Abstract
Abusive head injury, characterized by repeated acceleration–deceleration forces, is associated with retinal hemorrhages as demonstrated in many clinical and postmortem studies. The theory that vitreoretinal traction is the major factor in the pathogenesis of retinal hemorrhages is presently the most widely accepted explanation based on different lines of research. Postmortem examination of the eye and orbital structures is essential for recognizing abusive head injury and also for identifying other possible medical conditions which can cause retinal hemorrhage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abusive head injury includes the application of repeated acceleration–decelerationforces with or without head impact (also known as shaken baby syndrome, SBS). This syndrome is characterized by intracranial injury (most often subdural hemorrhage, subarachnoid hemorrhage and cerebral edema), fractures of the ribs, long bones and or skull, and retinal hemorrhage. Although 30% of victims do not survive the first episode of shaking trauma, survivors may be significantly disabled [1–5]. Despite increasing awareness of this syndrome it is still likely to be under-diagnosed worldwide. Up to one-third of cases are not identified when initially presenting to the emergency room especially since external evidence of trauma may be absent [6]. Postmortem findings can assist in diagnosis.
Retinal hemorrhages are a cardinal manifestation of abusive head injury characterized by repeated acceleration–decelerationwith or without blunt impact (Shaken Baby syndrome). The incidence of retinal hemorrhages in different studies ranges from 30 to 100% [7–12]. On average, 85% of victims will demonstrate retinal hemorrhages [13–15]. The incidence is not related to patient age or whether blunt head trauma was part of the insult. The repeated acceleration deceleration forces appear to be the primary factor in inducing the hemorrhages. In postmortem studies, using microscopic sections, the incidence of retinal hemorrhage may reach 100% due to the fact that clinically unidentified hemorrhages may be detected and also due to a correlation between severity of brain injury with severity of hemorrhagic retinopathy. In rare cases, even with no brain injury on brain CT or MRI, or no intracranial blood on CT scan, retinal hemorrhages have been identified [16, 17].
Types and patterns
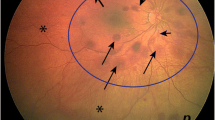
Retinal hemorrhages may be located anywhere anterior to the surface of the retina (preretinal hemorrhage), within the retinal tissue (intraretinal hemorrhage) or beneath the retina (subretinal hemorrhage). A vitreous hemorrhage occurs when blood extends into the well formed vitreous gel that fills the eye behind the lens and in front of the retina. Hemorrhages within the superficial retinal layers appear as flame shaped or “splinter” hemorrhages, so called because of their linear appearance caused by the superficial retinal nerve fiber layer in which they are located (Fig. 1). Hemorrhages located in deeper layers of the retina are classified as dot or blot hemorrhages, the former being smaller than the latter (Fig. 1).
Traumatic retinoschisis refers to splitting of the layers of the neurosensory retina, creating an intraretinal cavity within which blood can accumulate, most often under the inner limiting membrane. The accumulated blood can then separate by gravity, creating a blood-serum level distinction (Fig. 2). This finding is very specific to abusive head injury being otherwise reported in children less than 5 years old only in the context of fatal accidental crush head injury and fatal motor vehicle accidents. Even in head crush injury, the lesion appears to be rare and somewhat dissimilar to that seen in abuse. Traumatic retinoschisis most commonly occurs in the macula. In any cause of retinal bleeding, blood can become trapped between the blood vessel from which it arose and the internal limiting membrane, creating a non specific schisis-like lesion that is usually small.
Right retina of child victim of abusive head injury (Shaken Baby syndrome). * Denotes blood under internal limiting membrane within traumatic retinoschisis cavity in macula. S = subretinal hemorrhage, v = blood breaking out of schisis cavity into vitreous, arrows denote temporal edge of schisis cavity
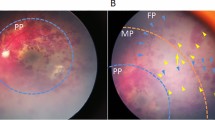
The edges of the retinoschisis lesions of the macula may be demarcated by a hemorrhagic ring or hypopigmentation due to injury to the underlying retinal pigment epithelium. In addition, circumlinear retinal folds may be seen (Fig. 3). These must be differentiated from the randomly and diffusely oriented short folds and the circumferential fold at the retinal edge (Lange’s fold) formed by postmortem fixation in children which are normal findings. At autopsy, vitreous may be seen attached to the apices of the paramacular folds of abusive head injury reflecting the role of vitreo-retinal traction in generating this pleating of the retina.
It is well established that the hemorrhages in abusive head injury may be asymmetric between the eyes [14, 15, 18, 19]. Unilateral retinal hemorrhages and retinoschisis may also occur [8, 18]. The mechanism for unilaterality is unknown and may not be related to the laterality of the intracranial findings. One group found a correlation but also included some eyes with evidence of direct blunt trauma.
Although posterior pole involvement is most common, hemorrhages in abusive trauma extending to the ora have been shown to have statistically significant implications in distinguishing abuse from accidental head injury [15].
Documentation
The standard of care is to have an ophthalmologist write a detailed description of the ocular findings, with or without a labeled drawing, after bedside examination pre-mortem. It is suggested that the note be written, or at least countersigned, by the attending staff ophthalmologist, having examined the patient, rather than a trainee. If available, retinal photography may also be useful. In cases of death prior to ophthalmic examination, indirect ophthalmoscopy can be performed up to 3 days after death in some cases.
Postmortem documentation should include detailed written descriptions in addition to photographs of the external eye and orbital tissues (from intracranial view) in situ [20]. It is also possible to use ocular endoscopy to view the retinal hemorrhages postmortem [21–23], but this may cause iatrogenic retinal detachment.
Orbital findings
Optic nerve sheath subdural and subarachnoid hemorrhage is a non specific finding that is common in victims of abusive head injury (Fig. 4). These hemorrhages are most often located in the anterior and posterior portions of the nerve and may be discontinuous. In these locations the optic nerve is firmly attached to the bony optic canal and sclera, creating fulcrums for increased shear as the globe translates within the orbit as repetitive acceleration–decelerationforces are applied to the child. Such hemorrhages may also occur in other situations (accidental head trauma, increased intracranial pressure) presumably from blood or increased intracranial pressure transmitted into the optic nerve sheath [18, 19]. Optic nerve sheath hemorrhages may occur with or without retinal hemorrhages. The optic nerve hemorrhage may at times be a direct extension of the central nervous system hemorrhage [24]. What seems to potentially distinguish abusive head injury is the presence of intradural hemorrhage, hemorrhage into the extraocular muscles and orbital fat hemorrhage. These lesions, in the absence of orbital fracture, seem to have a statistically significant association with abuse. Given the potential importance of these orbital findings, it has been recommended that autopsies of all young children with suspected abusive head injury or other apparently unexplained sudden death have the orbital tissues removed and examined along with the globe [20, 25].
Technique for orbital exenteration at postmortem
The techniques for orbital exenteration have been previously described [20, 25]. After the brain is removed and the optic nerves severed just posterior to their exit from the optic canal, the orbit is unroofed taking care to preserve the periosteum. The periosteum is then bluntly dissected away from the orbital walls and severed at the margins of the inferior orbital fissure. Using a standard approach for enucleation, a 360 degree conjunctival peritomy is performed and the capsulo-palpebral ligaments, lower lid retractors, inferior oblique and superior oblique tendons (in the area of the trochlea) are severed while leaving the horizontal and vertical recti in place. After careful retraction of the eyelids, often with the use of a lid speculum, the orbital septum is severed to establish a connection to the intracranial portion of the orbit. The entire globe and orbital contents, enclosed by periosteum, along with the canalicular optic nerve are then removed via the intracranial space en bloc. The specimen is then fixed in buffered formaldehyde for 48–72 h and then sectioned for examination.
The globe should be separated from the optic nerve by coronal section using a hand held blade (Fig. 4). Axial sections of the globe should be examined including the macula and the optic nerve. Coronal sections of the orbital contents are taken sequentially in an anterior-posterior direction and examined grossly and by light microscopy. Observed abnormalities should be photo documented and described.
Gilliland and Folberg described a method for so called replicating the clinician’s view of the eye by fixating the eye for 48 h, cutting the optic nerve at the sclera and thereafter removing the anterior segment through the pars plana and photographing [26].
Forensic timing
Retinal hemorrhages can not be dated by clinical examination. The rate of resolution of the retinal hemorrhage may be extremely fast, in particular with intraretinal hemorrhages which are sometimes resorbed within 24 h. This creates a situation where hemorrhages seen clinically may not be found at autopsy. Deeper and larger hemorrhages, retinoschisis, macular folds, vitreous hemorrhage, sub- and preretinal hemorrhage and optic nerve swelling resolve at a much slower rate.
Dating of retinal hemorrhages related to the normal process of birth has been thoroughly studied. Flame hemorrhages usually resolve in 3 days [27] but always by 1 week. Dot and blot hemorrhages usually resolve in 1 week after birth but may occasionally last up to 4–6 weeks especially when they are intrafoveal in which case they can last for months [28]. Preretinal and vitreous hemorrhage due to birth may also last beyond 1–2 months. Therefore attributing retinal hemorrhages to birth must be considered based on hemorrhage type and the age of the child. Otherwise the type and pattern of retinal hemorrhage may be indistinguishable from abuse. Retinoschisis has not been described as a result of birth.
Dating retinal hemorrhages postmortem is a difficult task. The presence of hemosiderin in autopsy tissue may indicate previous episodes of trauma or that the fatal injury occurred sufficiently before death for hemoglobin to be converted to hemosiderin. Hemosiderin may be detected as early as 2 days after the insult but may not be apparent by histochemical staining until 5–7 days after trauma, Hemosiderin may be present without concurrent hemorrhages [29]. Hemosiderin detected in an infant eye over the age of 2–3 months implies that the retinal hemorrhage occurred after birth [30].
Identification of iron staining in the optic nerve and retina is uncommon except in death caused by trauma. As with homosiderin, interpretation of the presence of iron requires information regarding the survival interval following the injury. If the interval is greater than 2–4 days the iron from a previous injury will not be distinguishable from organization of the current hemorrhage [31]. The value of hemosiderin in general remains unclear and in the retina the timing implications likely are so variable as to limit its forensic utility other than to identify that hemorrhage was present at some time [32, 33].
Pathogenesis of ocular findings
The preponderance of evidence points to vitreoretinal traction as the causative mechanism for retinal hemorrhages. The vitreous of young children is firmly attached to the retina at the optic nerve, macula, retinal vessels and retinal periphery. Repetitive abusive acceleration–decelerationforces may induce direct damage to vessels perhaps with a secondary disruption of autoregulation. This may be aggravated by orbital tissue injury involving the cranial nerves which carry autonomic supply to these vessels as discussed above. In addition, traumatic retinoschisis and perimacular folds are also caused by traction at the macula. Ocular coherence tomography studies have supported this mechanism [34, 35]. The preponderance of retinal hemorrhage in the retinal periphery is another manifestation of vitreoretinal traction.
In a study of the woodpecker, a bird which spends its lifetime submitting itself to repeated acceleration–decelerationwith head impact [35], it was interesting to note that the eyes are protected by restriction of globe movement in a tight orbit with many fascial connections between the sclera and the orbital rim. In addition, the sclera is reinforced by intra scleral cartilage and bone and their vitreous is not attached to the retina. This reduces, if not eliminates, shearing forces on the retina. Other animal models have also demonstrated hemorrhages in the areas of vitreoretinal attachment [36]. Finite element analysis computer modeling predicts maximal shear forces at areas of vitreoretinal traction [37, 38].
Although there is little evidence to suggest that increased intracranial or intrathoracic pressure play a significant role in retinal hemorrhage formation in SBS [39, 40]. They may have influence in conjunction with other factors such as imbalances of sodium chemistry, hypoxia, anemia and brain injury induced coagulopathy, and possibly potential factors currently under study such as vitamin C levels and thrombophilia, in modulating the appearance of hemorrhages. This is due to the fact that no correlation was found between raised intracranial pressure levels, raised intrathoracic pressure levels or side of the brain hemorrhages with the presence or severity of the retinal hemorrhages [14, 41, 42].
Differential diagnosis
Birth by any route (although most commonly after spontaneous or vacuum assisted vaginal delivery) [29] is the most common cause of pediatric retinal hemorrhages. Up to 50% of normal full term babies examined in the first 24 h of life will exhibit hemorrhages [27].
The rate of retinal hemorrhage after accidental trauma is <3%, with most studies showing no retinal hemorrhages [43, 44]. When hemorrhages occur, they are sparse and confined to the posterior pole. In severe fatal motor vehicle accidents the rate rises to only 17% [43, 44], still far less than that of abusive head trauma. This underscores the unique mechanisms resulting in retinal hemorrhage following repeated abusive acceleration-deceleration. There have been only three reported cases of fatal head crush injury resulting in severe hemorrhagic retinopathy and macular lesions reminiscent of retinoschisis [45, 46]. Shearing may once again have an important role [47]. These children should show other signs of head crush injury by history or autopsy [47, 48]. It is highly unlikely that the forces needed to generate retinal hemorrhages in a young child can be induced by a reasonable person playing with a child, attempting to arouse an apparently unconscious child or from a short fall. One paper looking at short falls cited only 18 out of 75,000 playground falls of children resulting in death, of which only six had eye examinations and four had retinal hemorrhage [49]. None had an ophthalmology consultation, none were infants, and none had truly short falls. This study underscores the importance of retinal hemorrhage, especially when extensive throughout the retina, multilayered, and associated with retinoschisis, as a marker to instigate investigation of abuse unless a satisfactory alternate explanation such as a fatal head crush or motor vehicle injury is known [50].
There are many other causes of retinal hemorrhage but these can be readily diagnosed by medical history, physical examination and laboratory tests. Leukemia is one of the few disorders where severe hemorrhages can be seen similar to those in SBS victims. Although in leukemia the hemorrhages are mostly located in the posterior pole they can also be observed in the periphery. The leukemias are readily diagnosed by complete blood count (CBC) and the retinopathy often has distinctive findings such as leukemic infiltrates, involvement of the optic nerve, thickening of the choroid on ultrasound, or leukemic itirits, all of which would help to distinguish these cases from abuse [51].
An imitator of child abuse due to the presence of both retinal and subdural hemorrhages following minor trauma is type 1 glutaric aciduria. Pre existing macrocrania is seen in most cases. Metabolic testing and extra pyramidal neurologic findings on physical examination and involvement of the basal ganglia on imaging differentiate this entity from SBS [52, 53]. The retinal hemorrhages tend to be few in number and confined to the posterior pole.
Papilledema is often associated with peripapillary flame hemorrhages. Victims of abusive head injury characterized by repeated acceleration–decelerationwith or without head impact tend not to develop papilledema even when increased intracranial pressure is present [8, 15, 32]. When present, hemorrhages in papilledema tend to be few in number, intra- or preretinal, and confined to the optic disc [54].
Even though many child abuse victims undergo cardiopulmonary resuscitation with chest compression during their treatment, sometimes delivered by untrained individuals at the site of the event, retinal hemorrhage due to this intervention are rare and the hemorrhages are very limited in number and again confined to the posterior pole [13, 55, 56]. One should not attribute more than a few intraretinal or preretinal hemorrhages to cardiopulmonary resuscitation. Likewise, Purtscher retinopathy, which would be the expected finding in chest crush injury, has never been observed following cardiopulmonary resuscitation. Characteristically, the expected features will be white intraretinal polygonal patches in the posterior pole more so than hemorrhages. Increased intrathoracic pressure can also be produced by valsalva maneuver during cough, seizure or severe vomiting. However, these events are not associated with retinal hemorrhage in children [57–60].
Conclusion
Abusive head injury is a major cause for childhood death worldwide. Retinal hemorrhage is a cardinal feature which when extensive, multilayered, extending to the ora, and associated with macular retinoschisis, perimacular folds, and evidence of orbital soft tissue injury, appears to have high diagnostic sensitivity for abusive injury characterized by repeated acceleration–decelerationforces with or without blunt head impact, particularly when there is no other obvious explanation. Attention to the copius literature on this subject, and the multiple converging lines of research, informs the clinician well and allows solid evidence based interpretations of postmortem findings. Ongoing research is essential and should focus on analysis of modulating factors for hemorrhage, standardizing documentation, developing scoring methodologies, and the pursuit of a basic biochemical understanding of retinal hemorrhage pathophysiology on the microscopic level.
Key points
-
1.
Abusive head injury includes the application of repeated acceleration–decelerationforces with or without head impact. This syndrome is characterized by intracranial injury, fractures of the ribs, long bones and/or skull, and retinal hemorrhage.
-
2.
The incidence of retinal hemorrhages is approximately 85%, but higher in autopsy studies.
-
3.
Vitreoretinal traction is the major factor in the pathogenesis of retinal hemorrhage in this form of child abuse.
-
4.
The rate of retinal hemorrhage after accidental head trauma is <3% with most studies showing no retinal hemorrhages. Rates may be higher (approximately 15%) for severe fatal head injury such as motor vehicle accidents and in fatal head crush injury.
-
5.
It is recommended that all autopsies of young children with suspected abusive head injury or other apparently unexplained sudden death have the orbital tissues removed en bloc with the globe as orbital injury may be an important feature of this form of abusive head injury.
References
Newton A, Vandeven A. Update on child maltreatment with a special focus on shaken baby syndrome. Curr Opin Pediatr. 2005;17:246–51.
Barlow K, Thompson E, Johnson D, Minns R. Late neurologic and cognitive sequelae of inflicted traumatic brain injury in infancy. Pediatrics. 2005;116:174–86.
Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. Jama. 2003;290:621–6.
King W, MacKay M, Sirnick A, Group CSBS. Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. Can Med Assoc J. 2003;168:155–9.
Lancon J, Haines D, Parent A. Anatomy of the shaken baby syndrome. Anat Rec. 1998;253:13–8.
Oral R, Yagmur F, Nashelsky M, et al. Fatal abusive head trauma cases: consequence of medical staff missing milder forms of physical abuse. Pediatr Emerg Care. 2008;24:816–21.
Ludwig S, Warman M. Shaken baby syndrome: a review of 20 cases. Ann Emerg Med. 1984;13:51–4.
Munger CE, Peiffer RL, Bouldin TW, et al. Ocular and associated neuropathologic observations in suspected whiplash shaken syndrome: a retrospective study of 12 cases. Am J Forensic Med Pathol. 1993;14:193–200.
Duhaime AC, Gennarelli TA, Thibault LE, et al. The shaken baby syndrome: a clinical, pathological, and biomechanical study. J Neurosurg. 1987;66:409–15.
Hadley M, Sonntag UK, Rekate HL, et al. The infant whiplash-shake injury syndrome: a clinical and pathological study. Neurosurgery. 1989;24:536–40.
Harcourt B, Hopkins D. Ophthalmic manifestations of the battered baby syndrome. Br Med J. 1971;3:398–401.
Mushin A. Ocular damage in the battered-baby syndrome. Br Med J. 1971;3:402–4.
Levin A. Retinal haemorrhage and child abuse. In: David T, editor. Recent advances in paediatrics. London: Churchill Livingstone; 2000. p. 151–219.
Kivlin J, Simons K, Lazoritz S, Ruttum M. Shaken baby syndrome. Ophthalmology. 2000;107(7):1246–54.
Morad Y, Kim Y, Armstrong D, Huyer D, Mian M, Levin A. Correlation between retinal abnormalities and intracranial abnormalities in the shaken baby syndrome. Am J Ophthalmol. 2002;134:354–9.
Bandak F. Shaken baby syndrome: a biomechanics analysis of injury mechanisms. Forensic Sci Int. 2005;151:71–9.
Merten DF, Radkowski MA, Leonidas JC. The abused child: a radiological reappraisal. Radiology. 1983;146:377–8.
Riffenburgh RS, Sathyavavagiswaran L. Ocular findings at autopsy of child abuse victims. Ophthalmology. 1991;98:1519–24.
Riffenburgh RS, Sathyavavagiswaran L. The eyes of child abuse victims: autopsy findings. J Forensic Sci. 1991;36:741–7.
Gilliland MG, Levin AV, Enzenauer AV, et al. Guidelines for postmortem protocol for ocular investigation of sudden unexplained infant death and suspected physical abuse. Am J Forensic Med Pathol. 2007;28:323–9.
Amberg R, Pollak S. Postmortem endoscopy of the ocular fundus: a valuable tool in forensic postmortem practice. Forensic Sci Int. 2001;124:157–62.
Davis NL, Wetli CV, Shakin JL. The retina in forensic medicine: applications of ophthalmic endoscopy: the first 100 cases. Am J Forensic Med Pathol. 2006;27(1):1–10.
Tsujinaka M, Bunai Y. Postmortem ophthalmologic examination by endoscopy. Am J Forensic Med Pathol. 2006;27(4):287–91.
Riffenburgh R. Ocular hemorrhages in autopsies of child abuse victims. Clin Surg Ophthalmol. 2005;23:178–86.
Wygnanski-Jaffe T, Levin AV, Shafiq A, et al. Postmortem orbital findings in shaken baby syndrome. Am J Ophthalmol. 2006;142:233–40.
Gilliland MG, Folberg R. Retinal hemorrhages: replicating the clinician’s view of the eye. Forensic Sci Int. 1992;56:77–80.
Kaur B, Taylor D. Fundus hemorrhages in infancy. Surv Ophthalmol. 1992;37:1–17.
Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. JAAPOS. 2006;10:102–6.
Emerson MV, Jakobs E, Green WR. Ocular autopsy and histopathologic features of child abuse. Ophthalmology. 2007;114:1384–94.
Matschke J, Puschel K, Glatzel M. Ocular pathology in shaken baby syndrome and other forms of infantile non-accidental head injury. Int J Legal Med. 2009;123:189–97.
Gilliland M. Why do histology on retinal haemorrhages in suspected non-accidental injury? Histopathology. 2003;43:592–4.
Elner S, Elner V, Albert D, Arnall M. In reply: the medicolegal implications of detecting hemosiderin in the eyes of children who are suspected of being abused. Arch Ophthalmol. 1991;109:322.
Gilliland M, Folberg R, Hayreh S. Age of retinal hemorrhages by iron detection. Am J Forensic Med Pathol. 2005;26(1):1–4.
Sturm V, Knecht PB, Landau K, et al. Rare retinal hemorrhages in translational accidental head trauma in children. Eye. 2009;23:1535–41.
Wygnanski-Jaffe T, Murphy CJ, Smith C, et al. Protective ocular mechanisms in woodpeckers. Eye. 2007;21:83–9.
Coats B, Binenbaum G, Peiffer RL, Forbes BJ. Margulies, SS ocular hemorrhage in single, non-impact head rotations: a porcine model. Second international conference on pediatric abusive head trauma. Wyoming: Jackson Hole; 2009.
Bhola R, Cirovic S, Parson M, Hose D, Lawford P, Howard I. Modeling of the eye and orbit to simulate Shaken Baby syndrome. Invest Ophthalmol Vis Sci. 2005;46:E-Abstract 4090.
Rangarajan N, Kamalakkannan S, Hasija H, et al. Finite element model of ocular injury in Shaken Baby syndrome. JAAPOS. 2009; (in press).
Schloff S, Mullaney PB, Armstrong DC, et al. Retinal findings in children with intracranial hemorrhage. Ophthalmology. 2002;109:1472–6.
Tomasi L, Rosman P. Purtscher retinopathy in the battered child syndrome. Am J Dis Child. 1986;93:1335–7.
Stoodley N. Controversies in non-accidental head injury in infants. Br J Radiol. 2006;79:550–3.
Marshall DH, Brownstein S, Dorey MW. The spectrum of postmortem ocular findings in victims of shaken baby syndrome. Can J Ophthalmol. 2001;36:377–83.
Bechtel K, Stoessel K, Leventhal JM, et al. Characteristics that distinguish accidental from abusive injury in hospitalized young children with head trauma. Pediatrics. 2004;114:165–8.
Vinchon M, Defoort-Dhellemmes S, Desurmont M, Dhellemmes P. Accidental and nonaccidental head injuries in infants: a prospective study. J Neurosurg. 2005;102:380–4.
Lueder GT, Turner JW, Paschall R. Perimacular retinal folds simulating nonaccidental injury in an infant. Arch Ophthalmol. 2006;124:1782–3.
Lantz PE, Sinal SH, Stanton CA, et al. Perimacular retinal folds from childhood head trauma. Br Med J. 2004;328:754–6.
Levin AV. The spectrum of postmortem ocular findings in victims of shaken baby syndrome discussion. Can J Ophthalmol. 2001;36:383–4.
Gnanaraj L, Gilliland MG, Yahya RR, et al. Ocular manifestations of crush head injury in children. Eye. 2007;21:5–10.
Plunkett J. Fatal pediatric head injuries caused by short-distance falls. Am J Forensic Med Pathol. 2001;22:1–12.
Adams G, Ainsworth J, Butler L, et al. Update from the ophthalmology child abuse working party: Royal College ophthalmologists. Eye. 2004;18:795–8.
Reddy SC, Jackson N. Retinopathy in acute leukaemia at initial diagnosis: correlation of fundus lesions and haematological parameters. Acta Ophthalmol Scand. 2004;82:81–5.
Gago L, Wegner R, Capone A, Williams G. Intraretinal hemorrhages and chronic subdural effusions: glutaric aciduria type 1 can be mistaken for Shaken Baby syndrome. Retina. 2003;23:724–6.
Strauss KA, Puffenberger EG, Robinson DL, Morton DH. Type I glutaric aciduria, part 1: natural history of 77 patients. Am J Med Genet C Semin Med Genet. 2003;121C:38–52.
Coppeto JR, Monteiro ML. Juxtapapillary subretinal hemorrhages in pseudotumor cerebri. J Clin Neuroophthalmol. 1985;5:45–53.
Gilliland M, Luckenbach M. Are retinal hemorrhages found after resuscitation attempts? A study of the eyes of 169 children. Am J Forensic Med Pathol. 1993;14:187–92.
Goetting M, Sowa B. Retinal haemorrhage after cardiopulmonary resuscitation in children: an etiologic evaluation. Pediatrics. 1990;85:585–8.
Chapman-Davies A, Lazarevic A. Valsalva maculopathy. Clin Exp Optom. 2002;85:42–5.
Herr S, Pierce M, Berger R, Ford H, Pitetti R. Does Valsalva retinopathy occur in infants? An initial investigation in infants with vomiting caused by pyloric stenosis. Pediatrics. 2004;113:1658–61.
Goldman M, Dagan Z, Yair M, Elbaz U, Lahat E, Yair M. Severe cough and retinal hemorrhage in infants and young children. J Pediatr. 2006;148:835–6.
Curcoy AI, Trenchs V, Morales M. Do retinal hemorrhages occur in infants with convulsions? Arch Dis Child. 2009;11:873–5.
Acknowledgments
This work was supported in part by The Foerderer Fund
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wygnanski-Jaffe, T., Morad, Y. & Levin, A.V. Pathology of retinal hemorrhage in abusive head trauma. Forensic Sci Med Pathol 5, 291–297 (2009). https://doi.org/10.1007/s12024-009-9134-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12024-009-9134-4