Abstract
Thyroid cancers (TCs) are the most frequent endocrine malignancy with an unpredictable fast-growing incidence, especially in females all over the world. Fine-needle aspiration biopsy (FNAB) analysis is an accurate diagnostic method for detecting thyroid nodules and classification of TC. Though simplicity, safety, and accuracy of FNAB, 15–30% of cases are indeterminate, and it is not possible to determine the exact cytology of the specimen. This demands the need for innovative methods capable to find crucial biomarkers with adequate sensitivity for diagnosis and prediction in TC researches. Cancer-based metabolomics is a vast emerging field focused on the detection of a large set of metabolites extracted from biofluids or tissues. Using analytical chemistry procedures allows for the potential recognition of cancer-based metabolites for the purposes of advancing the era of personalized medicine. Nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry (MS) coupled with separation techniques e.g., gas chromatography (GC) and liquid chromatography (LC) are the main approaches for metabolic studies in cancers. The immense metabolite profiling has provided a chance to discover novel biomarkers for early detection of thyroid cancer and reduce unnecessary aggressive surgery. In this review, we recapitulate the recent advances and developed methods of diverse metabolomics tools and metabolic phenotypes of thyroid cancer, following a brief discussion of recent challenges in the thyroid cancer diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer (TC) is the most common endocrine disorder. The worldwide incidence of this type of cancer has been dramatically growing in recent years, with the average age of the individuals at diagnosis being 30–39 years [1]. It has become the fifth most common cancer in females with the global highest incidence rate (three times higher than men) [2,3,4]. The greater prevalence of thyroid cancer in females suggests that hormonal factors may be involved in its development [5]. Noteworthy, thyroid cancers often appear as thyroid nodules, therefore, the diagnosis and follow-up of this type of cancer is associated with thyroid nodules. This type of cancer may occurs due to the accumulation of a variety of genetic and epigenetic changes that lead to activation of some oncogenes and inactivation of the tumor suppressor genes [6]. Radiation exposure in childhood, a history of goiter, and a history of benign nodules are also strong risk factors that are considered to cause thyroid cancer [7, 8]. However, the main causes of this malignancy are still unclear.
Based on the histopathological characteristics, thyroid cancers (TCs) are categorized into four main types; papillary thyroid cancer (PTC), follicular thyroid cancer (FTC), medullary thyroid cancer (MTC), and anaplastic thyroid cancer (ATC). PTC accounts for 70–80% of thyroid cancers making it the main histological type of TCs. Due to its slow growth and metastasis, it is less invasive than other types of thyroid cancers. Approximately 14% of thyroid cancers can be attributed to FTC. It is more invasive than PTC and may be associated with iodine deficiency. Both PTC and FTC are originated from follicular thyroid epithelium cells. Medullary thyroid cancer accounts for roughly 3% of thyroid cancers, which arise from parafollicular C cells. The main feature of this cancer is excess production of calcitonin which is used as a tumor marker to detect this type of cancer. Anaplastic thyroid cancer is the most aggressive and deadly form of thyroid cancer. It rapidly metastasizes to the lymph nodes and the distant area. It accounts for ~2% of thyroid cancers [9].
The widely used and efficient method for the diagnosis of thyroid nodules is fine-needle aspiration biopsy (FNAB) under ultrasound control followed by cytological evaluation [10]. According to the Bethesda System for reporting thyroid cytopathology, the FNAB results are classified into six different categories including; (I) non-diagnostic or unsatisfactory, (II) benign, (III) atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS), (IV) follicular neoplasm (FN) or suspicious for FN, (V) suspicious for malignancy, and (VI) malignant [11].
Based on the abovementioned general categorization, ~15–30% of all FNABs have low accuracy and reliability as cannot differentiate between benign and malignant lesions [12]. Therefore, thyroid FNABs have to be repeated for indeterminate lesions [13, 14]. In some cases, lobectomy or thyroidectomy is the only option for diagnosis and treatment [15].
Discovery of new methods and novel biomarkers are of growing needs and could eliminate the unnecessary repetition of FNABs and surgical procedures. They could also make the treatment procedure more specific and targeted compared with other aggressive and costly treatments.
For this purpose, the analysis of BRAF and RAS mutations in FNAB samples has been recently used to improve the diagnostic accuracy of FNAB cytology results. A meta-analysis study indicated that the addition of the BRAF V600E test to the standard FNAB cytology increased the diagnostic sensitivity and reduced the false-negative results, especially in indeterminate nodules classified as suspicious for malignant cells (SMC) [16]. However, the BRAF V600E evaluation in follicular suspicious lesions was doubtful and lacked accuracy in diagnosis. In addition, the results of RAS tests have shown lower sensitivity in some studies [17].
There are also promising markers that have been reported in some studies using immunocytochemical analysis and other genetic tests as supplements to FNAB cytology analysis of indeterminate lesions. These markers included: miR-151-5p, miR-222, let-7e, galectin-3, E-cadherin, fibronectin, CD44v6, thyroid transcription factor 1 (TTF-1), Cbp/p300-interacting transactivator1 (CITED1), thyroglobulin, calcitonin, carcinoembryonic antigen (CEA), p27, cyclin D1, cytokeratin 19, thyroid peroxidase, Hector Battifora mesothelial-1 (HBME-1), beta-catenin, and p53 [18,19,20,21].
Although the above-mentioned methods and obtained markers have shown usefulness, they have had intrinsic limitations, particularly in terms of low sensitivity, negative predictive value, and high costs. The OMICS tools are strong and widely considered as efficient methods in cancer research. These include genomics, transcriptomics, proteomics, and metabolomics, which trail and complement each other with simultaneously elevated gene expression and measuring protein and metabolite in different biological samples.
Among these, metabolomics has been the newest emerging one form of omics that can provide an overview of the physiological state of the biological system with unconditional connectivity with the phenotype [22]. Changes in metabolism provide new insight for the diagnosis and prognosis of different diseases. Subsequently, patients can be stratified into different groups based on a low- or high-risk profile of developing the disease or monitoring metabolic responses to therapeutic interventions. In addition, metabolomics has the potential to develop a new understanding of phenotypic changes resulting from genetic changes and environmental impacts [23].
As neoplastic cells have a unique metabolic phenotype in relation to cancer development, the identification of metabolic pathways through metabolism can be effective in identifying cancer biomarkers and discovering therapeutic goals.
Lipidomics is another emerging approach in tumor characterization, which is known as a subset of metabolomics. Lipids play essential roles in cellular structures and functions, including cellular barriers, membrane matrices, signaling, and energy storage [24]. They constantly change under physiological, pathological, and environmental conditions [25]. Lipids play important roles in cell growth and metabolism, accordingly, they are related to carcinogenesis pathways [25, 26].
In recent years, several studies have shown significant differences in the status of metabolites and lipids in normal and cancerous thyroid tissues [27,28,29,30,31,32]. In the thyroid cancer-based metabolomics studies, on the assumption that the change of metabolites analyzed profoundly, could be considered as a potential way for differentiating between benign and malignant lesions.
The rapid advances in metabolomics and lipidomics techniques and their applications to identified novel biomarkers in thyroid cancers will be discussed in this review.
Metabolomics workflow and technique
Variety of analytical platforms (include, nuclear magnetic resonance (NMR) spectroscopy and mass spectrometry (MS) coupled with GC or LC chromatography) have been developed along the years for detection of metabolic profiling and cancer metabolism changes. The most common workflow for cancer studies-based metabolomics of biological samples (biofluides; universally serum/plasma and urine, tissue, and cell lines) includes sample preparation, data acquisition, and data processing (for more details see Fig. 1). The proper collection, storage, and processing of samples for successfully implemented metabolic studies is essential [33, 34].
Appraisal of a sample preparation method depends on the sample type and characteristic of the compounds set being studied, targeted, and untargeted metabolomics approach and the analytical platform.
Urine samples, in most methods, can be analyzed directly or after dilution with a solvent, or by adding internal standard, followed by filtration or centrifugation to remove particulates. Also, urea is present at high concentration in the urine, and this could be harmful to affect the performance of GC instruments. For this purpose, urease treatment is used to reduce urea content especially for GC/MS applications [34, 35]. Moreover, in GC/MS analysis, derivatization process is crucial in order to convert polar metabolites to volatile compounds. In the NMR method, adjustment of pH is essential by adding phosphate buffer at pH 7.4 for urine samples, and deuterium (D2O) solvent is required for sample dilution, as well [36]. It has been noticed that, in blood samples, deproteinization procedure is a must to remove the high protein content. The volume of biofluid samples required for processing, are typically about 0.1 ml−0.5 ml.
Another biological sample is tissue that its collection is more complex than urine and blood sampling due to it typically contains blood, and characterized by large heterogeneity. Indeed, tissue requires complicated preparation procedures, such as use of saline for washing and laser-capture microdissection (LCM) techniques before storage. Furthermore, for the metabolite extraction from tissue, a homogenizer and an appropriate extraction buffer are required [37]. Then the samples must be dried and reconstituted with the proper solvent for LC/MS analysis. Here, chemically derivatization processing is needed for tissue samples in GC/MS analysis as well.
Another important issue in metabolomics study is using the proper chemical solvents. Indeed, for comprehensive extraction of metabolites, including amino acids, sugars, organic acids, fatty acids, and phospholipids, either by GC/MS or LC/MS, methanol, chloroform (while methyl tert-butyl ether (MTBE) or butanol/methanol (BUME) for high lipidomics) are reported to be applied [37]. In NMR Method, 4, 4-dimethyl-4-silapentane-1-sulfonic acid (DSS) or trimethylsilylpropanoic acid (TSP) are commonly uses as an internal standard and make an exact NMR reference for quantification of metabolites [38]. After the data are acquired, the primary step for identification of metabolites is data processing that is performed in some steps: normalization, scaling, and mean centering (for further information see Fig. 1). Furthermore, statistical analysis such as univariate and multivariate that is divided into main two categories; supervised (such as; principal component analysis (PCA) and hierarchical clustering analysis (HCA) and unsupervised such as; orthogonal projections to latent structures-discriminant analysis (OPLS-DA) are needed. For pathway analysis and quantification of biomarkers, bioinformatics tools and online software can be employed, e.g., Metaboanalyst or Cytoscape.
The state-of-the-art of metabolomics tools in thyroid cancer
Quantification of metabolites among biological samples in cancer studies is being conducted using either NMR or mass spectrometry-based techniques. A routine extraction method, no need for derivatization, fast and easy instrumental analysis, and most importantly robust data analysis have made NMR a suitable means for cancer researchers. NMR has been widely used for thyroid cancer metabolomics studies by biochemists.
An early report by Russell P et al. used proton magnetic resonance spectroscopy (1H MRS) in order to discriminate malignancy (PTC, MTC, FTC, and ATC) from benignity [39]. This study revealed that the most significant altered metabolites in PTC cases were related to the presence of free and bound amino acids, including glutamic acid/glutathione, threonine, valine, taurine, and bound fructose compared with healthy subjects. Two years after this work, in another experiment that was conducted by the same group, 2D 1H MRS was used for 93 thyroid tissue specimens to identified chemical changes in thyroid neoplasms in comparison with thyroid benign cases [40]. Their result showed a progressive increase in cross peaks of di-/triglycerides in malignant lesions when comparing with benign nodules. Moreover, an increased cross peak of cholesterol/cholesteryl esters was found in malignant groups.
Yoshioka et al. used 1H-NMR in order to the assessment of some important lipids in 61 thyroid tissue samples divided into four groups including 27 normal tissue as a control group, 15 PTC, 13 adenoma, and 6 Basedow disease. The lower level of dolichols in PTC and Basedow groups and the higher levels of cholesterol and acyl chain double bounds in PTC group was found [41]. Another report using NMR published by King et al. described a whole-body MR imaging system for the detection tumor changes. Certain thyroid tumors e.g., anaplastic carcinomas, papillary carcinomas, follicular carcinoma, and metastatic nodes from papillary carcinoma were studied by in vivo MRS. Choline/creatine were observed to be elevated in malignant tissues compared with normal subjects [42].
The major drawback of NMR is that it works with only aqueous solutions, and it cannot produce sufficient spectral resolutions to identify and quantify individual metabolites of intact tissues and cells. HRMAS is an alternative method that can measure single metabolites of intact tissue and cells. Moreover, during analysis the tissue intact preserved for further histopathologic or cytopathologic evaluations. Experiments by Jordan et al. used 26 thyroid FNAB samples including four papillary thyroid carcinomas, four follicular thyroid adenomas, and five normal thyroid tissues in order to verify the validity of the high-resolution magic angle spinning proton magnetic resonance spectroscopy (HRMAS 1HMRS) as an diagnostic technique [43]. The authors successfully classified the tumors based on their metabolite profiles of intact tissues.
In another study, 1H HRMAS NMR was utilized to classify benign and malignant thyroid legions. They found elevated levels of lactate and taurine and lower levels of several lipids in malignant group when compared with benign samples (see Table 1) [27]. In a similar study, promising results were obtained by Torregrossa et al. while study of 1H HRMAS NMR spectroscopy to separate benign (Adenoma, nodular goiter (NG)), malignant (PTC, FTC, and ATC) and normal thyroid tissue lesions. Increases in the levels of lactate, taurine, and phenylalanine and decreases in choline, choline derivatives, myoinositol and scyllo-inositol, and various unknown compound levels were observed in malignant groups compared with benign groups. In addition, their results suggest that these changes in metabolite levels are linked with the Warburg effect [44].
Experiments on 1H-NMR-based metabolic as an alternative way of investigating cancer lesions performed in 2013 by Deja et al. to identify the presence of metabolites in aqueous tissue extracts of healthy thyroid tissue (H), nonneoplastic nodules (NN), follicular adenomas (FA), and malignant thyroid cancer [45]. The remarkable metabolite biomarkers in all samples were alanine, methionine, acetone, glutamate, glycine, lactate, tyrosine, phenylalanine, and hypoxanthine. Furthermore, they observed that the most striking metabolic changes in thyroid cancer were taurine, scyllo- and myoinositol, and citrate. In addition, they suggest that chemometrics study allowed the discrimination of FA from benign NN and thyroid cancer with similar accuracy [45]. Two years after this study, Tian et al. dedicated their study to analyze the metabolites of thyroid tissues and their extracts from thyroid lesion patients and their adjacent healthy thyroid tissues with the combination of 1H-NMR spectroscopy and measurement of fatty acid compositions using GC with Flame Ionization Detector (FID)/MS techniques [46]. They showed multiple metabolic pathways are altered in thyroid lesions, including energy metabolism (glycolysis, lipid, and tricarboxylic acid cycle (TCA)), rising in protein turnover, nucleotide biosynthesis as well as lipids biosynthesis (see Table 1). Furthermore, Ryoo et al. describe their testing with NMR analysis of percutaneous FNA samples in order to discriminating benign and malignant thyroid cancers, including 35 PTC lesions and 69 FA samples [47]. They observed that the relative concentrations of lactate, choline, O-phosphocholine, and glycine were significantly higher in malignant lesions than in benign samples. In another study that was carried out by Lu et al. using NMR-based metabolomics in order to assessment the status of metabolites in tissue and plasma of patients with papillary thyroid microcarcinoma (PTMC). They showed that the variety of fatty acids levels were decreased and some amino acids levels were increased in thyroid tissues, as well as the reduction of some amino acid levels and elevated levels of some carbohydrates in plasma were found (Table 1) [48]. Serum and urine metabolome profiles comparison of nodular thyroid diseases (including NN, FA, and PTC) were performed by Wojtowicz applying NMR [49]. Increased lactate levels were noted in blood serum of patients who had nodular thyroid disease compared with healthy subjects. They suggested that lactate is a trustable biomarker for the disease (see Table 1 for further metabolites). More Recently in another article with the aim of predicting LN metastasis in PTC with HNMR method, 56 PTC samples with central and lateral LN metastasis were examined [50]. It has been highlighted that for samples with no clinical or histopathological characteristic, Lactate could be used as a biomarker to predict LN metastasis.
The plasma-free amino acid profile findings were confirmed by Gu et al. who conducted a study with amino acid analyzer instrument in 33 TC patients and 137 matched healthy people as a control group. The presented study showed that the levels of threonine and arginine were higher and the aspartate, glutamate, and proline were lower in thyroid cancer samples compared with healthy subjects [51].
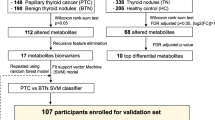
The last decade has seen a renewed importance and rapid rise in the use of GC/MS- and LC/MS-based metabolomics studies. Recent finding regarding GC/MS and LC/MS metabolic profiling of cancer cells have led to providing accurate quantification of hundreds of metabolites in the cell cycles. In a study by Yao et al. collected 140 serum samples from PTC (n = 30), NG (as a benign thyroid nodules n = 80), and healthy controls (n = 30). Using liquid chromatography–LTQ Orbitrap mass spectrometry, the major altered metabolites between benign and malignant nodules were in lipid metabolism, substantially of 3-hydroxybutyric acid [52]. Wojakowska et al. performed GC/MS-based metabolomics to compare different types of thyroid malignancies (follicular, Papillary/classical variant, papillary/follicular variant, medullary, and anaplastic cancers), benign follicular adenoma and normal thyroid tissue samples [53]. They identified several metabolites with significant changes in pathways e.g., beta-oxidation of very long-chain fatty acids, citric acid cycle, and galactose metabolism. The authors concluded that these metabolome signatures could be successfully used as a diagnostic tool for classification of different subtypes of follicular thyroid cancer. Identified metabolites are presented in Table 1.
Another study was conducted by Chen et al. using a GC/MS method to analyze metabolomics alterations in matched PTC and normal thyroid tissues. The results were accompanied with mRNA levels of the associated metabolic enzyme genes [32]. They recognized that various metabolites related to carbohydrate metabolism were downregulated while metabolites in nucleotide metabolism, including malonic acid and inosine, and lipids metabolism significantly increased in PTC. Interestingly, these observations were highly matched with mRNA levels of related genes (see Table 1). Xu et al. utilized a combination of GC-TOF/MS and LC-Q/TOF methods to differentiate the PTC and benign thyroid adenoma (BTA) [54]. They provided samples from 57 PTC and 48 BTA patients and compared them with normal (non-tumor) samples. Similarities between two diseases were found to be in increased glycolysis, amino acid metabolism, one carbon metabolism, and tryptophan metabolism. On the other hand, purine, pyrimidine, taurine, and hypotaurine levels were significantly elevated in the PTC specimens, and increased fatty acid and bile acid levels were especially found in the BTA tissues [54]. An interesting investigation for metabolic analysis of thyroid cancer disease was conducted by Guo by exhaled breath collected from 64 patients [30]. After breath sampling from 64 patients by Solid Phase Micro-Extraction (SPME), the volatile organic compounds (VOCs) were analyzed by GC/MS and the results were compared with healthy profiles. The results showed significant metabolite changes between healthy and nodular goiter such as sulfurous acid, cyclohexylmethyl hexylester, isolongifolene-5-ol, 3,5-decadien-7-yne, and cyclohexanone; in addition, some metabolites, including cyclohexanone, 4-hydroxybutyric acid, phenol, 2,2-dimethyldecane, and ethylhexanol, showed a significant alteration between PTC and the healthy group.
For improving the diagnostic accuracy of FNAB cytology in patients with thyroid cancer, Shang et al. combined targeted and nontargeted approach using GC-TOF/MS analysis validated by UPLC/QqQ/MS to identify tissue metabolic profile of PTC [31]. Their work led to the introduction of the galactose metabolism pathway as an important factor influencing PTC development by modifying energy metabolism by means of its key metabolites those were assigned as significant in both GC/MS and LC/MS experiments (see Table 1 for further altered metabolites).
Imaging mass spectrometry (IMS) is a newly developed tool that is able to identify large and unstable molecules, such as peptides, proteins and lipids on a tissue section, or cell samples [55].
MALDI matrix has been successfully applied for detection of the lipid profiles of cells and tissue in lipidomic studies [46]. Ishikawa et al. applied matrix-assisted laser desorption/ionization MALDI-TOF/TOF in seven patients with PTC by comparison with healthy subjects in order to identified different phospholipid compounds. A higher levels of phosphatidylcholine (16:0/18:1) and (16:0/18:2) and sphingomyelin (d18:0/16:1) were found in PTC compared with healthy samples [56]. Using fast and accurate technique of matrix-assisted laser desorption/ionization Fourier transform ion cyclotron resonance mass spectrometry (MALDI/FT/ICR), Guo et al. also succeeded to observe monounsaturated lipids profiles in six different tissue and serum types of cancers, including thyroid cancer (124 PTC and FTC vs. 122 healthy subjects and benign thyroid samples) [57]. Their results revealed that thyroid cancers sera had altered levels of 10 lipids, including three phosphatidylcholine, six phosphatidic acids, and a sphingomyelin (see Table 1). In another article that is published by the same author (Guo et al.), MALDI-FTICR MS was used to quantify serum and tissue lipidome of 124 MTC patients, 43 BTT patients, and 122 normal controls. Their results indicated that PC (34:1) had a strong ability as a discriminator biomarker between both MTC and BTT patients versus healthy subjects, further, PA (36:3) and SM (34:1) could use as discriminator biomarkers between MTC and BTT [58]. A similar study was conducted utilizing MALDI imaging by Wojakowska et al. [59]. For discrimination of papillary thyroid cancer from noncancerous thyroid tissue a MALDI-Q-Ion Mobility-TOF-MS technique was used for lipidomic analysis of formalin-fixed thyroid tissue samples. Their results investigated that cancerous tissue had the most significant altered levels of eight lipids, including four phosphatidylcholines, tow sphingomyelins, and tow phosphatidic acids (for further metabolite changes see Table 1).
Pathway analysis and regulations of thyroid cancer
The first outstanding characteristic of the tumor-specific metabolism was postulated by Otto Warburg a German physiologist in 1923 and 1956 [60, 61]. This unique feature of cancer cells that is known as the “Warburg effect”, is a cellular metabolic change in the aerobic glycolysis pathway that is regulated even in the presence of normal or excess levels of oxygen in order to produce rapid supply of ATP for proliferation [62]. Overall, for cellular metabolism in healthy cells, the breakdown of glucose begins by the cytoplasmic pathway called glycolysis; this process is the conversion of one molecule of glucose into two molecules of pyruvate. Pyruvate is oxidized into acetyl-CoA, in order to enter the tricarboxylic acid cycle (Krebs cycle, TCA) that take place in the mitochondrial matrix. The TCA cycle consists of consecutive reactions that lead to the transfer of electrons with electron transport chain (ETC) to NAD +/ FAD+ to produce NADH/FADH2, and a proton gradient is generated across the inner mitochondrial membrane, which is essential for the synthesis of ATP and energy production, in a process called oxidative phosphorylation (OXPHOS). In contrast, under pervasive physiological processes such as hypoxic (low oxygen tension) conditions, intracellular ATP is reduced, consequently glucose uptake and aerobic glycolysis metabolism is increased, and higher levels of lactate are produced from pyruvate. Most cancer cells, due to their high levels of proliferation, show the indicated phenotype, which increases the demand for high energy and ATP [63, 64]. In a study by Coelho et al. that was carried out on two thyroid carcinoma papillary cell lines (BCPAP and TPC1) and the nontumor cell line (NTHY-ori), discriminated that all tumor cell lines had a high rate of glycolysis with increased lactate production when compared to NTHY-ori [65]. In that work, it was observed that Warburg effect occurred in both PTC cell lines with decreased levels of oxygen consumption. The Warburg effect mechanism suppresses oxidative phosphorylation in cancer cells, in consequence elevated levels of reactive oxygen species (ROS), which can be produced as a result of OXPHOS dysfunction in the mitochondria, is associated with some metabolic changes [66]. The main source of H2O2 in the thyroid gland is dual oxidases (DUOX1 and DUOX2), but some studies showed that the thyroid gland expressed NADPH oxidase 4 (NOx4), which is positively regulated by TSH, and related to an important ROS source and notably expressed in PTC [67,68,69]. In addition, there is a significant positive link between thyroid cancer, harboring the BRAFV600E mutation and NOX4 expression [69].
Isocitrate dehydrogenase (IDH) is one of the important enzymes in TCA cycle that contributes to the production of NADPH with catalyze the oxidative decarboxylation of isocitrate to alpha-ketoglutarate (α-KG). IDH isoform 1 and IDH isoform 2 are localized in the cytosol and mitochondria, respectively. Somatic mutation in the IDH can lead to the S-2-hydroxyglutaric acids and R-2-hydroxyglutaric acids production which cause neurological impairment and glioblastoma. In human brain tumor patient mutations in the enzyme cytosolic isocitrate dehydrogenase 1 (IDH1) are found in ~80% of grades II–III gliomas and secondary glioblastomas [70]. The demonstration that cancer-associated IDH1 mutations result in a new ability of the enzyme to catalyze the NADPH-dependent reduction of α-ketoglutarate to the oncometabolite R (−)-2-hydroxyglutarate represents a milestone event in cancer biology [71]. In one study, mutations of IDH1 have not been detected in MTC and PTC [72]. In contrast, another study that was performed on FTC and ATC samples identified a novel homozygous G367A IDH1 mutation in FTC and ATC with the high prevalence mutations in ATC, which suggest that IDH1 may have a role in tumorigenesis and could be used as a marker for therapeutic procedures in thyroid cancers [73].
According to high rate of glycolysis due to the Warburg effect, the expression levels of various types of glycolytic enzymes and glucose transports are changed in cancer cells. Fourteen types of glucose transporter proteins are known that passes glucose through the plasma membrane. Among them, an increase expression of GLUT1 in thyroid cancer was first noted by Haber et al. in 1997, using immunostaining procedure [74]. The authors have shown that GLUT1 expression is highly regulated in thyroid cancers, but are poorly expressed in benign nodules and normal thyroid tissue. Afterwards, Matsuzu et al. studied the expression of differences in the GLUT isoform genes, by reverse transcription–polymerase chain reaction (RT-PCR) method in normal and pathologic thyroid tissues. In that work, results showed the mRNA expression of GLUT 1, 3, 4, and 10 was present in all thyroid tissues [75]. In addition, the authors demonstrated a significant increase of the GLUT1 mRNA expression in thyroid carcinoma cases. Another study that was performed on the PTC cells by Coelho et al. indicated that the levels of GLUT1 mRNA are higher than the nontumor cells, which may increase glucose uptake in these cells [65]. Finally, in a study by Nahm et al., immunohistochemical staining of thyroid cancer tissues indicated that PTC not only expresses GLUT1 but also expresses GLUT3. In addition, the highest expression levels of GLUT1 were found in ATC, which suggests that GLUT expression levels may promote tumor invasion [76]. In metabolic pathways, some enzymes catalyze critical irreversible reactions. One of them is HK that catalyzes the first irreversible glycolysis reaction, and its product is glucose 6-phosphate (G6P), which is a substrate for glycolysis or the pentose phosphate pathway (PPP). There are various forms of HK in the body. HK1 and HK2 isoforms are the most commonly expressed at high levels and promotes cancer cells growth [77, 78]. Rijksen et al. in a study with animal models of MTC and ATC tumors did not show a difference in both HK1 and HK2 biochemical activity and characteristics [79]. According to Hooft et al., studies that were carried out in two different years separately, the expression of HK1 was similar between the primary DTC and the metastatic tumors [80, 81]. In a study published recently, analysis of 342 PTC specimens was revealed higher HK2 levels in 50% of PTC specimens with BRAFV600E mutations [76]. In another study, it has been shown that both HK1 and HK2 isoforms in BCPAP and TPC1 cells were more overexpressed than the nontumor cells, also the authors observed that the activity of HK in the cytosol and mitochondrial sections of BCPAP and TPC1 cell lines was substantially different [65].
The PK enzyme catalyzes the last step of the glycolysis. PK isoform M1 (PKM1) converted phosphoenolpyruvate (PEP) and ADP to pyruvate and ATP, respectively. PK isoform M2 (PKM2) was detected in normal proliferating cells [82], and also overexpressed in tumor cells [83] then introduced as a major PK isoform that expressed in cancerous cells. Its activity regulated by acetylation, phosphorylation, and oxidation in a dominant-negative manner. When PKM2 is expressed in the tumor, thereby negligible pyruvates are produced, and this leads to a limited mitochondrial substrate that contributes to the metabolic switch from OXPHOS to aerobic glycolysis [84]. The higher expression of PKM2 has been identified in thyroid cancer [65, 85]
Feng et al. showed that the PKM2 expression in human PTC was associated with advanced tumor and metastasis of the lymph node [85]. Recently in another research, Coelho has shown that the activity of PKM2 depends on the PTC driver, BRAF mutation [65].
Lactate is an aerobic metabolite which is formed by converting pyruvate and NADH into a reversible catalyzed reaction with lactate dehydrogenase (LDH). LDH isoforms and enantiomers are expressed in several tissues. This enzyme is regulated in a wide range of tumor tissues [70, 86]. An experiment by Mirabeau-Prunier et al. showed a lower LDHA/LDHB ratio (decreased by 30%) in thyroid oncocytomas and follicular thyroid tumors. They suggested that the low concentration of LDHA expression is related to adjusting the levels of the estrogen-related receptor alpha, leading to changes in the oxidative metabolic profile of the tumor [87]. Another study by Kachel et al. revealed that LDHA is overexpressed in the FTC and PTC, compared with the goiter tissues, in addition, they suggest that LDHA could be used as a tumor marker for thyroid cancer [88]. Monocarboxylate transporters (MCTs) are part of a family of transmembrane protein carriers that composed of 14 isoforms, involving in multiple metabolic pathways, such as glycolysis, thyroid hormone metabolism, fatty acid homeostasis, and spermatogenesis [89]. MCTs 1–4 are proton-coupled transporters, playing a role in transporting a number of monocarboxylates, such as lactate, pyruvate, butyrate, as well as ketone bodies across the plasma membrane [90]. In tumor cells, these carriers are essential for maintenance of glycolysis under hypoxia and normoxia conditions, so, in turn, tumor cells can metabolize lactate and produce high-energy agents [91]. In a study that was conducted by Johnson et al. MCT1 has been highly expressed in ATC when compared with normal thyrocytes and PTC [92]. They suggest that MCT1 may use as a therapeutic target for ATC. Curry et al. showed that cancer-associated fibroblasts (CAFs) with higher MCT4 expression can be used as a marker for glycolytic metabolism that were observed in progressive PTC specimen. On the other hand, higher levels of extracellular lactate suggest that MCT4 is responsible for the export of intracellular lactate in the extracellular space of PTC cells [93]. Glutaminolysis is another metabolic property of cancer cells that mediate anaplerotic fluxes to produce TCA cycle intermediates [94]. The glutamine is transported through the amino acid transporter-2 (ASCT2) to enter the glutaminolysis pathway, and can be transformed into glutamate that is converted to a-ketoglutarate (aKG), and then shuttled to the Krebs cycle. The catalyzing enzymes that play a critical role in this biomedical reaction are glutaminase 1 (GLS1), glutamate dehydrogenase (GlDH), glutamate pyruvate transaminase (GPT), and glutamate oxaloacetate transaminase (GOT). In some cancer studies, elevated level of glutamine metabolism has been found [95, 96]. Kim et al. studied 557 thyroid cancer specimens, including (PTC: 344, [FC]: 112, [MC]: 70, poorly differentiated carcinoma [PDC]: 23, and anaplastic carcinoma [AC]: 8) found that the expression of glutamine metabolism-related proteins, such as GLS1 GDH and ASCT2, were different in the thyroid cancer subtype. Furthermore, they observed the highest expression of glutamine metabolism-related proteins in ATC and PTC that were related to BRAFV600E mutation [97]. More recently, in an experiment that was conducted by Yu Y et al. revealed that the overexpression of GLS was associated with the development and progression of papillary thyroid carcinoma [98].
The way that signaling pathways are controlling the energy metabolism of thyroid cancer cells is still not well-known.
C-Myc oncogene is one of the major metabolic regulators. Some studies investigated that c-Myc-induced genes were involved in glucose and glutamine metabolism, such as GLUT1, HK2, PKM2, ASCT2 and SLC7A5, and some microRNAs as well [99, 100]. In addition, c-Myc is the direct regulator of LDH-A, which is the enzyme that catalyzes the conversion of L-lactate into pyruvate in an anaerobic condition [100]. In year 2017, Qu et al. showed that BRAFV600V signaling results in an increased expression of c-Myc in the human PTC cell line [101]. Furthermore, they revealed that the high expression of this gene is involved in the metabolism of glucose.
Another critical regulator in energy metabolism is hypoxia-inducible factors (HIF). HIF-1α increases the expression of genes involved in glucose and energy metabolism by adjusting the values of glucose transports, enzymes involved in glycolysis, LDH-A, and MCT4 [102, 103]. Intriguingly, HIF-1α also cooperates with c-Myc oncogene when c-Myc is overexpressed, then, promotes aerobic glycolysis, and decreases mitochondrial biogenesis [104, 105]. In some studies that were carried out on different types of thyroid cancer such as PTC, FTC, and MTC, results all together showed that the expression of HIF-1α was firmly associated with poor prognosis and plays a prominent role in metastasis process [106,107,108]. In addition, HIF-1 stimulates the development of blood vessels, in a process called angiogenesis by increasing the vascular endothelial growth factor (VEGF) expression and promoting the mass of the tumor. Some studies have also shown that VEGF is a risk factor for PTC and tumor progression [109, 110].
Other metabolism reprogramming that investigated in thyroid cancer is unusual mitochondrial proliferation. Thyroid oncocytomas that are called Hürthle cell carcinoma are an eccentric rare type of differentiated thyroid cancer, which is characterized by presence of abnormally proliferation of mitochondria. The gene profiling of thyroid oncocytomas indicated overexpression of encoded genes that were related to glycolysis pathway, the TCA cycle, and oxidative phosphorylation enzymes as described by Baris et al. [111]. Furthermore, they showed downregulation of gene that encoded lactate dehydrogenase A (LDH-A) when compared with normal thyroid tissue. This work suggests that due to the defective oxidative phosphorylation in the mitochondria, thyroid oncocytomas-generated energy through an aerobic pathway.
Schematic illustration of the metabolic reprogramming in thyroid cancer cells: c-Myc and Hif-1 contributing to the Warburg effect and regulate the important genes that involved in glucose metabolism. High levels of c-Myc and Hif-1 stimulate the expression of PKM2, GLU1/3, HK2, MCT, and LDHA. HIF1 activation also drives the expression of VEGF and PDK. PDK can inhibit the PDH activity. On the other hand, glutamine is taken up via the ASCT2 and enters into the glutaminolysis pathway and is converted into glutamate via GLS1. The upregulation of lactate dehydrogenase facilitates the conversion of pyruvate to lactate, which is then transferred to the tumor microenvironment via the MCT. Glut1/3 glucose transporter 1 or 3, HK hexokinase, PKM2 pyruvate kinase isoforms 2, LDHA lactate dehydrogenase A, 6PDG 6-phosphogluconate dehydrogenase, MCT monocarboxylate transporter-1, HIF-1 hypoxia-inducible factor-1, ASCT Asc-type amino acid transporter, GSL glutaminase 1
Over the past few years, lipids metabolism has been considered as the other metabolic phenotype that contributes to the tumorigenesis. The most abundant classes of membrane lipids are triacylglycerides (TGs), phospholipids (PLs) including phosphatidylcholine (PC) and phosphatidylethanolamine (PE), sterols, and sphingolipids that de novo biosynthesis of them are mainly regulated in the liver, adipose tissue, intestine, and the lactating breast tissues. They represent the main structure of cell membranes and have a function as the first and second messengers in signal transduction [112]. Cancer cells have illustrated high rates of de novo fatty acid synthesis. These altered and modification of lipids metabolism frequently mediate aggressive phenotype and poor prognosis in cancer patients [113]. In a study that was carried out by Roemeling et al. [114], gene array analysis of ATC samples showed significant alterations in the expression of genes involved in lipid metabolism when compared with healthy thyroid tissue samples. Among them, upregulation of stearoyl-CoA desaturase SCD1 that play a critical role in de novo lipogenesis was found in ATC. Furthermore, IHC analysis showed elevated levels of SCD1 in PTC and advanced FTC as well. This study further implicates that SCD1 may use as a therapeutic target in patients with thyroid cancer. Figure 2 summarizes the major altered metabolic pathways in thyroid cancer cells.
Conclusion
Taken together, TCs diagnosis at the first step is relying on FNAB and it encounter to around 25% indeterminate cases, so, it demands a new biomarker platform to detect and fortunately accurate techniques are growing in this field. Metabolomics-based techniques provide insights into the future of this field and upcoming achievements. Researches in TC are mainly focused on NMR, and the results have shown suggestions on the metabolic insights of the disease. On the other hand, LC- and GC-based metabolomics have provided the opportunity for the simultaneous analysis of a wide range of polar and nonpolar metabolites, and larger metabolic information has been provided by these methods. The role of lactate, choline, monosaccharides, and TCA intermediates have been well discovered in TC, and precise investigation are to be continued for new biomarkers detection. MALDI imaging MS has also found a unique role in the TC researches regarding its ability to metabolic analysis of intact tissues. Furthermore, the pathways described in this review have improved our knowledge about metabolism functions and thyroid cancer cells proliferation. Among them, Warburg effect and glutaminolysis are the main metabolic reprogramming in thyroid cancer cells. Clearly further researches in the field of TC metabolomics are yet to be done for providing larger information set for metabolic markers and better understanding of the associated between metabolic dysfunctions and thyroid tumorigenesis.
References
S. Vaccarella, S. Franceschi, F. Bray, C.P. Wild, M. Plummer, L. Dal Maso, Worldwide thyroid-cancer epidemic? the increasing impact of overdiagnosis. N. Engl. J. Med. 375, 614 (2016)
L.Z.K. Enewold, E. Ron, A.J. Marrogi, A. Stojadinovic, G.E. Peoples, S.S. Devesa, Rising thyroid cancer incidence in the United States by demographic and tumor characteristics. Cancer Epidemiol. Biomarkers. Prev. 18, 784–779 (2009)
L.G. Morris, D. Myssiorek, Improved detection does not fully explain the rising incidence of well-differentiated thyroid cancer: a population-based analysis. Am. J. Surg. 200, 454–461; https://doi.org/10.1016/j.amjsurg.2009.11.008 (2010)
F. Bray, J. Ferlay, I. Soerjomataram, R.L. Siegel, L.A. Torre, A. Jemal, Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J. Clin. 68, 394–424 (2018)
G.D. Braunstein, Thyroid Cnacer. In: Melmed, editor. Endocrine Updates. Vol. 32 (Springer, NY, USA, 2012)
N.R.M.E. Lemoine, F.S. Wyllie, C.J. Farr, D. Hughes, R.A. Padua et al., Activated ras oncogenes in human thyroid cancers. Cancer Res. 48, 4459–4463 (1998)
D. Sarne, SA, External radiation and thyroid neoplasia. Endocrinol. Metab. Clin. North. Am. 25, 181–195 (1996)
H.N.I. Yamashita, S. Noguchi, N. Murakami, A. Moriuchi, S. Yokoyama et al., Thyroid carcinoma in benign thyroid diseases:an analysis from minute carcinoma. Acta Pathol. Jpn. 35, 781–788 (1985)
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer CD, G.M. Doherty, B.R. Haugen, R.T. Kloos, S.L. Lee, S.J. Mandel, E.L. Mazzaferri, B. McIver, F. Pacini, M. Schlumberger, S.I. Sherman, D.L. Steward, R.M. Tuttle, Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 19, 1167–1214 (2009)
E.S.A.S. Cibas, The Bethesda system for reporting thyroid cytopathology. Thyroid. 19, 1159–1165 (2009)
J. Yang, V. Schnadig, R. Logrono, P.G. Wasserman, Fine-needle aspiration of thyroid nodules: a study of 4703 patients with histologic and clinical correlations. Cancer 25 111, 306–315 (2007)
L. Yassa, E.S. Cibas, C.B. Benson, M.C. Frates, P.M. Doubilet, A.A. Gawande, F.D. Moore Jr, B.W. Kim, V. Nosé, E. Marqusee, Long‐term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer Cytopathol.: Interdisciplinary International Journal of the American Cancer Society 111, 508–516 (2007)
F. Pacini, M. Schlumberger, H. Dralle, R. Elisei, J.W. Smit, W. Wiersinga, Erratum: European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur. J. Endocrinol. 155, 385 (2006)
M. Bongiovanni, A. Spitale, W.C. Faquin, L. Mazzucchelli, Z.W. Baloch, The Bethesda system for reporting thyroid cytopathology: a meta-analysis. Acta Cytol. 56, 333–339 (2012)
A.S. Ho, E.E. Sarti, K.S. Jain, H. Wang, I.J. Nixon, A.R. Shaha, J.P. Shah, D.H. Kraus, R. Ghossein, S.A. Fish, Malignancy rate in thyroid nodules classified as Bethesda category III (AUS/FLUS). Thyroid. 24, 832–839 (2014)
X. Su, X. Jiang, X. Xu, W. Wang, X. Teng, A. Shao, L. Teng, Diagnostic value of BRAFV600E-mutation analysis in fine-needle aspiration of thyroid nodules: a meta-analysis. Onco. Targets Ther. 9, 2495 (2016)
W. Clinkscales, A. Ong, S. Nguyen, E.E. Harruff, M.B. Gillespie, Diagnostic value of RAS mutations in indeterminate thyroid nodules: systematic review and meta-analysis. Otolaryngology–Head and Neck Surgery 156, 472–479 (2017)
M. Eszlinger, A. Krogdahl, S. Münz, C. Rehfeld, E.M. Precht Jensen, C. Ferraz, E. Bösenberg, N. Drieschner, M. Scholz, L. Hegedüs, Impact of molecular screening for point mutations and rearrangements in routine air-dried fine-needle aspiration samples of thyroid nodules. Thyroid. 24, 305–313 (2014)
S. Yu, Y. Liu, J. Wang, Z. Guo, Q. Zhang, F. Yu, Y. Zhang, K. Huang, Y. Li, E. Song, Circulating microRNA profiles as potential biomarkers for diagnosis of papillary thyroid carcinoma. The Journal of Clinical Endocrinology & Metabolism 97, 2084–2092 (2012)
S. Fischer, S.L. Asa, Application of immunohistochemistry to thyroid neoplasms. Arch. Pathol. Lab. Med. 132, 359–372 (2008)
S. Serra, S.L. Asa, Controversies in thyroid pathology: the diagnosis of follicular neoplasms. Endocr. Pathol. 19, 156–165 (2008)
J.K. Nicholson, J.C. Lindon, E. Holmes, ‘Metabonomics’: understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 29, 1181–1189 (1999)
W.M. Claudino, P.H. Goncalves, A. di Leo, P.A. Philip, F.H. Sarkar, Metabolomics in cancer: a bench-to-bedside intersection. Crit. Rev. Oncol. Hematol. 84, 1–7 (2012)
A. Shevchenko, K. Simons, Lipidomics: coming to grips with lipid diversity. Nat. Rev. Mol. Cell Biol. 11, 593 (2010)
M.R. Wenk, The emerging field of lipidomics. Nat. Rev. Drug. Discov. 4, 594 (2005)
R. Bandu, H.J. Mok, K.P. Kim, Phospholipids as cancer biomarkers: mass spectrometry‐based analysis. Mass. Spectrom. Rev. 37, 107–138 (2018)
P. Miccoli, L. Torregrossa, L. Shintu, A. Magalhaes, J. Chandran, A. Tintaru, C. Ugolini, M.N. Minuto, M. Miccoli, F. Basolo, Metabolomics approach to thyroid nodules: A high-resolution magic-angle spinning nuclear magnetic resonance–based study. Surgery 152, 1118–1124 (2012)
A. Wojakowska, M. Chekan, P. Widlak, M. Pietrowska, Application of metabolomics in thyroid cancer research. Int. Jo. Endocrinol 2015, 258763 (2015)
R.H. Grogan, E.J. Mitmaker, O.H. Clark, The evolution of biomarkers in thyroid cancer—from mass screening to a personalized biosignature. Cancers 2, 885–912 (2010)
L. Guo, C. Wang, C. Chi, X. Wang, S. Liu, W. Zhao, C. Ke, G. Xu, E. Li, Exhaled breath volatile biomarker analysis for thyroid cancer. Translational Research 166, 188–195 (2015)
X. Shang, X. Zhong, X. Tian, Metabolomics of papillary thyroid carcinoma tissues: potential biomarkers for diagnosis and promising targets for therapy. Tumor Biology 37, 11163–11175 (2016)
M. Chen, M. Shen, Y. Li, C. Liu, K. Zhou, W. Hu, B. Xu, Y. Xia, W. Tang, GC-MS-based metabolomic analysis of human papillary thyroid carcinoma tissue. Int. J. Mol. Med. 36, 1607–1614 (2015)
G.N. Gowda, S. Zhang, H. Gu, V. Asiago, N. Shanaiah, D. Raftery, Metabolomics-based methods for early disease diagnostics. Expert. Rev. Mol. Diagn. 8, 617–633 (2008)
A. Scalbert, L. Brennan, O. Fiehn, T. Hankemeier, B.S. Kristal, B. van Ommen, E. Pujos-Guillot, E. Verheij, D. Wishart, S. Wopereis, Mass-spectrometry-based metabolomics: limitations and recommendations for future progress with particular focus on nutrition research. Metabolomics. 5, 435 (2009)
R. Beger, A review of applications of metabolomics in cancer. Metabolites 3, 552–574 (2013)
L. Brennan, NMR-based metabolomics: from sample preparation to applications in nutrition research. Prog. Nucl. Magn. Reson. Spectros. 83, 42–49 (2014)
J.L. Griffin, R.A. Kauppinen, Tumour metabolomics in animal models of human cancer. J. Proteome. Res. 6, 498–505 (2007)
I.C. Felli, B. Brutscher, Recent advances in solution NMR: fast methods and heteronuclear direct detection. Chemphyschem 10, 1356–1368 (2009)
P. Russell, C.L. Lean, L. Delbridge, G.L. May, S. Dowd, C.E. Mountford, Proton magnetic resonance and human thyroid neoplasia I: discrimination between benign and malignant neoplasms. Am. J. Med. 96, 383–388 (1994)
W.B. Mackinnon, L. Delbridge, P. Russell, C.L. Lean, G.L. May, S. Doran, S. Dowd, C.E. Mountford, Two-dimensional proton magnetic resonance spectroscopy for tissue characterization of thyroid neoplasms. World J. Surg. 20, 841–847 (1996)
Y. Yoshioka, J. Sasaki, M. Yamamoto, K. Saitoh, S. Nakaya, M. Kubokawa, Quantitation by 1H‐NMR of dolichol, cholesterol and choline‐containing lipids in extracts of normal and phathological thyroid tissue. NMR. Biomed. 13, 377–383 (2000)
A.D. King, D.K. Yeung, A.T. Ahuja, M. Gary, A.B. Chan, S.S. Lam, A.C. van Hasselt, In vivo 1H MR spectroscopy of thyroid carcinoma. Eur. J. Radiol. 54, 112–117 (2005)
K.W. Jordan, C.B. Adkins, L.L. Cheng, W.C. Faquin, Application of magnetic-resonance-spectroscopy-based metabolomics to the fine-needle aspiration diagnosis of papillary thyroid carcinoma. Acta Cytol. 55, 584–589 (2011)
L. Torregrossa, L. Shintu, J. Nambiath Chandran, A. Tintaru, C. Ugolini, Magalhães Ar, F. Basolo, P. Miccoli, S. Caldarelli, Toward the reliable diagnosis of indeterminate thyroid lesions: a HRMAS NMR-based metabolomics case of study. J. Proteome. Res. 11, 3317–3325 (2012)
S. Deja, T. Dawiskiba, W. Balcerzak, M. Orczyk-Pawiłowicz, M. Głód, D. Pawełka, P. Młynarz, Follicular adenomas exhibit a unique metabolic profile. 1H NMR studies of thyroid lesions. PLoS ONE. 8, e84637 (2013)
Y. Tian, X. Nie, S. Xu, Y. Li, T. Huang, H. Tang, Y. Wang, Integrative metabonomics as potential method for diagnosis of thyroid malignancy. Sci. Rep. 5, 14869 (2015)
I. Ryoo, H. Kwon, S.C. Kim, S.C. Jung, J.A. Yeom, H.S. Shin, H.R. Cho, T.J. Yun, S.H. Choi, C.-H. Sohn, Metabolomic analysis of percutaneous fine-needle aspiration specimens of thyroid nodules: potential application for the preoperative diagnosis of thyroid cancer. Sci. Rep. 6, 30075 (2016)
J. Lu, S. Hu, P. Miccoli, Q. Zeng, S. Liu, L. Ran, C. Hu, Non-invasive diagnosis of papillary thyroid microcarcinoma: a NMR-based metabolomics approach. Oncotarget 7, 81768 (2016)
W. Wojtowicz, A. Zabek, S. Deja, T. Dawiskiba, D. Pawelka, M. Glod, W. Balcerzak, P. Mlynarz, Serum and urine 1 H NMR-based metabolomics in the diagnosis of selected thyroid diseases. Sci. Rep. 7, 9108 (2017)
J.W. Seo, K. Han, J. Lee, E.-K. Kim, H.J. Moon, J.H. Yoon, V.Y. Park, H.-M. Baek, J.Y. Kwak, Application of metabolomics in prediction of lymph node metastasis in papillary thyroid carcinoma. PLoS ONE. 13, e0193883 (2018)
Y. Gu, T. Chen, S. Fu, X. Sun, L. Wang, J. Wang, Y. Lu, S. Ding, G. Ruan, L. Teng, Perioperative dynamics and significance of amino acid profiles in patients with cancer. J. Transl. Med. 13, 35 (2015)
Z. Yao, P. Yin, D. Su, Z. Peng, L. Zhou, L. Ma, W. Guo, L. Ma, G. Xu, J. Shi, Serum metabolic profiling and features of papillary thyroid carcinoma and nodular goiter. Mol. Biosyst. 7, 2608–2614 (2011)
A. Wojakowska, M. Chekan, Ł. Marczak, K. Polanski, D. Lange, M. Pietrowska, P. Widlak, Detection of metabolites discriminating subtypes of thyroid cancer: molecular profiling of FFPE samples using the GC/MS approach. Mol. Cell. Endocrinol. 417, 149–157 (2015)
Y. Xu, X. Zheng, Y. Qiu, W. Jia, J. Wang, S. Yin, Distinct metabolomic profiles of papillary thyroid carcinoma and benign thyroid adenoma. J. Proteome. Res. 14, 3315–3321 (2015)
S. Shimma, Y. Sugiura, T. Hayasaka, N. Zaima, M. Matsumoto, M. Setou, Mass imaging and identification of biomolecules with MALDI-QIT-TOF-based system. Anal. Chem. 80, 878–885 (2008)
S. Ishikawa, I. Tateya, T. Hayasaka, N. Masaki, Y. Takizawa, S. Ohno, T. Kojima, Y. Kitani, M. Kitamura, S. Hirano, Increased expression of phosphatidylcholine (16: 0/18: 1) and (16: 0/18: 2) in thyroid papillary cancer. PLoS ONE. 7, e48873 (2012)
S. Guo, Y. Wang, D. Zhou, Z. Li, Significantly increased monounsaturated lipids relative to polyunsaturated lipids in six types of cancer microenvironment are observed by mass spectrometry imaging. Sci. Rep. 4, 5959 (2014)
S. Guo, L. Qiu, Y. Wang, X. Qin, H. Liu, M. He, Y. Zhang, Z. Li, X. Chen, Tissue imaging and serum lipidomic profiling for screening potential biomarkers of thyroid tumors by matrix-assisted laser desorption/ionization-Fourier transform ion cyclotron resonance mass spectrometry. Anal. Bioanal. Chem. 406, 4357–4370 (2014)
A. Wojakowska, L. Cole, M. Chekan, K. Bednarczyk, M. Maksymiak, M. Oczko-Wojciechowska, B. Jarzab, M. Clench, J. Polańska, M. Pietrowska, Discrimination of papillary thyroid cancer from non-cancerous thyroid tissue based on lipid profiling by MALDI-MSI. Endokrynologia Polska 69, 2–8 (2015)
O. Warburg, S. Minami, Versuche an überlebendem carcinom-gewebe. J. Mol. Med. 2, 776–777 (1923)
S. Weinhouse, O. Warburg, D. Burk, A.L.Schade, On Respiratory Impairment in Cancer Cells. Science 124, 267–272 (1956). https://doi.org/10.1126/science.124.3215.267
D.C. Ngo, K. Ververis, S.M. Tortorella, T.C. Karagiannis, Introduction to the molecular basis of cancer metabolism and the Warburg effect. Mol. Biol. Rep. 42, 819–823 (2015)
R.J. DeBerardinis, J.J. Lum, G. Hatzivassiliou, C.B. Thompson, The biology of cancer: metabolic reprogramming fuels cell growth and proliferation. Cell. Metab. 7, 11–20 (2008)
Y. Asgari, Z. Zabihinpour, A. Salehzadeh-Yazdi, F. Schreiber, A. Masoudi-Nejad, Alterations in cancer cell metabolism: the Warburg effect and metabolic adaptation. Genomics 105, 275–281 (2015)
R.G. Coelho, Jd.M. Cazarin, C. de Albuquerque, J.P. Albuquerque, B.M. de Andrade, D.P. Carvalho, Differential glycolytic profile and Warburg effect in papillary thyroid carcinoma cell lines. Oncol. Rep. 36, 3673–3681 (2016)
S.S. Sabharwal, P.T. Schumacker, Mitochondrial ROS in cancer: initiators, amplifiers or an Achilles’ heel? Nat. Rev. Cancer 14, 709 (2014)
U. Weyemi, B. Caillou, M. Talbot, R. Ameziane-El-Hassani, L. Lacroix, O. Lagent-Chevallier, A. Al Ghuzlan, D. Roos, J.-M. Bidart, A. Virion, Intracellular expression of reactive oxygen species-generating NADPH oxidase NOX4 in normal and cancer thyroid tissues. Endocr. Relat. Cancer 17, 27–37 (2010)
U. Weyemi, O. Lagente-Chevallier, M. Boufraqech, F. Prenois, F. Courtin, B. Caillou, M. Talbot, M. Dardalhon, A. Al Ghuzlan, J. Bidart, ROS-generating NADPH oxidase NOX4 is a critical mediator in oncogenic H-Ras-induced DNA damage and subsequent senescence. Oncogene 31, 1117 (2012)
N. Azouzi, J. Cailloux, J.M. Cazarin, J.A. Knauf, J. Cracchiolo, A. Al Ghuzlan, D. Hartl, M. Polak, A. Carré, M. El Mzibri, NADPH oxidase NOX4 is a critical mediator of BRAFV600E-induced downregulation of the sodium/iodide symporter in papillary thyroid carcinomas. Antioxid. Redox. Signal. 26, 864–877 (2017)
I. Moroni, L. D’incerti, E. Maccagnano, M. Bugiani, M. Rimoldi, G. Broggi, G. Uziel, L-2-hydroxyglutaric aciduria and brain malignant tumors. J. Inherit. Metab. Dis. 25, 59 (2002)
A.M. Intlekofer, R.G. Dematteo, S. Venneti, L.W. Finley, C. Lu, A.R. Judkins, A.S. Rustenburg, P.B. Grinaway, J.D. Chodera, J.R. Cross, Hypoxia induces production of L-2-hydroxyglutarate. Cell. Metab. 22, 304–311 (2015)
F.E. Bleeker, S. Lamba, S. Leenstra, D. Troost, T. Hulsebos, W.P. Vandertop, M. Frattini, F. Molinari, M. Knowles, A. Cerrato, IDH1 mutations at residue p. R132 (IDH1R132) occur frequently in high‐grade gliomas but not in other solid tumors. Hum. Mutat. 30, 7–11 (2009)
A.K. Murugan, E. Bojdani, M. Xing, Identification and functional characterization of isocitrate dehydrogenase 1 (IDH1) mutations in thyroid cancer. Biochem. Biophys. Res. Commun. 393, 555–559 (2010)
R.S. Haber, K.R. Weiser, A. Pritsker, I. Reder, D.E. Burstein, GLUT1 glucose transporter expression in benign and malignant thyroid nodules. Thyroid. 7, 363–367 (1997)
K. Matsuzu, F. Segade, U. Matsuzu, A. Carter, D.W. Bowden, N.D. Perrier, Differential expression of glucose transporters in normal and pathologic thyroid tissue. Thyroid. 14, 806–812 (2004)
J.H. Nahm, H.M. Kim, J.S. Koo, Glycolysis-related protein expression in thyroid cancer. Tumor Biology 39, 1010428317695922 (2017)
J.E. Wilson, Isozymes of mammalian hexokinase: structure, subcellular localization and metabolic function. J. Exp. Biol. 206, 2049–2057 (2003)
Paweł. Lis, Mariusz Dyl ag, Katarzyna Nied´zwiecka, YoungH. Ko, PeterL. Pedersen AG, S. Ułaszewski, The HK2 dependent “Warburg Effect” and mitochondrial oxidative phosphorylation in cancer: targets for effective therapy with 3-bromopyruvate. Molecules 21, 1730 (2016)
G. Rijksen, R. Oskam, C.F. Molthoff, S.-J.L. On, M. Streefkerk, G.E. Staal, Hexokinase isoenzymes from anaplastic and differentiated medullary thyroid carcinoma in the rat. Eur. J. Cancer 20, 967–973 (1984)
L. Hooft, A. Van der Veldt, P. Van Diest, O. Hoekstra, J. Berkhof, G. Teule, C. Molthoff, [18F] fluorodeoxyglucose uptake in recurrent thyroid cancer is related to hexokinase I expression in the primary tumor. J. Clin. Endocrinol. Metab. 90, 328–334 (2005)
L. Hooft, A. Van Der Veldt, O. Hoekstra, M. Boers, C. Molthoff, P. Van Diest, Hexokinase III, cyclin A and galectin‐3 are overexpressed in malignant follicular thyroid nodules. Clin. Endocrinol. (Oxf). 68, 252–257 (2008)
K. Imamura, T. TANAKA, Multimolecular forms of pyruvate kinase from rat and other mammalian tissues. J. Biochem. 71, 1043–1051 (1972)
H.R. Christofk, M.G. Vander Heiden, M.H. Harris, A. Ramanathan, R.E. Gerszten, R. Wei, M.D. Fleming, S.L. Schreiber, L.C. Cantley, The M2 splice isoform of pyruvate kinase is important for cancer metabolism and tumour growth. Nature 452, 230 (2008)
M.I. Koukourakis, A. Giatromanolaki, E. Sivridis, Lactate dehydrogenase isoenzymes 1 and 5: differential expression by neoplastic and stromal cells in non-small cell lung cancer and other epithelial malignant tumors. Tumor Biol. 24, 199–202 (2003)
C. Feng, Y. Gao, C. Wang, X. Yu, W. Zhang, H. Guan, Z. Shan, W. Teng, Aberrant overexpression of pyruvate kinase M2 is associated with aggressive tumor features and the BRAF mutation in papillary thyroid cancer. J. Clin. Endocrinol. Metab. 98, E1524–E1533 (2013)
V.R. Fantin, J. St-Pierre, P. Leder, Attenuation of LDH-A expression uncovers a link between glycolysis, mitochondrial physiology, and tumor maintenance. Cancer Cell. 9, 425–434 (2006)
D. Mirebeau-Prunier, S. Le Pennec, C. Jacques, J.-F. Fontaine, N. Gueguen, N. Boutet-Bouzamondo, A. Donnart, Y. Malthièry, F. Savagner, Estrogen-related receptor alpha modulates lactate dehydrogenase activity in thyroid tumors. PLoS ONE. 8, e58683 (2013)
P. Kachel, B. Trojanowicz, C. Sekulla, H. Prenzel, H. Dralle, C. Hoang-Vu, Phosphorylation of pyruvate kinase M2 and lactate dehydrogenase A by fibroblast growth factor receptor 1 in benign and malignant thyroid tissue. BMC. Cancer 15, 140 (2015)
A.P. Halestrap, The SLC16 gene family–structure, role and regulation in health and disease. Mol. Aspects. Med. 34, 337–349 (2013)
A.P. Halestrap, M.C. Wilson, The monocarboxylate transporter family—role and regulation. IUBMB Life 64, 109–119 (2012)
C. Pinheiro, A. Longatto-Filho, J. Azevedo-Silva, M. Casal, F.C. Schmitt, F. Baltazar, Role of monocarboxylate transporters in human cancers: state of the art. J. Bioenerg. Biomembr. 44, 127–139 (2012)
J.M. Johnson, S.Y. Lai, P. Cotzia, D. Cognetti, A. Luginbuhl, E.A. Pribitkin, T. Zhan, M. Mollaee, M. Domingo-Vidal, Y. Chen, Mitochondrial Metabolism as a Treatment Target in Anaplastic Thyroid Cancer. Semin Oncol. 42, 915–922 (2015)
J.M. Curry, P. Tassone, P. Cotzia, J. Sprandio, A. Luginbuhl, D.M. Cognetti, M. Mollaee, M. Domingo‐Vidal, E.A. Pribitkin, W.M. Keane, Multicompartment metabolism in papillary thyroid cancer. Laryngoscope 126, 2410–2418 (2016)
R.J. DeBerardinis, T. Cheng, Q’s next: the diverse functions of glutamine in metabolism, cell biology and cancer. Oncogene 29, 313 (2010)
C.L. Collins, M. Wasa, W.W. Souba, S.F. Abcouwer, Regulation of glutamine synthetase in human breast carcinoma cells and experimental tumors. Surgery 122, 451–464 (1997)
E. Friday, R. Oliver, T. Welbourne, F. Turturro, Glutaminolysis and glycolysis regulation by troglitazone in breast cancer cells: Relationship to mitochondrial membrane potential. J. Cell. Physiol. 226, 511–519 (2011)
H.M. Kim, Y.K. Lee, J.S. Koo, Expression of glutamine metabolism-related proteins in thyroid cancer. Oncotarget 7, 53628 (2016)
Y. Yu, X. Yu, C. Fan, H. Wang, R. Wang, C. Feng, H. Guan, Targeting glutaminase-mediated glutamine dependence in papillary thyroid cancer. J. Mol. Med. 96, 777–790 (2018)
J.-w Kim, P. Gao, Y.-C. Liu, G.L. Semenza, C.V. Dang, Hypoxia-inducible factor 1 and dysregulated c-Myc cooperatively induce vascular endothelial growth factor and metabolic switches hexokinase 2 and pyruvate dehydrogenase kinase 1. Mol. Cell. Biol. 27, 7381–7393 (2007)
H. Shim, C. Dolde, B.C. Lewis, C.-S. Wu, G. Dang, R.A. Jungmann, R. Dalla-Favera, C.V. Dang, c-Myc transactivation of LDH-A: implications for tumor metabolism and growth. Proc. Natl. Acad. Sci. 94, 6658–6663 (1997)
Y. Qu, Q. Yang, J. Liu, B. Shi, M. Ji, G. Li, P. Hou, c-Myc is required for BRAFV600E-induced epigenetic silencing by H3K27me3 in tumorigenesis. Theranostics 7, 2092 (2017)
J.-w Kim, I. Tchernyshyov, G.L. Semenza, C.V. Dang, HIF-1-mediated expression of pyruvate dehydrogenase kinase: a metabolic switch required for cellular adaptation to hypoxia. Cell Metab. 3, 177–185 (2006)
J. Pouysségur, F. Dayan, N.M. Mazure, Hypoxia signalling in cancer and approaches to enforce tumour regression. Nature 441, 437 (2006)
C.V. Dang, Kim J-w, P. Gao, J. Yustein, The interplay between MYC and HIF in cancer. Nat. Rev. Cancer 8, 51 (2008)
J.D. Gordan, C.B. Thompson, M.C. Simon, HIF and c-Myc: sibling rivals for control of cancer cell metabolism and proliferation. Cancer Cell. 12, 108–113 (2007)
O. Koperek, E. Akin, R. Asari, B. Niederle, N. Neuhold, Expression of hypoxia-inducible factor 1 alpha in papillary thyroid carcinoma is associated with desmoplastic stromal reaction and lymph node metastasis. Virchows. Arch. 463, 795–802 (2013)
A. Klaus, O. Fathi, T.-W. Tatjana, N. Bruno, K. Oskar, Expression of hypoxia-associated protein HIF-1α in follicular thyroid cancer is associated with distant metastasis. Pathol. Oncol. Res. 24, 289–296 (2018)
L. Lodewijk, P. van Diest, P. van der Groep, N. ter Hoeve, A. Schepers, J. Morreau, J. Bonenkamp, A. van Engen-van Grunsven, S. Kruijff, B. van Hemel, Expression of HIF-1α in medullary thyroid cancer identifies a subgroup with poor prognosis. Oncotarget 8, 28650 (2017)
Y. Lv, Y. Sun, T. Shi, C. Shi, H. Qin, Z. Li, Pigment epithelium-derived factor has a role in the progression of papillary thyroid carcinoma by affecting the HIF1α-VEGF signaling pathway. Oncol. Lett. 12, 5217–5222 (2016)
İ. Bingül, P. Vural, S. Doğru‐Abbasoğlu, E. Çil, M. Uysal, Vascular endothelial growth factor G + 405C polymorphism may contribute to the risk of developing papillary thyroid carcinoma. J. Clin. Lab. Anal. 31, e22110 (2017)
O. Baris, Fdr Savagner, Vr Nasser, Ba Loriod, S. Granjeaud, S. Guyetant, B. Franc, P. Rodien, V. Rohmer, Fo Bertucci, Transcriptional profiling reveals coordinated up-regulation of oxidative metabolism genes in thyroid oncocytic tumors. J. Clin. Endocrinol. Metab. 89, 994–1005 (2004)
E. Currie, A. Schulze, R. Zechner, T.C. Walther, R.V. Farese Jr, Cellular fatty acid metabolism and cancer. Cell Metab. 18, 153–161 (2013)
C.R. Santos, A. Schulze, Lipid metabolism in cancer. FEBS. J. 279, 2610–2623 (2012)
C.A. Von Roemeling, L.A. Marlow, A.B. Pinkerton, A. Crist, J. Miller, H.W. Tun, R.C. Smallridge, J.A. Copland, Aberrant lipid metabolism in anaplastic thyroid carcinoma reveals stearoyl CoA desaturase 1 as a novel therapeutic target. J. Clin. Endocrinol. Metab. 100, E697–E709 (2015)
Acknowledgements
This study is supported by a research grant from Endocrine Research Center, Shahid Beheshti University of Medical Sciences. The authors are grateful to Dr. S. Adeleh Razavi, Cellular and Molecular Endocrine Research Center (CMERC), Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, for critically reading the manuscript. The authors also would like to thank a graphic designer, Alireza Gerami, for his kind cooperation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animal performed by any of the authors.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abooshahab, R., Gholami, M., Sanoie, M. et al. Advances in metabolomics of thyroid cancer diagnosis and metabolic regulation. Endocrine 65, 1–14 (2019). https://doi.org/10.1007/s12020-019-01904-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-019-01904-1