Abstract
Purpose
Scanty data about glucose metabolism and hypertension have been reported in Paget’s disease of bone (PDB) to be related with increased cardiovascular mortality. The aim of the present study was to evaluate glucose and blood pressure levels in PDB, looking for their association with disease severity.
Methods
We performed an observational cross-sectional study in 54 patients with PDB and 54 age, sex and BMI-matched controls. Glucose and blood pressure levels and parameters of bone and mineral metabolism were assessed.
Results
Patients with PDB showed increased glucose levels (6.3 ± 1.7 vs 5.3 ± 1.4 mmol/l, p < 0.001) and prevalence of impaired fasting glucose (14.8%, 5.3–24.3 vs 1.9%, 0–5.4, p < 0.02) as well as enhanced systolic blood pressure (145.9 ± 21.3 vs 132.9 ± 18.9 mmHg, p < 0.005), pulse pressure (69.6 ± 20.0 vs 56.0 ± 16.9 mmHg, p < 0.01) and prevalence of isolated systolic hypertension (46.3%, 33.0–59.6 vs 16.7%, 6.7–26.6, p < 0.003) in comparison to controls. Moreover, we found a positive association of (1) glucose levels with ionized calcium and bone alkaline phosphatase; (2) both systolic and pulse pressure with total and bone alkaline phosphatase (p < 0.05). By multiple linear regression analysis (R2 = 0.26; p < 0.05) serum ionized calcium correlated with glucose levels (β = 0.44; p < 0.04), after adjusting for age and BMI.
Conclusions
Our study shows increased fasting glucose, systolic and pulse pressure levels as well as enhanced prevalence of impaired fasting glucose and isolated systolic hypertension in PDB, potentially accounting for increased cardiovascular mortality. Furthermore, our findings suggest high serum calcium and/or increased bone alkaline phosphatase as a link between PDB and cardio-metabolic disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paget’s disease of bone (PDB) is a focal disorder of bone remodeling affecting one or several bones, with preferential target on the axial skeleton [1]. The disease is mostly asymptomatic and incidentally diagnosed while performing bone imaging or evaluating serum alkaline phosphatase (ALP) levels for other clinical indications. Clinical complaints of the disease may consist of bone pain, fragility fracture, osteoarthritis and spinal stenosis, while less common manifestations are bone deformity, warmth of the skin overlying the affected bone and deafness. Other rare complications include high-output cardiac failure and hypercalcemia.
Interestingly, among various comorbidities, some very old reports described a higher prevalence of altered glucose tolerance and hypertension in PDB [2,3,4] leading to an enhanced cardiovascular morbidity and mortality [5], but these findings were not confirmed by other authors [6, 7] leaving the association between PDB and cardio-metabolic disorders a question unanswered until now.
Noteworthy, it has recently emerged that the skeleton probably acts as an endocrine organ with implications in the regulation of glucose and energy metabolism, which may be mediated by several factors including serum undercarboxylated osteocalcin and bone alkaline phosphatase (BAP) [8,9,10]. These factors could be highly synthesized and released in conditions of both systemic and focal enhanced bone turnover such as hyperparathyroidism and PDB. In fact many findings in primary and secondary hyperparathyroidism have shown an increased prevalence of cardio-metabolic disorders such as type 2 diabetes mellitus (DM2) and hypertension [11, 12]. Conversely, as anticipated, data on glucose metabolism and hypertension are scanty in PDB. Therefore we aimed to investigate the prevalence of impaired fasting glucose (IFG), DM2 and hypertension in PDB. Moreover, we looked also for the association between these cardio-metabolic disorders and biochemical indices of PDB severity after adjusting for confounding factors.
Materials and methods
Fifty-four patients with PDB and fifty-four controls were recruited among people referred consecutively to our Bone Metabolism Diseases Centre from January 2004 until December 2014, in order to perform an observational cross-sectional study. We enrolled controls among people with suspected osteoporosis, matching them to patients with PDB for sex, age (±5 years) and BMI (±2.5 kg/m2). Considering the exploratory nature of this research, we did not perform a power analysis and sample size estimation in designing the study.
Some PDB patients as well as some controls were previously treated with anti-resorptive agents included oral bisphosphonates, without significant differences among the two groups (data not shown). However, no intravenous bisphosphonates were administered before the study. Moreover, calcium and vitamin D supplementation was similar between PDB (33.3%, 20.8–45.9 and 64.8%, 52.1–77.6) and controls (48.1%, 34.8–61.5 and 59.3%, 46.2–72.4, respectively; p = NS).
Exclusion criteria include multiple endocrine neoplasia, hyperparathyroidism, familial hypocalciuric hypercalcemia, hypothyroidism, thyrotoxicosis, spontaneous or iatrogenic hypercortisolism and neoplastic diseases. People with severe physical limitations and those who were unable to perform activities of daily living were also excluded from the study.
At each participant’s visit, we collected weight and height, we calculated body mass index and we measured systolic (SBP) and diastolic blood pressure (DBP). The average of three measurements in a seated position after a 5 min rest was considered as the final SBP and DBP. Pulse pressure (PP) was calculated as the difference between SBP and DBP values. The diagnosis of PDB was based on the detection of typical bone lesions on plain radiographs of the involved regions of the skeleton and elevated serum BAP levels. Moreover, disease’s extension and activity were investigated also by bone scintigraphy. Diagnosis of IFG and DM2 were based on WHO criteria [13], while diagnosis of hypertension was made according to the The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology [14].
Serum total calcium (Ca, mmol/l) and phosphate (P, mmol/l) were tested using automated methods based on colorimetric and enzymatic assays (Cobas, Roche). For serum iCa (mmol/l) a specific probe was used after correction for pH. Intact PTH assay (ng/l) based on an immunoradiometric sandwich method (IRMA) that used two polyclonal antibodies (DiaSorin): an antibody, recognizing the C-terminal region (aa 39–84) was used as the capture antibody while an antibody recognizing the N-terminal region was used for detection. Serum 25 OH vitamin D (nmol/l) was tested by a radioimmunoassay method using an antibody with specificity to 25 OH vitamin D (DiaSorin). Plasma glucose (mmol/l) and creatinine levels (µmol/l), were measured by enzymatic colorimetric tests (Cobas, Roche). Glomerular filtration rate (GFR) was calculated according to Cockroft-Gault formula. ALP (UI/l) was tested using colorimetric assay in accordance with a standardized method (Cobas, Roche): in the presence of magnesium and zinc ions, p-nitrophenyl phosphate was cleaved by phosphatases into phosphate and p-nitrophenol, proportional to the ALP activity, that was measured photometrically. BAP (µg/l) was measured by an immunoradiometric sandwich method that uses mouse monoclonal antibodies directed against two different epitopes of BAP and hence not competing (Beckman Coulter).
Bone mineral density (BMD) was assessed by dual-energy x-ray absorptiometry (DXA) on a Hologic QDR 4500 instrument (Bedford, MA). BMD measurements are given as grams per square centimeter. Affected bones were excluded from DXA analysis. Fragility fracture rate was assessed by medical history recall supported by radiographic documentation including lateral vertebral radiographs.
Data are presented as mean ± SD or as mean, 95% confidence interval (CI). Normality of frequency distribution functions was tested by the Shapiro–Wilk W-test. Significant differences were sought by the Mann–Whitney U-test, ANOVA test or Pearson’s Χ2 analysis. Spearman’s R coefficient was used to look for associations of calcium metabolism parameters with glucose, systolic, diastolic and pulse pressure levels. Calculations were performed using SPSS Windows release 24.0; p < 0.05 was considered significant.
Results
Clinical and biochemical features of patients with PDB and controls are shown in Table 1. As expected we found no significant difference in age, sex distribution and BMI among the two groups.
PDB showed increased levels of ALP (mean ± SD: 437.5 ± 638 UI/l, p < 0.001), BAP (55.2 ± 34.5 µg/l, p < 0.001) and ionized calcium (1.16 ± 0.09 mmol/l, p < 0.02) in comparison to controls (67.1 ± 20.4 UI/l, 9.2 ± 5.1 µg/l and 1.11 ± 0.09 mmol/l, respectively). There was no difference in other metabolic bone parameters, creatinine and GFR between the two groups.
BMD (g/cm2) was not statistically different between patients with PDB (0.68 ± 0.25 at femoral neck and 0.84 ± 0.16 at lumbar spine) and controls (0.63 ± 0.18 and 0.82 ± 0.17, respectively, p = NS). Fragility fracture rate was also similar between the two groups (frequency %, 95% confidence interval: 29.6%, 17.5–41.8 vs 24.1%, 12.7–35.5, p = NS).
No difference was found among patients with PDB and controls in family history of Type 2 DM (5.6%, 0–11.7 vs 1.9%, 0–5.4, p = NS) and family history of CAD (1.9%, 0–5.4 vs 7.4%, 0.4–14.4, p = NS).
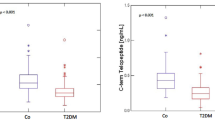
Table 2 shows fasting glucose, SBP, DBP and PP levels as well as prevalence of IFG and/or DM2 and hypertension in patients with PDB and controls.
We found that glucose levels in PDB were higher than in controls. This difference was maintained also after excluding patients on antidiabetic therapy or after excluding those with DM2. PDB showed glucose levels higher than controls even after adjusting for BMI (p < 0.04). Consistently, the former had an increased prevalence of IFG (14.8%, 5.3–24.3) in comparison to controls (1.9%, 0–5.4, p < 0.02), while there was no difference in frequency of DM2 (16.7%, 6.7–26.6 vs 13.0%, 4.0–21.9, p = NS) and use of antidiabetic drugs (9.3%, 1.5–17.0 vs 13.0%, 4.0–21.9, p = NS) between the two groups. When considering patients with IFG and DM2 as a whole group, prevalence was higher in PDB than in controls (31.5%, 19.1–43.9 vs 14.8%, 5.3–24.3, p < 0.05).
SBP and PP were significantly increased in PDB vs controls, even after excluding patients on antihypertensive therapy or those with hypertension. Moreover, PDB showed higher SBP and PP levels than controls even after adjusting for BMI (p < 0.02). Conversely, DBP was similar between the two groups even after adjusting for confounding factors. Accordingly we found an enhanced prevalence of isolated systolic hypertension (SH; 46.3%, 33.0–59.6 vs 16.7%, 6.7–26.6, p < 0.003) and a trend towards a higher prevalence of hypertension (51.9%, 38.5–65.2 vs 44.4%, 31.2–57.7, p = NS) and CAD (11.1%, 2.7–19.5 vs 5.6%, 0–11.7, p = NS) in PDB than in controls. There was no difference in use of anti-hypertensive drugs (50.0%, 36.7–63.3 vs 37.0%, 24.2–49.9, p = NS) between the two groups.
In all patients glucose and blood pressure levels were related in univariate analysis to some calcium metabolism parameters (Table 3). Both serum ionized calcium and BAP showed significant positive association with glucose levels, while both ALP and BAP were positively related to both SBP and PP. Considering all participants (i.e., PDB and controls), those with IFG showed higher serum ionized calcium levels than those without IFG (1.20 ± 0.06 vs 1.13 ± 0.10, p < 0.05), while patients with hypertension showed higher BAP levels than those without hypertension (49.2 ± 32.1 vs 39.7 ± 38.4 µg/l, p < 0.05).
In a model of multiple linear regression (R2 = 0.26; p < 0.05), serum ionized calcium was significantly correlated with glucose levels (β = 0.44; p < 0.04) after adjusting for age and BMI.
Discussion
In present study in Paget’s disease of bone (PDB) we find increased fasting glucose levels as well as enhanced prevalence of impaired fasting glucose (IFG); also the prevalence of IFG and type 2 diabetes mellitus (DM2) as a whole was higher in PDB than in controls. Similarly we show higher systolic blood pressure (SBP) and pulse pressure (PP) values and increased frequency of isolated systolic hypertension (SH) in PDB than in controls. Moreover glucose levels show positive correlation with bone alkaline phosphatase (BAP) and ionized serum calcium, while SBP and PP display a relationship with both total alkaline phosphatase (ALP) and BAP.
In 40’s some authors had reported metabolic alterations in PDB, including glucose intolerance and hypertension which could partly explain the reduced survival observed in this disease [2,3,4], though these studies were carried out in small sample size, in the absence of well-matched control groups and without reporting some relevant biochemical features and other clinical confounding factors. These findings were questioned by more recent studies that did not describe any correlation between PDB and DM2, hypertension [5] and CAD [6]. However, these last authors performed epidemiological reports not specifically designed to investigate cardio-metabolic alterations in PDB, so that various bias could hamper their results. In fact, in these studies, participants were not matched for BMI and were not characterized about family history of DM2, hypertension and CAD, with one study even performed as questionnaire-based survey. Accordingly, the lack of difference among PDB and controls in prevalence of gout, a well-known and typical finding in PDB [6], supports patients’ selection bias. Conversely, in present report, we perform a well-designed cross-sectional study with PDB patients and controls matched for age, sex and BMI. Moreover, in comparison to the above-mentioned old reports, we reach a larger sample size and we analyze other relevant biochemical and clinical factors known to affect glucose metabolism and blood pressure. Furthermore, the increased prevalence of IFG and SH in PDB is supported by the relationship of some bone and mineral parameters with glucose and blood pressure levels.
It has been previously hypothesized that in PDB an accelerated rate of intestinal glucose absorption and an increased dephosphorylation of glucose phosphates mediated by the elevated serum BAP could contribute to glucose intolerance [3], whereas the loss of elasticity in calcified vessels or nephrosclerosis might lead to hypertension [4]. However, it could be that also other alterations in calcium metabolism parameters and/or factors released from typical focal bone lesions due to high bone turnover are potentially involved. Among these, hypercalcemia has been reported in PDB [7], possibly ascribed to increased bone resorption in pagetic skeletal lesions and/or reduced physical activity. Our data suggest a role of serum calcium in determining the alterations of glucose metabolism in PDB. In fact, we found ionized calcium levels to be higher in PDB than in controls and we observed a positive correlation between ionized serum calcium and glucose levels, even after adjusting for age and BMI. Consistently, many studies in other clinical settings have shown an association between increased calcium levels and glucose intolerance. For example, in primary hyperparathyroidism increased frequency of cardiovascular risk factors including insulin resistance, glucose intolerance and metabolic syndrome have been reported [11, 15]. Moreover, a relationship between serum calcium and glucose tolerance has been documented also in a population-based cohort study involving adult people free of known DM2 [16].
It has also been suggested by some authors that the increased levels of BAP in PDB might be a contributory factor in developing altered glucose tolerance [3]. Accordingly, our data indicate a relationship between this biochemical index and glucose levels in PDB. Consistently, in a recent large cross-sectional study involving people without DM2, Cheung et al. [10] found a positive and significant correlation between BAP and both glucose levels and insulin resistance. It may be that an increased bone turnover, through the release of BAP and/or other molecules, would promote the onset of insulin resistance and then altered glucose metabolism. In line with these findings, a recent retrospective cohort study suggested that the exposure to bisphosphonates, anti-resorptive agents able to suppress BAP and bone resorption, could be associated with a significant reduction in the risk of incident DM2 [17].
As already known, undercarboxylated osteocalcin has shown to be involved in regulation of glucose metabolism, probably stimulating both pancreatic β-cell proliferation and insulin secretion, as well as improving insulin sensitivity [18]. One might speculate that in a high bone turnover disease like PDB, changes in undercarboxylated osteocalcin levels could induce some effects on glucose metabolism. However, serum osteocalcin is less consistently raised in PDB compared with other formation markers such as ALP and procollagen type-1 N-terminal propeptide [19] and some authors found a normal fraction of decarboxylated osteocalcin in PDB [20]. In line with current clinical practice we focused on ALP and BAP levels and so we did not collect osteocalcin levels in our study.
The high prevalence of hypertension in PDB could be likely associated with the above-mentioned altered glucose tolerance and increased insulin resistance. In fact, higher BAP levels could contribute to this association leading to both enhanced insulin resistance and vascular calcification in PDB. Accordingly, other high bone turnover diseases, like primary hyperparathyroidism, could be associated with an increased vascular calcification, endothelial dysfunction and peripheral vascular resistance, promoting hypertension and cardiovascular morbidity [21]. In line with these data, it has been shown that BAP levels correlate, beyond insulin resistance, also with mean arterial pressure leading to hypothesize that BAP may be the link between insulin resistance and vascular calcification as well as cardiovascular events [10]. However, the cross-sectional nature of this study does not allow to surely define the direction of causality and it also maybe that an increased bone turnover, through the release of BAP, would promote the onset of insulin resistance, hypertension and increased cardiovascular morbidity and mortality. In addition, as already known, people with PDB is characterized by an increased cardiac output caused by an enhanced blood flow through normally constituted but quantitatively increased osseous vascular bed in pagetic lesions, leading to an increased SBP. Furthermore, these anatomic alterations comprised of enlarged vascular bed could lead to reduced peripheral resistance accounting for the lack of increased DBP in our study and contributing to the increase in PP.
Overall IFG, SH and increased PP may account for the trend towards higher prevalence of CAD that we find in affected patients, in line with the reduced survival due to diseases of the circulatory system reported as the first cause of death in PDB [5].
On the other hand we recognize that our study has some limitations. Firstly, its cross-sectional design does not allow to exclude the casual association between PDB and cardio-metabolic alterations. In fact, it has to be noted that PDB as well as altered glucose metabolism and hypertension are more common in the elderly and could be coincident in the same individual. Moreover, we did not perform glucose tolerance tests and we did not measure either insulin, glycosylated hemoglobin and insulin resistance indices to better characterize glucose metabolism, or other components of metabolic syndrome. Furthermore, we did not evaluate C-peptide levels, deemed to promote bone formation [22]. Finally, due to the exploratory nature of this investigation, we did not perform a power analysis and sample size estimation in designing the study. Nevertheless, strength of our findings is the relatively high sample size, considering the low prevalence of PDB in general population and the well controlled study design with participants comparable for age, sex, BMI and other factors known to affect glucose metabolism and blood pressure.
In conclusion our data show an increased prevalence of IFG and SH, as well as enhanced PP in PDB, potentially accounting for increased death due to diseases of the circulatory system. Furthermore, they suggest increased BAP and/or serum ionized calcium as factors contributing to cardio-metabolic diseases.
References
S.H. Ralston, Clinical practice. Paget’s disease of bone. N. Engl. J. Med. 368(7), 644–50 (2013)
R.C. Moehlig, H.L. Abbott, Carbohydrate metabolism in osteitis deformans, or Paget’s disease. J. Am. Med. Assoc. 134(18), 1521–4 (1947)
N.G. Schneeberg, Observations on the glucose tolerance test in Paget’s disease (osteitis deformans). Am. J. Med. Sci. 219(6), 664–73 (1950)
C.F. Sornberger, M.I. Smedal, The mechanism and incidence of cardiovascular changes in Paget’s disease (osteitis deformans); a critical review of the literature with case studies. Circulation 6(5), 711–26 (1952)
T.P. Van Staa, P. Selby, H.G.M. Leufkens, K. Lyles, J.M. Sprafka, C. Cooper, Incidence and natural history of Paget’s disease of bone in England and Wales. J. Bone Miner. Res. 17(3), 465–71 (2002)
E.S. Siris, Epidemiological aspects of Paget’s disease: family history and relationship to other medical conditions. Semin. Arthritis Rheum. 23(4), 222–5 (1994)
R.A. Wermers, R.D. Tiegs, E.J. Atkinson, S.J. Achenbach, L.J. Melton, Morbidity and mortality associated with Paget’s disease of bone: a population-based study. J. Bone Miner. Res. 23(6), 819–25 (2008)
T.A.P. Fernandes, L.M.L. Gonçalves, J.A.A. Brito, Relationships between bone turnover and energy metabolism. J. Diabetes Res. 2017, 9021314 (2017)
M. Ghodsi, B. Larijani, A.A. Keshtkar, E. Nasli-Esfahani, S. Alatab, M.R. Mohajeri-Tehrani, Mechanisms involved in altered bone metabolism in diabetes: a narrative review. J. Diabetes Metab. Disord. 15, 52 (2016)
C.L. Cheung, K.C.B. Tan, K.S.L. Lam, B.M.Y. Cheung, The relationship between glucose metabolism, metabolic syndrome, and bone-specific alkaline phosphatase: a structural equation modeling approach. J. Clin. Endocrinol. Metab. 98(9), 3856–63 (2013)
M. Procopio, M. Barale, S. Bertaina, S. Sigrist, R. Mazzetti, M. Loiacono, G. Mengozzi, E. Ghigo, M. Maccario, Cardiovascular risk and metabolic syndrome in primary hyperparathyroidism and their correlation to different clinical forms. Endocrine 47(2), 581–9 (2014)
E. Kamycheva, R. Jorde, Y. Figenschau, E. Haug, Insulin sensitivity in subjects with secondary hyperparathyroidism and the effect of a low serum 25-hydroxyvitamin D level on insulin sensitivity. J. Endocrinol. Invest. 30(2), 126–32 (2007)
World Health Organization, International Diabetes Federation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation (2006), http://www.who.int/diabetes/publications/diagnosis_diabetes2006/en/. Accessed 12 Apr 2018
G. Mancia, 2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood. Press. 23(1), 3–16 (2014)
R. Luboshitzky, Y. Chertok-Schaham, I. Lavi, A. Ishay, Cardiovascular risk factors in primary hyperparathyroidism. J. Endocrinol. Invest. 32(4), 317–21 (2009)
N.J. Wareham, C.D. Byrne, C. Carr, N.E. Day, B.J. Boucher, C.N. Hales, Glucose intolerance is associated with altered calcium homeostasis: a possible link between increased serum calcium concentration and cardiovascular disease mortality. Metabolism 46(10), 1171–7 (1997)
K.A. Toulis, K. Nirantharakumar, R. Ryan, T. Marshall, K. Hemming, Bisphosphonates and glucose homeostasis: a population-based, retrospective cohort study. J. Clin. Endocrinol. Metab. 100(5), 1933–40 (2015)
P. Tangseefa, S.K. Martin, S. Fitter, P.A. Baldock, C.G. Proud, A.C.W. Zannettino, Osteocalcin-dependent regulation of glucose metabolism and fertility: Skeletal implications for the development of insulin resistance. J. Cell. Physiol. 233(5), 3769–83 (2018)
S. Shankar, D.J. Hosking, Biochemical assessment of Paget’s disease of bone. J. Bone Miner. Res. 21(Suppl 2), P22–27 (2006)
B. Merle, P.D. Delmas, Normal carboxylation of circulating osteocalcin (bone Gla-protein) in Paget’s disease of bone. Bone Miner. 11(2), 237–45 (1990)
C. Letizia, P. Ferrari, D. Cotesta, C. Caliumi, R. Cianci, S. Cerci, L. Petramala, M. Celi, S. Minisola, E. D’Erasmo, G.F. Mazzuoli, Ambulatory monitoring of blood pressure (AMBP) in patients with primary hyperparathyroidism. J. Hum. Hypertens. 19(11), 901–6 (2005)
A. Pujia, C. Gazzaruso, T. Montalcini, An update on the potential role of C-peptide in diabetes and osteoporosis. Endocrine 58(3), 408–12 (2017)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Due to the retrospective design of the study, formal informed consent is not required.
Rights and permissions
About this article
Cite this article
Barale, M., Cappiello, V., Ghigo, E. et al. Increased frequency of impaired fasting glucose and isolated systolic hypertension in Paget’s disease of bone. Endocrine 63, 385–390 (2019). https://doi.org/10.1007/s12020-018-1771-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-018-1771-5