Abstract
Mutations of the Wiskott–Aldrich Syndrome Protein (WASP) are responsible for classic Wiskott–Aldrich Syndrome (WAS), X-linked thrombocytopenia (XLT), and in rare instances congenital X-linked neutropenia (XLN). WASP is a regulator of actin polymerization in hematopoietic cells with well-defined functional domains that are involved in cell signaling and cell locomotion, immune synapse formation, and apoptosis. Mutations of WASP are located throughout the gene and either inhibit or disregulate normal WASP function. Analysis of a large patient population demonstrates a strong phenotype–genotype correlation. Classic WAS occurs when WASP is absent, XLT when mutated WASP is expressed and XLN when missense mutations occur in the Cdc42-binding site. However, because there are exceptions to this rule it is difficult to predict the long-term prognosis of a given affected boy solely based on the analysis of WASP expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Following the discovery of the gene responsible for the Wiskott–Aldrich Syndrome (WAS) [1], it became possible to associate unique clinical phenotypes caused by mutations of the WAS Protein gene (WASP), suggesting a strong genotype–phenotype correlation with some degree of predictability for clinical outcome. This review examines the functional complexity of the WAS Protein (WASP), the variability of clinical symptoms and the effect of WASP mutations on the clinical phenotype.
Clinical and pathologic manifestations
A familial blood disorder characterized by thrombocytopenia and small platelets, which was associated with recurrent infections, and early death of the affected males, was described some 70 years ago by Alfred Wiskott, a young Bavarian hematologist who differentiated this rare congenital disease from Morbus Werlhofii, an eponym for idiopathic thrombocytopenic purpura (ITP) [2]. Subsequent reports demonstrated X-linked inheritance [3] and defective humoral and cellular immunity [4–7]. Most studies implicated a predominant T cell defect [7–9] but impaired maturation, decreased motility, reduced migration, and abnormal morphology of B cells have also been recognized [10, 11]. More recently, a profound defect in marginal B cell maturation has been observed independently by two groups [12, 13]. Abnormal natural killer (NK) cell function [14–16], reduced chemotaxis of monocytes [17] and impaired in vivo dendritic cell homing [18, 19] indicate that innate immunity is also affected. WASP+ regulatory T cells (Treg) were shown to exhibit a marked selective advantage in vivo in a WAS patient with a spontaneous revertant mutation, indicating that altered Treg fitness likely explains the autoimmune features in WAS [20]. Similarly, in WASP-deficient mice, the total percentage of FoxP3+ Tregs among CD4+ T cells was reduced and wasp−/− Tregs were rapidly out-competed by wasp+ Tregs in vivo [20].
Autoimmune diseases are frequent in patients with classic WAS, being present in 40% of a large cohort of families [7]. A retrospective review of risk factors, clinical features, and outcomes of autoimmune complications in patients with mutations of WASP, from a single center, further underlines the importance of this problem [21]. Of 55 WAS patients, 40 had at least one autoimmune or inflammatory complication. Malignant tumors can occur during childhood, but are more frequent in adolescents and young adults with the classic WAS phenotype. In a North American cohort studied by Sullivan et al., malignancies were present in 13%, with an average age at onset of 9.5 years. The most frequent malignancies reported were B cell lymphoma, often EBV positive [7].
Molecular basis of WAS
The gene responsible for this syndrome has been identified by positional cloning and by demonstrating mutations in lymphoblastoid cell lines derived from affected WAS patients [1]. The WASP gene encodes a 502-amino acid protein expressed exclusively in the cytoplasm of hematopoietic cells. WASP is a member of a distinct family of proteins that participate in the transduction of signals from the cell surface to the actin cytoskeleton. The WASP family of proteins are characterized by a C-terminal tripartite domain containing a common actin monomer-binding motif, the verprolin homology domain (V) and a central acidic region (A) that is capable of activating the actin-related protein (Arp)2/3 complex, a potent nucleator of actin polymerization [22]. A proline-rich region in exon 10 required for optimal actin polymerization activity, has been shown to be indispensable for effective recruitment of WASP to the immunologic synapse in T cells [23]. This sequence provides binding sites for multiple SH3-domain containing proteins, including the adaptor proteins P47nck, Grb2, and several protein tyrosine kinases including Btk, Tec, PLC-γ1, and Itk which directly activate WASP by means of tyrosine phosphorylation.
The N-terminal region of WASP allows recruitment of the WASP-interacting protein (WIP). In resting lymphocytes, WASP constitutively associates with WIP, stabilizing the inactive conformation of WASP [24]. Following engagement of the T cell antigen receptor, WIP is phosphorylated resulting in disengagement of WASP from the WIP/WASP complex, thus allowing WASP activation by Cdc42, which leads to actin polymerization and stabilization of actin filaments [25].
The Cdc42 binding domain (CBD) or CRIB domain, encoded by exons 7 and 8 of the WASP gene, allows the association of WASP with Cdc42, a member of the Rho family of GTPases which regulates the formation of filopodia and controls cell polarity and chemotaxis [26]. WASP recognizes the GTP bound, but not the GDP bound form of Cdc42, and binds to Cdc42-GTP with a 500-fold greater affinity than to Cdc42-GDP [27].
Computer modeling and binding experiments strongly suggest an autoinhibitory contact between the GBD and the carboxy-terminal region of WASP, which can be released by the activated (GTP) form of Cdc42 [28]. The Rho-like GTPases such as Cdc42 and Rac are key elements in the dynamic organization of the actin cytoskeleton. This hypothesis postulates that GBD has a profound effect on actin polymerization by controlling the interaction of the C-terminus of WASP with the Arp2/3 actin nucleating complex.
Genotype–phenotype correlation
Since its discovery in 1994 [1], WASP has been studied extensively in vitro and in vivo. The multiple functional domains of WASP were shown to be important for cell-signaling, actin polymerization, synapse formation, cell/cell interaction, chemotaxis, NK cell activity, and Treg function. It is therefore not surprising that the clinical phenotype of patients with alterations of the WASP gene may differ widely depending on the type and location of the mutation. While mutations that disrupt WASP expression are typically associated with the classic phenotype of WAS as reported by Wiskott [2], missense mutations in exons 1, 2, and 3 of the WASP gene are most often identified in patients with a milder variant of the disease, X-Linked thrombocytopenia (XLT). An even milder phenotype characterized by intermittent thrombocytopenia has been reported in a few Italian families [29]. The importance of autoinhibition of WASP is illustrated by the observation that missense mutations in the GBD that impair its interaction with the VCA-domain result in a constitutively active form of WASP which is responsible for X-linked neutropenia. [30–33]. Missense mutations within the hydrophobic core of the GDB (L270P, S272P; and I294T) have been shown to cause enhanced actin polymerization by interfering with the autoinhibition of WASP. This is achieved by either disrupting the α-helical structure or through insertion of a polar residue (I294T) adjacent to Tyr291. The most prominent features of patients with these GBD mutations are neutropenia and monocytopenia, suggestive of inhibited myelopoiesis. The mechanisms by which unregulated actin polymerization induces these features are not clear.
Thus, mutations of the WASP gene result in three distinct phenotypes:
-
(1)
The classic WAS triad of thrombocytopenia/micro-platelets, recurrent infections due to defective cognate and innate immunity, and eczema—complicated by increased risk of autoimmunity and malignancies.
-
(2)
The milder XLT variant, characterized predominantly by thrombocytopenia, sometimes occurring intermittently;
-
(3)
Congenital neutropenia without the clinical findings characteristic of WAS or XLT.
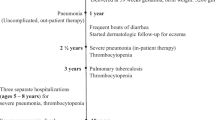
To distinguish these clinical phenotypes, a scoring system based on clinical and laboratory findings has been designed [34]. The most consistent genotype–phenotype correlation was observed when the patients were divided into two categories: WASP-positive if the mutated protein was present and of normal size, and WASP-negative if the protein was absent or truncated [35]. Patients with mutations that allowed the expression of normal-sized mutated protein (in most instances missense mutations in exons 1–3) often in reduced quantity, developed the XLT phenotype (score 1–2), whereas those patients with mutations that prevented lymphocytes to express WASP, or to express only truncated WASP (e.g., nonsense and splice site mutations, deletions, and insertion), were more likely to have the classic WAS phenotype (score 3–4). Progression to a score of 5 due to either autoimmune disease or malignancy was observed in both groups, but was far more prevalent in WASP-negative patients with an initial score of 3–4. Using the same scoring system in a group of Japanese patients, autoimmune diseases were equally frequent in those with a low symptom score, representing XLT, and in those with a high score, representing WAS. This result was predominantly due to the high incidence of IgA nephropathy in the Japanese patients. However, overall, the clinical phenotype observed in each patient correlated best with the presence or absence of WASP. Lack of protein expression was associated with susceptibility to bacterial, viral, and opportunistic infections, and with severe hemorrhage and malignancies. Overall, survival was significantly lower in WASP-negative patients [36].
It should be noted, however, that genotype–phenotype correlation in WAS/XLT is not absolute and that progression to a severe phenotype is possible [34, 35]. This discrepancy between WASP expression and clinical phenotype may be accounted for by other genetic or environmental factors. For these reasons, the long-term prognosis of WAS and XLT is difficult to be predicted solely based on the analysis of WASP expression. Additional studies are needed to define the long-term disease phenotype in the cohort of patients who initially present with the XLT phenotype.
References
Derry JM, Ochs HD, Francke U. Isolation of a novel gene mutated in Wiskott–Aldrich Syndrome. Cell. 1994;78:635–44.
Wiskott A. Familiärer, angeborener Morbus Werihofii? Monastsschr Kinderheilkd. 1937;68:212–6.
Aldrich R, Steinberg A, Campbell D. Pedigree demonstrating a sex-linked recessive condition characterized by draining ears, eczematoid dermatits and bloody diarrhea. Pediatrics. 1954;13:133–9.
Blaese RM, Strober W, Brown RS, et al. The Wiskott–Aldrich Syndrome. A disorder with a possible defect in antigen processing or recognition. Lancet. 1968;1:1056–61.
Cooper MD, Chae HP, Lowman JT, et al. Wiskott–Aldrich Syndrome. An immunologic deficiency disease involving the afferent limb of immunity. Am J Med. 1968;44:499–513.
Ochs HD, Slichter SJ, Harker LA, et al. The Wiskott–Aldrich Syndrome: studies of lymphocytes, granulocytes, and platelets. Blood. 1980;55:243–52.
Sullivan KE, Mullen CA, Blaese RM, et al. A multiinstitutional survey of the Wiskott–Aldrich Syndrome. J Pediatr. 1994;125:876–85.
Molina IJ, Sancho J, Terhorst C, et al. T cells of patients with the Wiskott–Aldrich Syndrome have a restricted defect in proliferative responses. J Immunol. 1993;151:4383–90.
Gallego MD, Santamaria M, Pena J, et al. Defective actin reorganization and polymerization of Wiskott–Aldrich T cells in response to CD3-mediated stimulation. Blood. 1997;90:3089–97.
Park JY, Shcherbina A, Rosen FS, et al. Phenotypic perturbation of B cells in the Wiskott–Aldrich Syndrome. Clin Exp Immunol. 2005;139:297–305.
Westerberg L, Larsson M, Hardy SJ, et al. Wiskott–Aldrich Syndrome Protein deficiency leads to reduced B-cell adhesion, migration, and homing, and a delayed humoral immune response. Blood. 2005;105:1144–52.
Westerberg LS, de la Fuente MA, Wermeling F, et al. WASP Confers selective advantage for specific hematopoietic cell populations and serves a unique role in marginal zone B cell homeostasis and function. Blood. 2008;112:4139–47.
Meyer-Bahlburg A, Becker-Herman S, Humblet-Baron S, et al. Wiskott–Aldrich Syndrome Protein deficiency in B cells results in impaired peripheral homeostasis. Blood. 2008;112:4158–69.
Orange JS, Ramesh N, Remold-O’Donnell E, et al. Wiskott–Aldrich Syndrome Protein is required for NK cell cytotoxicity and colocalizes with actin to NK cell-activating immunologic synapses. Proc Natl Acad Sci USA. 2002;99:11351–6.
Gismondi A, Cifaldi L, Mazza C, et al. Impaired natural and CD16-mediated NK cell cytotoxicity in patients with WAS and XLT: ability of IL-2 to correct NK cell functional defect. Blood. 2004;104:436–43.
Huang W, Ochs HD, Dupont B, et al. The Wiskott–Aldrich Syndrome Protein regulates nuclear translocation of NFAT2 and NF-kappa B (RelA) independently of its role in filamentous actin polymerization and actin cytoskeletal rearrangement. J Immunol. 2005;174:2602–11.
Badolato R, Sozzani S, Malacarne F, et al. Monocytes from Wiskott–Aldrich patients display reduced chemotaxis and lack of cell polarization in response to monocyte chemoattractant protein–1 and formyl-methionyl-leucyl-phenylalanine. J Immunol. 1998;161:1026–33.
Binks M, Jones GE, Brickell PM, et al. Intrinsic dendritic cell abnormalities in Wiskott–Aldrich Syndrome. Eur J Immunol. 1998;28:3259–67.
de Noronha S, Hardy S, Sinclair J, et al. Impaired dendritic-cell homing in vivo in the absence of Wiskott–Aldrich Syndrome Protein. Blood. 2005;105:1590–7.
Humblet-Baron S, Sather B, Anover S, et al. Wiskott–Aldrich Syndrome Protein is required for regulatory T cell homeostasis. J Clin Invest. 2007;117:407–18.
Dupuis-Girod S, Medioni J, Haddad E, et al. Autoimmunity in Wiskott–Aldrich Syndrome: risk factors, clinical features, and outcome in a single-center cohort of 55 patients. Pediatrics. 2003;111:622–7.
Welch MD, Mullins RD. Cellular control of actin nucleation. Annu Rev Cell Dev Biol. 2002;18:247–88.
Badour K, Zhang J, Shi F, et al. The Wiskott–Aldrich Syndrome Protein acts downstream of CD2 and the CD2AP and PSTPIP1 adaptors to promote formation of the immunological synapse. Immunity. 2003;18:141–54.
Sasahara Y, Rachid R, Byrne MJ, et al. Mechanism of recruitment of WASP to the immunological synapse and of its activation following TCR ligation. Mol Cell. 2002;10:1269–81.
Volkman BF, Prehoda KE, Scott JA, et al. Structure of the N-WASP EVH1 domain-WIP complex: insight into the molecular basis of Wiskott–Aldrich Syndrome. Cell. 2002;111:565–76.
Hall A. Rho GTPases and the actin cytoskeleton. Science. 1998;279:509–14.
Rudolph MG, Bayer P, Abo A, et al. The Cdc42/Rac interactive binding region motif of the Wiskott Aldrich Syndrome Protein (WASP) is necessary but not sufficient for tight binding to Cdc42 and structure formation. J Biol Chem. 1998;273:18067–76.
Kim AS, Kakalis LT, Abdul-Manan N, et al. Autoinhibition and activation mechanisms of the Wiskott–Aldrich Syndrome Protein. Nature. 2000;404:151–8.
Notarangelo LD, Mazza C, Giliani S, et al. Missense mutations of the WASP gene cause intermittent X-linked thrombocytopenia. Blood. 2002;99:2268–9.
Devriendt K, Kim AS, Mathijs G, et al. Constitutively activating mutation in WASP causes X-linked severe congenital neutropenia. Nat Genet. 2001;27:313–7.
Ancliff PJ, Blundell MP, Cory GO, et al. Two novel activating mutations in the Wiskott–Aldrich Syndrome Protein result in congenital neutropenia. Blood. 2006;108:2182–9.
Moulding DA, Blundell MP, Spiller DG, et al. Unregulated actin polymerization by WASp causes defects of mitosis and cytokinesis in X-linked neutropenia. J Exp Med. 2007;204:2213–24.
Beel K, Cotter MM, Blatny J, et al. A large kindred with X-linked neutropenia with an I294T mutation of the Wiskott-Aldrich Syndrome gene. Br J Haematol. 2008, Nov 1 [Epub ahead of print].
Ochs HD, Rosen FS. Wiskott–Aldrich Syndrome. In: Ochs HD, Smith CIE, Puck JM, editors. Primary immunodeficiency diseases, a molecular and genetic approach. New York: Oxford University Press; 2007. p. 454–69.
Jin Y, Mazza C, Christie JR, et al. Mutations of the Wiskott–Aldrich Syndrome Protein (WASP): hotspots, effect on transcription, and translation and phenotype/genotype correlation. Blood. 2004;104:4010–9.
Imai K, Morio T, Zhu Y, et al. Clinical course of patients with WASP gene mutations. Blood. 2004;103:456–64.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ochs, H.D. Mutations of the Wiskott–Aldrich Syndrome Protein affect protein expression and dictate the clinical phenotypes. Immunol Res 44, 84–88 (2009). https://doi.org/10.1007/s12026-008-8084-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12026-008-8084-3