Abstract
Medical student education continues to evolve, with an increasing emphasis on evidence-based decision making in clinical settings. Many schools are introducing scholarly programs to their curriculum in order to foster the development of critical thinking and analytic skills, encourage self-directed learning, and develop more individualized learning experiences. In addition, participation in rigorous scholarly projects teaches students that clinical care and research should inform each other, with the goal of providing more benefit to patients and society. Physician-scientists, and physicians who have a better appreciation of science, have the potential to be leaders in the field who will deliver outstanding clinical care, contribute new knowledge, and educate their patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Academic health centers have embraced the missions of advancing clinical care and research in order to improve the health of our patients and our communities. Over the past half century, advances in the biological sciences have become more translational, with greater application to patient care than ever before. At the same time, clinical care has become increasingly evidence based, providing patients with data-driven care. This growing alignment between the lab and the clinic means that our best investigators must have, or develop, a clinical perspective when thinking about their science. It also means that our best clinicians must have, or develop, a scientific approach to the care they deliver. In order to best prepare medical students to integrate new scientific and medical knowledge throughout their careers, medical schools must develop a two-pronged approach: (1) curricula have to continuously evolve to incorporate new knowledge and scientific advances and (2) students must learn analytical skills and the fundamental principles of critical thinking.
Physician investigators in traditional Medical Scientist Training Programs (MSTP) are in a unique position to lead this effort. However, while MD/PhD programs have a long and successful history of producing physician investigators, the majority of physicians in training do not participate in these programs [1]. Embedding research experiences and training programs into the medical school curriculum for all students provides a mechanism to seamlessly integrate research and clinical medicine. Research training programs enable medical students to conduct carefully mentored projects that not only enhance critical thinking skills, but also inspire creativity and promote intellectual independence. They help students appreciate the unique opportunity that clinical training affords them within team science. The Carnegie Foundation’s recent recommendations for training physicians include individualized learning, integration of knowledge, identity formation, and the pursuit of excellence [2]. Opportunities for independent scholarship can help students achieve these goals. Conducting research can also sharpen their skills for critical analysis of the literature, important in the development of physicians who are able to apply the principles of evidence-based medicine to their practice.
How to incorporate research into undergraduate medical education, how to determine appropriate goals and objectives, how to define their success, and how patients and society in general might benefit from physicians trained with this background, continues to be a topic of much discussion [3–5]. In this article, we review our experience with the creation and integration of research training programs into the medical school curriculum at a large academic institution.
Medical student scholarship at Mount Sinai
The Mount Sinai School of Medicine (MSSM) has a long history of basic, clinical, and translational research. MSSM currently ranks 18 of the Nation’s 134 medical schools in NIH funding. In fiscal year 2010, the federal government awarded 595 grants and contracts to 337 of MSSM’s investigators. Mount Sinai has held a Clinical and Translational Science Award (CTSA) since 2009.
The Mount Sinai Hospital provides advanced tertiary and quaternary care to a broad cross-section of New York City’s population, including patients from the underserved and ethnically diverse communities of East and Central Harlem. The school’s mission is “To produce physicians and scientists who are prepared to enter society as informed advocates and activists, able to advance clinical care and science, and capable of promoting change.” Consistent with this mission, the medical school curriculum at MSSM is directed at educating physicians who have the training necessary to be leaders in both patient care and research.
Students are informed about the opportunities for research from the very beginning of their medical education. The Medical Student Research Office provides help in identifying research opportunities and support in mentor selection to all students who are interested in an independent scholarly project. Every attempt is made to integrate scholarly and research programs with required courses and clinical experiences, allowing students to appreciate the role that clinical and translational research play in patient care, as well as to encourage self-directed learning and critical thinking. The longitudinal scholarly curriculum consists of strongly mentored research training programs designed for students at different levels of their education. Research programs begin during the first year, continue throughout medical school, and include the possibility of a 5th year for research, providing diverse opportunities for students and offering increasing levels of independence as they advance in their education.
Mentorship is perhaps the most important component of these programs. Faculty members have many reasons to serve as research mentors for medical students. The student–faculty relationship can be extremely rewarding, working with a student helps faculty to improve their mentoring skills and enhance their mentoring portfolio, and mentorship offers an opportunity to identify and nurture talent. Mentors also serve as critically important career role models. It has been reported that students with a research experience display an increased interest in an academic career in general and that the experience may influence the clinical specialty chosen by the trainee [5]. Our programs also include opportunities for peer mentorship.
Overview and design of research training programs
Patient-oriented research, training, and leadership (PORTAL)
PORTAL is an honors track developed to provide students with a multidisciplinary approach to clinical investigation. The program, to which students apply at the same time they apply to the MD program, integrates learning about clinical medicine and developing the skills required to conduct clinical research from the first year of medical school. Participants follow the rigorous Master of Science in Clinical Research (MSCR) curriculum, along with the medical curriculum, and conduct independent thesis research, earning both the MD and MSCR degrees after 5 years. Students learn clinical research methodology, including clinical trial and experimental design, data management, and data analysis, as well as how to write a grant and how to navigate regulatory requirements. For their thesis research, completed largely during a Scholarly Year, students identify a mentor and a clinical or translational research project. A thesis committee ensures that they make adequate progress in their research. Monthly group sessions during preclinical years 1 and 2 help to maintain contact among PORTAL students, expose them to cutting-edge questions in diverse areas, and provide a perspective on future career options. Most of the meetings are devoted to a clinical journal club led by outstanding clinical and translational investigators. For the student, this is a multiyear commitment to excellence that is made possible by strong faculty support, as well as dedicated institutional resources.
Fellows as mentors experience (FAME)
As early as the first year of medical school, students are invited to participate in the FAME program. FAME is designed to provide an interactive experience through which students learn firsthand how clinical/translational research and clinical medicine intersect. The program is unique because it offers these beginning students the opportunity to participate actively in an original research project during the preclinical school year. Also unique is that mentors are more senior students doing a mentored, full year of research, referred to as a Scholarly Year. The senior student’s own faculty mentor must agree to the arrangement and, in most cases, oversees the progress from a distance.
Interested students submit a brief application that describes their current career goals and what they hope to gain from participation in the program. FAME begins in January and ends in May. The student mentor and mentee are responsible for determining the amount of time the mentee spends on the project and the mentee’s responsibilities. Both benefit from the experience. The student mentors have the opportunity to improve their teaching skills while getting assistance with their projects. The mentees have the chance to work with someone closer to their level than a faculty mentor, to better understand the research process and to experience what it is like to do a year of full-time clinical/translational research. Outcomes from our first 3 cohorts of FAME participants, which included 15 students, indicate high satisfaction with the program (Table 1). The data also suggest that participation increases both students’ understanding of the research process and their interest in participating in research in later years.
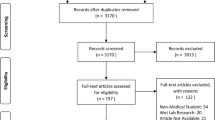
Summer research scholars program
Most of our medical students pursue a scholarly research project during the summer following their first year, and participation continues to grow (Fig. 1). Projects include those in basic, clinical, and translational research; community-based participatory research; global health; epidemiology; public policy; medical education; and medical humanities. Students receive help in finding a mentor and are supported by stipends from various sources. Students are encouraged to begin organizing their projects during the spring semester of the first year, especially if the project requires regulatory approval, in order to make more efficient use of the summer period. Workshops sponsored by the Medical Student Research Office during the academic year are offered to help students learn how to write an abstract, prepare a poster, and give an oral talk. Support from the Office of Clinical Research, part of the CTSA-supported Mount Sinai Institutes for Translational Sciences, is provided to those students whose projects need to be submitted to the institutional review board (IRB).
The following summer programs have been developed in order to offer students a wide range of scholarly projects:
-
The Patient Research in Science and Medicine (PRISM) program supports clinical and translational research studies. These students are required to take the Summer Course in Clinical Research, offered by the Clinical Research Education Program, and they earn a certificate of completion.
-
The Patricia S. Levinson Program in Community Based Research is directed at supporting interdisciplinary projects that involve physicians and other health care providers, such as nurses or social workers.
-
The Global Health Training Center supports mentored projects that are done in resource-poor settings in the USA and abroad.
-
The Center for Multicultural and Community Affairs (CMCA) funds projects that focus on health care disparities and cultural competence.
-
The Medical Student Training in Aging Research (MSTAR) focuses on multidisciplinary projects in Geriatrics and Palliative Care.
All students present the results of their work at the annual Medical Student Research Day in November as a talk or a poster. Research Day offers many students their first opportunity to present original research. No classes are scheduled on Research Day, and attendance is mandatory for first- and second-year students.
Individual scholarly project and independent research experience (INSPIRE)
INSPIRE, currently a 12-week program during the fall semester of 4th year, was developed to enable advanced students to express their creativity and develop their intellectual independence by working on an original project without adding additional time to medical school. The project can be a new, focused project or a continuation of a project begun earlier. A curriculum provides students with feedback on their progress and introduces them to faculty members who are clinician scholars. At the end of the program, students present their findings at INSPIRE Research Day. Because INSPIRE students are nearing completion of their medical education and applying for residencies, INSPIRE often provides an opportunity for them to explore cutting-edge research in their chosen field. As part of the program, they have the opportunity to attend departmental research and clinical conferences, from which they benefit greatly at this stage in their education.
The Scholarly Year
The Scholarly Year is a chance for students to pursue full-time scholarly projects or a second advanced degree. Scholarly projects are carried out within programs sponsored by national foundations such as the Howard Hughes Medical Institute, Sarnoff Foundation, or Doris Duke Charitable Foundation; at the CDC, as part of the CDC Experience; at the NIH, as part of the Medical Research Scholars Program; at a global health site, as a Fulbright-Fogarty Fellowships in Public Health Scholar; or overseen by an individual faculty mentor at Mount Sinai or another academic institution. Mount Sinai has been the site of a Doris Duke Clinical Research Training Program since 2002. The Doris Duke program, with its strongly mentored research projects and didactic curriculum, has served as a model for the development of our other scholarly programs. The number of students electing a Scholarly Year has been steadily rising, from 5 in 1997 to 38 in 2011–2012 (Fig. 2).
Students who work with an individual mentor, whether at MSSM or another institution, are supported academically by the Medical Student Research Office. They are required to submit a research proposal, a mentor’s letter of support, and to have identified a source of funding for the year before they can obtain approval. At the completion of the year, submission of a scholarly product is required for all students who have done research. This most often follows the form of an original manuscript for publication.
Discussion
Greater success in preventing, diagnosing, and treating disease will depend upon a multidisciplinary approach that involves individuals with diverse and complementary areas of expertise. The Carnegie Foundation’s four recommendations for training physicians, among them to integrate formal knowledge with clinical experience and to incorporate habits of inquiry and improvements into medical education at all levels, can be satisfied, at least in part, by providing research training to medical students [2]. Medical schools have developed different models for elective or required scholarly programs, either within the 4-year medical school curriculum or as part of a 5-year program [6–9]. At Mount Sinai, Immunology faculty members are active participants in medical student research programs. Medical students who participate in research training programs may be more comfortable questioning dogma, more likely to reflect on the underlying mechanisms of disease, and better prepared to participate in the development of novel approaches to solve complex health problems.
Immunology is a perfect example of this. More than any other field in the past half century, work in immunology has led to the elucidation of underlying mechanisms, the creation of new knowledge, the development of novel therapies, and a seamless transition from the bench to the bedside, and back. Successful teams have consistently included the best basic, translational, and clinical researchers, as well as seasoned clinicians. The fundamental importance of questioning basic principles and extending the application of immunology to such diverse areas of medicine as infectious disease, oncology, gastroenterology, cardiovascular disease, and rheumatology has been the key to the field’s success.
Yet, students entering medical school may not realize that career opportunities that combine clinical medicine and research exist. Research training programs that are offered early in medical school and that continue with increased degrees of independence as students advance may lead to increased participation in the programs [10]. They also may help students appreciate that it is possible to integrate clinical interests into a career with a research component. Mount Sinai School of Medicine has developed a portfolio of strongly mentored research training programs that begin during year 1 of medical school, continue until graduation, and offer students increasing independence as they advance in their training. Medical educators are still learning how to provide medical students with the knowledge, attitudes, and skills they need to participate in team science. We hope that beginning research training early and offering diverse programs will promote the development of students into critical thinking physicians and physician-scientists who are lifelong learners and active participants in the creation of new knowledge and novel approaches to improve healthcare.
References
Brass LF, Akabas MH, Burnley LD, Engman DM, Wiley CA, Andersen OS. Are MD-PhD programs meeting their goals? An analysis of career choices made by graduates of 24 MD-PhD programs. Acad Med. 2010;85:692–701.
Irby DM, Cooke M, O’Brien B. Calls for reform of medical education by the Carnegie foundation for the advancement of teaching: 1910 and 2010. Acad Med. 2010;85:220–7.
Green EP, Borkan JM, Pross SH, Adler SR, Nothnagle M, Parsonnet J, Gruppuso PA. Encouraging scholarship: medical school programs to promote student inquiry beyond the traditional medical curriculum. Acad Med. 2010;85:409–18.
Schor NF, Troen P, Kanter SL, Levine AS. The scholarly project initiative: introducing scholarship in medicine through a longitudinal, mentored curricular program. Acad Med. 2005;80:824–31.
Bierer SB, Chen HC. How to measure success: the impact of scholarly concentrations on students–a literature review. Acad Med. 2010;85:438–52.
Parsonnet J, Gruppuso PA, Kanter SL. Required versus elective research and in-depth scholarship programs in the medical student curriculum. Acad Med. 2010;85:405–8.
Boninger M, Troen P, Green E, Borkan J, Lance-Jones C, Humphrey A, Gruppuso P, Kant P, McGee J, Willochell M, Schor N, Kanter SL, Levine AS. Implementation of a longitudinal mentored scholarly project: an approach at two medical schools. Acad Med. 2010;85:429–37.
Laskowitz DT, Drucker RP, Parsonnet J, Cross PC, Gesundheit N. Engaging students in dedicated research and scholarship during medical school: the long-term experiences at Duke and Stanford. Acad Med. 2010;85:419–28.
Fishleder AJ, Henson LC, Hull AL. Cleveland Clinic Lerner College of Medicine: an innovative approach to medical education and the training of physician investigators. Acad Med. 2007;82:390–6.
Zier K, Friedman E, Smith L. Supportive programs increase medical students’ research interest and productivity. J Investig Med. 2006;54:201–7.
Acknowledgments
The authors gratefully acknowledge the support of medical student research programs offered by the Medical Student Research Office from the Doris Duke Charitable Foundation, The Mount Sinai Alumni, and grant #UL1RR029887 funded by the National Center for Research Resources’ Clinical and Translational Science Award (CTSA).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zier, K., Wyatt, C. & Muller, D. An innovative portfolio of research training programs for medical students. Immunol Res 54, 286–291 (2012). https://doi.org/10.1007/s12026-012-8310-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-012-8310-x