Abstract
Thyroid nodules are very common all over the world, and China is no exception. Ultrasound plays an important role in determining the risk stratification of thyroid nodules, which is critical for clinical management of thyroid nodules. For the past few years, many versions of TIRADS (Thyroid Imaging Reporting and Data System) have been put forward by several institutions with the aim to identify whether nodules require fine-needle biopsy or ultrasound follow-up. However, no version of TIRADS has been widely adopted worldwide till date. In China, as many as ten versions of TIRADS have been used in different hospitals nationwide, causing a lot of confusion. With the support of the Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of the Chinese Medical Association, the Chinese-TIRADS that is in line with China’s national conditions and medical status was established based on literature review, expert consensus, and multicenter data provided by the Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As a highly prevalent disease, thyroid nodules can be detected by ultrasound among 19–68% of the general population, and majority of these were benign nodules without any clinical significance [1, 2]. The prevalence of thyroid nodules detected by ultrasound in China is about 20–35% [3,4,5,6]. Of all the patients with thyroid nodules, 7–15% are malignant based on their age, gender, radiation history, family history, and other factors [2]. Ultrasound is the best imaging method for thyroid, and plays an important role in the diagnosis and management of thyroid nodules.
However, there are often some inconsistencies in terms of reporting terminology or management recommendations due to subjective interpretation of medical images. In view of this, the American College of Radiology (ACR) has published the Breast Imaging Reporting and Data System (BIRADS) in 1992, which developed a standardized image lexicon, standardized the risk stratification of the breast lesions, and proposed corresponding management recommendations [7]. BIRADS has been widely recognized and applied in clinical practice worldwide. Inspired by the ACR BIRADS, Chilean scholars have initially tried to set up Thyroid Imaging Reporting and Data System (TIRADS) that is specific to thyroid nodules [8]. Subsequently, researchers from South Korea [9, 10], France [11], Germany [12], American [13], and Thailand [14] have established various versions of TIRADS. In China, TIRADS has also been established in Shanghai Ruijin Hospital based on single center study [15]. In May 2016, the K-TIRADS (Korean-TIRADS) was jointly published by the Korean Society of Radiology and the Korean Society of Thyroid Radiology, which was the first TIRADS published with the name of Academic Society in the world [16]. In August 2017, the European Thyroid Association released the European version of TIRADS, and named it as the Eu-TIRADS [17].
ACR, being a pioneer in the concept of RADS, did not officially publish the ACR-TIRADS lexicon until 2015 [18] and the TIRADS classification system until 2017 [19], while the Chilean scholars have published the TIRADS 8 years back, i.e., in 2009. Due to delayed publication of the ACR version of the TIRADS, and the mismatch between the classification system and the current medical situation in China, the TIRADS application is very confusing in China. Furthermore, owing to the adoption of varied classification systems by different hospitals, it not only brought great difficulties for ultrasound radiologists and clinicians in the interpretation of the thyroid ultrasound reports, but also confused many patients as to which management to choose. To change this situation, the Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of the Chinese Medical Association in 2017 has put forward the idea of establishing Chinese-TIRADS (C-TIRADS) that is specific to China’s national conditions and medical conditions, and organized an expert panel to perform relevant preliminary preparations. Two questionnaires for thyroid disease-related doctors were carried out in order to get a sense of the current situation: in August 2018, the expert panel conducted a questionnaire survey on TIRADS nationwide; in May 2019, the expert panel conducted a national questionnaire survey on thyroid fine-needle aspiration (FNA). This is because TIRADS involves the choice of clinical management protocols for thyroid nodules, in which FNA plays a vital role. Both surveys were designed with the help of statisticians and were conducted through WeChat, China’s largest social software, where participating doctors, from all 31 provincial administrative regions in mainland China, filled out and submitted their answers via the WeChat client. The expert panel analyzed the current versions of TIRADS risk stratification and non-TIRADS risk stratification (e.g., ATA and AACE/ACE/AME guidelines [2, 20]) and agreed with many studies that there is no absolute perfect risk stratification system and that each one has specific strengths and limitations [21,22,23,24,25,26,27,28,29]. The regression equation method, the weighting method, the counting method, and the pattern-based method have been used to establish different versions of TIRADS [8,9,10, 15, 17]. The expert panel was acutely aware that a complex and time-consuming stratification system cannot really be applied to clinical routines, no matter how accurate it is. On the premise of balancing the accuracy and ease of use of risk stratification, the expert panel tended to use the counting method to establish C-TIRADS, because this method was easy for clinical application and promotion.
Based on the above situation and the results of the questionnaire survey (see below), the expert panel proceeded to develop the C-TIRADS suitable for Chinese clinical practice by using the Chinese thyroid ultrasound database. In the process, the expert panel referred to the current versions of TIRADS risk stratification and non-TIRADS risk stratification, as well as to the latest domestic and international literature. The national conditions of China have also been fully considered.
According to the evidence-based clinical imaging guidelines [30], the recommendations of the C-TIRADS were graded according to the level of evidence as grade A (recommended), grade B (conditional recommended), grade C (not recommended), and grade I (no recommendation): grade A, intervention or examination has sufficient evidence to support desired effect; grade B, intervention or examination has moderate to sufficient evidence to support the desired effect; grade C, intervention or examination has sufficient evidence to support an undesired effect; and grade I, intervention or examination does not have sufficient evidence to either support or reject effectiveness [30].
Part I: Role of ultrasound in the diagnosis and management of thyroid nodules
A thyroid nodule is a lesion of the thyroid gland that can be distinguished from thyroid tissue by ultrasound or other imaging modalities.
Value of ultrasound in evaluating thyroid nodules
Ultrasound is the most important imaging method for evaluating thyroid nodules [2, 16, 17, 19], and it assists in determining whether the nodule is solitary or multiple, as well as the size, the morphological characteristics and the blood supply of the nodule. Ultrasound can be applied to determine the risk of malignancy of thyroid nodules by assessing the morphological characteristics, and sometimes by combining with the blood supply characteristics. At times, ultrasound elastography (UE) and contrast-enhanced ultrasound (CEUS) also have certain value in evaluating the nodules, but only under the preconditions of combining with morphological characteristics of nodules [31,32,33,34]. The evaluation of cervical lymph nodes is helpful in determining the nature of thyroid nodules [2, 35]. In addition, ultrasound can accurately demonstrate the spatial location of nodules in the thyroid gland, the relationship between nodules and the thyroid capsule, as well as the relationship between nodules and the surrounding important structures such as blood vessels and nerves. All these are essential for the formulation of surgical resection or thermal ablation treatment strategies. Moreover, for patients who are planning to undergo thyroid cancer surgery, ultrasound examination must be performed before surgery to assess whether there are abnormal cervical lymph nodes [2]. Preoperative ultrasound evaluation can optimize surgical treatment, change surgical procedures, facilitate the complete removal of lesions and reduce recurrence [36, 37]. For postoperative patients with thyroid cancer, ultrasound also plays an important role in follow-up [35].
Ultrasound-guided fine-needle aspiration biopsy of thyroid nodules
According to the ultrasound features and size of nodules, as well as clinical context, whether ultrasound-guided FNA is required can be determined. FNA is generally required for determining the next management strategy for suspicious nodules that reach the corresponding size threshold [2, 16, 17, 19, 38]. Ultrasound-guided FNA is the most accurate and cost-effective method for evaluating thyroid nodules [2, 39, 40]. However, the successful application of FNA requires not only mastering technical skills but also a comprehensive understanding of the limitations, the indications, and the factors that affect the acquisition of adequate specimens [41]. For example, attention should be paid regarding the potential value of the combined use of conventional smear and liquid-based preparation [42, 43]. Ultrasound-guided FNA can also be used to diagnose suspicious lesions in thyroid bed and other regions of the neck of the postoperative patients with thyroid cancer [35].
Ultrasound and overdiagnosis and overtreatment of papillary thyroid microcarcinoma (PTMC)
In recent years, the incidence of thyroid cancer has been dramatically increased, among which PTMC of <10 mm diameter is the main type. However, the mortality rate related to thyroid cancer showed no significant change. Therefore, the problem of overdiagnosis and overtreatment of PTMC due to extensive application of imaging methods, mainly ultrasound, has attracted wide attention [44,45,46,47,48]. Of course, besides the factors of overdiagnosis, changes in environmental risks, radiation, obesity, and other undefined factors also contributed to a real increase of thyroid cancer incidence [49, 50].
The mortality rate of thyroid cancer remained relatively low, with only 0.2–0.3/100,000 in developed countries [50]. Most of the PTMCs demonstrated mild biological behavior, and patients may not have clinical manifestations for a lifetime. Therefore, there is a growing support for the use of active surveillance strategies for low-risk PTMCs (which are cytologically suggestive of non-highly invasive, nonadjacent to the trachea or recurrent laryngeal nerve, and without any evidence of cervical lymph node metastasis and systemic metastasis) rather than traditional surgical resection [2, 51,52,53,54,55,56].
Role and problems associated with ultrasound and FNA in diagnosing and managing thyroid nodules in China
Similar to the situation abroad, the incidence of thyroid cancer in China is steadily increasing, especially PTMC [57, 58]. However, different from the developed countries, the application of thyroid nodule FNA is not yet widespread in China, and there are therefore many differences exist in the process of diagnosis and management of thyroid nodules between China and developed countries. In terms of standardization of diagnosis and management, China still needs to be in line with the international standards. In May 2019, a nationwide questionnaire survey on thyroid FNA was conducted by the expert panel, wherein 5044 questionnaires were collected from the physicians, surgeons, ultrasound radiologists, nuclear medicine doctors, radiologists, and pathologists from all levels of hospitals in all provinces, autonomous regions, and municipalities that are directly under the Central Government of China, including Tibet. The results showed that only 52.0% of the doctors from the tertiary hospitals (with the highest medical level) interviewed and 12.9% of the doctors from the non-tertiary hospitals interviewed mentioned that thyroid FNA is widely carried out in their hospitals. Of the 845 surgeons interviewed, 70.4% reported that less than half of their patients underwent thyroid FNA before surgery. Therefore, many thyroid surgeries in China were based on only ultrasound findings or other relevant clinical evidence instead of FNA results.
Among the 1124 thyroid physicians and surgeons interviewed, 82.3% believed that there was over-operation of benign thyroid nodules, and 58.6% believed that there was over-operation of PTMCs in China.
However, there are still many difficulties that change the current situation regarding the diagnosis and management of thyroid nodules in China. For example, cultural tradition, patients’ preference, population mobility, and medical liability concerns can all impact the implementation of active surveillance strategy for low-risk PTMCs [52]. In particular, the self-financing medical system of public hospitals and cultural tradition under which common people get jittery by mentioning cancer are real problems that need to be addressed in China.
Recommendation
R1: Ultrasound is the best imaging method to determine the risk of malignancy of thyroid nodules (Grade A).
R2: FNA is an important procedure in the evaluation of thyroid nodules with indications (Grade A).
R3: The application of thyroid nodule FNA is not widespread in China (Grade B).
R4: Attention should be paid to the problem of overdiagnosis and overtreatment of PTMC due to extensive application of ultrasound (Grade A).
Part II: C-TIRADS
In August 2018, a nationwide questionnaire survey on TIRADS was conducted, wherein 6395 responses were collected from physicians, surgeons, ultrasound radiologists, nuclear medicine doctors, radiologists and pathologists from all administrative regions of mainland China, including Tibet. The results revealed that there are almost ten different versions of TIRADS used in different hospitals nationwide, which caused huge discrepancies. Meanwhile, 82.6% of the interviewed doctors agreed that the ultrasound risk stratification of thyroid nodules is necessary. If risk stratification is to be established, 82.1% of the interviewed doctors hoped to follow the ACR-BIRADS classification model to establish TIRADS as well as 89.2% of the interviewed doctors hoped to establish C-TIRADS adapted to the current situation in China.
The classical TIRADS, especially the “academic society” version of the TIRADS, provided complete lexicon to describe the ultrasound features of thyroid nodules, classification system to determine the malignant risk of nodules and management recommendations on whether nodules require FNA or not [16,17,18,19]. It should be noted that the management recommendations of all versions of TIRADS did not contain any provisions for determining whether a nodule needs surgical treatment or not. This is due to the fact that FNA is usually required before thyroid nodule surgery in accordance with the internationally accepted principles [59]. For this reason, the risk of malignancy for ACR-TIRADS category 5 nodules is >20% only, and that of Eu-TIRADS category 5 is >26% only. However, as mentioned above, currently thyroid FNA is not widely carried out in China and surgical treatment decisions are usually based on ultrasound findings of nodules rather than FNA results. The difference in the diagnosis and treatment process of thyroid nodules between China and developed countries makes it difficult for many doctors to accept the risk stratification system of ACR-TIRADS or Eu-TIRADS in China.
Based on the above situation, the expert panel, after careful assessment, believed that it is necessary to establish C-TIRADS that is in line with the China’s national conditions. This system should be established according to the following principles: (1) applicable to all thyroid nodules as much as possible; (2) taking into account the accuracy and ease of use; (3) adapt to the current process of diagnosis and management of thyroid nodules in China; (4) adapt to the Chinese cultural traditions and patient preference; (5) gradually reduce the overtreatment of benign thyroid nodules as well as PTMCs.
Image-quality control of thyroid ultrasound
The quality of ultrasound images is a key factor in detecting thyroid nodules and determining the risk stratification of nodules. The image quality depends on the performance of the ultrasound systems, proper adjustment of the imaging parameters, and the scanning skills of the ultrasound radiologists or sonographers.
Ultrasound systems
Thyroid gland is superficially located in the neck, and the diameter of thyroid nodules can be as small as a few millimeters. Therefore, it is necessary to use a medium or high-grade high-resolution ultrasound system equipped with high-frequency wide-band linear array probe with a frequency range of 7–18 MHz. The frequency can be flexibly adjusted according to the depth and the degree of enlargement of the thyroid. In a few cases, such as those with very enlarged thyroid, retrosternal goiter, a convex array probe with a relatively low frequency can be used.
Scanning method and imaging parameter adjustment
The patient is placed in supine position with a pillow at the back of the neck. The neck is overstretched to fully expose the anterior cervical region. When scanning one side of the lobe, the patient’s head can be turned to the opposite side to facilitate scanning. Both lobes and isthmus of thyroid should be fully scanned on both transverse and longitudinal sections, and the pyramidal lobe should not be omitted. Transverse and longitudinal scanning of thyroid bed is required for patients who have underwent unilateral or bilateral thyroidectomy [60].
As an important part of thyroid ultrasound, cervical lymph node scanning should be performed based on the lymph node level classification system of AJCC [61], focusing on the lymph nodes in levels VI, III, and IV. If necessary, lymph nodes in levels I, II, V, and VII also should be assessed. However, ultrasound scanning of the level VII lymph nodes is often technically difficult, and CT or MRI is more appropriate.
Gray-scale ultrasound is the most basic and important method of thyroid ultrasound imaging, and color/power Doppler is a common component of thyroid ultrasound. In order to obtain higher resolution images of the anatomical structure and blood flow, the position of the ultrasound probe and the angle of incidence of the ultrasound need to be adjusted to make the thyroid tissue as close to the probe as possible to facilitate the use of higher-frequency ultrasound. UE and CEUS can be adopted selectively. The scanning techniques and imaging parameters should be adjusted for different ultrasound imaging modalities according to different ultrasound systems and patient conditions [62].
Gray-scale ultrasound
The optimal imaging quality of thyroid nodules could be achieved by adjusting probe frequency, focus number and position, gain, time gain compensation (TGC) curve, imaging depth and width, etc.
Color/power Doppler ultrasound
Settings such as flow velocity scale, gain, and wall filter should be adjusted whenever necessary. The velocity scale is usually set to 1–5 cm/s according to different ultrasound systems. All settings are standardized for the highest sensitivity in the absence of apparent noise. The probe is in full contact with the skin, but no pressure is applied as much as possible to avoid compressing the small blood vessels and affecting the blood flow display [63].
Ultrasound elastography (UE)
The ultrasound probe should touch the skin of the neck lightly, and try to keep it perpendicular to the skin. When acquiring elastic data, the patients are asked to hold breath for a few seconds if breathing causes significant neck movement. In two-dimensional elastography, the location and size of the region of interest (ROI) should be adjusted to include the target nodule as well as the thyroid tissue around the nodule. The details are as follows: in strain elastography (SE), the pressure and frequency of compression are adjusted to meet the preset requirements of the elastography system; in shear-wave elastography (SWE), the stable SWE images of the nodules without artifactual stiffness are selected and stored, which is under the premise of with no pressure induced by the probe. In point shear-wave elastography, the ROI is placed in the target area of the nodule with no pressure induced by the probe [31, 32].
Contrast-enhanced ultrasound (CEUS)
In order to obtain the best quality of the image, the mechanical index (MI) should be adjusted to <0.3, and the frequency, the position of focus, gain, TGC curve, imaging depth, and imaging width were adjusted at the same time [64]. To obtain better perfusion signal of microcirculation, apply as little pressure as possible while ensuring full contact between the probe and the skin.
Recommendation
R5: Image-quality control of ultrasound is critical for detecting thyroid nodules and determining the risk stratification of thyroid nodules (Grade B).
Ultrasound lexicon of thyroid nodules
For developing the C-TIRADS lexicon, the expert panel referred to the lexicon provided by various versions of TIRADS and non-TIRADS risk stratification, as well as the terminology provided by the extensive thyroid ultrasound literatures since the 1990s, which involved gray-scale ultrasound, color/power Doppler ultrasound, and UE and CEUS of thyroid nodules. The literature was searched using the PubMed, Embase, Web of Knowledge, and Google Scholar search engines. Three experts of the expert panel listed the ultrasound terms used in the literature to describe thyroid nodules, which were then submitted to all experts of the expert panel to determine which terms were included in the lexicon using the principle of consensus.
It should be emphasized that despite the terms of color Doppler, UE and CEUS are included in lexicon as these imaging techniques have gradually become the basic functional components of modern ultrasound instruments, the expert panel does not consider it appropriate to include these techniques in the risk stratification system of thyroid nodules at present due to the unsatisfactory reproducibility, the instrument dependence, and the operator dependence, as well as the limited value in predicting malignancy of these techniques [2, 20, 63, 65, 66].
In addition, observer variabilities of TIRADS regarding the interpretation of ultrasound features or FNA recommendation are receiving increasing attention [67,68,69]. Experienced and less experienced radiologists may have different interpretations of thyroid nodule ultrasound features and therefore requires a continuous and specialized training for residents to improve the agreement and performance thyroid ultrasound in residents [70, 71].
Gray-scale ultrasound
Location
The spatial distribution of nodules in the thyroid is regarded as the location. Each lobe of the thyroid gland is divided into three regions: upper, middle, and lower. Together with isthmus, the thyroid includes seven regions [72,73,74].
Significance: The ultrasound features of nodules can be affected by their locations. For example, papillary thyroid carcinoma (PTC) located in the isthmus is usually horizontal and has smooth margins [75]. The location of PTC is also associated with the location of cervical lymph node metastasis and the manner of metastasis [73, 76,77,78,79,80], which may affect the surgical strategy [81, 82]. Location also forms an important basis for determining whether the active surveillance strategy can be used for PTMC [2, 51,52,53,54,55,56]. The relationship between nodal location and the risk of malignancy is uncertain. Different studies have shown that the upper pole nodules, isthmus nodules, and mid-lobar nodules were risk factors for malignancy, respectively [83,84,85].
Orientation
Orientation, equivalent to shape in many literatures, reflects the relationship between the long axis of the nodule and the skin line of the neck. It is suggested to judge orientation on the basis of accurate measurement, but visual evaluation is also acceptable.
-
(1)
Vertical (taller-than-wide): On transverse or longitudinal sections, the long axis of the nodule and skin line tended to be vertical. When measured accurately, the anteroposterior diameter of the nodule is larger than the longitudinal diameter in longitudinal section or the transverse diameter in transverse section.
-
(2)
Horizontal (wider-than-tall): On both transverse and longitudinal sections, the long axis of the nodule and skin line tended to be parallel. When measured accurately, the anteroposterior diameter of nodule is less than/equal to the longitudinal diameter in longitudinal section or the transverse diameter in transverse section.
Significance: It is not uniform to choose which section to evaluate the nodule orientation. Some studies were evaluated based on transverse section [10, 86], while others are not limited to transverse or longitudinal section [87, 88]. Vertical orientation in either transverse or longitudinal section had better accuracy and sensitivity for predicting malignancy than that in single section [89]. However, horizontal orientation can also be seen in malignant nodules at times, especially the follicular thyroid carcinoma or the follicular variant of PTC [16, 65, 86, 87, 89,90,91,92].
Margin
The margin is referred to as the border or edge of the nodule, which can be classified according to the degree of clarity and regularity.
-
(1)
Circumscribed: The margin appears as clear, smooth, and complete curve.
-
(2)
Irregular margin: The margin is spiculated, angular, or microlobulated.
-
(3)
Ill-defined: The margin of the nodule is difficult to distinguish from the surrounding thyroid parenchyma.
-
(4)
Extrathyroidal extension: The nodule spreads to the thyroid capsule, which can lead to disruption of capsular and, in severe cases, invasion of the adjacent soft tissue and/or vascular structures [18, 93].
Significance: It is sometimes more difficult to tell if extrathyroidal extension (e.g., disruption of capsular) is present, especially when the image quality is poor. It is generally believed that the circumscribed margin is a benign feature, while irregular margin and/or extrathyroidal extension are malignant manifestations. However, different reports have varied results based on the meaning of ill-defined margin [9, 21, 65, 94,95,96,97,98].
Halo
Halo is defined as a hypoechoic or anechoic rim that encircles the nodule.
(1) Present halo
According to the thickness of the halo, the halo is divided into thin halo and thick halo. Furthermore, the halo is divided into even thickness halo and uneven thickness halo based on the homogeneity of the halo thickness.
(2) Absent halo
Significance: At present, there is no uniform standard for distinguishing thick halo and thin halo. Some studies used 2 mm as the threshold [99,100,101], while others used 1 mm as the threshold [102]. A study suggested that thin halo is considered as an important sign of benign nodules, while malignant nodules often lacked halo or have thick halo [17]. The halo of PTC often shows uneven thickness [100]. However, there are different opinions regarding the diagnostic value of halo [9, 15,16,17,18, 20, 65, 74, 97, 99, 100, 103,104,105].
Composition
The distribution of solid and cystic components in nodules.
-
(1)
Solid: The nodule is entirely composed of solid tissue, without any cystic components.
-
(2)
Predominately solid: solid components accounted for more than 50% of the nodules.
-
(3)
Predominately cystic: solid components accounted for <50% of the nodules.
-
(4)
Cystic: The nodules are completely or almost completely cystic with thin wall, and there might be thin internal septa or debris.
-
(5)
Spongiform: multiple tiny cystic spaces occupy the entire nodules without aggregated solid tissues.
Significance: Solid components are regarded as suspicious ultrasound feature. The malignant probability of mixed cystic and solid nodules, that is, predominately solid nodules or predominately cystic nodules, is lower than that of solid nodules. Cystic or spongiform nodules are generally considered benign [10, 17, 18, 21, 23, 74, 97].
Echogenicity
The echogenicity level of the solid components of nodules is defined by comparison with the echogenicity of the thyroid parenchyma and the strap muscles of the neck.
-
(1)
Hyperechoic: The echogenicity is higher than that of the surrounding thyroid parenchyma.
-
(2)
Isoechoic: The echogenicity is similar to that of the surrounding thyroid parenchyma.
-
(3)
Hypoechoic: The echogenicity is lower than that of the surrounding thyroid parenchyma.
-
(4)
Markedly hypoechoic: The echogenicity is lower than that of the strap muscles of the neck.
-
(5)
Anechoic: seen in cystic nodules, usually accompanied by posterior enhancement.
Significance: In the case of Hashimoto’s thyroiditis and other conditions that cause changes in the echogenicity of the thyroid parenchyma, the echogenicity level of the solid components of nodules should still be described relative to the thyroid parenchyma. However, the changes in the echogenicity of thyroid parenchyma should be described in the report [18]. It should be noted that when the echogenicity of nodule is lower than that of the thyroid parenchyma but similar to that of the strap muscles, the nodule is still defined as hypoechoic rather than markedly hypoechoic. It is generally believed that hypoechoic or markedly hypoechoic are suspicious ultrasound features. If hypoechoic is used as the diagnostic criteria, the diagnosis is more sensitive, but less specific. If markedly hypoechoic is used as the diagnostic criteria, the diagnosis is less sensitive but more specific [9, 16,17,18, 20, 23, 65, 74, 94].
Echotexture
The consistency and diversity of the echoes in the solid components of the nodules.
-
(1)
Homogeneous: The solid components of the nodules are consistent in echogenicity.
-
(2)
Heterogeneous: The solid components of the nodules are diverse in echogenicity.
Significance: The echotexture has limited value in the diagnosis of benign and malignant nodules [9, 17, 20, 74, 106]. In a study involving 1694 nodules, Park et al. [9] found that malignant nodules tended to manifest homogeneous echoes. However, another study involving 849 nodules was carried out by Moon et al. [94], which indicated that both benign and malignant nodules tended to show heterogeneous echoes, and no statistical difference between the two was observed.
Echogenic foci
One or more of the following echogenic foci might be observed in the same nodule.
-
(1)
Microcalcifications: punctate echogenic foci of less than about 1 mm with or without shadowing.
-
(2)
Comet-tail artifacts: A comet-tail artifact is mostly caused by dense colloid material and occurred in either the cystic or the solid regions of the nodules. It usually appears as punctate echogenic foci with a dense tapering trail of echoes in the rear, and is believed to be a special form of reverberation artifact.
-
(3)
Punctate echogenic foci of undetermined significance: punctate echogenic foci are <1 mm without shadowing and comet-tail artifact, which make it difficult to tell whether they are microcalcifications or dense colloid materials, or other components.
-
(4)
Macrocalcifications: echogenic foci that are larger than 1 mm, usually accompanied by posterior shadowing.
-
(5)
Peripheral calcifications: echogenic foci are located at the periphery of the nodules, and might appear as a continuous or discontinuous ring or arc involving more than a third of the margin.
-
(6)
No echogenic foci.
Significance: Several studies have revealed that all types of calcifications detected by ultrasound increase the probability of malignancy [16,17,18,19,20, 65, 107, 108]. The comet-tail artifacts may represent dense colloids, fibrin debris and microcalcifications, and so on. The presence of comet-tail artifacts in a cystic nodule is highly suggestive of benign nodules, but it cannot be used to rule out malignancy if present in the solid components [16,17,18, 107, 109,110,111,112,113,114]. It should be noted that the punctate echogenic foci do not necessarily represent the psammoma bodies that are most commonly observed in PTC. Punctate echogenic foci may also refer to dystrophic calcifications or dense colloid microdeposits. Although ultrasound radiologists can empirically determine whether the punctate echogenic foci are microcalcifications or dense colloid materials, it must be admitted that the judgment is subjective. It remained difficult to judge the nature of the punctate echogenic foci in many cases.
Posterior features
The change of the echo level behind the nodule reflects the acoustic attenuation characteristics of the nodule.
-
(1)
Enhancement: The echo behind the nodule is higher than that of the surrounding tissue at the same depth.
-
(2)
Shadowing: The echo behind the nodule is lower than that of the surrounding tissue at the same depth.
-
(3)
No posterior features: The echo behind the nodules is similar to that of the surrounding tissues at the same depth.
-
(4)
Combined pattern: The echo behind the nodules is a combination of the above patterns.
Significance: There are few studies on the posterior acoustic features of the thyroid nodules. Compared with benign nodules, malignant nodules have a higher rate of posterior shadowing, but lymphoma often shows posterior enhancement [15, 115,116,117,118,119].
Size
The anteroposterior diameter, the transverse diameter, and the longitudinal diameter of the nodules are measured on the transverse and longitudinal sections. The measured value should be accurate to 0.1 mm. If that nodule appears with a halo, the nodule measurement should include the halo [99]. The maximum size should involve the longest axis of the nodule, and the next measurement should be perpendicular to the previous measurement [19].
Significance: It should be pointed out that the measurement accuracy depends on the equipment and probe used. Furthermore, considerable intraobserver and interobserver variability in nodule size measurement was described in literature [120]. It is generally accepted that the size of the nodules do not help to predict or exclude malignant lesions. However, the size of the nodules is important for determining whether the biopsy is required or not. Moreover, size is also an important indicator for evaluation during follow-up [2, 16,17,18,19,20, 59]. The increase in size was defined as more than a 20% increase in at least two nodule dimensions, or more than a 50% increase in nodule volume in solid nodule or the solid portion in mixed nodule [121].
Color/power Doppler ultrasound
According to the spatial distribution of vessels in the nodule, the vessels of the nodule are divided into peripheral vessels and central vessels. The vascular pattern of the nodules is divided into five types according to the presence and combination of the peripheral and central vessels.
-
(1)
Avascularity: no blood flow signal is observed in the nodule.
-
(2)
Peripheral vascularity: only peripheral vessels are observed in the nodule, and no central vessels are present.
-
(3)
Mainly peripheral vascularity: The nodule vascularity is dominated by the presence of peripheral vessels with few central vessels.
-
(4)
Mainly central vascularity: The nodule vascularity is dominated by the presence of central vessels with few peripheral vessels.
-
(5)
Mixed vascularity: The abundance of both central and peripheral vessels in the nodules is similar.
Significance: There are many studies on the vascular pattern of the nodules by Doppler ultrasound, but they come to different conclusions [16, 17, 20, 66, 74, 97, 122,123,124,125]. Therefore, the value of Doppler ultrasound in differential diagnosis of benign and malignant nodules remained controversial [65, 66].
Ultrasound elastography (UE)
For assessing nodule malignancy, the stiffness of thyroid nodules that is evaluated by UE must be combined with morphological characteristics provided by conventional ultrasound.
-
(1)
Soft
-
(2)
Intermediate
-
(3)
Hard
Significance: The malignant nodules tend to be hard, while benign nodules tend to be soft. UE has certain value in evaluating thyroid nodules, but the results of it are controversial [126, 127]. SE uses the scoring system or the strain ratio to determine the stiffness of the nodules. However, the scoring method has not been unified, and the strain ratio is affected by the algorithm of different UE systems. As a result, the measured values of different UE systems cannot be referred to each other. Similarly in SWE, the shear-wave velocity or Young’s modulus measured by different ultrasound systems is quite different, and therefore these values cannot be referred to each other [17, 31, 32, 126,127,128].
Contrast-enhanced ultrasound (CEUS)
CEUS has great significance value in the diagnosis of collapsing benign cystic or predominantly cystic thyroid nodules. But it would be better if a comprehensive judgment combined with clinical history can be made.
-
(1)
No enhancement: There is no enhancement in the whole or most of the regions of the nodules.
-
(2)
Scant punctate-linear enhancement: The whole or most of the regions of the nodules show scant punctate-linear enhancement.
-
(3)
Mild enhancement: The enhancement of the nodules is lower than that of the thyroid parenchyma.
-
(4)
Moderate enhancement: The enhancement of the nodule is equivalent to that of the thyroid parenchyma.
-
(5)
High enhancement: The enhancement of the nodule is higher than that of the thyroid parenchyma.
Significance: After absorption of cystic fluid, the cystic or predominantly cystic thyroid nodules often demonstrated ultrasound features similar to those of the PTC in gray-scale ultrasound. In CEUS, no enhancement or scant punctate-linear enhancement in the whole or most areas of the nodules has good specificity, but relatively low sensitivity in determining this type of benign nodules [129,130,131,132].
Recommendation
R6: The ultrasound radiologists should have an accurate grasp of each ultrasound term and its definition (Grade A).
Ultrasound category system and management recommendations for thyroid nodules
This classification system is based on the ultrasound data of Chinese thyroid nodules, and is designed to be simple and easy to use in clinical practice while taking into account the accuracy of risk stratification. The management recommendations fully take into account the actual harm of thyroid cancer to patients and China’s national conditions as well as traditional culture.
Establishment process of C-TIRADS
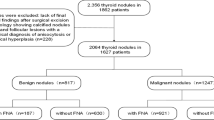
To determine the risk stratification of nodules of C-TIRADS, the expert panel established a multicenter research team based on the Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound [133]. The team included a total of 131 hospitals in all administrative regions of China, except Tibet. The team collected a total of 2141 thyroid nodules as confirmed by surgery and pathology from 2141 patients. Among these, 1572 nodules were benign, 565 nodules were malignant, and 4 nodules were borderline. Based on these 2141 nodules, suspicious ultrasound features were determined by multivariate logistic regression by the collaboration of the ultrasound radiologists and statistics experts of the committee. After that, the prediction models based on the regression equation, weighting, and counting methods were established, respectively, and the area under the receiver operating characteristic curve (Az value) of different models was compared.
C-TIRADS category
Multiple logistic regression analysis revealed that solid composition, microcalcifications, markedly hypoechoic, ill-defined or irregular margins, or extrathyroidal extensions, and vertical orientation as malignant ultrasound features, while comet-tail artifact showed association with benign status. Logistic regression equation yielded the highest Az of 0.913 for predicting malignant thyroid nodules. The Az value for counting method (0.890) was similar to that of the weighting method (0.893) (P = 0.3316) [133].
By taking into account both diagnostic accuracy and clinical ease of use, the counting method was used to establish C-TIRADS, in which the risk stratification was obtained by adding the number of the abovementioned malignant ultrasound features and then subtracting 1 if negative feature of the comet-tail artifacts was present. Table 1 and Figs 1 and 2 showed the C-TIRADS established by the counting method [133].
a C-TIRADS 1: diffusely enlarged thyroid with heterogeneous echotexture, but no nodule was found. Diagnosis: Hashimoto’s thyroiditis; b C-TIRADS 2: predominantly solid nodule (0) with horizontal orientation (0), circumscribed margin (0), hypoechoic (0), with internal comet-tail artifact (−1). The counting value is −1. Diagnosis: follicular adenoma; c C-TIRADS 3: predominantly solid nodule (0) with horizontal orientation (0), circumscribed margin (0), hypoechoic (0), with punctate echogenic foci of undetermined significance in the caudal margin of the nodule (0). The counting value is 0. Diagnosis: nodular goiter; d C-TIRADS 4A: solid nodule (1) with horizontal orientation (0), circumscribed margin (0), hypoechoic (0), no punctate echogenic foci (0). The counting value is 1. Diagnosis: follicular adenoma; e C-TIRADS 4B: solid nodule (1) with horizontal orientation (0), circumscribed margin (0), hypoechoic (0), punctate echogenic foci of undetermined significance combined with microcalcifications (1). The counting value is 2. Diagnosis: papillary thyroid cancinoma; f C-TIRADS 4C: solid nodule (1) with horizontal orientation (0), irregular margin (1), hypoechoic (0), microcalcifications (1). The counting value is 3. Diagnosis: papillary thyroid cancinoma; g C-TIRADS 4C: solid nodule (1) with horizontal orientation (0), irregular margin (1), markedly hypoechoic (1), microcalcifications (1). The counting value is 4. Diagnosis: papillary thyroid cancinoma; h C-TIRADS 5: solid nodule (1) with vertical orientation (1), irregular margin (1), markedly hypoechoic (1), microcalcifications (1). The counting value is 5. Diagnosis: papillary thyroid cancinoma
Notes for classification
Doctor’s personal experience and C-TIRADS category
C-TIRADS based on counting method is recommended according to statistical analysis. It has the advantage of being simple and practical, especially for beginners. However, medical ultrasound highly depends on experience, thus personal experience of ultrasound radiologists cannot be ignored in judging the risk stratification of nodules. Based on the long-term experience of thyroid ultrasound, experienced doctors are allowed to revise the C-TIRADS category obtained by the counting method. In addition, there are inter- or intraobserver variabilities in the interpretation of the ultrasound features of nodules [122, 134]. Therefore, specialized training for less experienced ultrasound radiologists is necessary for the reliability and consistency of the C-TIRADS classification.
Clinical history
-
(1)
As mentioned above, thyroid cystic or predominantly cystic nodules might present a number of suspicious ultrasound features after natural absorption or aspiration of cystic fluid. These nodules may be classified into category 4 or 5 according to the above established model. However, such nodules were classified into category 2 if the history is confirmed, or if the nodules are significantly or progressively smaller than before.
-
(2)
Thyroid nodules lacking spherical shape with ill-defined margins or other suspicious ultrasound features should take into consideration the possibility of subacute thyroiditis, especially in the case of multifocal [135, 136]. However, such nodules might be classified into category 4 or 5 according to the model. In this case, it is necessary to ask the patient whether there is a history of cold or neck pain. If an affirmative response is received, the nodules can be assessed as category 3 or even 2, but short-term follow-up is required; if the history is unclear, the nodules can be assessed as category 4A, and short-term follow-up rather than FNA is required; if the nodules continued to shrink during the follow-up period, the nodules can be classified into category 2; and if the nodule was not detected by ultrasound several months earlier, the nodules can be classified into category 2.
Ultrasound findings of cervical lymph nodes
Ultrasound assessment of cervical lymph nodes, especially in the lateral region, provides important information regarding risk stratification of thyroid nodules. The main suspicious features of cervical lymph node metastasis from PTC were as follows: round shape, microcalcifications, cystic degeneration, focal hyperechoic area, focally or diffusely increased vascularization [2, 35, 62].
-
(1)
If typical cervical metastatic lymph nodes of thyroid cancer and suspicious nodules in the ipsilateral thyroid are found simultaneously by ultrasound, the nodules should be classified into category 5.
-
(2)
If typical cervical metastatic lymph nodes of thyroid cancer are detected by ultrasound, but there are no suspicious nodules in the ipsilateral and contralateral thyroid glands, this might be due to extremely small occult thyroid cancer that cannot be found by ultrasound. In this case, it is necessary to indicate in the report that the cervical metastatic lymph nodes might originate from thyroid cancer to provide reference for clinical management.
Punctate echogenic foci
The punctate echogenic foci can be divided into three types: microcalcifications, comet-tail artifacts, and undetermined significance. When punctate echogenic foci are present in the nodules, microcalcifications are recorded preferentially according to the principle of suspicious feature priority. For example, when the above three types of punctate echogenic foci are present simultaneously in a nodule, then only microcalcifications are recorded, and one point is added in the counting method for determining the C-TIRADS category of the nodule. The comet-tail artifacts are recorded only in the absence of punctate echogenic foci of microcalcifications.
UE and CEUS
The above thyroid nodule classification model is established based on gray-scale ultrasound, which has low requirements for instruments as well as operators, and so it is suitable for wide application in hospitals with various grades. UE and CEUS may have some value in the evaluation of thyroid nodules, but there is no broad consensus at present. No TIRADS incorporates these two imaging techniques into the risk stratification system currently. For example, Eu-TIRADS pointed out that UE cannot be adopted into the TIRADS until multicenter, large-sample studies confirms the reliability and repeatability of UE in distinguishing benign from malignant nodules [17]. The expert panel believed that in some specific cases, the classification of TIRADS based on model can be altered by the results of UE or CEUS.
-
(1)
For solid nodules of 5–30 mm without macrocalcifications, if the nodules are neither deep nor located in the isthmus, the category of nodules can be adjusted as appropriate according to the stiffness of the nodules as reflected by UE [31]. However, the operator dependence of SE should also be considered.
Some category 4 or 5 solid nodules that do not show any enhancement in all or most areas of the nodule on ultrasound should be considered as mummified nodules, i.e., thyroid cystic or cystic changes after absorption of the cystic fluid of the main nodule, thus downgrading the nodule to category 2.
-
(1)
Some solid nodules of category 4 or 5 that do not show any enhancement in the whole or most of the regions of the nodules in CEUS should be considered as mummified thyroid nodules, i.e., the changes of cystic or predominantly cystic nodules after spontaneous absorption of the cystic portion. Consequently, the nodules can be downgraded to category 2. If there is only scant punctate-linear enhancement in the whole or most of the regions of the nodules in CEUS, the nodules can be downgraded to category 3. The larger the nodule, the higher reliability and rationality the above degrading methods is.
Classification of special cases
Cystic and spongiform nodules
Cystic or spongiform nodules are generally benign [10, 17, 18, 21, 23, 74, 97], and therefore are assessed as C-TIRADS 2 (Fig. 3a, b). Attention should be paid to the definition of spongiform nodule, wherein aggregated solid components cannot be present inside the nodules.
a Almost completely cystic with internal debris, C-TIRADS 2. Diagnosis: nodular goiter; b, spongiform nodule, C-TIRADS 2. Diagnosis: nodular goiter; c, white knight nodules of Hashimoto’s thyroiditis, C-TIRADS 2. Diagnosis: Hashimoto’s thyroiditis; d multiple predominantly solid nodules and predominantly cystic nodules of similar ultrasound appearance, C-TIRADS 3. Diagnosis: nodular goiter; e nodules with macrocalcifications causes strong acoustic shadowing that precludes full assessment of internal characteristics, C-TIRADS 4A. Diagnosis: nodular goiter. f nodules with snowstorm pattern of microcalcifications, C-TIRADS 5. Diagnosis: papillary thyroid cancinoma; g incalculable nodule-independent snowstorm-like microcalcifications in the right lobe thyroid. Diagnosis: papillary thyroid cancinoma
Uniform hyperechoic nodule of Hashimoto’s thyroiditis
The so-called “white knight” nodules are referred to uniform hyperechoic nodules that appear on a background of Hashimoto’s thyroiditis, which are generally not more than 15 mm in diameter, and typically <10 mm. The white knight nodules are typically benign and should be assessed as C-TIRADS 2 (Fig. 3c) [137,138,139,140].
Nodular goiter
According to the literature and experts opinion [19, 59], the probability of malignancy is very low when there are multiple predominately solid nodules and/or predominately cystic nodules with similar ultrasound appearance scattered within the thyroid, and the corresponding pathological diagnosis is usually nodular goiter. Therefore, such cases can be evaluated as C-TIRADS category 3 (Fig. 3d).
Uncertainty of internal characteristics because of calcifications
Macrocalcifications or peripheral calcifications with strong acoustic shadowing will preclude fully assessment of internal characteristics of the nodules. According to the ACR-TIRADS, such nodules can be assessed as at least ACR-TIRADS 4, with a malignant risk of >5% [19]. Thus, it is appropriate that such nodules fall under C-TIRADS 4A category (Fig. 3e).
Nodule with snowstorm pattern of microcalcifications
Snowstorm pattern of microcalcifications are referred to a large number of incalculable microcalcifications present in the nodules. According to a study, all nodules that showed snowstorm pattern of microcalcifications were malignant [141]. Consequently, such nodules can be classified as C-TIRADS category 5 (Fig. 3f).
Incalculable nodule-independent microcalcifications
A large number of incalculable nodule-independent microcalcifications that are typically snowstorm-like are diffusely scattered in the whole or large area of unilateral or bilateral thyroid gland, which is always seen in the diffuse sclerosing variant of PTC [142, 143]. If typical cervical metastatic lymph nodes of thyroid cancer are observed, these findings are assessed to belong to C-TIRADS category 5 (Fig. 3g). However, if no suspicious cervical lymph node is found, it could be assessed into more than category 4B or even category 5 based on the personal experience of the doctor.
Recommendation
R7: Gray-scale ultrasound features are the most important factor in judging the risk stratification of thyroid nodules (Grade A).
R8: Ultrasound assessment of cervical lymph nodes can provide important information regarding risk stratification of thyroid nodules (Grade A).
R9: The C-TIRADS category based on the counting method can be modified according to the experience of radiologists, the clinical history, and the special ultrasound features (Grade B).
R10: Doppler Ultrasound, SE, and CEUS can sometimes be complementary (Grade B).
Suggestions on the management of thyroid nodules
As mentioned above, many thyroid surgeries in China are based not on FNA results, but on ultrasound reports, sometimes in combination with other relevant clinical evidences. Our survey report also showed that China faces the problem of over-operation of both benign thyroid nodules and PTMCs.
Due to large gap at medical level in hospitals of different grades nationwide, and striking cognitive differences in diseases among patients with different educational levels and from different regions, our grasp of principles at present for thyroid nodule management should embody a certain flexibility, in which regional disparity, national character, cultural tradition, and healthcare systems should be considered, in addition to the nodule itself.
However, following the internationally accepted principles for diagnosis and management of thyroid nodules is the direction of our future efforts. Therefore, this management proposal also refers to the guidelines of the United States, Europe, and Korea [16, 17, 19]. The expert panel hoped that ultrasound-guided FNA can be widely carried out in all regions of China by the efforts of all parties, thereby alleviating the problem of overtreatment of benign nodules and PTMCs, reducing the harm to the patients and wasting of medical resources.
Management recommendations
TIRADS 1: no need to deal with nodule-related problems.
TIRADS 2 (malignancy rate is 0%): FNA is not required. In cases of cystic nodules, cystic fluid suctioning can be performed under ultrasound guidance when the cyst is too large to cause compression symptoms or cosmetic problems. If cytology confirms that the cystic nodule is benign, chemical ablation can be performed [16]. If the nodules are mixed cystic and solid and cause compression symptoms or cosmetic problems, the following treatment options are available:
-
(1)
Surgical treatment;
-
(2)
For patients who refuses surgery, if the nodule is confirmed as benign by biopsy, debulking thermal ablation and even the complete cytoreduction thermal ablation under ultrasound guidance can be adopted [144];
-
(3)
Thermal ablation is not recommended if the nodule is too large to compress the trachea and causes obvious tracheal collapse and deformation.
TIRADS 3 (malignancy rate is <2%): FNA is not required. If the nodules are too large to cause compression symptoms or cosmetic problems, the management principle of TIRADS 2 nodules is referred to, provided the biopsy results are benign.
TIRADS 4A (malignancy rate is 2–10%):
-
(1)
If the nodule is >15 mm, FNA-guided ultrasound is recommended [16, 17, 19];
-
(2)
Multifocality, subcapsular nodule, trachea, and recurrent laryngeal nerve invasion are considered as predictors of poor prognosis of PTC [145,146,147,148,149]. Thus, when category 4A nodules are multiple, or immediately adjacent to the trachea or recurrent laryngeal nerve, ultrasound-guided FNA can be considered if the nodule is >10 mm;
-
(3)
For solitary nodule of ≤10 mm that is not immediately adjacent to the capsule, trachea or recurrent laryngeal nerve, regular follow-up is optional;
-
(4)
If the nodules are too large to cause compression symptoms or cosmetic problems, the management principle of TIRADS 2-3 nodules can be referred to, provided the biopsy results are benign.
TIRADS 4B (malignancy rate is 10–50%):
-
(1)
If the nodule is >10 mm, FNA-guided by ultrasound is recommended [16, 17, 19];
-
(2)
If nodules are multiple, or immediately adjacent to the capsule, trachea, or recurrent laryngeal nerve, ultrasound-guided FNA can be considered if the nodule is >5 mm [20];
-
(3)
If nodules <5 mm are multiple, or are immediately adjacent to the capsule, trachea, or the recurrent laryngeal nerve, then biopsy is required by comprehensively considering the skills of the doctor and the anxiety level of the patient;
-
(4)
For solitary nodule of ≤10 mm that is not immediately adjacent to the capsule, trachea, or recurrent laryngeal nerve, an active surveillance strategy can be chosen with full informed consent.
TIRADS 4C (malignancy rate is 50–90%): recommended management is similar to category 4B nodules.
TIRADS 5 (malignancy rate is >90%): The recommended management is similar to that of category 4B nodules. If there are typical cervical metastatic lymph nodes of thyroid cancer, then the most suspicious nodules of any size in the ipsilateral thyroid require ultrasound-guided FNA.
TIRADS 6 (FNA confirmed Bethesda VI nodules; core needle Biopsy confirmed malignant nodules): surgery, thermal ablation, or active surveillance. See below for details.
Notes on management recommendations
For patients with familial thyroid carcinoma or history of radiation exposure during childhood, the threshold size for FNA as described above can be appropriately reduced [2]. For determining if FNA can be performed in each specific case, the patient’s personal preference and anxiety level should also be taken into account.
If nodules have been underwent thyroid scintigraphy and demonstrated to be warm/hot, FNA is not recommended because these nodules are usually benign. One study showed that all hyperfunctioning thyroid nodules were benign regardless of their TIRADS classifications [150]. Therefore, integrating the information of thyroid scintigraphy and ultrasound can avoid unnecessary FNA.
Although the management recommendations for C-TIRADS 4B, 4C, and 5 nodules are the same, these different classifications can provide clinicians and patients with information on the probability of malignancy. The expert panel does not encourage or advocate the treatment strategy of surgical removal of thyroid nodules according to the risk stratification of ultrasound without FNA. However, it must be recognized that such situation will exist for a long time in China in the future. For those medical institutions where FNA has not been practiced at present, the results of nodule classification of C-TIRADS might act as a reference for the surgeon to decide whether or not to perform surgery. However, it must be emphasized that the C-TIRADS classification is established with the aim to determine which nodules require FNA. This in turn promotes FNA to be widely carried out in the future, reducing the problem of overtreatment of thyroid nodules in China.
Recommendation
R11: Thyroid nodules of different risk of malignancy should undergo FNA when their size reaches the corresponding threshold (Grade A).
R12: For suspicious solitary nodule of ≤10 mm that is not immediately adjacent to the capsule, trachea, or recurrent laryngeal nerve, an active surveillance strategy can be chosen with full informed consent (Grade B).
R13: For those medical institutions where FNA has not been practiced, the results of nodule classification of C-TIRADS might act as a reference for the surgeon to decide whether or not to perform surgery (Grade I).
Reporting system
The report should be concise and focused. After briefly describing the echogenic texture of the thyroid gland, the ultrasound characteristics of the nodule(s) should be recorded in detail. Finally, the C-TIRADS assessment classification and management recommendations should be given.
The terminology in the lexicon should be used without embellishment to describe the ultrasound features of the target nodule. It is not necessary to use all the terms to describe the nodule, but the five categories of terms that determine the C-TIRADS classification, i.e., orientation, margin, composition, echogenicity, and echogenic foci, should be used. Nodule(s) with the highest C-TIRADS classification, sometimes with the largest size, in each lobe and isthmus should be described in detail using the abovementioned five categories of terms. In order to facilitate follow-up or determine whether FNA is needed, the location and size of the target nodule should also be described in detail. When the nodule is adjacent to the thyroid capsule, the distance between the nodule and the capsule should be described [2, 51,52,53,54,55,56].
Recommendation for management was made according to the C-TIRADS category. The recommendation also takes into account China’s medical resources and medical costs as a developing country. In principle, no more than 1 nodule each lobe is recommended for FNA when one or more nodules meet the category and size threshold for FNA. For patients who do not meet the FNA criteria and choose to follow-up, the follow-up interval is 6–24 months, depending on the classification, size, and location of the nodules, as well as the degree of anxiety of the patients. Considering the current medical situation in China and the national character of China, the expert panel does not recommend the development and implementation of overly specific follow-up interval standards at this time.
Recommendation
R14: Terminology should be used to describe the nodule, and the classification and management recommendation should be given in the reporting system (Grade A).
R15: The management recommendation should take into account China’s medical resources and medical costs as a developing country (Grade B).
As mentioned above, there is a growing opinion on the strategy of active surveillance rather than surgical treatment for low-risk PTMCs, therefore the corresponding content is included in C-TIRADS management recommendations. However, due to the constraints of national character and cultural tradition, the management strategy of active surveillance is currently difficult to achieve a widespread response in China. So, this requires joint efforts of Chinese medical workers including ultrasound radiologists to let the public know more about PTMC.
Recently, with the development of thermal ablation technologies such as laser, radiofrequency, and microwave, an increasing number of researchers has been trying to use thermal ablation to treat low-risk PTMCs and has achieved satisfactory results [144, 151,152,153,154]. In the opinion of expert panel, if the nodule is confirmed to be PTC by biopsy, ultrasound-guided thermal ablation can be performed under the following conditions and with full informed consent from the patient: (1) nodule ≤10 mm; (2) solitary; (3) nodule does not involve the trachea and is more than 1–2 mm away from the dorsal medial thyroid capsule (depends on the experience of the operator); (4) no evidence of cervical lymph node metastasis; and (5) no evidence of distant metastasis [155, 156]. However, it must be clearly recognized that thermal ablation for low-risk PTMCs is still in the early stage, and its long-term efficacy remains to be observed for a long time [157]. The expert panel will continue to follow this up.
Recommendation
R16: For PTMC that meets strict indications, ultrasound-guided thermal ablation can be chosen with full informed consent (Grade B).
Disclaimer
This guideline is only used as a professional standard for reference by ultrasound radiologists in medical institutions of various grades in China, but not as a legal basis.
References
C. Durante, G. Grani, L. Lamartina, S. Filetti, S.J. Mandel, D.S. Cooper, The diagnosis and management of thyroid nodules: a review. JAMA 319(9), 914–924 (2018). https://doi.org/10.1001/jama.2018.0898
B.R. Haugen, E.K. Alexander, K.C. Bible, G.M. Doherty, S.J. Mandel, Y.E. Nikiforov, F. Pacini, G.W. Randolph, A.M. Sawka, M. Schlumberger, K.G. Schuff, S.I. Sherman, J.A. Sosa, D.L. Steward, R.M. Tuttle, L. Wartofsky, 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1), 1–133 (2016). https://doi.org/10.1089/thy.2015.0020
Z. Chen, W. Xu, Y. Huang, X. Jin, J. Deng, S. Zhu, H. Liu, S. Zhang, Y. Yu, Associations of noniodized salt and thyroid nodule among the Chinese population: a large cross-sectional study. Am. J. Clin. Nutr. 98(3), 684–692 (2013). https://doi.org/10.3945/ajcn.112.054353
J. Yin, C. Wang, Q. Shao, D. Qu, Z. Song, P. Shan, T. Zhang, J. Xu, Q. Liang, S. Zhang, J. Huang, Relationship between the Prevalence of Thyroid Nodules and Metabolic Syndrome in the Iodine-Adequate Area of Hangzhou, China: A Cross-Sectional and Cohort Study. Int J. Endocrinol. 2014, 675796 (2014). https://doi.org/10.1155/2014/675796
W. Xu, Z. Chen, N. Li, H. Liu, L. Huo, Y. Huang, X. Jin, J. Deng, S. Zhu, S. Zhang, Y. Yu, Relationship of anthropometric measurements to thyroid nodules in a Chinese population. BMJ Open 5(12), e008452 (2015). https://doi.org/10.1136/bmjopen-2015-008452
Y. Li, D. Teng, J. Ba, B. Chen, J. Du, L. He, X. Lai, X. Teng, X. Shi, Y. Li, H. Chi, E. Liao, C. Liu, L. Liu, G. Qin, Y. Qin, H. Quan, B. Shi, H. Sun, X. Tang, N. Tong, G. Wang, J.A. Zhang, Y. Wang, Y. Xue, L. Yan, J. Yang, L. Yang, Y. Yao, Z. Ye, Q. Zhang, L. Zhang, J. Zhu, M. Zhu, G. Ning, Y. Mu, J. Zhao, Z. Shan, W. Teng, Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 provinces of Mainland China. Thyroid 30(4), 568–579 (2020). https://doi.org/10.1089/thy.2019.0067
American College of Radiology (ACR). Breast Imaging Reporting and Data System Atlas (BI-RADS Atlas), 1st edn. (American College of Radiology, Reston, VA, 1992)
E. Horvath, S. Majlis, R. Rossi, C. Franco, J.P. Niedmann, A. Castro, M. Dominguez, An ultrasonogram reporting system for thyroid nodules stratifying cancer risk for clinical management. J. Clin. Endocrinol. Metab. 94(5), 1748–1751 (2009). https://doi.org/10.1210/jc.2008-1724
J.Y. Park, H.J. Lee, H.W. Jang, H.K. Kim, J.H. Yi, W. Lee, S.H. Kim, A proposal for a thyroid imaging reporting and data system for ultrasound features of thyroid carcinoma. Thyroid 19(11), 1257–1264 (2009)
J.Y. Kwak, K.H. Han, J.H. Yoon, H.J. Moon, E.J. Son, S.H. Park, H.K. Jung, J.S. Choi, B.M. Kim, E.K. Kim, Thyroid imaging reporting and data system for US features of nodules: a step in establishing better stratification of cancer risk. Radiology 260(3), 892–899 (2011). https://doi.org/10.1148/radiol.11110206
G. Russ, C. Bigorgne, B. Royer, A. Rouxel, M. Bienvenu-Perrard, The Thyroid Imaging Reporting and Data System (TIRADS) for ultrasound of the thyroid. J. Radio. 92(7–8), 701–713 (2011). https://doi.org/10.1016/j.jradio.2011.03.022
J.F. Sánchez, TI-RADS classifcation of thyroid nodules based on a score modifed according to ultrasound criteria for malignancy. Rev. Argent. Radiol. 78(3), 138–148 (2014)
A.R. Zayadeen, M. Abu-Yousef, K. Berbaum, JOURNAL CLUB: retrospective evaluation of ultrasound features of thyroid nodules to assess malignancy risk: a step toward TIRADS. AJR Am. J. Roentgenol. 207(3), 460–469 (2016). https://doi.org/10.2214/AJR.15.15121
D. Songsaeng, S. Soodchuen, P. Korpraphong, A. Suwanbundit, Siriraj thyroid imaging reporting and data system and its effcacy. Siriraj Med. J. 69(5), 262–267 (2017)
S.Y. Xu, W.W. Zhan, W.H. Wang, Evaluation of thyroid nodules by a scoring and categorizing method based on sonographic features. J. Ultrasound Med. 34(12), 2179–2185 (2015). https://doi.org/10.7863/ultra.14.11041
J.H. Shin, J.H. Baek, J. Chung, E.J. Ha, J.H. Kim, Y.H. Lee, H.K. Lim, W.J. Moon, D.G. Na, J.S. Park, Y.J. Choi, S.Y. Hahn, S.J. Jeon, S.L. Jung, D.W. Kim, E.K. Kim, J.Y. Kwak, C.Y. Lee, H.J. Lee, J.H. Lee, J.H. Lee, K.H. Lee, S.W. Park, J.Y. Sung, Korean Society of Thyroid Radiology, Korean Society of Radiology, Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology Consensus Statement and Recommendations. Korean J. Radio. 17(3), 370–395 (2016). https://doi.org/10.3348/kjr.2016.17.3.370
G. Russ, S.J. Bonnema, M.F. Erdogan, C. Durante, R. Ngu, L. Leenhardt, European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur. Thyroid J. 6(5), 225–237 (2017). https://doi.org/10.1159/000478927
E.G. Grant, F.N. Tessler, J.K. Hoang, J.E. Langer, M.D. Beland, L.L. Berland, J.J. Cronan, T.S. Desser, M.C. Frates, U.M. Hamper, W.D. Middleton, C.C. Reading, L.M. Scoutt, A.T. Stavros, S.A. Teefey, Thyroid ultrasound reporting lexicon: white paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J. Am. Coll. Radiol. 12(12 Pt A), 1272–1279 (2015). https://doi.org/10.1016/j.jacr.2015.07.011
F.N. Tessler, W.D. Middleton, E.G. Grant, J.K. Hoang, L.L. Berland, S.A. Teefey, J.J. Cronan, M.D. Beland, T.S. Desser, M.C. Frates, L.W. Hammers, U.M. Hamper, J.E. Langer, C.C. Reading, L.M. Scoutt, A.T. Stavros, ACR Thyroid Imaging, Reporting and Data System (TI-RADS): white paper of the ACR TI-RADS Committee. J. Am. Coll. Radiol. 14(5), 587–595 (2017). https://doi.org/10.1016/j.jacr.2017.01.046
H. Gharib, E. Papini, J.R. Garber, D.S. Duick, R.M. Harrell, L. Hegedus, R. Paschke, R. Valcavi, P. Vitti, AACE/ACE/AME Task Force on Thyroid Nodules, American Association of Clinical Endocrinologists, American College of Endocrinology, and Associazione Medici Endocrinologi Medical Guidelines for Clinical Practice for the Diagnosis and Management of Thyroid Nodules—2016 update. Endocr. Pract. 22(5), 622–639 (2016). https://doi.org/10.4158/EP161208.GL
E.J. Ha, D.G. Na, J.H. Baek, J.Y. Sung, J.H. Kim, S.Y. Kang, US fine-needle aspiration biopsy for thyroid malignancy: diagnostic performance of seven society guidelines applied to 2000 thyroid nodules. Radiology 287(3), 893–900 (2018). https://doi.org/10.1148/radiol.2018171074
J.H. Yoon, K. Han, E.K. Kim, H.J. Moon, J.Y. Kwak, Diagnosis and management of small thyroid nodules: a comparative study with six guidelines for thyroid nodules. Radiology 283(2), 560–569 (2017). https://doi.org/10.1148/radiol.2016160641
J.H. Yoon, H.S. Lee, E.K. Kim, H.J. Moon, J.Y. Kwak, Malignancy risk stratification of thyroid nodules: comparison between the thyroid imaging reporting and data system and the 2014 American Thyroid Association Management Guidelines. Radiology 278(3), 917–924 (2016). https://doi.org/10.1148/radiol.2015150056
S.M. Ha, H.S. Ahn, J.H. Baek, H.Y. Ahn, Y.J. Chung, B.Y. Cho, S.B. Park, Validation of three scoring risk-stratification models for thyroid nodules. Thyroid 27(12), 1550–1557 (2017). https://doi.org/10.1089/thy.2017.0363
M. Castellana, C. Castellana, G. Treglia, F. Giorgino, L. Giovanella, G. Russ, P. Trimboli, Performance of five ultrasound risk stratification systems in selecting thyroid nodules for FNA. J. Clin. Endocrinol. Metab. 105(5) (2020). https://doi.org/10.1210/clinem/dgz170
G. Grani, L. Lamartina, V. Ascoli, D. Bosco, M. Biffoni, L. Giacomelli, M. Maranghi, R. Falcone, V. Ramundo, V. Cantisani, S. Filetti, C. Durante, Reducing the number of unnecessary thyroid biopsies while improving diagnostic accuracy: toward the “Right” TIRADS. J. Clin. Endocrinol. Metab. 104(1), 95–102 (2019). https://doi.org/10.1210/jc.2018-01674
S.J. Yoon, D.G. Na, H.Y. Gwon, W. Paik, W.J. Kim, J.S. Song, M.S. Shim, Similarities and differences between thyroid imaging reporting and data systems. AJR Am. J. Roentgenol. 213(2), W76–W84 (2019). https://doi.org/10.2214/AJR.18.20510
J.H. Yoon, H.S. Lee, E.K. Kim, H.J. Moon, V.Y. Park, J.Y. Kwak, Pattern-based vs. score-based guidelines using ultrasound features have different strengths in risk stratification of thyroid nodules. Eur. Radiol. (2020). https://doi.org/10.1007/s00330-020-06722-y
Q. Zhang, J. Ma, W. Sun, L. Zhang, Comparison of diagnostic performance between the American College of Radiology Thyroid Imaging Reporting and Data System and American Thyroid Association Guidelines: a systematic review. Endocr. Pract. 26(5), 552–563 (2020). https://doi.org/10.4158/EP-2019-0237
S.J. Choi, W.K. Jeong, A.J. Jo, J.A. Choi, M.J. Kim, M. Lee, S.E. Jung, K.H. Do, H.S. Yong, S. Sheen, M. Choi, J.H. Baek, Methodology for developing evidence-based clinical imaging guidelines: joint recommendations by Korean Society of Radiology and National Evidence-Based Healthcare Collaborating Agency. Korean J. Radiol. 18(1), 208–216 (2017). https://doi.org/10.3348/kjr.2017.18.1.208
D. Cosgrove, R. Barr, J. Bojunga, V. Cantisani, M.C. Chammas, M. Dighe, S. Vinayak, J.M. Xu, C.F. Dietrich, WFUMB guidelines and recommendations on the clinical use of ultrasound elastography: part 4. Thyroid. Ultrasound Med. Biol. 43(1), 4–26 (2017). https://doi.org/10.1016/j.ultrasmedbio.2016.06.022
D. Cosgrove, F. Piscaglia, J. Bamber, J. Bojunga, J.M. Correas, O.H. Gilja, A.S. Klauser, I. Sporea, F. Calliada, V. Cantisani, M. D’Onofrio, E.E. Drakonaki, M. Fink, M. Friedrich-Rust, J. Fromageau, R.F. Havre, C. Jenssen, R. Ohlinger, A. Saftoiu, F. Schaefer, C.F. Dietrich; Efsumb, EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall Med. 34(3), 238–253 (2013). https://doi.org/10.1055/s-0033-1335375
Q. Peng, C. Niu, Q. Zhang, M. Zhang, S. Chen, Q. Peng, Mummified thyroid nodules: conventional and contrast-enhanced ultrasound features. J. Ultrasound Med. 38(2), 441–452 (2019). https://doi.org/10.1002/jum.14712
F. Gu, L. Han, X. Yang, H. Liu, X. Li, K. Guo, Z. Zhao, X. Zhou, W. Luo, Value of time-intensity curve analysis of contrast-enhanced ultrasound in the differential diagnosis of thyroid nodules. Eur. J. Radiol. 105, 182–187 (2018). https://doi.org/10.1016/j.ejrad.2018.05.013
L. Leenhardt, M.F. Erdogan, L. Hegedus, S.J. Mandel, R. Paschke, T. Rago, G. Russ, 2013 European thyroid association guidelines for cervical ultrasound scan and ultrasound-guided techniques in the postoperative management of patients with thyroid cancer. Eur. Thyroid J. 2(3), 147–159 (2013). https://doi.org/10.1159/000354537
M.A. Kouvaraki, S.E. Shapiro, B.D. Fornage, B.S. Edeiken-Monro, S.I. Sherman, R. Vassilopoulou-Sellin, J.E. Lee, D.B. Evans, Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery 134(6), 946–954 (2003). https://doi.org/10.1016/s0039-6060(03)00424-0
P.J. Mazzaglia, Surgeon-performed ultrasound in patients referred for thyroid disease improves patient care by minimizing performance of unnecessary procedures and optimizing surgical treatment. World J. Surg. 34(6), 1164–1170 (2010). https://doi.org/10.1007/s00268-010-0402-y
A.E. Cox, S.O. LeBeau, Diagnosis and treatment of differentiated thyroid carcinoma. Radiol. Clin. North Am. 49(3), 453–462 (2011). https://doi.org/10.1016/j.rcl.2011.02.006
Z.W. Baloch, V.A. LiVolsi, Fine-needle aspiration of the thyroid: today and tomorrow. Best. Pract. Res Clin. Endocrinol. Metab. 22(6), 929–939 (2008)
R.H. Cobin, H. Gharib, D.A. Bergman, O.H. Clark, D.S. Cooper, G.H. Daniels, R.A. Dickey, D.S. Duick, J.R. Garber, I.D. Hay, J.S. Kukora, H.M. Lando, A.B. Schorr, M.A. Zeiger; Thyroid Carcinoma Task Force, AACE/AAES medical/surgical guidelines for clinical practice: management of thyroid carcinoma. American Association of Clinical Endocrinologists. American College of Endocrinology. Endocr. Pract. 7(3), 202–220 (2001)
M.J. Kim, E.K. Kim, S.I. Park, B.M. Kim, J.Y. Kwak, S.J. Kim, J.H. Youk, S.H. Park, US-guided fine-needle aspiration of thyroid nodules: indications, techniques, results. RadioGraphics 28(7), 1869–1886 (2008). https://doi.org/10.1148/rg.287085033
N. Nagarajan, E.B. Schneider, S.Z. Ali, M.A. Zeiger, M.T. Olson, How do liquid-based preparations of thyroid fine-needle aspiration compare with conventional smears? An analysis of 5475 specimens. Thyroid 25(3), 308–313 (2015). https://doi.org/10.1089/thy.2014.0394
H. Chang, E. Lee, H. Lee, J. Choi, A. Kim, B.H. Kim, Comparison of diagnostic values of thyroid aspiration samples using liquid-based preparation and conventional smear: one-year experience in a single institution. APMIS 121(2), 139–145 (2013). https://doi.org/10.1111/j.1600-0463.2012.02944.x
S. Vaccarella, S. Franceschi, F. Bray, C.P. Wild, M. Plummer, L. Dal Maso, Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N. Engl. J. Med. 375(7), 614–617 (2016). https://doi.org/10.1056/NEJMp1604412
H.S. Ahn, H.J. Kim, H.G. Welch, Korea’s thyroid-cancer “epidemic”–screening and overdiagnosis. N. Engl. J. Med. 371(19), 1765–1767 (2014). https://doi.org/10.1056/NEJMp1409841
H.S. Ahn, H.G. Welch, South Korea’s thyroid-cancer “epidemic”—turning the tide. N. Engl. J. Med 373(24), 2389–2390 (2015). https://doi.org/10.1056/NEJMc1507622
C. La Vecchia, M. Malvezzi, C. Bosetti, W. Garavello, P. Bertuccio, F. Levi, E. Negri, Thyroid cancer mortality and incidence: a global overview. Int J. Cancer 136(9), 2187–2195 (2015). https://doi.org/10.1002/ijc.29251
J.J. Cronan, Thyroid nodules: is it time to turn off the US machines? Radiology 247(3), 602–604 (2008). https://doi.org/10.1148/radiol.2473072233
H. Lim, S.S. Devesa, J.A. Sosa, D. Check, C.M. Kitahara, Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317(13), 1338–1348 (2017). https://doi.org/10.1001/jama.2017.2719
C. La Vecchia, E. Negri, Thyroid cancer: the thyroid cancer epidemic—overdiagnosis or a real increase? Nat. Rev. Endocrinol. 13(6), 318–319 (2017). https://doi.org/10.1038/nrendo.2017.53
Y. Ito, A. Miyauchi, H. Oda, Low-risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur. J. Surg. Oncol. 44(3), 307–315 (2018). https://doi.org/10.1016/j.ejso.2017.03.004
G.C. Haser, R.M. Tuttle, H.K. Su, E.E. Alon, D. Bergman, V. Bernet, E. Brett, R. Cobin, E.H. Dewey, G. Doherty, L.L. Dos Reis, J. Harris, J. Klopper, S.L. Lee, R.A. Levine, S.J. Lepore, I. Likhterov, M.A. Lupo, J. Machac, J.I. Mechanick, S. Mehra, M. Milas, L.A. Orloff, G. Randolph, T.A. Revenson, K.J. Roberts, D.S. Ross, M.E. Rowe, R.C. Smallridge, D. Terris, R.P. Tufano, M.L. Urken, Active surveillance for papillary thyroid microcarcinoma: new challenges and opportunities for the health care system. Endocr. Pract. 22(5), 602–611 (2016). https://doi.org/10.4158/EP151065.RA
S. Leboulleux, R.M. Tuttle, F. Pacini, M. Schlumberger, Papillary thyroid microcarcinoma: time to shift from surgery to active surveillance? Lancet Diabetes Endocrinol. 4(11), 933–942 (2016). https://doi.org/10.1016/S2213-8587(16)30180-2
Y. Ito, T. Uruno, K. Nakano, Y. Takamura, A. Miya, K. Kobayashi, T. Yokozawa, F. Matsuzuka, S. Kuma, K. Kuma, A. Miyauchi, An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 13(4), 381–387 (2003). https://doi.org/10.1089/105072503321669875
Y. Ito, A. Miyauchi, H. Inoue, M. Fukushima, M. Kihara, T. Higashiyama, C. Tomoda, Y. Takamura, K. Kobayashi, A. Miya, An observational trial for papillary thyroid microcarcinoma in Japanese patients. World J. Surg. 34(1), 28–35 (2010). https://doi.org/10.1007/s00268-009-0303-0
Y. Ito, A. Miyauchi, M. Kihara, T. Higashiyama, K. Kobayashi, A. Miya, Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid 24(1), 27–34 (2014). https://doi.org/10.1089/thy.2013.0367
L. Du, Y. Wang, X. Sun, H. Li, X. Geng, M. Ge, Y. Zhu, Thyroid cancer: trends in incidence, mortality and clinical-pathological patterns in Zhejiang Province, Southeast China. BMC Cancer 18(1), 291 (2018). https://doi.org/10.1186/s12885-018-4081-7
S.H. Xie, J. Chen, B. Zhang, F. Wang, S.S. Li, C.H. Xie, L.A. Tse, J.Q. Cheng, Time trends and age-period-cohort analyses on incidence rates of thyroid cancer in Shanghai and Hong Kong. BMC Cancer 14, 975 (2014). https://doi.org/10.1186/1471-2407-14-975
M.C. Frates, C.B. Benson, J.W. Charboneau, E.S. Cibas, O.H. Clark, B.G. Coleman, J.J. Cronan, P.M. Doubilet, D.B. Evans, J.R. Goellner, I.D. Hay, B.S. Hertzberg, C.M. Intenzo, R.B. Jeffrey, J.E. Langer, P.R. Larsen, S.J. Mandel, W.D. Middleton, C.C. Reading, S.I. Sherman, F.N. Tessler, Management of thyroid nodules detected at US: Society of Radiologists in Ultrasound consensus conference statement. Radiology 237(3), 794–800 (2005)
AIUM practice parameter for the performance of a thyroid and parathyroid ultrasound examination. J. Ultrasound Med. 35(9), 1–11 (2016). https://doi.org/10.7863/ultra.35.9.1-c
S. Edge, D. Byrd, C. Compton, A. Fritz, F. Greene, A. Trotti. AJCC Cancer Staging Manual, 7th edn. (Springer, New York, NY, 2010)
S. Yan, W. Zhan, J.Q. Zhou. Ultrasound of the Thyroid and Parathyroid Glands.1st edn. (Science and Technology Literature Publishing House, Beijing, 2009)
M.C. Chammas, H.J. Moon, E.K. Kim, Why do we have so many controversies in thyroid nodule Doppler US? Radiology 259(1), 304 (2011). https://doi.org/10.1148/radiol.10101830
P.S. Sidhu, V. Cantisani, C.F. Dietrich, O.H. Gilja, A. Saftoiu, E. Bartels, M. Bertolotto, F. Calliada, D.A. Clevert, D. Cosgrove, A. Deganello, M. D’Onofrio, F.M. Drudi, S. Freeman, C. Harvey, C. Jenssen, E.M. Jung, A.S. Klauser, N. Lassau, M.F. Meloni, E. Leen, C. Nicolau, C. Nolsoe, F. Piscaglia, F. Prada, H. Prosch, M. Radzina, L. Savelli, H.P. Weskott, H. Wijkstra, The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in non-hepatic applications: update 2017 (Long Version). Ultraschall Med. 39(2), e2–e44 (2018). https://doi.org/10.1055/a-0586-1107
H. Seo, D.G. Na, J.H. Kim, K.W. Kim, J.W. Yoon, Ultrasound-based risk stratification for malignancy in thyroid nodules: a four-tier categorization system. Eur. Radiol. 25(7), 2153–2162 (2015). https://doi.org/10.1007/s00330-015-3621-7
W.J. Moon, J.H. Baek, S.L. Jung, D.W. Kim, E.K. Kim, J.Y. Kim, J.Y. Kwak, J.H. Lee, J.H. Lee, Y.H. Lee, D.G. Na, J.S. Park, S.W. Park; Korean Society of Thyroid Radiology, Korean Society of Radiology, Ultrasonography and the ultrasound-based management of thyroid nodules: consensus statement and recommendations. Korean J. Radiol. 12(1), 1–14 (2011). https://doi.org/10.3348/kjr.2011.12.1.1
M. Itani, R. Assaker, M. Moshiri, T.J. Dubinsky, M.K. Dighe, Inter-observer variability in the American College of Radiology Thyroid Imaging Reporting and Data System: in-depth analysis and areas for improvement. Ultrasound Med. Biol. 45(2), 461–470 (2019). https://doi.org/10.1016/j.ultrasmedbio.2018.09.026
J.K. Hoang, W.D. Middleton, A.E. Farjat, S.A. Teefey, N. Abinanti, F.J. Boschini, A.J. Bronner, N. Dahiya, B.S. Hertzberg, J.R. Newman, D. Scanga, R.C. Vogler, F.N. Tessler, Interobserver variability of sonographic features used in the American College of Radiology Thyroid Imaging Reporting and Data System. AJR Am. J. Roentgenol. 211(1), 162–167 (2018). https://doi.org/10.2214/AJR.17.19192
Z.T. Sahli, A.K. Sharma, J.K. Canner, F. Karipineni, O. Ali, S. Kawamoto, J.F. Hang, A. Mathur, S.Z. Ali, M.A. Zeiger, S. Sheth, TIRADS interobserver variability among indeterminate thyroid nodules: a single-institution study. J. Ultrasound Med. 38(7), 1807–1813 (2019). https://doi.org/10.1002/jum.14870
S.H. Kim, C.S. Park, S.L. Jung, B.J. Kang, J.Y. Kim, J.J. Choi, Y.I. Kim, J.K. Oh, J.S. Oh, H. Kim, S.H. Jeong, H.W. Yim, Observer variability and the performance between faculties and residents: US criteria for benign and malignant thyroid nodules. Korean J. Radiol. 11(2), 149–155 (2010). https://doi.org/10.3348/kjr.2010.11.2.149
R. Chung, A.B. Rosenkrantz, G.L. Bennett, B. Dane, J.E. Jacobs, C. Slywotzky, P.N. Smereka, A. Tong, S. Sheth, Interreader concordance of the TI-RADS: impact of radiologist experience. AJR Am. J. Roentgenol. 214(5), 1152–1157 (2020). https://doi.org/10.2214/AJR.19.21913
Y. Ito, C. Tomoda, T. Uruno, Y. Takamura, A. Miya, K. Kobayashi, F. Matsuzuka, K. Kuma, A. Miyauchi, Papillary microcarcinoma of the thyroid: how should it be treated? World J. Surg. 28(11), 1115–1121 (2004)
G. Li, J. Lei, Q. Peng, K. Jiang, W. Chen, W. Zhao, Z. Li, R. Gong, T. Wei, J. Zhu, Lymph node metastasis characteristics of papillary thyroid carcinoma located in the isthmus: a single-center analysis. Medicine 96(24), e7143 (2017). https://doi.org/10.1097/MD.0000000000007143
M. Andrioli, C. Carzaniga, L. Persani, Standardized ultrasound report for thyroid nodules: the endocrinologist’s viewpoint. Eur. Thyroid J. 2(1), 37–48 (2013). https://doi.org/10.1159/000347144
S.Y. Hahn, B.K. Han, E.Y. Ko, J.H. Shin, E.S. Ko, Ultrasound findings of papillary thyroid carcinoma originating in the isthmus: comparison with lobe-originating papillary thyroid carcinoma. AJR Am. J. Roentgenol. 203(3), 637–642 (2014). https://doi.org/10.2214/AJR.13.10746
Y.J. Chai, S.J. Kim, J.Y. Choi, H. Koo do, K.E. Lee, Y.K: Youn, Papillary thyroid carcinoma located in the isthmus or upper third is associated with Delphian lymph node metastasis. World J. Surg. 38(6), 1306–1311 (2014). https://doi.org/10.1007/s00268-013-2406-x
M. Li, X.Y. Zhu, J. Lv, K. Lu, M.P. Shen, Z.L. Xu, Z.S. Wu, Risk factors for predicting central lymph node metastasis in papillary thyroid microcarcinoma (CN0): a study of 273 resections. Eur. Rev. Med Pharm. Sci. 21(17), 3801–3807 (2017)
D. Xiang, L. Xie, Y. Xu, Z. Li, Y. Hong, P. Wang, Papillary thyroid microcarcinomas located at the middle part of the middle third of the thyroid gland correlates with the presence of neck metastasis. Surgery 157(3), 526–533 (2015). https://doi.org/10.1016/j.surg.2014.10.020
J.Y. Kwak, E.K. Kim, M.J. Kim, E.J. Son, W.Y. Chung, C.S. Park, K.H. Nam, Papillary microcarcinoma of the thyroid: predicting factors of lateral neck node metastasis. Ann. Surg. Oncol. 16(5), 1348–1355 (2009). https://doi.org/10.1245/s10434-009-0384-x
W.X. Jin, Y.X. Jin, D.R. Ye, Z.C. Zheng, Y.H. Sun, X.F. Zhou, Q. Li, O.C. Wang, H.G. Liu, X.H. Zhang, Predictive factors of skip metastasis in papillary thyroid cancer. Med Sci. Monit. 24, 2744–2749 (2018). https://doi.org/10.12659/MSM.907357
J. Lei, J. Zhu, Z. Li, R. Gong, T. Wei, Surgical procedures for papillary thyroid carcinoma located in the thyroid isthmus: an intention-to-treat analysis. Onco Targets Ther. 9, 5209–5216 (2016). https://doi.org/10.2147/OTT.S106837
I. Vasileiadis, G. Boutzios, M. Karalaki, E. Misiakos, T. Karatzas, Papillary thyroid carcinoma of the isthmus: total thyroidectomy or isthmusectomy? Am. J. Surg. 216(1), 135–139 (2018). https://doi.org/10.1016/j.amjsurg.2017.09.008
F. Zhang, O. Oluwo, F.B. Castillo, P. Gangula, M. Castillo, F. Farag, S. Zakaria, T. Zahedi, Thyroid nodule location on ultrasonography as a predictor of malignancy. Endocr. Pract. 25(2), 131–137 (2019). https://doi.org/10.4158/EP-2018-0361
S. Jasim, T.J. Baranski, S.A. Teefey, W.D. Middleton, Investigating the effect of thyroid nodule location on the risk of thyroid cancer. Thyroid 30(3), 401–407 (2020). https://doi.org/10.1089/thy.2019.0478
V. Ramundo, L. Lamartina, R. Falcone, L. Ciotti, C. Lomonaco, M. Biffoni, L. Giacomelli, M. Maranghi, C. Durante, G. Grani, Is thyroid nodule location associated with malignancy risk? Ultrasonography 38(3), 231–235 (2019). https://doi.org/10.14366/usg.18050
E.K. Kim, C.S. Park, W.Y. Chung, K.K. Oh, D.I. Kim, J.T. Lee, H.S. Yoo, New sonographic criteria for recommending fine-needle aspiration biopsy of nonpalpable solid nodules of the thyroid. AJR Am. J. Roentgenol. 178(3), 687–691 (2002)
W.J. Moon, S.L. Jung, J.H. Lee, D.G. Na, J.H. Baek, Y.H. Lee, J. Kim, H.S. Kim, J.S. Byun, D.H. Lee, Benign and malignant thyroid nodules: US differentiation—multicenter retrospective study. Radiology 247(3), 762–770 (2008)
Y.J. Choi, J.H. Baek, S.H. Baek, W.H. Shim, K.D. Lee, H.S. Lee, Y.K. Shong, E.J. Ha, J.H. Lee, Web-based malignancy risk estimation for thyroid nodules using ultrasonography characteristics: development and validation of a predictive model. Thyroid 25(12), 1306–1312 (2015). https://doi.org/10.1089/thy.2015.0188
H.J. Moon, J.Y. Kwak, E.K. Kim, M.J. Kim, A taller-than-wide shape in thyroid nodules in transverse and longitudinal ultrasonographic planes and the prediction of malignancy. Thyroid 21(11), 1249–1253 (2011). https://doi.org/10.1089/thy.2010.0372
S.K. Jeh, S.L. Jung, B.S. Kim, Y.S. Lee, Evaluating the degree of conformity of papillary carcinoma and follicular carcinoma to the reported ultrasonographic findings of malignant thyroid tumor. Korean J. Radiol. 8(3), 192–197 (2007). https://doi.org/10.3348/kjr.2007.8.3.192
J.H. Yoon, E.K. Kim, S.W. Hong, J.Y. Kwak, M.J. Kim, Sonographic features of the follicular variant of papillary thyroid carcinoma. J. Ultrasound Med. 27(10), 1431–1437 (2008)
S.P. Chen, Y.P. Hu, B. Chen, Taller-than-wide sign for predicting thyroid microcarcinoma: comparison and combination of two ultrasonographic planes. Ultrasound Med Biol. 40(9), 2004–2011 (2014). https://doi.org/10.1016/j.ultrasmedbio.2014.03.023
C.Y. Lee, S.J. Kim, K.R. Ko, K.W. Chung, J.H. Lee, Predictive factors for extrathyroidal extension of papillary thyroid carcinoma based on preoperative sonography. J. Ultrasound Med. 33(2), 231–238 (2014). https://doi.org/10.7863/ultra.33.2.231
W.J. Moon, S.L. Jung, J.H. Lee, D.G. Na, J.H. Baek, Y.H. Lee, J. Kim, H.S. Kim, J.S. Byun, D.H. Lee; Thyroid Study Group, Korean Society of Neuro- and Head and Neck Radiology, Benign and malignant thyroid nodules: US differentiation–multicenter retrospective study. Radiology 247(3), 762–770 (2008). https://doi.org/10.1148/radiol.2473070944
D.M. Richman, C.B. Benson, P.M. Doubilet, H.E. Peters, S.A. Huang, E. Asch, A.J. Wassner, J.R. Smith, C.E. Cherella, M.C. Frates, Thyroid nodules in pediatric patients: sonographic characteristics and likelihood of cancer. Radiology 288(2), 591–599 (2018). https://doi.org/10.1148/radiol.2018171170
L.R. Remonti, C.K. Kramer, C.B. Leitao, L.C. Pinto, J.L. Gross, Thyroid ultrasound features and risk of carcinoma: a systematic review and meta-analysis of observational studies. Thyroid 25(5), 538–550 (2015). https://doi.org/10.1089/thy.2014.0353
G. Anil, A. Hegde, F.H. Chong, Thyroid nodules: risk stratification for malignancy with ultrasound and guided biopsy. Cancer Imaging 11, 209–223 (2011). https://doi.org/10.1102/1470-7330.2011.0030
V. Ramundo, C.R.T. Di Gioia, R. Falcone, L. Lamartina, M. Biffoni, L. Giacomelli, S. Filetti, C. Durante, G. Grani, Diagnostic performance of neck ultrasonography in the preoperative evaluation for extrathyroidal extension of suspicious thyroid nodules. World J. Surg. (2020). https://doi.org/10.1007/s00268-020-05482-6
M.C. Chammas, R. Gerhard, I.R. de Oliveira, A. Widman, N. de Barros, M. Durazzo, A. Ferraz, G.G. Cerri, Thyroid nodules: evaluation with power Doppler and duplex Doppler ultrasound. Otolaryngol. Head. Neck Surg. 132(6), 874–882 (2005)
W.H. Yuan, H.J. Chiou, Y.H. Chou, H.C. Hsu, C.M. Tiu, C.Y. Cheng, C.H. Lee, Gray-scale and color Doppler ultrasonographic manifestations of papillary thyroid carcinoma: analysis of 51 cases. Clin. Imaging 30(6), 394–401 (2006)
R.L.C. Delfim, L. Veiga, A.P.A. Vidal, F. Lopes, M. Vaisman, P. Teixeira, Likelihood of malignancy in thyroid nodules according to a proposed Thyroid Imaging Reporting and Data System (TI-RADS) classification merging suspicious and benign ultrasound features. Arch. Endocrinol. Metab. 61(3), 211–221 (2017). https://doi.org/10.1590/2359-3997000000262
W.J. Moon, H.J. Kwag, D.G. Na, Are there any specific ultrasound findings of nodular hyperplasia (“leave me alone” lesion) to differentiate it from follicular adenoma? Acta Radiol. 50(4), 383–388 (2009). https://doi.org/10.1080/02841850902740940
E. Koike, S. Noguchi, H. Yamashita, T. Murakami, A. Ohshima, H. Kawamoto, H. Yamashita, Ultrasonographic characteristics of thyroid nodules: prediction of malignancy. Arch. Surg. 136(3), 334–337 (2001)
B.K. Chan, T.S. Desser, I.R. McDougall, R.J. Weigel, R.B. Jeffrey Jr, Common and uncommon sonographic features of papillary thyroid carcinoma. J. Ultrasound Med. 22(10), 1083–1090 (2003)
J.Z. Zhang, B. Hu, Sonographic features of thyroid follicular carcinoma in comparison with thyroid follicular adenoma. J. Ultrasound Med. 33(2), 221–227 (2014). https://doi.org/10.7863/ultra.33.2.221
A. Lyshchik, V. Drozd, Y. Demidchik, C. Reiners, Diagnosis of thyroid cancer in children: value of gray-scale and power doppler US. Radiology 235(2), 604–613 (2005)
A.M. Tahvildari, L. Pan, C.S. Kong, T. Desser, Sonographic-pathologic correlation for punctate echogenic reflectors in papillary thyroid carcinoma: what are they? J. Ultrasound Med. 35(8), 1645–1652 (2016). https://doi.org/10.7863/ultra.15.09048
H.Y. Gwon, D.G. Na, B.J. Noh, W. Paik, S.J. Yoon, S.J. Choi, D.R. Shin, Thyroid nodules with isolated macrocalcifications: malignancy risk of isolated macrocalcifications and postoperative risk stratification of malignant tumors manifesting as isolated macrocalcifications. Korean J. Radiol. 21(5), 605–613 (2020). https://doi.org/10.3348/kjr.2019.0523
H. Malhi, M.D. Beland, S.Y. Cen, E. Allgood, K. Daley, S.E. Martin, J.J. Cronan, E.G. Grant, Echogenic foci in thyroid nodules: significance of posterior acoustic artifacts. AJR Am. J. Roentgenol. 203(6), 1310–1316 (2014). https://doi.org/10.2214/AJR.13.11934
A. Ahuja, W. Chick, W. King, C. Metreweli, Clinical significance of the comet-tail artifact in thyroid ultrasound. J. Clin. Ultrasound 24(3), 129–133 (1996)
D.T. Ginat, D. Butani, E.J. Giampoli, N. Patel, V. Dogra, Pearls and pitfalls of thyroid nodule sonography and fine-needle aspiration. Ultrasound Q. 26(3), 171–178 (2010). https://doi.org/10.1097/RUQ.0b013e3181efa710
K. Klang, A. Kamaya, A.M. Tahvildari, R.B. Jeffrey, T.S. Desser, Atypical thyroid cancers on sonography. Ultrasound Q. 31(1), 69–74 (2015). https://doi.org/10.1097/RUQ.0000000000000079
H. Wu, B. Zhang, J. Li, Q. Liu, T. Zhao, Echogenic foci with comet-tail artifact in resected thyroid nodules: not an absolute predictor of benign disease. PLoS ONE 13(1), e0191505 (2018). https://doi.org/10.1371/journal.pone.0191505
M.D. Beland, L. Kwon, R.A. Delellis, J.J. Cronan, E.G. Grant, Nonshadowing echogenic foci in thyroid nodules: are certain appearances enough to avoid thyroid biopsy? J. Ultrasound Med. 30(6), 753–760 (2011)
B. Mallikarjunappa, S.R. Ashish, Ultrasound evaluation of thyroid nodules and its pathological correlation. JIMSA Jan. 27(1), 9–11 (2014)
D.W. Kim, Sonographic features of thyroidal fatty lesions in the thyroid gland: a preliminary study. AJR Am. J. Roentgenol. 207(2), 411–414 (2016). https://doi.org/10.2214/AJR.15.15984
Q.S. Li, S.H. Chen, H.H. Xiong, X.H. Xu, Z.Z. Li, G.Q. Guo, Papillary thyroid carcinoma on sonography. Clin. Imaging 34(2), 121–126 (2010). https://doi.org/10.1016/j.clinimag.2009.03.003
H. Ota, Y. Ito, F. Matsuzuka, S. Kuma, S. Fukata, S. Morita, K. Kobayashi, Y. Nakamura, K. Kakudo, N. Amino, A. Miyauchi, Usefulness of ultrasonography for diagnosis of malignant lymphoma of the thyroid. Thyroid 16(10), 983–987 (2006)
Y. Ito, N. Amino, A. Miyauchi, Thyroid ultrasonography. World J. Surg. 34(6), 1171–1180 (2010). https://doi.org/10.1007/s00268-009-0211-3
H.J. Lee, D.Y. Yoon, Y.L. Seo, J.H. Kim, S. Baek, K.J. Lim, Y.K. Cho, E.J. Yun, Intraobserver and Interobserver variability in ultrasound measurements of thyroid nodules. J. Ultrasound Med. 37(1), 173–178 (2018). https://doi.org/10.1002/jum.14316
J.Y. Kwak, I. Jung, J.H. Baek, S.M. Baek, N. Choi, Y.J. Choi, S.L. Jung, E.K. Kim, J.A. Kim, J.H. Kim, K.S. Kim, J.H. Lee, J.H. Lee, H.J. Moon, W.J. Moon, J.S. Park, J.H. Ryu, J.H. Shin, E.J. Son, J.Y. Sung, D.G. Na, Korean Society of Thyroid Radiology, Korean Society of Radiology, Image reporting and characterization system for ultrasound features of thyroid nodules: multicentric Korean retrospective study. Korean J. Radiol. 14(1), 110–117 (2013). https://doi.org/10.3348/kjr.2013.14.1.110
S.H. Choi, E.K. Kim, J.Y. Kwak, M.J. Kim, E.J. Son, Interobserver and intraobserver variations in ultrasound assessment of thyroid nodules. Thyroid 20(2), 167–172 (2010). https://doi.org/10.1089/thy.2008.0354
H.K. Su, L.L. Dos Reis, M.A. Lupo, M. Milas, L.A. Orloff, J.E. Langer, E.M. Brett, E. Kazam, S.L. Lee, G. Minkowitz, E.H. Alpert, E.H. Dewey, M.L. Urken, Striving toward standardization of reporting of ultrasound features of thyroid nodules and lymph nodes: a multidisciplinary consensus statement. Thyroid 24(9), 1341–1349 (2014). https://doi.org/10.1089/thy.2014.0110
H.J. Moon, J.Y. Kwak, M.J. Kim, E.J. Son, E.K. Kim, Can vascularity at power Doppler US help predict thyroid malignancy? Radiology 255(1), 260–269 (2010). https://doi.org/10.1148/radiol.09091284
D.W. Kim, S.J. Jung, J.W. Eom, T. Kang, Color Doppler features of solid, round, isoechoic thyroid nodules without malignant sonographic features: a prospective cytopathological study. Thyroid 23(4), 472–476 (2013). https://doi.org/10.1089/thy.2012.0238
H.J. Moon, J.M. Sung, E.K. Kim, J.H. Yoon, J.H. Youk, J.Y. Kwak, Diagnostic performance of gray-scale US and elastography in solid thyroid nodules. Radiology 262(3), 1002–1013 (2012). https://doi.org/10.1148/radiol.11110839
U. Unluturk, M.F. Erdogan, O. Demir, S. Gullu, N. Baskal, Ultrasound elastography is not superior to grayscale ultrasound in predicting malignancy in thyroid nodules. Thyroid 22(10), 1031–1038 (2012). https://doi.org/10.1089/thy.2011.0502
C. Asteria, A. Giovanardi, A. Pizzocaro, L. Cozzaglio, A. Morabito, F. Somalvico, A. Zoppo, US-elastography in the differential diagnosis of benign and malignant thyroid nodules. Thyroid 18(5), 523–531 (2008). https://doi.org/10.1089/thy.2007.0323
Q. Peng, C. Niu, Q. Zhang, M. Zhang, S. Chen, Q. Peng, Mummified thyroid nodules: conventional and contrast-enhanced ultrasound features. J. Ultrasound Med. (2018). https://doi.org/10.1002/jum.14712
A. Lacout, C. Chevenet, P.Y. Marcy, Mummified thyroid syndrome. AJR Am. J. Roentgenol. 206(4), 837–845 (2016). https://doi.org/10.2214/AJR.15.15267
Y. Peng, W. Zhou, W.W. Zhan, S.Y. Xu, Ultrasonographic assessment of differential diagnosis between degenerating cystic thyroid nodules and papillary thyroid microcarcinomas. World J. Surg. 41(10), 2538–2544 (2017). https://doi.org/10.1007/s00268-017-4060-1
Q. Wu, Y. Wang, Y. Li, B. Hu, Z.Y. He, Diagnostic value of contrast-enhanced ultrasound in solid thyroid nodules with and without enhancement. Endocrine 53(2), 480–488 (2016). https://doi.org/10.1007/s12020-015-0850-0
J.Q. Zhou, Y.Y. Song, W.W. Zhan, X. Wei, S. Zhang, R.F. Zhang, Y. Gu, X. Chen, L.Y. Shi, X.M. Luo, L.C. Yang, Q.Y. Li, B.Y. Bai, X.H. Ye, H. Zhai, H. Zhang, X.H. Jia, Y.J. Dong, J.W. Zhang, Z.F. Yang, H.T. Zhang, Y. Zheng, W.W. Xu, L.M. Lai, L.X. Yin, The Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of Chinese Medical Association, The Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound, Thyroid Imaging Reporting and Data System (TIRADS) for ultrasound features of nodules: multicentric retrospective study in China. Endocrine in press (2020)
C.S. Park, S.H. Kim, S.L. Jung, B.J. Kang, J.Y. Kim, J.J. Choi, M.S. Sung, H.W. Yim, S.H. Jeong, Observer variability in the sonographic evaluation of thyroid nodules. J. Clin. Ultrasound 38(6), 287–293 (2010). https://doi.org/10.1002/jcu.20689
C. Cappelli, I. Pirola, E. Gandossi, A.M. Formenti, B. Agosti, M. Castellano, Ultrasound findings of subacute thyroiditis: a single institution retrospective review. Acta Radiol. 55(4), 429–433 (2014). https://doi.org/10.1177/0284185113498721
S.Y. Park, E.K. Kim, M.J. Kim, B.M. Kim, K.K. Oh, S.W. Hong, C.S. Park, Ultrasonographic characteristics of subacute granulomatous thyroiditis. Korean J. Radiol. 7(4), 229–234 (2006). https://doi.org/10.3348/kjr.2006.7.4.229
J.A. Bonavita, Sonographic patterns of benign thyroid nodules. AJR Am. J. Roentgenol. 198(1), W102–103 (2012). https://doi.org/10.2214/AJR.11.7737
V. Virmani, I. Hammond, Sonographic patterns of benign thyroid nodules: verification at our institution. AJR Am. J. Roentgenol. 196(4), 891–895 (2011). https://doi.org/10.2214/AJR.10.5363
J.A. Bonavita, J. Mayo, J. Babb, G. Bennett, T. Oweity, M. Macari, J. Yee, Pattern recognition of benign nodules at ultrasound of the thyroid: which nodules can be left alone? AJR Am. J. Roentgenol. 193(1), 207–213 (2009). https://doi.org/10.2214/AJR.08.1820
I. Zosin, M. Balas, Clinical, ultrasonographical and histopathological aspects in Hashimoto’s thyroiditis associated with malignant and benign thyroid nodules. Endokrynol. Pol. 64(4), 255–262 (2013)
J.D. Iannuccilli, J.J. Cronan, J.M. Monchik, Risk for malignancy of thyroid nodules as assessed by sonographic criteria: the need for biopsy. J. Ultrasound Med. 23(11), 1455–1464 (2004). https://doi.org/10.7863/jum.2004.23.11.1455
H.K. Jung, S.W. Hong, E.K. Kim, J.H. Yoon, J.Y. Kwak, Diffuse sclerosing variant of papillary thyroid carcinoma: sonography and specimen radiography. J. Ultrasound Med. 32(2), 347–354 (2013). https://doi.org/10.7863/jum.2013.32.2.347
Y. Zhang, D. Xia, P. Lin, L. Gao, G. Li, W. Zhang, Sonographic findings of the diffuse sclerosing variant of papillary carcinoma of the thyroid. J. Ultrasound Med. 29(8), 1223–1226 (2010). https://doi.org/10.7863/jum.2010.29.8.1223
J.H. Kim, J.H. Baek, H.K. Lim, H.S. Ahn, S.M. Baek, Y.J. Choi, Y.J. Choi, S.R. Chung, E.J. Ha, S.Y. Hahn, S.L. Jung, D.S. Kim, S.J. Kim, Y.K. Kim, C.Y. Lee, J.H. Lee, K.H. Lee, Y.H. Lee, J.S. Park, H. Park, J.H. Shin, C.H. Suh, J.Y. Sung, J.S. Sim, I. Youn, M. Choi, D.G. Na; Guideline Committee for the Korean Society of Thyroid Radiology, Korean Society of Radiology, 2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology. Korean J. Radiol. 19(4), 632–655 (2018). https://doi.org/10.3348/kjr.2018.19.4.632
H. Kim, H.J. Jung, S.Y. Lee, T.K. Kwon, K.H. Kim, M.W. Sung, J. Hun Hah, Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur. Arch. Otorhinolaryngol. 273(7), 1919–1926 (2016). https://doi.org/10.1007/s00405-015-3724-4
W. Chen, J. Lei, J. You, Y. Lei, Z. Li, R. Gong, H. Tang, J. Zhu, Predictive factors and prognosis for recurrent laryngeal nerve invasion in papillary thyroid carcinoma. Onco Targets Ther. 10, 4485–4491 (2017). https://doi.org/10.2147/OTT.S142799
A. Al Afif, B.A. Williams, M.H. Rigby, M.J. Bullock, S.M. Taylor, J. Trites, R.D. Hart, Multifocal papillary thyroid cancer increases the risk of central lymph node metastasis. Thyroid 25(9), 1008–1012 (2015). https://doi.org/10.1089/thy.2015.0130
L. Genpeng, L. Jianyong, Y. Jiaying, J. Ke, L. Zhihui, G. Rixiang, Z. Lihan, Z. Jingqiang, Independent predictors and lymph node metastasis characteristics of multifocal papillary thyroid cancer. Medicine 97(5), e9619 (2018). https://doi.org/10.1097/MD.0000000000009619
J. Jiang, H. Lu, Immediate surgery might be a better option for subcapsular thyroid microcarcinomas. Int. J. Endocrinol. 2019, 6 (2019). https://doi.org/10.1155/2019/3619864
S. Schenke, P. Seifert, M. Zimny, T. Winkens, I. Binse, R. Gorges, Risk stratification of thyroid nodules using the Thyroid Imaging Reporting and Data System (TIRADS): the omission of thyroid scintigraphy increases the rate of falsely suspected lesions. J. Nucl. Med. 60(3), 342–347 (2019). https://doi.org/10.2967/jnumed.118.211912
W. Zhou, S. Jiang, W. Zhan, J. Zhou, S. Xu, L. Zhang, Ultrasound-guided percutaneous laser ablation of unifocal T1N0M0 papillary thyroid microcarcinoma: preliminary results. Eur. Radiol. 27(7), 2934–2940 (2017). https://doi.org/10.1007/s00330-016-4610-1
D. Teng, G. Sui, C. Liu, Y. Wang, Y. Xia, H. Wang, Long-term efficacy of ultrasound-guided low power microwave ablation for the treatment of primary papillary thyroid microcarcinoma: a 3-year follow-up study. J. Cancer Res. Clin. Oncol. 144(4), 771–779 (2018). https://doi.org/10.1007/s00432-018-2607-7
S.Y. Jeong, J.H. Baek, Y.J. Choi, S.R. Chung, T.Y. Sung, W.G. Kim, T.Y. Kim, J.H. Lee, Radiofrequency ablation of primary thyroid carcinoma: efficacy according to the types of thyroid carcinoma. Int. j. Hyperth. Off. J. Eur. Soc. Hyperth. Oncol. N. Am. Hyperth. Group 1–6 (2018). https://doi.org/10.1080/02656736.2018.1427288
W. Zhou, X. Ni, S. Xu, L. Zhang, Y. Chen, W. Zhan, Ultrasound-guided laser ablation versus microwave ablation for patients with unifocal papillary thyroid microcarcinoma: a retrospective study. Lasers Surg. Med. (2020). https://doi.org/10.1002/lsm.23238
M.H. Ge, D. Xu, A.K. Yang, R.C. Cheng, H. Sun, H.C. Wang, J.Q. Zhang, Z.G. Cheng, Z.Y. wu, Expert consensus on thermal ablation for thyroid benign nodes, microcarcinoma and metastatic cervical lymph nodes (2018 Edition). China Cancer 27(10), 768–773 (2018)
Thyroid Cancer committee of Zhejiang Anti-Cancer Association, Expert consensus on thermal ablation for thyroid benign nodes, microcarcinoma and metastatic cervical lymph nodes (2015 edition). Chin. J. Gen. Surg. 25(7), 944–946 (2016). https://doi.org/10.3978/j.issn.1005-6947.2016.07.002
M. Gao, M. Ge, Q. Ji, R. Cheng, H. Lu, H. Guan, L. Gao, Z. Guo, T. Huang, X. Huang, X. Li, Y. Lin, Q. Liu, X. Ni, Y. Pan, J. Qin, Z. Shan, H. Sun, X. Wang, Z. Xu, Y. Yu, D. Zhao, N. Zhang, S. Zhang, Y. Zheng, J. Zhu, D. Li, X. ZhengChinese Association of Thyroid Oncology (CATO), Chinese Anti-Cancer Association, 2016 Chinese expert consensus and guidelines for the diagnosis and treatment of papillary thyroid microcarcinoma. Cancer Biol. Med 14(3), 203–211 (2017). https://doi.org/10.20892/j.issn.2095-3941.2017.0051
Acknowledgements
We would like to express our sincere gratitude to all doctors from the Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound (CAAU) member hospitals who provided ultrasound data on thyroid nodules for this study.
The Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of the Chinese Medical Association
BaoMing Luo24, BeiJian Huang25, ChaoYang Wen26, ChengRong Mi27, DaoZhong Huang28, EnSheng Xue29, Gang Wu30, GuoQing Du31, HaiTao Ran32, HuiJuan Xiang33, JiaAn Zhu34, Jian Wang35, JianChu Li36, Jie Tang37, Jing Li38, JingChun Yang39, Lei Zhang39, LiGang Cui40, LingYun Bao41, LiXue Yin42, Man Lu43, Mei Zhu44, Min Chen45, Nima Yuzhen46, PengFei Zhang47, Rong Wu48, RuiJun Guo49, ShaoYun Hao24, ShiBao Fang50, Tao Chen51, WeiWei Zhan52, Ying Zhu53, YingJia Li54, YongPing Lu55, YouBin Deng28, YuanYi Zheng56, Yue Chen57, YuKun Luo37, YuLan Peng58
The Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound
Bai BaoYan59, Cai YuanJin60, Chang Xin61, Che Guihua62, Chen Fu63, Chen HongTian64, Chen HongYan65,66, Chen HuiPin67, Chen Jiehuan68, Chen NianQiao69, Chen Wu35, Chen Xinguang70, Chen XiuPing71, Cui Guanghe72, Dai LiPing73, Deng XueDong74, Dong LiLi75, Du Gang76, Fang Chao77, Fang FengKai78, Fei ZhengDong79, Feng LiLi80, Fu Jian81, Guan Ling82, Guo JianQin83, Han Wen84, He Nianan85, He ShaoZheng86, He XueMei87, Hou AiQin88, Hu Jie89, Hu LiYan90, Huang DingWei91, Huang JianYuan92, Huang Li93, Huang PeiPei94, Huang WeiWei95, Jia LiQiong96, Jiang Xinhui97, Kang huiLi98, Kong XiangChong99, Lei XiaoQing100, Li AnYang101, Li Chen102, Li Cheng103, Li ChuanYin104, Li Dong105, Li HaiYan106, Li HongMei107, Li HuiWen108, Li JianXin109, Li Ning110, Li QiaoYing111, Li QinYing112, Li Tao113, Li WenDong114, Li XingYun115, Li Zhao116, Liang GuoSheng117, Lin Jie118, Liu Aihua119, Liu HongMin120, Liu Jia121, Liu Kun122, Liu YanChao123, Lou KeXin124, Lu YeJun125, Mao Feng126, Miao Juan127, Ni XueJun128, Pan XiaoJie129, Pang Yun130, Peng Mei131, Peng ZhenYi72, Pi YanMin132, Qi TingYue133, Qin QianMiao134, Qing Shunhua135, Qu JianFeng136, Ren Jinhe137, RenaguLi AiSha138, Ru RongRong139, Shen Tao140, Shi HongWei141, Shi Jie142, Shi LiYing143, Shou JinDuo144, Song LinLin145, Su DeMin146, Sun AnYi147, Sun Zhuogui148, Tang Binhui149, Tang Li Na150, Wan Qing151, Wang Fang152,153, Wang Jing154, Wang JinPing155, Wang Li156, Wang Wei157, Wang XinFang158, Wang YaLi159, Wang YanBin160, Wang YanQing161, Wang YanZhen162, Wang YingChun163, Wang YuanSheng46, Wang ZhaoRui164, Wu ChangJun165, Wu HaiYan166, Wu Jing167, Wu JinYu168, Wu Liang169, Wu LinSong170, Wu Qing171, Wu Tao172, Wu Ting74,173, Wu WenJing174, Wu ZhiLing175, Wu ZhongQiu176, Xiao LiFang177, Xie ChuanWen178, Xie Xiaohong179, Xu Quan180, Xue Dan181, Yan JingBin182, Yan JiPing183, Yang JianQing184, Yang Jie185, Yang QingYa186, Yang XiaoQing187, Yang XueWen188, Yang Yan189, Yang YingMei190, Yang Yinguang191, Ye Xinhua192, Ye YuQuan193, You Tao194, Yu Liang195, Yu XiaoQin196, Yuan Hui197, Yuan Zhihong74, Ze Liang198, Zeng Shue199, Zhang Hui200, Zhang Jian201, Zhang JianLei202, Zhang LiJuan203, Zhang LiLi204, Zhang Na205, Zhang PanPan206, Zhang Tong207, Zhang WenJun208, Zhang XiaoDong209, Zhang Yan210,211, Zhang Yuhong212, Zhang Yuhua213, Zhang YunFei214, Zhang ZiZhen32, Zhang ZiZhen215, Zhao Feng216, Zhao Li217, Zhao Yu218, Zhou Hong219, Zhou JianQiao103, Zhou Na220, Zhou Peng221, Zhou Ruhai222, Zhou XianLi31, Zhou YiBo223, Zhu Bin224, Zhu LiSha225, Zhu Zheng226, Zou Bao227
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of The Superficial Organ and Vascular Ultrasound Group of the Society of Ultrasound in Medicine of the Chinese Medical Association and The Chinese Artificial Intelligence Alliance for Thyroid and Breast Ultrasound are listed below Acknowledgements.
Rights and permissions
About this article
Cite this article
Zhou, J., Yin, L., Wei, X. et al. 2020 Chinese guidelines for ultrasound malignancy risk stratification of thyroid nodules: the C-TIRADS. Endocrine 70, 256–279 (2020). https://doi.org/10.1007/s12020-020-02441-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02441-y