Abstract
Background and aims
Although low-density lipoprotein cholesterol (LDL-C) has been considered as a risk factor of atherosclerotic cardiovascular disease, limited studies can be available to evaluate the association of LDL-C with risk of mortality in the general population. This study aimed to examine the association of LDL-C level with risk of mortality using a propensity-score weighting method in a Chinese population, based on the health examination data.
Methods
We performed a retrospective cohort study with 65,517 participants aged 40 years or older in Ningbo city, Zhejiang. LDL-C levels were categorized as five groups according to the Chinese dyslipidemia guidelines in adults. To minimize potential biases resulting from a complex array of covariates, we implemented a generalized boosted model to generate propensity-score weights on covariates. Then, we used Cox proportional hazard regression models with all-cause and cause-specific mortality as the dependent variables to estimate hazard ratios (HRs) and 95% confidence intervals (95% CIs).
Results
During the 439,186.5 person years of follow-up, 2403 deaths occurred. Compared with the median LDL-C group (100–130 mg/dL), subjects with extremely low LDL-C levels (group 1) had a higher risk of deaths from all-cause (HR = 2.53, 95% CI:1.80–3.53), CVD (HR = 1.84, 95% CI: 1.28–2.61), ischemic stroke (HR = 2.29, 95% CI:1.32–3.94), hemorrhagic stroke (HR = 3.49, 95% CI: 1.57–7.85), and cancer (HR = 2.12, 95% CI: 1.04–4.31) while the corresponding HRs in LDL-C group 2 were relatively lower than that in group 1.
Conclusions
Low LDL-C levels were associated with an increased risk of all-cause, CVD, ischemic stroke, hemorrhagic stroke, and cancer mortality in the Chinese population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lower low-density lipoprotein cholesterol (LDL-C) level has been indicated to decrease the risk of atherosclerotic cardiovascular disease (ASCVD) [1,2,3,4]. LDL-C has now largely replaced total cholesterol as a primary lipid measurement for evaluation of risk due to atherogenic lipoproteins [5] and most current guidelines include LDL-C as a primary target for initiating and adjusting lipid-lowering interventions [6,7,8,9,10]. Achieving low LDL-C levels by lipid-lowering agents has been demonstrated to be associated with reduced risk of nonfatal cardiovascular events and CVD mortality [11,12,13].
Although previous studies have investigated the association between LDL-C levels and mortality, most of the findings were from randomized clinical trials and limited to the high-risk population, and showed beneficial effects of achieving low levels of LDL-C by intensive treatment. However, the relationship between LDL-C and mortality in the general population remains inconsistent. Results from the Cooper Center Longitudinal Study showed that LDL-C ≥160 mg/dL were independently associated with an increased risk of CVD mortality in a low 10-year risk population [14]. However, other studies indicated no associations for CVD mortality in a high-risk population [15]. And results from a Chinese study demonstrated strong positive associations of LDL-C with ischemic stroke and inverse associations with intracerebral hemorrhage [16]. For cancer mortality, low LDL-C level has been reported to be associated with cancer mortality in a middle-aged Korean population [17] but not in a Chinese population [18], but low LDL-C level in Korean study could not be ruled out the explanation of debilitation and illness. In this Korean study, all participants were non-statin users, and beneficial effects might be found in patients with lipid-lowering treatment. Furthermore, a recent Denmark study found the U-shaped association between LDL-C levels and all-cause and cancer mortality [19].
Propensity scores (PS) have been now commonly used in observational studies to adjust for baseline characteristics of treatment groups and potential bias, including four methods: covariate adjustment using the propensity score, stratification on the propensity score, propensity-score matching, and inverse probability of treatment weighting (IPTW) using the propensity score. Of which, IPTW has superior performance than the other three methods [20]. For independent variables with multiple levels, a multinomial propensity score may allow to some extent for a better comparison of multiple treatment groups, but this is still underused and not widely known [21].
Herein, we performed a cohort study using the health examination data from the Yinzhou Health Information System (YHIS) in Ningbo city to examine the association between LDL-C concentration and risk of all-cause and cause-specific mortality in a Chinese population using PS weighted model.
Methods
Study design and population
This retrospective population-based cohort study was based on the YHIS in Ningbo city. Yinzhou district is the biggest district in Ningbo city with over 800,000 residents. YHIS is composed of residents’ healthcare records, Chronic Diseases Recording System and Hospital Information System [22]. In the present study, we recruited 76,107 residents who had at least one measurement record of LDL-C from the YHIS during 2010–2014. Of these subjects, a total of 10,312 were excluded due to a history of cardiovascular events (heart disease and stroke), diabetes mellitus, and cancer, and 278 due to <1 year of follow-up. Thus, a total of 65,517 subjects with at least one measurement of LDL-C were included into our analysis to examine the association of LDL-C levels at baseline with mortality. Written informed consent was obtained from each subject for the use of the data.
LDL-C measurement
LDL-C was measured using fasting serum samples by an automatic biochemical analyzer for all subjects. In our analysis, to represent more accurate baseline LDL-C level of individuals, we used the mean LDL-C value for each subject during the baseline period instead of using the first measurement. We divided LDL-C levels into five groups (group 1: <70 mg/dL, group 2: 70–100 mg/dL, group 3: 100–130 mg/dL, group 4: 130–160 mg/dL and group 5: ≥160 mg/dL) according to the Chinese dyslipidemia guidelines in adults [6].
Data collection
Data on demographic characteristics (such as age at baseline, gender, marital status, and education level), and lifestyle factors (such as smoking status, alcohol drinking status, and physical activity frequency) were obtained from the YHIS. Cigarette smoking was defined as smoking at least one cigarette per day for 1 year or more, and categorized as current, former, and never; Alcohol consumption was defined as drinking any alcohol at least 100 g per week during the last year, and categorized as current, former, and never; physical activity (PA) was defined as running, biking and brisk walking and other aerobic activities at least 20 min once [22]. PA frequency was categorized as less than one time weekly, 1–4 times weekly, or more than 4 times weekly; We also obtained lipid-lowing medication status for all participants. All physical examinations (including weight, height, and blood pressure (BP)) and data collection followed a standard protocol. Weight and height were recorded while individuals were not wearing shoes. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared, and categorized as underweight (<18.5 kg/m2), normal (18.5–23.9 kg/m2), and overweight or obese (≥24 kg/m2). BP was measured when participants were in a seated position after resting for 5 min using the mercury sphygmomanometer. High-density lipoprotein cholesterol (HDL-C) was measured using fasting serum samples by an automatic biochemical analyzer for all subjects. History of hypertension was self-reported or current use of antihypertensive medication or defined as systolic BP (SBP) ≥140 mmHg, or diastolic BP (DBP) ≥90 mmHg.
Outcome
All-cause and cause-specific mortality were considered as endpoints in this study. Death status was monitored with official death certificates from Yinzhou Center for Disease Control and Prevention (Yinzhou CDC). Primary causes of death were identified by the International Classification of Disease, 10th Revision (ICD10). Death status for each subject was ascertained by linking them to the Yinzhou Death Database, with the most recent update on 31 December 2017. In our study, we also considered cause-specific mortality as follows: (1) cardiovascular disease, CVD (ICD10 code: I00-I99), (2) cerebrovascular disease: hemorrhagic stroke (HS) (ICD10 code: I60–I62) and ischemic stroke (IS) (ICD10 code: I63 or I69.3), and (3) cancer (ICD10 codes: C00-C99).
Statistical analysis
Continuous and categorical variables were presented as median values (interquartile range (IQR)) and n (%), respectively. Person years were calculated from the date of the LDL-C measurement at baseline until death, or 31 December 2017, whichever came first. Comparisons of baseline characteristics among subjects with different categories of LDL-C were performed using nonparametric Kruskal–Wallis test for continuous variables and Pearson Chi-square test for categorical variables. In the primary analysis, we used IPTW of propensity score to improve the comparability of LDL-C groups on observed covariates to reduce bias in the effect estimates [21]. PS were estimated using generalized boosted model using the “TWANG” (Toolkit for Weighting and Analysis of Nonequivalent Groups) package (version 1.6) [23] and R statistical software (version 3.6.1, The R Project for Statistical Computing), which implements an automated, nonparametric machine learning method. PS were estimated based on demographic characteristics, lifestyle factors, BMI status, SBP, DBP, HDL-C concentration, history of hypertension, and lipid-lowing medication status. The weights were derived to obtain estimates of the average treatment effect on the treated (ATT) for each group as compared with the reference group (group 3). ATT weights were generated using the R mnps (multinomial PS) function in the twang package for the study sample. Balance between potential confounding factors was assessed by the standardized mean difference. Differences <0.10 were considered as evidence of balance [21]. After establishing the weights described above, we estimated hazard ratios (HRs) and 95% confidence intervals (95% CIs) for the associations of LDL-C with risk of all-cause and cause-specific mortality using Cox proportional hazards regression models [24].
In the sensitivity analysis, we adjusted for above covariates or only included PS as a covariate in the Cox models as compared with the results in the primary analysis. The proportional hazard assumption was tested on the basis of Schoenfeld residuals(P > 0.05 for all tests). All tests were two sided, and P < 0.05 was considered statistically significant. All statistical analyses were performed using R version 3.6.1.
Results
A total of 65,517 subjects were included in our study. During the 439,186.5 person years of follow-up, 2403 deaths occurred, including 721 form CVD, and 811 from cancer. The mortality density was 5.47 deaths per 1000 person years for all participants. The mean LDL-C concentration was 112.92 mg/dL and age at baseline ranged from 40 to 97 years. Of eligible participants, more than half (56.5%) were women. Individuals who had higher LDL-C concentration were more likely to be female and older, to have a higher prevalence of hypertension, overweight and lower education level, and were more commonly nonsmokers, nondrinkers, frequent exercisers, and lipid-lowing medication takers (Table 1).
Table 2 shows a summary of means of all covariates and standardized mean differences (SMDs) in Propensity-Score unweighted and weighted data. All SMDs were lower than 0.10 after PS weighting, indicating that PS successfully further minimized group differences in the covariates and balanced the potential confounders between the compared groups.
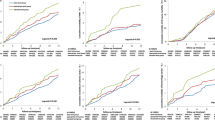
Table 3 presents the results of PS weighted Cox proportional hazard models. As compared with the reference LDL-C group (100–130 mg/dL), subjects in LDL-C group 1 had a higher risk of deaths from all-cause (HR = 2.53, 95% CI: 1.80–3.53), CVD (HR = 1.84, 95% CI: 1.28–2.61), IS (HR = 2.29, 95% CI:1.32–3.94), hemorrhagic stroke (HR = 3.49, 95% CI: 1.57–7.85), and cancer (HR = 2.12, 95% CI: 1.04–4.31). The corresponding HRs in LDL-C group 2 were 1.39 (95% CI: 1.07–1.31) for all-cause mortality, 1.40 (95% CI: 1.16–1.68) for CVD mortality, 1.23 for IS mortality (95% CI: 0.88–1.73), 1.70 (95% CI: 1.07–2.66) for hemorrhagic stroke mortality, and 1.35 (95% CI: 1.14–1.60) for cancer mortality, respectively. Subjects in group 5 (LDL-C ≥ 160 mg/dL) also had a higher risk of hemorrhagic stroke mortality (HR = 2.48, 95% CI:1.13–5.42).
Sensitivity analyses by using multivariable Cox models with no consideration of PS method or including PS as a covariate in models indicated relatively lower HRs for the associations of LDL-C with risk of mortality (Tables 4, 5).
Discussion
The present study examined the association of LDL-C level at baseline with risk of all-cause and cause-specific mortality in a Chinese population using PS weighted models, based on the health examination data. Overall, our primary results showed that extremely low LDL-C level (<70 mg/dL) was associated with an increased risk of deaths from all-cause, CVD, IS, HS and cancer. We also found a similar association of low levels (70–100 mg/dL) with risk of mortality except for IS.
In our study, we found that the associations in different levels of LDL-C were relatively attenuated but did not substantially change in the sensitivity analyses with regression-based covariates adjustment. As suggested in a previous study, propensity-score weighting methods are better than regression-based covariates adjustment or covariate adjustment using PS [20, 25]. Therefore, we presented the primary results from the PS weighted Cox models in this study.
Our results suggested that very low LDL-C levels were associated with an increased risk of all-cause, CVD, HS and cancer mortality, which was supported by the findings from recent studies in Korea and Denmark. The Korea study found that the lowest category of LDL-C (<70 mg/dL) was associated with higher risk of all-cause, CVD and cancer mortality in non-statin users [17] while another study also found similar results in the general population after adjusting lipid-lowering treatment [19]. For stroke mortality, we observed that the lowest level of LDL-C was associated with HS mortality. A prospective study demonstrated that participants with LDL-C concentrations <70 mg/dL had a significantly higher risk of developing intracerebral hemorrhage [16]. A 20-year epidemiologic study among the young and middle-aged population presented similar results for the association between low LDL-C levels (<70 mg/dL) and hemorrhagic stroke mortality [18]. Similarly, a Korean National Health Screening Cohort reported that persistently low cholesterol levels were associated with a higher risk of mortality [26]. However, we also found that high LDL-C levels (>160 mg/dL) was associated with hemorrhagic stroke mortality, which was inconsistent with the previous findings [27]. One possible explanation might be the lack of enough hemorrhagic stroke deaths (n = 130) in our study. The association between LDL-C and hemorrhagic stroke mortality should be confirmed in large cohort studies with enough hemorrhagic stroke deaths. Although some studies have demonstrated positive associations between LDL-C levels and IS [28, 29], there were limited studies about LDL-C and IS mortality and some studies suggested that LDL-C level was not associated with risk of IS [30]. Consequently, the association between LDL-C and IS mortality ought to be further explored. These findings suggested that very low LDL-C levels may cause higher risk of poor health outcomes. However, the potential mechanism remains to be elucidated. Our findings could be explained by the following: Some experiments have shown that LDL-C could play important anti-infective roles and protect against endotoxin-induced tissue damage [31, 32]. Furthermore, some studies have suggested that dysbiosis and altered bile acid metabolism [33,34,35,36] as a common mechanism may operate that links low LDL-C concentration to different disease status. Extremely low LDL-C levels may increase susceptibility to fatal disease.
The 2019 European Society of Cardiology/European Atherosclerosis Society guidelines for the management of dyslipidemia recommend a target of <70 mg/dL (or >50% reduction in LDL-C) in patients with CVD [9]. National Lipid Association (NLA) suggests that LDL-C levels for primary prevention are <100 mg/dL in the low/moderate/high-risk population and <70 mg/dL for very high-risk population [8]. The 2018 American Heart Association/American College of Cardiology Multi-society Guideline on the management of blood cholesterol suggests 70 mg/dL as the lowest value of LDL-C at which lipid-lowering therapy is recommended [37]. The Chinese dyslipidemia guideline in adults recommends that optimal LDL-C level is <100 mg/dL for primary prevention in the general population [6]. And individuals with very low LDL-C levels (usually <50 mg/dL) caused by familial hypobetalipoproteinemia were substantially healthy and found to have a decreased risk of arterial stiffness, indicating cardiovascular protection [38]. Unfortunately, we cannot evaluate the role of familial hypobetalipoproteinemia on LDL-C levels in our study due to a lack of data. Our findings showed that LDL-C levels below 70 mg/dL might lead to a higher risk of CVD mortality, which was inconsistent with evidence from clinical trials and above dyslipidemia guidelines. However, it would be incorrect to use our data against the beneficial effects of lipid-lowering therapy and keeping low LDL-C levels in the prevention of ASCVD. The possible explanations were as follows: firstly, reverse causality might exist in this study due to our study design of a retrospective cohort, some baseline information was collected incompletely such as history of chronic disease and family disease, which might be associated with risk of CVD; secondly, participants included in our study were selected from the health examination population who might be more susceptible to risk of CVD; thirdly, variability of LDL-C levels may exist during the follow-up period, because we only had a single data of LDL-C levels at baseline, and data on the first lipid-lowering medication usage could not be available. Moreover, a supportive argument in a recent cohort study stated that reduction in levels of LDL-C caused by lipid-lowering treatment does not explain the increased risk of mortality at low levels of LDL-C but rather low LDL-C levels is a predictor for mortality [19]. In addition, we also found a similar association of low LDL-C levels (70–100 mg/dL) with a higher risk of CVD mortality. It might be explained by the persistence of the effect of lipid-lowering therapy in subjects at high cardiovascular risk that were classified into the lower LDL-C groups in the study.
Strengths and limitations
Our study had several strengths including large sample size, collection of multiple confounders (such as lipid-lowering medication) and the use of PS weighting methods. In addition, we also excluded subjects who suffered from CVD, stroke, and cancer at baseline and were followed up <1 year, which could help decrease the influence of potential reverse causality. However, our study also had several limitations. Firstly, although this was a retrospective cohort study including a total of 65,517 subjects, we had a relatively smaller sample than similar studies in the Chinese population. Secondly, there were fewer deaths than other studies, causing low mortality due to the relatively short duration of follow-up. Thirdly, although we used IPTW to balance the distribution of measured confounders among different LDL-C groups, lipid-lowering treatment might affect subjects’ classification and the comparability of different LDL-C groups. Fourthly, several factors such as dietary and genetic factors were not measured in our study, which could affect our results. Finally, subjects in our study were enrolled from one district in Ningbo city, which may not represent our target population. Unfortunately, we cannot conduct a multicenter study due to a lack of data from other districts.
Conclusions
In summary, in this large retrospective cohort study, we found that very low LDC-C levels (<100 mg/dL) were associated with higher risk of all-cause, CVD IS, HS, and cancer mortality in this Chinese population. Our findings might have important clinical and public health implications, if confirmed in the future.
References
B.A. Ference, H.N. Ginsberg, I. Graham, K.K. Ray, C.J. Packard, E. Bruckert, R.A. Hegele, R.M. Krauss, F.J. Raal, H. Schunkert, G.F. Watts, J. Boren, S. Fazio, J.D. Horton, L. Masana, S.J. Nicholls, B.G. Nordestgaard, B. van de Sluis, M.R. Taskinen, L. Tokgozoglu, U. Landmesser, U. Laufs, O. Wiklund, J.K. Stock, M.J. Chapman, A.L. Catapano, Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38(32), 2459–2472 (2017). https://doi.org/10.1093/eurheartj/ehx144
B. Mihaylova, J. Emberson, L. Blackwell, A. Keech, J. Simes, E.H. Barnes, M. Voysey, A. Gray, R. Collins, C. Baigent, The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380(9841), 581590 (2012). https://doi.org/10.1016/s0140-6736(12)60367-5
M.G. Nanna, A.M. Navar, D. Wojdyla, E.D. Peterson, The Association between low-density lipoprotein cholesterol and incident atherosclerotic cardiovascular disease in older adults: results from the national institutes of health pooled cohorts. J. Am. Geriatr. Soc. 67(12), 2560–2567 (2019). https://doi.org/10.1111/jgs.16123
M.G. Silverman, B.A. Ference, K. Im, S.D. Wiviott, R.P. Giugliano, S.M. Grundy, E. Braunwald, M.S. Sabatine, Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: a systematic review and meta-analysis. Jama 316(12), 1289–1297 (2016). https://doi.org/10.1001/jama.2016.13985
R.K. Wadhera, D.L. Steen, I. Khan, R.P. Giugliano, J.M. Foody, A review of low-density lipoprotein cholesterol, treatment strategies, and its impact on cardiovascular disease morbidity and mortality. J. Clin. Lipidol. 10(3), 472–489 (2016). https://doi.org/10.1016/j.jacl.2015.11.010
Adults, J.C.f.R.C.g.o.P.a.T.o.D.i., Chinese guidelines on prevention and treatment of dyslipidemia in adults(2016 revison). Chin. Circ. J. 31(10), 937–953 (2016). https://doi.org/10.3969/j.issn.1000-3614.2016.10.001
Expert Dyslipidemia Panel of the International Atherosclerosis Society Panel, m., An International Atherosclerosis Society Position Paper: global recommendations for the management of dyslipidemia—full report. J. Clin. Lipidol. 8(1), 29–60 (2014). https://doi.org/10.1016/j.jacl.2013.12.005
T.A. Jacobson, M.K. Ito, K.C. Maki, C.E. Orringer, H.E. Bays, P.H. Jones, J.M. McKenney, S.M. Grundy, E.A. Gill, R.A. Wild, D.P. Wilson, W.V. Brown, National Lipid Association recommendations for patient-centered management of dyslipidemia: part 1—executive summary. J. Clin. Lipidol. 8(5), 473–488 (2014). https://doi.org/10.1016/j.jacl.2014.07.007
F. Mach, C. Baigent, A.L. Catapano, K.C. Koskinas, M. Casula, L. Badimon, M.J. Chapman, G.G. De Backer, V. Delgado, B.A. Ference, I.M. Graham, A. Halliday, U. Landmesser, B. Mihaylova, T.R. Pedersen, G. Riccardi, D.J. Richter, M.S. Sabatine, M.R. Taskinen, L. Tokgozoglu, O. Wiklund, 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 41(1), 111–188 (2020). https://doi.org/10.1093/eurheartj/ehz455
N.J. Stone, J.G. Robinson, A.H. Lichtenstein, C.N. Bairey Merz, C.B. Blum, R.H. Eckel, A.C. Goldberg, D. Gordon, D. Levy, D.M. Lloyd-Jones, P. McBride, J.S. Schwartz, S.T. Shero, S.C. Smith, K. Watson, P.W.F. Wilson, 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Circulation 129(25 suppl 2), S1–S45 (2014). https://doi.org/10.1161/01.cir.0000437738.63853.7a
P.J. Delahoy, D.J. Magliano, K. Webb, M. Grobler, D. Liew, The relationship between reduction in low-density lipoprotein cholesterol by statins and reduction in risk of cardiovascular outcomes: an updated meta-analysis. Clin. Ther. 31(2), 236–244 (2009). https://doi.org/10.1016/j.clinthera.2009.02.017
E.P. Navarese, J.G. Robinson, M. Kowalewski, M. Kolodziejczak, F. Andreotti, K. Bliden, U. Tantry, J. Kubica, P. Raggi, P.A. Gurbel, Association between baseline LDL-C level and total and cardiovascular mortality after LDL-C lowering: a systematic review and meta-analysis. Jama 319(15), 1566–1579 (2018). https://doi.org/10.1001/jama.2018.2525
R. Verbeek, R.M. Hoogeveen, A. Langsted, L.C.A. Stiekema, S.L. Verweij, G.K. Hovingh, N.J. Wareham, K.T. Khaw, S.M. Boekholdt, B.G. Nordestgaard, E.S.G. Stroes, Cardiovascular disease risk associated with elevated lipoprotein(a) attenuates at low low-density lipoprotein cholesterol levels in a primary prevention setting. Eur. Heart J. 39(27), 2589–2596 (2018). https://doi.org/10.1093/eurheartj/ehy334
S.M. Abdullah, L.F. Defina, D. Leonard, C.E. Barlow, N.B. Radford, B.L. Willis, A. Rohatgi, D.K. McGuire, J.A. de Lemos, S.M. Grundy, J.D. Berry, A. Khera, Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease. Circulation 138(21), 2315–2325 (2018). https://doi.org/10.1161/circulationaha.118.034273
G.A. Kaysen, X. Ye, J.G. Raimann, Y. Wang, A. Topping, L.A. Usvyat, S. Stuard, B. Canaud, F.M. van der Sande, J.P. Kooman, P. Kotanko, Monitoring dialysis outcomes, I.: lipid levels are inversely associated with infectious and all-cause mortality: international MONDO study results. J. Lipid Res. 59(8), 1519–1528 (2018). https://doi.org/10.1194/jlr.P084277
L. Sun, R. Clarke, D. Bennett, Y. Guo, R.G. Walters, M. Hill, S. Parish, I.Y. Millwood, Z. Bian, Y. Chen, C. Yu, J. Lv, R. Collins, J. Chen, R. Peto, L. Li, Z. Chen; China Kadoorie Biobank Collaborative, G., International Steering, C., International Co-ordinating Centre, O., National Co-ordinating Centre, B., Regional Co-ordinating, C., Causal associations of blood lipids with risk of ischemic stroke and intracerebral hemorrhage in Chinese adults. Nat. Med. 25(4), 569–574 (2019). https://doi.org/10.1038/s41591-019-0366-x
K.C. Sung, J.H. Huh, S. Ryu, J.Y. Lee, E. Scorletti, C.D. Byrne, J.Y. Kim, D.S. Hyun, S.B. Ko, Low levels of low-density lipoprotein cholesterol and mortality outcomes in non-statin users. J. Clin. Med. 8(10) (2019). https://doi.org/10.3390/jcm8101571
X. Zhang, J. Liu, M. Wang, Y. Qi, J. Sun, J. Liu, Y. Wang, Y. Hao, Y. Li, M. Zhou, D. Zhao, Twenty-year epidemiologic study on LDL-C levels in relation to the risks of atherosclerotic event, hemorrhagic stroke, and cancer death among young and middle-aged population in China. J. Clin. Lipidol. 12(5), 1179–1189.e1174 (2018). https://doi.org/10.1016/j.jacl.2018.06.011
C.D.L. Johannesen, A. Langsted, M.B. Mortensen, B.G. Nordestgaard, Association between low density lipoprotein and all cause and cause specific mortality in Denmark: prospective cohort study. Bmj 371, m4266 (2020). https://doi.org/10.1136/bmj.m4266
P.C. Austin, The performance of different propensity-score methods for estimating differences in proportions (risk differences or absolute risk reductions) in observational studies. Stat. Med. 29(20), 2137–2148 (2010). https://doi.org/10.1002/sim.3854
P.C. Austin, An Introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar. Behav. Res. 46(3), 399–424 (2011). https://doi.org/10.1080/00273171.2011.568786
J.B. Wang, Q.C. Huang, S.C. Hu, P.W. Zheng, P. Shen, D. Li, H.C. Lu, X. Gao, H.B. Lin, K. Chen, Baseline and longitudinal change in blood pressure and mortality in a Chinese cohort. J. Epidemiol. Community Health 72(12), 1083–1090 (2018). https://doi.org/10.1136/jech-2018-211050
D.F. McCaffrey, B.A. Griffin, D. Almirall, M.E. Slaughter, R. Ramchand, L.F. Burgette, A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat. Med. 32(19), 3388–3414 (2013). https://doi.org/10.1002/sim.5753
T. Lumley, Survey: analysis of complex survey samples. (2020). http://cran.fhcrc.org/web/packages/survey/survey.pdf
E.P. Martens, A. de Boer, W.R. Pestman, S.V. Belitser, B.H. Stricker, O.H. Klungel, Comparing treatment effects after adjustment with multivariable Cox proportional hazards regression and propensity score methods. Pharmacoepidemiol. Drug Saf. 17(1), 1–8 (2008). https://doi.org/10.1002/pds.1520
S.M. Jeong, S. Choi, K. Kim, S.M. Kim, G. Lee, J.S. Son, J.M. Yun, S.M. Park, Association of change in total cholesterol level with mortality: a population-based study. PLoS ONE 13(4), e0196030 (2018). https://doi.org/10.1371/journal.pone.0196030
X. Wang, Y. Dong, X. Qi, C. Huang, L. Hou, Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke 44(7), 1833–1839 (2013). https://doi.org/10.1161/STROKEAHA.113.001326
X. Gu, Y. Li, S. Chen, X. Yang, F. Liu, Y. Li, J. Li, J. Cao, X. Liu, J. Chen, C. Shen, L. Yu, J. Huang, T.H. Lam, X. Fang, Y. He, X. Zhang, X. Lu, S. Wu, D. Gu, Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke 50(12), 3376–3384 (2019). https://doi.org/10.1161/STROKEAHA.119.026402
M. Wu, X.H. Zhou, B. Ruozha, S.F. Song, Y.D. Li, J.H. Zhang, Q. Xing, Y.M. Lu, B.P. Tang, The relationship between LDL-C and ischemic stroke in 2470 patients with nonvalvular atrial fibrillation in Xinjiang region. Zhonghua Nei Ke Za Zhi 56(4), 258–262 (2017). https://doi.org/10.3760/cma.j.issn.0578-1426.2017.04.004
S. Zhao, Y. Tian, H. Yan, B. Zhang, J. Li, L. Xing, L. Liu, Association between low-density lipoprotein cholesterol (LDL-C) level and unfavorable outcomes in participants of ischemic stroke without diabetes: a multi-center retrospective study. Med. Sci. Monit. 25, 5934–5941 (2019). https://doi.org/10.12659/MSM.917798
R. Han, Plasma lipoproteins are important components of the immune system. Microbiol. Immunol. 54(4), 246–253 (2010). https://doi.org/10.1111/j.1348-0421.2010.00203.x
U. Ravnskov, K.S. McCully, Review and Hypothesis: Vulnerable plaque formation from obstruction of Vasa vasorum by homocysteinylated and oxidized lipoprotein aggregates complexed with microbial remnants and LDL autoantibodies. Ann. Clin. Lab. Sci. 39(1), 3–16 (2009)
L.A. David, C.F. Maurice, R.N. Carmody, D.B. Gootenberg, J.E. Button, B.E. Wolfe, A.V. Ling, A.S. Devlin, Y. Varma, M.A. Fischbach, S.B. Biddinger, R.J. Dutton, P.J. Turnbaugh, Diet rapidly and reproducibly alters the human gut microbiome. Nature 505(7484), 559–563 (2014). https://doi.org/10.1038/nature12820
S. Devkota, Y. Wang, M.W. Musch, V. Leone, H. Fehlner-Peach, A. Nadimpalli, D.A. Antonopoulos, B. Jabri, E.B. Chang, Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10-/- mice. Nature 487(7405), 104–108 (2012). https://doi.org/10.1038/nature11225
M. Mueller, A. Thorell, T. Claudel, P. Jha, H. Koefeler, C. Lackner, B. Hoesel, G. Fauler, T. Stojakovic, C. Einarsson, H.U. Marschall, M. Trauner, Ursodeoxycholic acid exerts farnesoid X receptor-antagonistic effects on bile acid and lipid metabolism in morbid obesity. J. Hepatol. 62(6), 1398–1404 (2015). https://doi.org/10.1016/j.jhep.2014.12.034
Z. Wang, E. Klipfell, B.J. Bennett, R. Koeth, B.S. Levison, B. Dugar, A.E. Feldstein, E.B. Britt, X. Fu, Y.M. Chung, Y. Wu, P. Schauer, J.D. Smith, H. Allayee, W.H. Tang, J.A. DiDonato, A.J. Lusis, S.L. Hazen, Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472(7341), 57–63 (2011). https://doi.org/10.1038/nature09922
S.M. Grundy, N.J. Stone, A.L. Bailey, C. Beam, K.K. Birtcher, R.S. Blumenthal, L.T. Braun, S. de Ferranti, J. Faiella-Tommasino, D.E. Forman, R. Goldberg, P.A. Heidenreich, M.A. Hlatky, D.W. Jones, D. Lloyd-Jones, N. Lopez-Pajares, C.E. Ndumele, C.E. Orringer, C.A. Peralta, J.J. Saseen, S.C. Smith Jr, L. Sperling, S.S. Virani, J. Yeboah, 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139(25), e1082–e1143 (2019). https://doi.org/10.1161/CIR.0000000000000625
R.R. Sankatsing, S.W. Fouchier, S. de Haan, B.A. Hutten, E. de Groot, J.J. Kastelein, E.S. Stroes, Hepatic and cardiovascular consequences of familial hypobetalipoproteinemia. Arterioscler. Thromb. Vasc. Biol. 25(9), 1979–1984 (2005). https://doi.org/10.1161/01.ATV.0000176191.64314.07
Funding
This research was supported by Natural Science Foundation of Zhejiang Province, China under Grant No. LY16H260002; and Research Center for Air Pollution and Health, Zhejiang University (519600-I21502). The funder had no role in decision to publish, content of this article or preparation of the article.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The author declares no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lu, JM., Wu, MY., Yang, ZM. et al. Low LDL-C levels are associated with risk of mortality in a Chinese cohort study. Endocrine 73, 563–572 (2021). https://doi.org/10.1007/s12020-021-02746-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-021-02746-6