Virol. 2005;79(9):5414–20. doi:10.1128/JVI.79.9.5414-5420.2005.
Ashour J, Laurent-Rolle M, Shi PY, Garcia-Sastre A. NS5 of dengue virus mediates STAT2 binding and degradation. J Virol. 2009;83(11):5408–18. doi:10.1128/JVI.02188-08.
Ashour J, Morrison J, Laurent-Rolle M, Belicha-Villanueva A, Plumlee CR, Bernal-Rubio D, et al. Mouse STAT2 restricts early dengue virus replication. Cell Host Microbe. 2010;8(5):410–21. doi:10.1016/j.chom.2010.10.007.
Johnson AJ, Roehrig JT. New mouse model for dengue virus vaccine testing. J Virol. 1999;73(1):783–6.
Endy TP, Yoon IK, Mammen MP. Prospective cohort studies of dengue viral transmission and severity of disease. Curr Top Microbiol Immunol. 2010;338:1–13. doi:10.1007/978-3-642-02215-9_1.
Balmaseda A, Standish K, Mercado JC, Matute JC, Tellez Y, Saborio S, et al. Trends in patterns of dengue transmission over 4 years in a pediatric cohort study in Nicaragua. J Infect Dis. 2010;201(1):5–14. doi:10.1086/648592.
Thein S, Aung MM, Shwe TN, Aye M, Zaw A, Aye K, et al. Risk factors in dengue shock syndrome. Am J Trop Med Hyg. 1997;56(5):566–72.
Gubler DJ. Dengue and dengue hemorrhagic fever. Clin Microbiol Rev. 1998;11(3):480–96.
Murgue B, Roche C, Chungue E, Deparis X. Prospective study of the duration and magnitude of viraemia in children hospitalised during the 1996–1997 dengue-2 outbreak in French Polynesia. J Med Virol. 2000;60(4):432–8. doi:10.1002/(SICI)1096-9071(200004)60:4<432:AID-JMV11>3.0.CO;2-7.
Vaughn DW, Green S, Kalayanarooj S, Innis BL, Nimmannitya S, Suntayakorn S, et al. Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity. J Infect Dis. 2000;181(1):2–9. doi:10.1086/315215.
Libraty DH, Endy TP, Houng HS, Green S, Kalayanarooj S, Suntayakorn S, et al. Differing influences of virus burden and immune activation on disease severity in secondary dengue-3 virus infections. J Infect Dis. 2002;185(9):1213–21. doi:10.1086/340365.
Sabin AB. Research on dengue during World War II. Am J Trop Med Hyg. 1952;1(1):30–50.
Russell PK, Udomsakdi S, Halstead SB. Antibody response in dengue and dengue hemorrhagic fever. Jpn J Med Sci Biol. 1967;20(Suppl):103–8.
Boonnak K, Slike BM, Burgess TH, Mason RM, Wu SJ, Sun P, et al. Role of dendritic cells in antibody-dependent enhancement of dengue virus infection. J Virol. 2008;82(8):3939–51. doi:10.1128/JVI.02484-07.
Goncalvez AP, Engle RE, St Claire M, Purcell RH, Lai CJ. Monoclonal antibody-mediated enhancement of dengue virus infection in vitro and in vivo and strategies for prevention. Proc Natl Acad Sci USA. 2007;104(22):9422–7. doi:10.1073/pnas.0703498104.
Yamanaka A, Kosugi S, Konishi E. Infection-enhancing and -neutralizing activities of mouse monoclonal antibodies against dengue type 2 and 4 viruses are controlled by complement levels. J Virol. 2008;82(2):927–37. doi:10.1128/JVI.00992-07.
Littaua R, Kurane I, Ennis FA. Human IgG Fc receptor II mediates antibody-dependent enhancement of dengue virus infection. J Immunol. 1990;144(8):3183–6.
Boonnak K, Dambach KM, Donofrio GC, Tassaneetrithep B, Marovich MA. Cell type specificity and host genetic polymorphisms influence antibody-dependent enhancement of dengue virus infection. J Virol. 2011;85(4):1671–83. doi:10.1128/JVI.00220-10.
Dejnirattisai W, Jumnainsong A, Onsirisakul N, Fitton P, Vasanawathana S, Limpitikul W, et al. Cross-reacting antibodies enhance dengue virus infection in humans. Science. 2010;328(5979):745–8. doi:10.1126/science.1185181.
Rodenhuis-Zybert IA, van der Schaar HM, da Silva Voorham JM, van der Ende-Metselaar H, van der Lei HY, Wilschut J, et al. Immature dengue virus: a veiled pathogen? PLoS Pathog. 2010;6(1):e1000718. doi:10.1371/journal.ppat.1000718.
Pierson TC, Xu Q, Nelson S, Oliphant T, Nybakken GE, Fremont DH, et al. The stoichiometry of antibody-mediated neutralization and enhancement of West Nile virus infection. Cell Host Microbe. 2007;1(2):135–45. doi:10.1016/j.chom.2007.03.002.
Rothman AL. Immunity to dengue virus: a tale of original antigenic sin and tropical cytokine storms. Nat Rev Immunol. 2011;11(8):532–43. doi:10.1038/nri3014.
Murphy BR, Whitehead SS. Immune response to dengue virus and prospects for a vaccine. Annu Rev Immunol. 2011;29:587–619. doi:10.1146/annurev-immunol-031210-101315.
Kurane I, Innis BL, Nimmannitya S, Nisalak A, Meager A, Janus J, et al. Activation of T lymphocytes in dengue virus infections. High levels of soluble interleukin 2 receptor, soluble CD4, soluble CD8, interleukin 2, and interferon-gamma in sera of children with dengue. J Clin Invest. 1991;88(5):1473–80. doi:10.1172/JCI115457.
Green S, Vaughn DW, Kalayanarooj S, Nimmannitya S, Suntayakorn S, Nisalak A, et al. Early immune activation in acute dengue illness is related to development of plasma leakage and disease severity. J Infect Dis. 1999;179(4):755–62. doi:10.1086/314680.
Green S, Vaughn DW, Kalayanarooj S, Nimmannitya S, Suntayakorn S, Nisalak A, et al. Elevated plasma interleukin-10 levels in acute dengue correlate with disease severity. J Med Virol. 1999;59(3):329–34. doi:10.1002/(SICI)1096-9071(199911)59:3<329:AID-JMV12>3.0.CO;2-G.
Chau TN, Quyen NT, Thuy TT, Tuan NM, Hoang DM, Dung NT, et al. Dengue in Vietnamese infants–results of infection-enhancement assays correlate with age-related disease epidemiology, and cellular immune responses correlate with disease severity. J Infect Dis. 2008;198(4):516–24. doi:10.1086/590117.
Rothman AL, Kurane I, Zhang YM, Lai CJ, Ennis FA. Dengue virus-specific murine T-lymphocyte proliferation: serotype specificity and response to recombinant viral proteins. J Virol. 1989;63(6):2486–91.
Rothman AL, Kurane I, Lai CJ, Bray M, Falgout B, Men R, et al. Dengue virus protein recognition by virus-specific murine CD8+ cytotoxic T lymphocytes. J Virol. 1993;67(2):801–6.
Rothman AL, Kurane I, Ennis FA. Multiple specificities in the murine CD4+ and CD8+ T-cell response to dengue virus. J Virol. 1996;70(10):6540–6.
Mathew A, Kurane I, Rothman AL, Zeng LL, Brinton MA, Ennis FA. Dominant recognition by human CD8+ cytotoxic T lymphocytes of dengue virus nonstructural proteins NS3 and NS1.2a. J Clin Invest. 1996;98(7):1684–91. doi:10.1172/JCI118964.
Green S, Kurane I, Pincus S, Paoletti E, Ennis FA. Recognition of dengue virus NS1-NS2a proteins by human CD4+ cytotoxic T lymphocyte clones. Virology. 1997;234(2):383–6. doi:10.1006/viro.1997.8648.
Mathew A, Kurane I, Green S, Stephens HA, Vaughn DW, Kalayanarooj S, et al. Predominance of HLA-restricted cytotoxic T-lymphocyte responses to serotype-cross-reactive epitopes on nonstructural proteins following natural secondary dengue virus infection. J Virol. 1998;72(5):3999–4004.
Zivna I, Green S, Vaughn DW, Kalayanarooj S, Stephens HA, Chandanayingyong D, et al. T cell responses to an HLA-B*07-restricted epitope on the dengue NS3 protein correlate with disease severity. J Immunol. 2002;168(11):5959–65.
Spaulding AC, Kurane I, Ennis FA, Rothman AL. Analysis of murine CD8(+) T-cell clones specific for the Dengue virus NS3 protein: flavivirus cross-reactivity and influence of infecting serotype. J Virol. 1999;73(1):398–403.
Mota J, Rico-Hesse R. Humanized mice show clinical signs of dengue fever according to infecting virus genotype. J Virol. 2009;83(17):8638–45. doi:10.1128/JVI.00581-09.
Anderson JR, Rico-Hesse R. Aedes aegypti vectorial capacity is determined by the infecting genotype of dengue virus. Am J Trop Med Hyg. 2006;75(5):886–92.
Rico-Hesse R, Harrison LM, Salas RA, Tovar D, Nisalak A, Ramos C, et al. Origins of dengue type 2 viruses associated with increased pathogenicity in the Americas. Virology. 1997;230(2):244–51.
Tuiskunen A, Monteil V, Plumet S, Boubis L, Wahlstrom M, Duong V, et al. Phenotypic and genotypic characterization of dengue virus isolates differentiates dengue fever and dengue hemorrhagic fever from dengue shock syndrome. Arch Virol. 2011;156(11):2023–32. doi:10.1007/s00705-011-1100-2.
Messer WB, Vitarana UT, Sivananthan K, Elvtigala J, Preethimala LD, Ramesh R, et al. Epidemiology of dengue in Sri Lanka before and after the emergence of epidemic dengue hemorrhagic fever. Am J Trop Med Hyg. 2002;66(6):765–73.
Messer WB, Gubler DJ, Harris E, Sivananthan K, de Silva AM. Emergence and global spread of a dengue serotype 3, subtype III virus. Emerg Infect Dis. 2003;9(7):800–9.
Stephens HA, Klaythong R, Sirikong M, Vaughn DW, Green S, Kalayanarooj S, et al. HLA-A and -B allele associations with secondary dengue virus infections correlate with disease severity and the infecting viral serotype in ethnic Thais. Tissue Antigens. 2002;60(4):309–18.
Chiewsilp P, Scott RM, Bhamarapravati N. Histocompatibility antigens and dengue hemorrhagic fever. Am J Trop Med Hyg. 1981;30(5):1100–5.
Loke H, Bethell DB, Phuong CX, Dung M, Schneider J, White NJ, et al. Strong HLA class I—restricted T cell responses in dengue hemorrhagic fever: a double-edged sword? J Infect Dis. 2001;184(11):1369–73. doi:10.1086/324320.
Malavige GN, Rostron T, Rohanachandra LT, Jayaratne SD, Fernando N, De Silva AD, et al. HLA class I and class II associations in dengue viral infections in a Sri Lankan population. PLoS ONE. 2011;6(6):e20581. doi:10.1371/journal.pone.0020581.
Vejbaesya S, Luangtrakool P, Luangtrakool K, Kalayanarooj S, Vaughn DW, Endy TP, et al. TNF and LTA gene, allele, and extended HLA haplotype associations with severe dengue virus infection in ethnic Thais. J Infect Dis. 2009;199(10):1442–8. doi:10.1086/597422.
Wang L, Chen RF, Liu JW, Lee IK, Lee CP, Kuo HC, et al. DC-SIGN (CD209) Promoter -336 A/G polymorphism is associated with dengue hemorrhagic fever and correlated to DC-SIGN expression and immune augmentation. PLoS Negl Trop Dis. 2011;5(1):e934. doi:10.1371/journal.pntd.0000934.
de la CSB, Kouri G, Guzman MG. Race: a risk factor for dengue hemorrhagic fever. Arch Virol. 2007;152(3):533–42. doi:10.1007/s00705-006-0869-x.
Acknowledgments
The work from the Fernandez-Sesma laboratory cited and discussed in this review is funded by the National Institutes of Health/National Institute of Allergy and Infectious Diseases grant 1R01AI073450 to AF-S.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pagni, S., Fernandez-Sesma, A. Evasion of the human innate immune system by dengue virus. Immunol Res 54, 152–159 (2012). https://doi.org/10.1007/s12026-012-8334-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-012-8334-2