Abstract
Purpose
The identification of somatic mutations in cancer specimens enables detection of molecular markers for personalized treatment. We recently developed a novel molecular assay and evaluated its clinical performance as an ancillary molecular method for indeterminate thyroid nodule cytology. Herein we describe the analytical validation of the novel targeted next-generation sequencing (NGS) assay in thyroid samples from different sources.
Methods
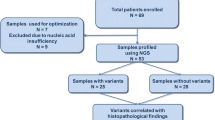
We present validation data of a novel NGS-based panel on 463 thyroid samples, including 310 fine-needle aspiration (FNA) specimens from different sources (FNA collected in preservative solution, liquid-based, and stained smears), 10 fresh frozen, and 143 formalin-fixed paraffin-embedded (FFPE) thyroid tissue specimens. Sequencing performance in the different samples was evaluated along with reproducibility, repeatability, minimum nucleic acid input to detect variants, and analytical sensitivity of the assay.
Results
All thyroid samples achieved high sequencing performance, with a mean base coverage depth ranging from 2228 × (in liquid-based FNA) to 3661 × (in FNA stained smears), and coverage uniformity ranging from 86% (in FFPE) to 95% (in FNA collected in preservative solution), with all target regions covered above the minimum depth required to call a variant (500×). The minimum nucleic acid input was 1 ng. Analytic sensitivity for mutation detection was 2–5% mutant allele frequency.
Conclusions
This validation study of a novel NGS-based assay for thyroid nodules demonstrated that the assay can be reliably used on multiple thyroid sample types, including FNA from different sources and FF and FFPE thyroid samples, thus providing a robust and reliable assay to genotype thyroid nodules, which may improve thyroid cancer diagnosis and care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid carcinoma accounts for the majority of endocrine cancers and its incidence has increased over the past 30 years, also due to overdiagnosis [1, 2]. Thyroid cancers generally present as asymptomatic nodules and diagnosis is usually based on fine-needle aspiration (FNA) cytology [3], which is inconclusive in up to 30% of cases [4].
Advances in the understanding of thyroid cancer genetics and in high-throughput technologies have substantially reduced the “dark matter” of the thyroid cancer genome, thus providing novel molecular markers of potential diagnostic, prognostic, and therapeutic significance [5].
Targeted next-generation sequencing (NGS) offers a convenient and cost-effective technique to detect mutations even in FNA specimens [3, 6]. We developed a dual-component molecular assay as an ancillary method for indeterminate thyroid FNA specimens that targets thyroid cancer-related somatic mutations in 23 genes [7,8,9] and one thyroid cancer-related microRNA [10, 11]. Clinical utility in liquid-based thyroid FNA samples has already been demonstrated in cytologically indeterminate thyroid nodules [12].
We report the analytical validation of the NGS-based assay for detecting novel and known somatic mutations in thyroid cancer. Sequencing performance was evaluated on multiple sample types, including FNA thyroid samples from different sources (collected in preservative solution, liquid-based, and stained smears), and fresh frozen (FF) and formalin-fixed paraffin-embedded (FFPE) thyroid tissue specimens. Assay reproducibility and robustness was described.
Materials and methods
Sample collection
Thyroid samples were collected and analyzed with local ethics committee approval. Written informed consent of all participants was obtained according to the Declaration of Helsinki.
Clinical samples for mutational analysis included: (1) FNA samples collected in tubes containing nucleic acid preservative solution (RNAlater; Thermo Fisher Scientific), (2) residual cytological material from thyroid nodule aspirates processed with the liquid-based cytology ThinPrep5000™ method (Hologic Co.) as previously described [13], and (3) cytology smear-stained slides.
Other samples used for analytical validation of the assay included FF and FFPE samples from surgically removed thyroid cancer, thyroid nontumor (Nthy-ori 3–1) and cancer cell lines (BCPAP and TPC1, two human papillary thyroid cancer-derived cell lines characterized by BRAFV600E mutation and CCDC6-RET gene fusion, respectively) [14], commercial reference materials (control DNA from CEPH Individual 1347-02, Thermo Fisher Scientific; control RNA from 64 normal thyroids, Clontech), and blood specimen from a healthy individual.
Details on cytological and histological classification of FNA samples and FF and FFPE tissues were included in Supplementary Table 1.
Nucleic acid isolation
AllPrep DNA/RNA Micro Kit (QIAGEN) was used to simultaneously isolate nucleic acid from FNA samples (RNAlater and liquid-based) and cell lines following manufacturer’s instructions [12].
RecoverAll Total Nucleic Acid Isolation Kit (Thermo Fisher Scientific) was used for nucleic acid isolation from FFPE tissue and FNA stained smear samples following manufacturer’s instructions [15]. To remove deaminated cytosine (uracil) bases, DNA from FFPE samples was treated with uracil-DNA glycosylase (UDG) (Thermo Fisher Scientific) following manufacturer’s instructions.
Trizol reagent (Thermo Fisher Scientific) was used for nucleic acid isolation from FF tissue [15]. QIAamp RNA Blood Mini Kit (Qiagen) was used for RNA isolation from blood following manufacturer’s recommendations.
Nucleic acids were measured using fluorescence-based Qubit® quantification assays for double-stranded DNA and RNA (Thermo Fisher Scientific).
NGS
Using targeted amplification-based NGS technology, the assay tested for single-nucleotide variants (SNVs)/small indels in 19 genes, 204 gene fusions of 7 genes with 72 fusion partners, and expression of 12 control genes to estimate adequate cellularity and cell quality (follicular, parafollicular, parathyroid cells) [12, 16]. Two libraries were created from 15 ng of DNA and 10 ng of RNA using Ion AmpliSeq™ Library Kit Plus and Ion Xpress™ Barcode Adapter 1–96 Kit following manufacturer’s instructions (Thermo Fisher Scientific). Pooled libraries were clonally amplified on the Ion One Touch2 System and sequenced on Ion Gene Studio S5 (Thermo Fisher Scientific). DNA data were analyzed with Torrent Suite v.5.10 software and annotated with IonReporter 5.12 and wANNOVAR web servers. RNA data were analyzed with Torrent Suite v.5.10 and IonReporter 5.12 software (Thermo Fisher Scientific) following analysis workflow for gene fusion detection [12].
Assay accuracy was evaluated by analyzing patient samples (FNA, FFPE, and FF), thyroid nontumor and cancer cell lines (NthyOri, BCPAP, and TPC1) [14] and commercial reference materials (control DNA/RNA) according to NGS-based oncology panel validation guidelines [17, 18]. We evaluated assay sequencing performance in different sample types, reproducibility, repeatability, minimum input quantity to detect variants, and analytical sensitivity.
Results
Sequencing performance
Sequencing performance was assessed from different sample types, including RNAlater (n = 160), liquid-based (n = 147), and stained smear (n = 3) FNA thyroid samples and FF (n = 10) and FFPE (n = 143) thyroid tissue specimens. All samples achieved high sequencing performance as assessed by average base coverage depth (Fig. 1a) and uniformity (Fig. 1b). Liquid-based thyroid FNA specimens showed the lowest base coverage depth (equal to 2680×), while FFPE samples showed the lowest coverage uniformity (86% vs. >94% in all other sample sources). However, all target regions were covered above 500×, that is the minimal depth of coverage required to call a variant.
Reproducibility and repeatability
Replicate (within run) and repeat (between run) testing were performed with six thyroid cancer samples (two FNA, two FFPE, two FF) with known genetic variants previously assessed by orthogonal methods [i.e., Sanger Sequencing for SNVs (BRAF p.V600E, and RET p.C634R) and reverse transcription polymerase chain reaction for gene fusions (PAX8-PPARG and RET-NCOA4)]. Each sample was assayed 3× within a single run and between runs. Expected DNA and RNA variants were detected in all sample types tested across the three intra and interassay replicates, with minimum variation in allele frequency and mapped reads (Supplementary Table 2a, b). These results show highly reproducible DNA variant and RNA fusion detection.
Minimum acceptable nucleic acid input to detect DNA and RNA variants
To identify the minimum input of nucleic acid necessary to reliably detect point mutations and gene fusions, four biological samples were tested (two FNA, two FFPE) at an amount of nucleic acid ranging from 1 to 10 ng. The assay was able to correctly identify genetic alterations (one SNV, BRAF p.V600E, and two gene fusions, RET-NCOA4 and HOOK3-RET) and classify them as positive in 100% of tested samples, both those isolated from thyroid FNA and from FFPE, indicating that 1 ng of nucleic acids is a well-tolerated quantity by the molecular test (Supplementary Table 3).
Analytical sensitivity
To determine the analytical sensitivity of the assay, BCPAP cells with homozygous BRAF p.V600E mutation and TPC1 cells with CCDC6-RET gene fusion were serially diluted in control samples negative for the genetic alterations.
The assay detected point mutations down to 5% allelic frequency. However, visual inspection of the aligned reads in the Integrative Genomics Viewer also revealed BRAF mutations at lower allele frequency (2%) (Supplementary Table 4).
Gene fusions were detected down to a dilution of 1:39 (2.5%) (Supplementary Table 5), both when thyroid tumor cells were diluted in nontumor thyroid cells (Nthy-ori cells) and in RNA from whole blood (Supplementary Table 5), indicating that the assay was not affected by interfering material.
Discussion
We describe the analytical validation of a novel NGS-based assay for detecting novel and known somatic molecular alterations in thyroid cancer. Clinical utility of the assay previously demonstrated a high sensitivity and negative predictive value in liquid-based FNA thyroid samples [12]. Here, we demonstrate that the assay can be reliably used on various sample sources that can be used as starting material, including liquid-based FNA samples, FNA samples collected in nucleic acid preservative solution, FNA stained smears, and FF and FFPE thyroid tissue samples. The assay employs relatively low amounts of nucleic acid and provides simultaneous high-accuracy screening of SNVs, indels, and gene fusions, thus providing a valuable tool for genotyping thyroid nodules.
The assay uses an amplification-based approach for targeted enrichment of genomic regions. This allows a low nucleic acid input, which is particularly important for FNA samples and limited biopsy specimens. Although recommended nucleic acid input for the AmpliSeqTM protocol (Thermo Fisher Scientific) is 10 ng, a large proportion of FNA samples have input below the required threshold [19]. Here we demonstrate that 1 ng of nucleic acid is sufficient for molecular assay. At this amount, the assay correctly identifies genetic alterations in 100% of analyzed samples.
The assay is also compatible with FFPE tissue. Testing of these tissues may be useful for refining the pathological diagnosis [2, 20] or the risk of persistence and recurrence [21]. FFPE preservation methods can lead to cytosine deamination within isolated DNA and to highly degraded nucleic acid isolation, resulting in decreased sequencing quality [22]. However, DNA treatment with UDG before target amplification can enzymatically remove deaminated cytosines [23]. Moreover, an amplification-based assay allows enrichment of short DNA. All tested samples had high sequencing performance. Although base coverage uniformity was lower in FFPE specimens, all target regions were covered above 500×, the minimum depth required to call a variant.
In summary, this validation study of a novel NGS-based assay demonstrates its applicability in multiple thyroid sample types, including FNA from different sources and FF and FFPE thyroid samples, thus providing a robust and reliable method to genotype thyroid nodules. This approach may aid clinical decision making on the basis of mutational signatures. As preoperative test, an NGS-based assay targeting thyroid cancer-related somatic mutations can increase diagnostic yield of FNA cytology. In addition to its diagnostic utility, a comprehensive mutational assay may contribute to refine the risk of recurrence of thyroid cancer patients [21] and to predict the more advanced cancers through the simultaneous detection of multiple mutations that frequently co-occur in aggressive cancers [5]. Finally, mutational profiling in primary and metastatic tissues may guide therapy selection and suggest novel targeted treatment options for patients who failed to respond to standard-of-care therapy.
References
C.D.Seib, J.A.Sosa, Evolving understanding of the epidemiology of thyroid cancer. Endocrinol. Metab. Clin. N. Am 48, 23–35 (2019)
S. Filetti, C. Durante, D. Hartl, S. Leboulleux, L.D. Locati, K. Newbold, M.G. Papotti, A. Berruti, Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30, 1856–1883 (2019). https://doi.org/10.1093/annonc/mdz400
D. Tumino, G. Grani, M. Di Stefano, M. Di Mauro, M. Scutari, T. Rago, L. Fugazzola, M.G. Castagna, F. Maino, Nodular thyroid disease in the era of precision medicine. Front. Endocrinol. (Lausanne) 10, 907–916 (2020). https://doi.org/10.3389/fendo.2019.00907
M. Bongiovanni, A. Spitale, W.C. Faquin, L. Mazzucchelli, Z.W. Baloch, The bethesda system for reporting thyroid cytopathology: a meta-analysis. Acta Cytol. 56, 333–339 (2012). https://doi.org/10.1159/000339959
A. Prete, P. Borges. de Souza, S. Censi, M. Muzza, N. Nucci, M. Sponziello, Update on fundamental mechanisms of thyroid Cancer. Front. Endocrinol. (Lausanne) 11, 102–111 (2020). https://doi.org/10.3389/fendo.2020.00102
Y.E. Nikiforov, Role of molecular markers in thyroid nodule management: then and now. Endocr. Pract. 23, 979–988 (2017). https://doi.org/10.4158/EP171805.RA
N. Agrawal, R. Akbani, B.A. Aksoy, A. Ally, H. Arachchi, S.L. Asa, J.T. Auman, M. Balasundaram, S. Balu, S.B. Baylin, M. Behera, B. Bernard, R. Beroukhim, J.A. Bishop, A.D. Black, T. Bodenheimer, L. Boice, M.S. Bootwalla, J. Bowen, R. Bowlby, C.A. Bristow, R. Brookens, D. Brooks, R. Bryant, E. Buda, Y.S.N. Butterfield, T. Carling, R. Carlsen, S.L. Carter, S.E. Carty, T.A. Chan, A.Y. Chen, A.D. Cherniack, D. Cheung, L. Chin, J. Cho, A. Chu, E. Chuah, K. Cibulskis, G. Ciriello, A. Clarke, G.L. Clayman, L. Cope, J.A. Copland, K. Covington, L. Danilova, T. Davidsen, J.A. Demchok, D. DiCara, N. Dhalla, R. Dhir, S.S. Dookran, G. Dresdner, J. Eldridge, G. Eley, A.K. El-Naggar, S. Eng, J.A. Fagin, T. Fennell, R.L. Ferris, S. Fisher, S. Frazer, J. Frick, S.B. Gabriel, I. Ganly, J. Gao, L.A. Garraway, J.M. Gastier-Foster, G. Getz, N. Gehlenborg, R. Ghossein, R.A. Gibbs, T.J. Giordano, K. Gomez-Hernandez, J. Grimsby, B. Gross, R. Guin, A. Hadjipanayis, H.A. Harper, D.N. Hayes, D.I. Heiman, J.G. Herman, K.A. Hoadley, M. Hofree, R.A. Holt, A.P. Hoyle, F.W. Huang, M. Huang, C.M. Hutter, T. Ideker, L. Iype, A. Jacobsen, S.R. Jefferys, C.D. Jones, S.J.M. Jones, K. Kasaian, E. Kebebew, F.R. Khuri, J. Kim, R. Kramer, R. Kreisberg, R. Kucherlapati, D.J. Kwiatkowski, M. Ladanyi, P.H. Lai, P.W. Laird, E. Lander, M.S. Lawrence, D. Lee, E. Lee, S. Lee, W. Lee, K.M. Leraas, T.M. Lichtenberg, L. Lichtenstein, P. Lin, S. Ling, J. Liu, W. Liu, Y. Liu, V.A. LiVolsi, Y. Lu, Y. Ma, H.S. Mahadeshwar, M.A. Marra, M. Mayo, D.G. McFadden, S. Meng, M. Meyerson, P.A. Mieczkowski, M. Miller, G. Mills, R.A. Moore, L.E. Mose, A.J. Mungall, B.A. Murray, Y.E. Nikiforov, M.S. Noble, A.I. Ojesina, T.K. Owonikoko, B.A. Ozenberger, A. Pantazi, M. Parfenov, P.J. Park, J.S. Parker, E.O. Paull, C.S. Pedamallu, C.M. Perou, J.F. Prins, A. Protopopov, S.S. Ramalingam, N.C. Ramirez, R. Ramirez, B.J. Raphael, W.K. Rathmell, X. Ren, S.M. Reynolds, E. Rheinbay, M.D. Ringel, M. Rivera, J. Roach, A.G. Robertson, M.W. Rosenberg, M. Rosenthal, S. Sadeghi, G. Saksena, C. Sander, N. Santoso, J.E. Schein, N. Schultz, S.E. Schumacher, R.R. Seethala, J. Seidman, Y. Senbabaoglu, S. Seth, S. Sharpe, K.R.M. Shaw, J.P. Shen, R. Shen, S. Sherman, M. Sheth, Y. Shi, I. Shmulevich, G.L. Sica, J.V. Simons, R. Sinha, P. Sipahimalani, R.C. Smallridge, H.J. Sofia, M.G. Soloway, X. Song, C. Sougnez, C. Stewart, P. Stojanov, J.M. Stuart, S.O. Sumer, Y. Sun, B. Tabak, A. Tam, D. Tan, J. Tang, R. Tarnuzzer, B.S. Taylor, N. Thiessen, L. Thorne, V. Thorsson, R.M. Tuttle, C.B. Umbricht, D.J. Van Den Berg, F. Vandin, U. Veluvolu, R.G.W. Verhaak, M. Vinco, D. Voet, V. Walter, Z. Wang, S. Waring, P.M. Weinberger, N. Weinhold, J.N. Weinstein, D.J. Weisenberger, D. Wheeler, M.D. Wilkerson, J. Wilson, M. Williams, D.A. Winer, L. Wise, J. Wu, L. Xi, A.W. Xu, L. Yang, L. Yang, T.I. Zack, M.A. Zeiger, D. Zeng, J.C. Zenklusen, N. Zhao, H. Zhang, J. Zhang, J. Zhang, W. Zhang, E. Zmuda, L. Zou, Integrated genomic characterization of papillary thyroid carcinoma. Cell. 159, 676–690 (2014). https://doi.org/10.1016/j.cell.2014.09.050
I. Landa, T. Ibrahimpasic, L. Boucai, R. Sinha, J.A. Knauf, R.H. Shah, S. Dogan, J.C. Ricarte-Filho, G.P. Krishnamoorthy, B. Xu, N. Schultz, M.F. Berger, C. Sander, B.S. Taylor, R. Ghossein, I. Ganly, J.A. Fagin, Genomic and transcriptomic hallmarks of poorly-differentiated and anaplastic thyroid cancers. J. Clin. Investig. 126, 1052–1066 (2016). https://doi.org/10.1172/JCI85271
M. Sponziello, S. Benvenuti, A. Gentile, V. Pecce, F. Rosignolo, A.R. Virzì, M. Milan, P.M. Comoglio, E. Londin, P. Fortina, A. Barnabei, M. Appetecchia, F. Marandino, D. Russo, S. Filetti, C. Durante, A. Verrienti, Whole exome sequencing identifies a germline MET mutation in two siblings with hereditary wild-type RET medullary thyroid cancer. Hum. Mutat. 39, 371–377 (2018). https://doi.org/10.1002/humu.23378
F. Rosignolo, L. Memeo, F. Monzani, C. Colarossi, V. Pecce, A. Verrienti, C. Durante, G. Grani, L. Lamartina, S. Forte, D. Martinetti, D. Giuffrida, D. Russo, F. Basolo, S. Filetti, M. Sponziello, MicroRNA-based molecular classification of papillary thyroid carcinoma. Int. J. Oncol. 50, 1767–1777 (2017). https://doi.org/10.3892/ijo.2017.3960
F. Rosignolo, M. Sponziello, L. Giacomelli, D. Russo, V. Pecce, M. Biffoni, R. Bellantone, C.P. Lombardi, L. Lamartina, G. Grani, C. Durante, S. Filetti, A. Verrienti, Identification of thyroid-associated serum microRNA profiles and their potential use in thyroid cancer follow-up. J. Endocr. Soc. 1, 3–13 (2017). https://doi.org/10.1210/js.2016-1032
M. Sponziello, C. Brunelli, A. Verrienti, G. Grani, V. Pecce, L. Abballe, V. Ramundo, G. Damante, D. Russo, C.P. Lombardi, C. Durante, E.D. Rossi, P. Straccia, G. Fadda, S. Filetti. Performance of a dual-component molecular assay in cytologically indeterminate thyroid nodules. Endocrine. (2020). https://doi.org/10.1007/s12020-020-02271-y
P. Straccia, C. Brunelli, E.D. Rossi, P. Lanza, M. Martini, T. Musarra, C.P. Lombardi, A. Pontecorvi, G. Fadda, The immunocytochemical expression of VE‐1 (BRAFV600E‐related) antibody identifies the aggressive variants of papillary thyroid carcinoma on liquid‐based cytology. Cytopathology 30, 460–467 (2019). https://doi.org/10.1111/cyt.12690
I. Landa, N. Pozdeyev, C. Korch, L.A. Marlow, R.C. Smallridge, J.A. Copland, Y.C. Henderson, S.Y. Lai, G.L. Clayman, N. Onoda, A.C. Tan, M.E.R. Garcia-Rendueles, J.A. Knauf, B.R. Haugen, J.A. Fagin, R.E. Schweppe, Comprehensive genetic characterization of human thyroid cancer cell lines: a validated panel for preclinical studies. Clin. Cancer Res. 25, 3141–3151 (2019). https://doi.org/10.1158/1078-0432.CCR-18-2953
V. Maggisano, M. Celano, G.E. Lombardo, S.M. Lepore, M. Sponziello, F. Rosignolo, A. Verrienti, F. Baldan, E. Puxeddu, C. Durante, S. Filetti, G. Damante, D. Russo, S. Bulotta, Silencing of hTERT blocks growth and migration of anaplastic thyroid cancer cells. Mol. Cell. Endocrinol. 448, 34–40 (2017). https://doi.org/10.1016/j.mce.2017.03.007
M. Sponziello, G. Silvestri, A. Verrienti, A. Perna, F. Rosignolo, C. Brunelli, V. Pecce, E.D. Rossi, C.P. Lombardi, C. Durante, S. Filetti, G. Fadda, A novel nonsense EIF1AX mutation identified in a thyroid nodule histologically diagnosed as oncocytic carcinoma. Endocrine 62, 492–495 (2018). https://doi.org/10.1007/s12020-018-1611-7
L.J. Jennings, M.E. Arcila, C. Corless, S. Kamel-Reid, I.M. Lubin, J. Pfeifer, R.L. Temple-Smolkin, K.V. Voelkerding, M.N. Nikiforova, Guidelines for validation of next-generation sequencing–based oncology panels: a joint consensus recommendation of the association for Molecular Pathology and College of American Pathologists. J. Mol. Diagn. 19, 341–365 (2017). https://doi.org/10.1016/j.jmoldx.2017.01.011
S. Roy-Chowdhuri, P. Pisapia, M. Salto-Tellez, S. Savic, M. Nacchio, D. de Biase, G. Tallini, G. Troncone, F. Schmitt, Invited review—next-generation sequencing: a modern tool in cytopathology. Virchows Arch. 475, 3–11 (2019). https://doi.org/10.1007/s00428-019-02559-z
S. Roy-Chowdhuri, J. Stewart, Preanalytic variables in cytology: lessons learned from next-generation sequencing—the MD Anderson experience. Arch. Pathol. Lab. Med. 140, 1191–1199 (2016). https://doi.org/10.5858/arpa.2016-0117-RA
L. Lamartina, G. Grani, C. Durante, S. Filetti, Recent advances in managing differentiated thyroid cancer. F1000Res 7, 86 (2018). https://doi.org/10.12688/f1000research.12811.1
L. Lamartina, G. Grani, C. Durante, I. Borget, S. Filetti, M. Schlumberger, Follow-up of differentiated thyroid cancer—what should (and what should not) be done. Nat. Rev. Endocrinol. 14, 538–551 (2018). https://doi.org/10.1038/s41574-018-0068-3
S. Kim, C. Park, Y. Ji, D.G. Kim, H. Bae, M. van Vrancken, D.H. Kim, K.M. Kim, Deamination effects in formalin-fixed, paraffin-embedded tissue samples in the era of precision medicine. J. Mol. Diagn. 19, 137–146 (2017). https://doi.org/10.1016/j.jmoldx.2016.09.006
M. Serizawa, T. Yokota, A. Hosokawa, K. Kusafuka, T. Sugiyama, Y. Tsubosa, H. Yasui, T. Nakajima, Y. Koh, The efficacy of uracil DNA glycosylase pretreatment in amplicon-based massively parallel sequencing with DNA extracted from archived formalin-fixed paraffin-embedded esophageal cancer tissues. Cancer Genet. 208, 415–427 (2015). https://doi.org/10.1016/j.cancergen.2015.05.001
Funding
The study was supported by “Sapienza” University of Rome (grant RP11916B8919C921 to M.S.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures involving humans were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee of Azienda Universitaria Policlinico Umberto I, Rome, Italy; Prot. 806/16, Rif. 4233) and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Written informed consent was obtained from all subjects included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Verrienti, A., Pecce, V., Abballe, L. et al. Analytical validation of a novel targeted next-generation sequencing assay for mutation detection in thyroid nodule aspirates and tissue. Endocrine 69, 451–455 (2020). https://doi.org/10.1007/s12020-020-02372-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-020-02372-8