Abstract
Background
Diabetes self-management education is an essential part of diabetes care, but its impact on all-cause mortality risk of type 2 diabetes patients is unclear. A systematic review and meta-analysis aiming to elucidate the impact of diabetes self-management education on all-cause mortality risk of type 2 diabetes patients was performed.
Methods
Randomised controlled trials were identified though literature search in Medline, Embase, CENTRAL, conference abstracts, and reference lists. Only randomised controlled trials comparing diabetes self-management education with usual care in type 2 diabetes patients and reporting outcomes after a follow-up of at least 12 months were considered eligible. Risk ratios with 95 %CIs were pooled. This study was registered at PROSPERO with the number of CRD42016043911.
Results
42 randomised controlled trials containing 13,017 participants were included. The mean time of follow-up was 1.5 years. There was no heterogeneity among those included studies (I 2 = 0 %). Mortality occurred in 159 participants (2.3 %) in the diabetes self-management education group and in 187 (3.1 %) in the usual care group, and diabetes self-management education significantly reduced risk of all-cause mortality in type 2 diabetes patients (pooled risk ratios : 0.74, 95 %CI 0.60–0.90, P = 0.003; absolute risk difference: −0.8 %, 95 %CI −1.4 to −0.3). Both multidisciplinary team education and nurse-led education could significantly reduce mortality risk in type 2 diabetes patients, and the pooled risk ratios were 0.66 (95 %CI 0.46–0.96, P = 0.02; I 2 = 0 %) and 0.64 (95 % CI 0.47– 0.88, P = 0.005; I 2 = 0 %), respectively. Subgroup analyses of studies with longer duration of follow-up (≥1.5 years) or larger sample size (≥300) also found a significant effect of diabetes self-management education in reducing mortality risk among type 2 diabetes. Significant effect of diabetes self-management education in reducing mortality risk was also found in those patients receiving diabetes self-management education with contact hours more than 10 h (pooled risk ratio: 0.60, 95 %CI 0.44–0.82, P = 0.001; I 2 = 0 %), those receiving repeated diabetes self-management education (pooled RR: 0.71, P = 0.001; I 2 = 0 %), those receiving diabetes self-management education using structured curriculum (pooled risk ratio: 0.72, P = 0.01; I 2 = 0 %) and those receiving diabetes self-management education using in-person communication (pooled risk ratio: 0.75, P = 0.02; I 2 = 0 %). The quality of evidence for the effect of diabetes self-management education in reducing all-cause mortality risk among type 2 diabetes patients was rated as moderate according to the Grading of Recommendations Assessment, Development, and Evaluation method, and the absolute risk reduction of all-cause mortality of type 2 diabetic patients by diabetes self-management education was estimated to be 4 fewer per 1000 person-years (from 1 fewer to 6 fewer).
Conclusions
The available evidence suggests that diabetes self-management education can reduce all-cause mortality risk in type 2 diabetes patients. Further clinical trials with longer time of follow-up are needed to validate the finding above.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes is a serious issue for public health worldwide and its global pandemic is still obviously increasing [1]. The incidence rate of type 2 diabetes in the United States was 7.1 per 1000 persons in 2012, and the estimated prevalence of type 2 diabetes among adults in the United States was 14 % in 2012, both of which had increased obvious since 1980s [2, 3]. There are approaching 400 million people suffering from diabetes worldwide, which largely results from high prevalent obesity and sedentary lifestyle changes in recent decades and has become a serious burden of public health worldwide [4]. Patients with types 2 diabetes are also at high risk of cardiovascular diseases and all-cause mortality [5–8]. High quality medical care and multifactorial risk-reduction interventions are needed to reduce the burden of microvascular and cardiovascular diseases, and improve the outcomes of types 2 diabetes patients [9, 10].
Diabetes self-management education (DSME) is an essential part of diabetes care [11, 12]. Guidelines for the treatment of diabetes recommend that all diabetes patients should take part in DSME to improve clinical outcomes and quality of life [11–13]. DSME can help types 2 diabetes patients improve the knowledge, skills, and ability of self-management in a cost-effective manner [12]. Several systematic reviews have suggested that DSME can improve patients’ self-management and blood glucose control, and it should be regarded as a crucial element in the treatment of diabetes [14–20]. DSME could lead to more than 0.4 % reduction in hemoglobin A1c (HbA1c) of type 2 diabetes patients, more than 5 mg/dl reduction in total cholesterol, and more than 1 mmol/L reduction in fasting blood glucose [14–19]. However, these systematic reviews focused on short-term outcomes, but the impact of DSME on long-term outcomes, such as all-cause mortality, had not been sufficiently assessed. The impact of DSME on all-cause mortality risk in type 2 diabetes patients is critical but is still unclear. A systematic review and meta-analysis was thus carried out to elucidate this question. The aim of this systematic review was to assess the effect of DSME in reducing risk of all-cause mortality among type 2 diabetes patients compared with usual care. This systematic review was registered at International Prospective Register of Systematic Reviews (PROSPERO) with the number of CRD42016043911. This study was reported by PRISMA statement [21].
Methods
Search strategy and selection criteria
Randomised controlled trials were identified though literature search in Medline, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) (from inception to June 2016). The conference abstracts from American Diabetes Association were also searched. In addition, the reference lists of relevant systematic reviews or relevant reviews were further searched [14–20, 22–31]. Both key words and Medical Subject Heading (MESH) terms were used, and the search strategies for Medline were: (“Self Care”[Mesh] OR “Health Behavior”[Mesh] OR “Education”[Mesh] OR “Behavior Therapy”[Mesh] OR self-care OR self-management OR educational OR education OR educator* OR lifestyle OR management program OR behavioral intervention* OR behavior intervention* OR case management) AND (“Diabetes Mellitus, Type 2”[Mesh] OR diabetes mellitus OR diabetes OR diabetic OR T2DM OR NIDDM) AND (“Randomized Controlled Trial” [Publication Type] OR random OR randomly OR randomized OR randomised OR double blind OR placebo controlled OR randomized controlled trial). No language restriction was applied in the literature search.
The inclusion criteria in the meta-analysis were: (1) randomised controlled trial; (2) individuals with type 2 diabetes; (3) compared DSME with usual care; (4) had a follow-up or intervention duration of at least 12 months; (5) reported events of all-cause mortality in each treatment groups. Studies were excluded if they were non-random trials, used an active comparator, used minimal intervention, compared the effect of different types of DSME, or had a follow-up of less than 12 months.
Data extraction and quality assessment
The primary outcome of interest was the risk ratio (RR) of all-cause mortality. The secondary outcome of interest was the absolute risk difference of all-cause mortality between two groups. Two investigators independently extracted data by using a structured form, and differences were settled by reaching consensus. Data extracted from included studies were as following: family name of first author, publication year, study design, newly-diagnosed or previously treated diabetes, types of DSME, duration of DSME, primary instructors, delivery methods (Group, individual, or mixed), communication methods (in person, through telephone, or mixed), use of structured curriculum or not, participants’ characteristics (age, sex, number, and disease duration), duration of follow-up, rate of drop-out, and events of mortality between two groups. The Cochrane Collaboration’s tool was used to assess the risk of bias of those included studies, which included selection bias, detection bias, performance bias, attrition bias, reporting bias, adequacy of follow-up, and bias from other possible sources [32].
Statistical analysis
The pooled RRs or risk difference with corresponding 95 %CIs were used to compare treatment effects. Both Cochrane’s Q test and I 2 test were used to evaluate the degree of heterogeneity, and I 2 > 50 % indicated high heterogeneity [33, 34]. For the existence of obvious heterogeneity, the random-effects model was used to pool data by DerSimonian–Laird method [35]; otherwise, the fixed-effects model was used to pool data by Mantel–Haenszel method [36]. Sensitivity analyses were performed by using alternative pooling methods, including Peto’s method and random-effect model [37]. Subgroup analyses were carried out by number of participants (≥300 vs. <300), follow-up (≥1.5 years vs. <1.5 years), contact hours (≥10 vs. <10 h), primary instructors (multidisciplinary team, nurses, or others), types of diabetes (newly diagnosed vs. previously treated), delivery methods (group only, individual delivery, or mixed), communication methods (in-person, through technology, or mixed), types of DSME (repeated courses vs. single course), structured curriculum (yes vs. unclear), study design (randomised controlled trial vs. cluster randomised controlled trial). Subgroup analysis of patients with secondary diseases was also performed. Publication bias was assessed by funnel plot, Begg’s test and Egger’s test [37–39]. Statistical analyses were carried out using Review Manager (Version 5.1.0) and Stata (Version 12.0). P value <0.05 indicated statistically significant difference. The quality of evidence was rated from very low to high by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) method, which reflected the confidence that the pooled effect estimate was correct [40].
Results
Characteristics of included studies
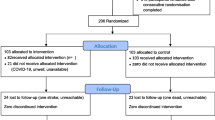
Of 10,559 studies identified through literature searches, 306 studies were retrieved for detailed assessment for further assessment (Fig. 1). A total of 264 full-text articles excluded, including 181 studies without outcomes on mortality, 61 studies for not relevant to DSME, 19 studies for not using usual care as control, and three studies with overlapping data (Supplementary material). Therefore, 42 randomised clinical trials were eligible for inclusion in meta-analysis [41–82]. The characteristics of these studies were described in Table 1 (Table 1). There were 37 randomised controlled trials [41–43, 45–55, 57, 59, 60, 62–77, 79–82] and 5 cluster randomised controlled trials [44, 56, 58, 61, 78] with a total of 13,017 participants (Table 1).
Among these 42 trials, 34 studies were performed in previously treated diabetes patients, five were performed in newly diagnosed diabetes patients (Table 1). The time of follow-up ranged from 12 months to 5 years, and the mean time of follow-up was 1.5 years (Table 1). 40 studies were performed in developed countries, while the other studies were performed in Argentina and India (Table 1). The sample sizes ranged from 58 to 1146, with a mean of 310. There was lack of clear definitions of “usual care” in most included studies, and there were also obvious differences in the methods of DSME interventions in different studies (Table 1). Among those 42 included trials, only 6 trials studied type 2 diabetes patients with comorbidities or diabetic complications, and the other trials included newly diagnosed or treated type 2 diabetes patients but didn’t focus on type 2 diabetes patients with specific comorbidities or complications (Table 1). Most included studies used routine hypoglycemic medications to treat diabetes (Table 1). Nurses were the primary instructors in 18 trials, and multidisciplinary team was the primary instructors in 13 trials (Table 1). The primary instructors in other studies were trained professional educators, pharmacists or community health workers (Table 1). Only 11 studies provided DSME with contact hours more than 10 h, and 18 studies reported they used structured curriculums (Table 1).
The outcomes of bias assessment of these 42 included studies were shown in Fig. 2 (Fig. 2). There was no obvious risk of selection bias (Fig. 2). However, owing to the nature of DSNE intervention, few of the interventions were blind and there was obvious risk of performance bias across most included studies (Fig. 2). In addition, some studies also had high drop-out rates (Fig. 2, Table 1). The proportion of patients lost to follow-up was reported in most studies, ranging from 0.3 to 19.7 % (Table 1).
Meta-analysis
Table 2 summarized the main findings of the meta-analysis (Table 2). There was no heterogeneity among those included studies (I 2 = 0 %). Mortality occurred in 159 participants (2.3 %) in the DSME group and in 187 (3.1 %) in the usual care group, and DSME significantly reduced risk of all-cause mortality in type 2 diabetes patients (pooled RR: 0.74, 95 % CI 0.60–0.90, P = 0.003; absolute risk difference: −0.8 %, 95 % CI −1.4 to −0.3) (Fig. 3). When using random-effect model, the pooled RR of all-cause mortality in the DSME group compared with the usual care group was 0.74 (95 % CI 0.60–0.91, P = 0.005). When using Peto’s method, the pooled Peto’s odds ratio of all-cause mortality in the DSME group compared with the usual care group was 0.72 (95 % CI 0.58–0.89, P = 0.003; I 2 = 0 %).
Meta-analysis of 20 trials with longer duration of follow-up (≥1.5 years) also suggested that DSME could obviously reduce all-cause mortality risk in type 2 diabetes patients (pooled RR: 0.72, 95 % CI 0.57–0.92, P = 0.007; absolute risk difference: −1.1 %, 95 % CI −1.8 to −0.3) (Fig. 4, Table 2). Meta-analysis of 13 studies with larger sample size (≥300) further suggested that DSME was obviously associated with decreased mortality risk in type 2 diabetes patients (pooled RR: 0.73, 95 % CI 0.56–0.96, P = 0.02; absolute risk difference: −0.8 %, 95 % CI −1.6 to −0.1) (Fig. 4, Table 2).
Both multidisciplinary team education and nurse-led education could reduce mortality risk, and the RRs were 0.66 (95 % CI 0.46–0.96; P = 0.02; I 2 = 0 %) and 0.64 (95 % CI 0.47–0.88; P = 0.005; I 2 = 0 %), respectively (Fig. 4, Table 2). Further subgroup analyses revealed significant effects of DSME in reducing all-cause mortality risk among type 2 diabetes patients receiving DSME with contact hours more than 10 h (pooled RR: 0.60, 95 % CI 0.44–0.82; P = 0.001; I 2 = 0 %), repeated DSME (pooled RR: 0.71, 95 % CI 0.57–0.87; P = 0.001; I 2 = 0 %), DSME using structured curriculum (pooled RR: 0.72, 95 % CI 0.55–0.93; P = 0.01; I 2 = 0 %), or DSME using in-person communication (pooled RR: 0.75, 95 % CI 0.58–0.96; P = 0.02; I 2 = 0 %) (Fig. 4, Table 2).
There were only two randomised controlled trials reporting risk of cardiovascular mortality [41, 42], and there was no heterogeneity between those two studies (I 2 = 0 %). Meta-analysis suggested that DSME was not significantly associated with reduced risk of cardiovascular mortality (pooled RR: 0.56, 95 % CI 0.19–1.65, P = 0.29).
The shape of funnel plots did not show evidence of asymmetry (Fig. 5). The P values of Begg’s test and Egger’s test in the meta-analysis of total 42 studies were 0.34 and 0.11, respectively. In the subgroup analysis of 13 studies with larger sample size (≥300), the P values of Begg’s test and Egger’s test were 0.99 and 0.67, respectively. Therefore, there was no obvious risk of publication bias.
Most studies did not report mortality as primary outcomes of interest and there was possible risk of performance bias (Fig. 2). In addition, since the mean time of follow-up was 18 months, the rates of mortality in patients receiving DSME or usual care were 2.3 and 3.1 % respectively, which were relatively low. Taking into account the above factors, the quality of evidence for the effect of DSME in reducing all-cause mortality risk among type 2 diabetes patients was rated as moderate according to GRADE method. The incidences of all-cause mortality in patients receiving DSME and those receiving usual care were 12 and 16 events per 1000 person-years, respectively. The absolute risk reduction in all-cause mortality in type 2 diabetes by DSME was estimated to be 4 fewer per 1000 person-years (from 1 fewer to 6 fewer).
Discussion
DSME is believed to be an essential element of diabetes care, but its impact on all-cause mortality risk in type 2 diabetes patients has not been systematically assessed. We thus did a systematic review and meta-analysis to elucidate the impact of DSME on all-cause mortality risk in type 2 diabetic patients. This study systematically reviewed 42 randomised controlled trials comparing DSME with usual care in type 2 diabetic patients. There was no heterogeneity among those included studies (I 2 = 0 %). Meta-analysis of total 42 trials suggested that DSME significantly reduced risk of all-cause mortality more than usual care in type 2 diabetes patients (pooled RR: 0.74, 95 % CI 0.60–0.90; P = 0.003; I 2 = 0 %) (Fig. 3). Subgroup analyses of studies with longer duration of follow-up (≥1.5 years) or larger sample size (≥300) also found a beneficial effect of DSME in reducing mortality risk among type 2 diabetes (Table 2, Fig. 4). Significant effect of DSME in reducing mortality risk was also found in those patients receiving DSME with contact hours more than 10 h, those receiving repeated DSME, those receiving DSME using structured curriculum and those receiving in-person communication (Table 2, Fig. 4). Therefore, the findings from the meta-analysis suggest that DSME can reduce risk of all-cause mortality in type 2 diabetes patients when compared with usual care, which supports the practice of DSME in type 2 diabetes to improve patients’ outcomes.
DSME is a cost-effective intervention which can help types 2 diabetes patients improve their self-management, and the short-term effect of DSME on HbA1c and BMI has been well established [14–18]. The finding from our study suggests that DSME can also effectively reduce mortality risk in type 2 diabetes patients. The absolute risk reduction in all-cause mortality by DSME was estimated to be 4 fewer per 1000 person-years (from 1 fewer to 6 fewer). The finding above is important, because DSME is a cost-effective method of reducing mortality risk in diabetes patients. Our findings also suggest the necessity and importance of DSME in the medical care for type 2 diabetes patients. Guidelines for the treatment of diabetes also recommend that all diabetes patients should take part in DSME to improve clinical outcomes and quality of life [11–13]. However, recent studies have shown that a large part of diabetes patients do not receive any diabetes education, and fewer than 50 % have participated in DSME, which is a serious problem that should be avoided [83, 84]. Therefore, to achieve better self-management and improve patients’ survival, it’s urgent for all diabetes patients to receive effective and structured DSME. In addition, quality improvement strategies aiming to increase access to DSME for type 2 diabetes patients are also needed in clinical practice [85, 86].
There is also some evidence from observational studies which supports the effect of DSME in reducing all-cause mortality risk among type 2 diabetes. Wong et al. performed a propensity-matched observational study of 27,278 type 2 diabetes patients and found that participants receiving structured diabetes education had a lower risk of all-cause mortality (Hazard ratio [HR]: 0.564, P < 0.001) [87]. Kornelius et al. also carried out a propensity-matched observational study of 8916 type 2 diabetes patients and found that participants receiving integrated diabetes education had a significantly lower risk of all-cause mortality (HR 0.78, 95 % CI 0.63–0.95) [88]. However, another propensity-matched observational study of 16,520 type 2 diabetes patients failed to find a beneficial effect of DSME in reducing all-cause mortality risk among patients (HR 0.97; P = 0.48) [89]. A retrospective cohort study by Perman et al. found that patients attending self-management education workshop had 33 % lower risk of all-cause crude mortality, but the effect estimate decreased after adjustment (HR 0.82; 95 % CI: 0.61–1.08) [90]. Despite there was obvious heterogeneity among those four observational studies [87–90] (I 2 = 89 %), meta-analysis of those four studies using random-effect model suggested that DSME was independently associated with decreased risk of all-cause mortality in type 2 diabetes patients (Pooled HR: 0.778, 96 % CI 0.607–0.998; P = 0.048). Therefore, there is also evidence from observational studies which supporting the effect of DSME in reducing all-cause mortality risk in type 2 diabetes, and DSME can be a significant contributor to long-term positive outcomes. The findings from observational studies also further validate the results of our meta-analysis of randomised controlled trials.
GRADE is a well-known system for rating the quality of evidence and strength of recommendations [40]. In present meta-analysis, GRADE was also used to assess the quality of evidence for the effect of DSME in reducing all-cause mortality risk among type 2 diabetes. Generally, there was moderate quality evidence for the effect of DSME in reducing mortality risk in type 2 diabetes patients, and the reasons for the decrease of evidence quality from high to moderate were the possible of risk of performance bias and the short time of follow-up in most included studies. Risk of performance bias is ineluctable because blinding of participants and personnel with respect to study design is almost impossible in clinical trials involving behavioral interventions. However, it’s feasible for clinical trials to prolong the duration of DSME or time of follow-up. Therefore, randomised controlled trials with a longer time of follow-up are urgently needed to identify the long-term beneficial effect of DSME in reducing mortality risk in type 2 diabetes patients [20, 22, 91].
Previous studies and meta-analyses have shown that DSME can improve patients’ self-management and blood glucose control when compared to usual care, and it has been considered a crucial element in the treatment of type 2 diabetes [14–20]. However, there is little evidence regarding the potential effect of DSME in reducing the risks of complications and mortality among type 2 diabetes patients. As is reported, our meta-analysis of 42 randomised controlled trials provides some evidence for the benefit of DSME in reducing the risk of mortality among type 2 diabetes patients, which further proves the importance of delivering a structured DSME to type 2 diabetic patients. Owing to the limited number of randomised controlled trials providing data on the impact of DSME on diabetic complications in type 2 diabetes patients, we didn’t perform a meta-analysis to assess the impact of DSME on diabetic complications in type 2 diabetes patients. However, several cohort studies have found that DSME may have a positive impact on the prevention of diabetic complications [22, 92, 93]. Therefore, DSME may also be an essential tool to reduce the occurrence of complications in type 2 diabetes patients [22]. On the contrary, an omission in delivering DSME in type 2 diabetes patients may have negative effects on the occurrence of complications and mortality [22].
There are a wide variety of self-management education programs for patients with chronic diseases [94–99], and it is the same with for DSME in type 2 diabetes patients [11, 16, 100]. At the moment, the ideal characteristics of DSME to provide the best benefit in type 2 diabetes patients have not been well defined [20, 22]. Structured DSME involving multiple topics usually provide more comprehensive interventions and benefits when compared with other simple DSME [12, 22]. However, although guidelines for the treatment of diabetes recommend structured DSME to type 2 diabetes patients, it is not always perceived by both health professionals and diabetes patients. In addition, there are many good models for DSME, but which type of DSME is the best cost-effectiveness intervention is still unclear and need future studies [12, 22]. In present meta-analysis, there were obvious variations in educational interventions used among included studies (Table 2).
In the subgroup analyses, significant effect of DSME in reducing all-cause mortality risk among type 2 diabetes was found in those patients receiving DSME with contact hours more than 10 h, those receiving repeated DSME, those receiving DSME using structured curriculum, and those receiving DSME using in-person communication (Table 2, Fig. 4). In structured DSME involving more or longer sessions, diabetes patients will have more opportunities to learn useful messages and gain more benefits from DSME, which may explain the significant findings in above subgroup analyses. On the contrary, DSME with shorter intervention durations or fewer topics may provide little benefit for type 2 diabetes patients.
There were several limitations in the meta-analysis. Firstly, there was lack of clear definitions of “usual care” in most included studies, and there were also obvious differences in the methods of DSME in different studies. Despite the obvious differences in the diabetes care provided for those patients involved in different trials, it’s no doubt that patients allocated to DSME groups received more diabetes education than those in control groups. Secondly, primary instructors in most included studies were multidisciplinary team or nurses. This non-significant finding in the subgroup analysis of studies involving other diabetes educators, such as community health workers and pharmacists, didn’t imply that interventions led by those educators were ineffective. It may arise from the limited number of included trials involving community health workers or pharmacists. Thirdly, the finding in the meta-analysis may not be generalized to all type 2 diabetes patients. The eligibility criteria for recruiting type 2 diabetes patients were different among those included studies, and there were obvious differences in the background of type 2 diabetes patients among those included in trials. Though we performed subgroup analysis by newly-diagnosed diabetes or previously treated diabetes, we were unable to performed further subgroup analyses by more characteristics in details, such as diabetes duration, diabetic complications, education levels, and socioeconomic status. The effect of DSME on risk of mortality in type 2 diabetes patients with specific secondary diseases is also interesting, but few relevant studies are available now. More studies are needed to further assess the effect of DSME in mortality risk in type 2 diabetes patients with different disease duration, diabetic complications, comorbidities, glycemic control status, education levels, and socioeconomic status, and find who will benefit more from DSME and who should receive it. Fourthly, the cost-effectiveness of DSME in type 2 diabetes patients has not been well evaluated, and future studies are also needed to determine the most effective and cost-effective model of DSME. Finally, our meta-analysis only assessed the impact of DSME on mortality risk, but the impact of DSME on risks of cardiovascular mortality, cardiovascular diseases, infectious diseases and diabetic complications is still unclear. The impact of DSME on life quality in type 2 diabetes patients also has not been well studied. More clinical trials with a large number of recruited patients and longer time of follow-up are needed to solve these unanswered questions.
In conclusion, the available evidence suggests that DSME can reduce risk of all-cause mortality in type 2 diabetes patients. Further clinical trials with outcomes of longer time of follow-up are needed to validate the finding above and to determine the most cost-effective format of DSME in type 2 diabetes patients. Such clinical trials will provide clinicians with a stronger evidence for the clinical practice of DSME in type 2 diabetes patients.
References
P.Z. Zimmet, D.J. Magliano, W.H. Herman, J.E. Shaw, Diabetes: a 21st century challenge. Lancet Diabetes Endocrinol. 2(1), 56–64 (2014). doi:10.1016/S2213-8587(13)70112-8
L.S. Geiss, J. Wang, Y.J. Cheng, T.J. Thompson, L. Barker, Y. Li, A.L. Albright, E.W. Gregg, Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980-2012. JAMA. 312(12), 1218–1226 (2014). doi:10.1001/jama.2014.11494
A. Menke, S. Casagrande, L. Geiss, C.C. Cowie, Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 314(10), 1021–1029 (2015). doi:10.1001/jama.2015.10029
D.M. Nathan, Diabetes: advances in diagnosis and treatment. JAMA. 314(10), 1052–1062 (2015). doi:10.1001/jama.2015.9536
A. Dinesh Shah, C. Langenberg, E. Rapsomaniki, S. Denaxas, M. Pujades-Rodriguez, C.P. Gale, J. Deanfield, L. Smeeth, A. Timmis, H. Hemingway, Type 2 diabetes and incidence of a wide range of cardiovascular diseases: a cohort study in 1.9 million people. Lancet. 385(Suppl 1), S86 (2015). doi:10.1016/S0140-6736(15)60401-9
S.E. Kahn, M.E. Cooper, S. Del Prato, Pathophysiology and treatment of type 2 diabetes: perspectives on the past, present, and future. Lancet. 383(9922), 1068–1083 (2014). doi:10.1016/S0140-6736(13)62154-6
M. Tancredi, A. Rosengren, A.M. Svensson, M. Kosiborod, A. Pivodic, S. Gudbjornsdottir, H. Wedel, M. Clements, S. Dahlqvist, M. Lind, Excess mortality among persons with type 2 diabetes. N. Engl. J. Med. 373(18), 1720–1732 (2015). doi:10.1056/NEJMoa1504347
J.R. Brownrigg, C.O. Hughes, D. Burleigh, A. Karthikesalingam, B.O. Patterson, P.J. Holt, M.M. Thompson, S. de Lusignan, K.K. Ray, R.J. Hinchliffe, Microvascular disease and risk of cardiovascular events among individuals with type 2 diabetes: a population-level cohort study. Lancet Diabetes Endocrinol. 4(7), 588–597 (2016). doi:10.1016/S2213-8587(16)30057-2
S.H. Ley, O. Hamdy, V. Mohan, F.B. Hu, Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 383(9933), 1999–2007 (2014). doi:10.1016/S0140-6736(14)60613-9
A.A. Tahrani, C.J. Bailey, S. Del Prato, A.H. Barnett, Management of type 2 diabetes: new and future developments in treatment. Lancet. 378(9786), 182–197 (2011). doi:10.1016/S0140-6736(11)60207-9
A.D. Association, 3. Foundations of care and comprehensive medical evaluation. Diabetes Care 39(Suppl 1), S23–S35 (2016). doi:10.2337/dc16-S006
L. Haas, M. Maryniuk, J. Beck, C.E. Cox, P. Duker, L. Edwards, E.B. Fisher, L. Hanson, D. Kent, L. Kolb, S. McLaughlin, E. Orzeck, J.D. Piette, A.S. Rhinehart, R. Rothman, S. Sklaroff, D. Tomky, G. Youssef, National standards for diabetes self-management education and support. Diabetes. Care. 37(Suppl 1), S144–S153 (2014). doi:10.2337/dc14-S144
M.A. Powers, J. Bardsley, M. Cypress, P. Duker, M.M. Funnell, A. Hess Fischl, M.D. Maryniuk, L. Siminerio, E. Vivian, Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American diabetes association, the American association of diabetes educators, and the academy of nutrition and dietetics. Diabetes Care 38(7), 1372–1382 (2015). doi:10.2337/dc15-0730
G. Welch, J. Garb, S. Zagarins, I. Lendel, R.A. Gabbay, Nurse diabetes case management interventions and blood glucose control: results of a meta-analysis. Diabetes Res. Clin. Pract. 88(1), 1–6 (2010). doi:10.1016/j.diabres.2009.12.026
S.L. Norris, J. Lau, S.J. Smith, C.H. Schmid, M.M. Engelgau, Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 25(7), 1159–1171 (2002)
J. Pillay, M.J. Armstrong, S. Butalia, L.E. Donovan, R.J. Sigal, B. Vandermeer, P. Chordiya, S. Dhakal, L. Hartling, M. Nuspl, R. Featherstone, D.M. Dryden, Behavioral programs for type 2 diabetes mellitus: a systematic review and network meta-analysis. Ann Intern Med 163(11), 848–860 (2015). doi:10.7326/M15-1400
D. Sherifali, J.W. Bai, M. Kenny, R. Warren, M.U. Ali, Diabetes self-management programmes in older adults: a systematic review and meta-analysis. Diabetes Med 32(11), 1404–1414 (2015). doi:10.1111/dme.12780
C.A. Chrvala, D. Sherr, R.D. Lipman, Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient. Educ. Couns. 99(6), 926–943 (2016). doi:10.1016/j.pec.2015.11.003
T. Deakin, C.E. McShane, J.E. Cade, R.D. Williams, Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 2, CD003417 (2005). doi:10.1002/14651858.CD003417.pub2
A. Coppola, L. Sasso, A. Bagnasco, A. Giustina, C. Gazzaruso, The role of patient education in the prevention and management of type 2 diabetes: an overview. Endocrine. 53(1), 18–27 (2016). doi:10.1007/s12020-015-0775-7
D. Moher, A. Liberati, J. Tetzlaff, D.G. Altman, Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 151(4), 264–269 (2009). W264
C. Gazzaruso, M. Fodaro, A. Coppola, Structured therapeutic education in diabetes: is it time to re-write the chapter on the prevention of diabetic complications? Endocrine 53(2), 347–349 (2016). doi:10.1007/s12020-016-0947-0
X. Zhang, S. Yang, K. Sun, E.B. Fisher, X. Sun, How to achieve better effect of peer support among adults with type 2 diabetes: a meta-analysis of randomized clinical trials. Patient Educ. Couns. 99(2), 186–197 (2016). doi:10.1016/j.pec.2015.09.006
X.L. Huang, J.H. Pan, D. Chen, J. Chen, F. Chen, T.T. Hu, Efficacy of lifestyle interventions in patients with type 2 diabetes: a systematic review and meta-analysis. Eur. J. Intern. Med. 27, 37–47 (2016). doi:10.1016/j.ejim.2015.11.016
W. Palmas, D. March, S. Darakjy, S.E. Findley, J. Teresi, O. Carrasquillo, J.A. Luchsinger, Community health worker interventions to improve glycemic control in people with diabetes: a systematic review and meta-analysis. J. Gen. Intern. Med. 30(7), 1004–1012 (2015). doi:10.1007/s11606-015-3247-0
M. Attridge, J. Creamer, M. Ramsden, R. Cannings-John, K. Hawthorne, Culturally appropriate health education for people in ethnic minority groups with type 2 diabetes mellitus. Cochrane Database Syst. Rev. 9, CD006424 (2014). doi:10.1002/14651858.CD006424.pub3
E.S. Schellenberg, D.M. Dryden, B. Vandermeer, C. Ha, C. Korownyk, Lifestyle interventions for patients with and at risk for type 2 diabetes: a systematic review and meta-analysis. Ann. Intern. Med. 159(8), 543–551 (2013). doi:10.7326/0003-4819-159-8-201310150-00007
J.K. Tshiananga, S. Kocher, C. Weber, K. Erny-Albrecht, K. Berndt, K. Neeser, The effect of nurse-led diabetes self-management education on glycosylated hemoglobin and cardiovascular risk factors: a meta-analysis. Diabetes Educ. 38(1), 108–123 (2012). doi:10.1177/0145721711423978
A. Steinsbekk, L.O. Rygg, M. Lisulo, M.B. Rise, A. Fretheim, Group based diabetes self-management education compared to routine treatment for people with type 2 diabetes mellitus. A systematic review with meta-analysis. BMC Health Serv. Res. 12, 213 (2012). doi:10.1186/1472-6963-12-213
S.E. Ellis, T. Speroff, R.S. Dittus, A. Brown, J.W. Pichert, T.A. Elasy, Diabetes patient education: a meta-analysis and meta-regression. Patient Educ. Couns. 52(1), 97–105 (2004)
T.L. Gary, J.M. Genkinger, E. Guallar, M. Peyrot, F.L. Brancati, Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educ. 29(3), 488–501 (2003)
J.P. Higgins, D.G. Altman, P.C. Gotzsche, P. Juni, D. Moher, A.D. Oxman, J. Savovic, K.F. Schulz, L. Weeks, J.A. Sterne, The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 343, d5928 (2011). doi:10.1136/bmj.d5928
J.P. Higgins, S.G. Thompson, J.J. Deeks, D.G. Altman, Measuring inconsistency in meta-analyses. BMJ. 327(7414), 557–560 (2003). doi:10.1136/bmj.327.7414.557
W.G. Cochran, The combination of estimates from different experiments. Biometrics. 10(1), 101–129 (1954)
R. DerSimonian, N. Laird, Meta-analysis in clinical trials. Control Clin. Trials 7(3), 177–188 (1986)
N. Mantel, W. Haenszel, Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 22(4), 719–748 (1959)
J.P. Higgins, S. Green (ed.), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration (2011). Available from www.handbook.cochrane.org
C.B. Begg, M. Mazumdar, Operating characteristics of a rank correlation test for publication bias. Biometrics. 50(4), 1088–1101 (1994)
M. Egger, G. Davey Smith, M. Schneider, C. Minder, Bias in meta-analysis detected by a simple, graphical test. BMJ. 315(7109), 629–634 (1997)
G.H. Guyatt, A.D. Oxman, G.E. Vist, R. Kunz, Y. Falck-Ytter, P. Alonso-Coello, H.J. Schunemann, GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 336(7650), 924–926 (2008). doi:10.1136/bmj.39489.470347.AD
W. Crasto, J. Jarvis, K. Khunti, T.C. Skinner, L.J. Gray, J. Brela, J. Troughton, H. Daly, I.G. Lawrence, P.G. McNally, M.E. Carey, M.J. Davies, Multifactorial intervention in individuals with type 2 diabetes and microalbuminuria: the microalbuminuria education and medication optimisation (MEMO) study. Diabetes Res. Clin. Pract. 93(3), 328–336 (2011). doi:10.1016/j.diabres.2011.05.008
M. Hanefeld, S. Fischer, H. Schmechel, G. Rothe, J. Schulze, H. Dude, U. Schwanebeck, U. Julius, Diabetes intervention study. Multi-intervention trial in newly diagnosed NIDDM. Diabetes Care. 14(4), 308–317 (1991)
I. Odnoletkova, G. Goderis, F. Nobels, S. Fieuws, B. Aertgeerts, L. Annemans, D. Ramaekers, Optimizing diabetes control in people with type 2 diabetes through nurse-led telecoaching. Diabetes Med. 33(6), 777–785 (2016). doi:10.1111/dme.13092
T. Johansson, S. Keller, H. Winkler, T. Ostermann, R. Weitgasser, A.C. Sonnichsen, Effectiveness of a peer support programme versus usual care in disease management of diabetes mellitus type 2 regarding improvement of metabolic control: A cluster-randomised controlled trial. J. Diabetes Res. 2016, 3248547 (2016). doi:10.1155/2016/3248547
M.K. Ali, K. Singh, D. Kondal, R. Devarajan, S.A. Patel, R. Shivashankar, V.S. Ajay, A.G. Unnikrishnan, V.U. Menon, P.K. Varthakavi, V. Viswanathan, M. Dharmalingam, G. Bantwal, R.K. Sahay, M.Q. Masood, R. Khadgawat, A. Desai, B. Sethi, D. Prabhakaran, K.M. Narayan, N. Tandon, Effectiveness of a multicomponent quality improvement strategy to improve achievement of diabetes care goals: a randomized, controlled trial. Ann. Intern. Med. (2016). doi:10.7326/M15-2807
R. Perez-Escamilla, G. Damio, J. Chhabra, M.L. Fernandez, S. Segura-Perez, S. Vega-Lopez, G. Kollannor-Samuel, M. Calle, F.M. Shebl, D. D’Agostino, Impact of a community health workers-led structured program on blood glucose control among latinos with type 2 diabetes: the DIALBEST trial. Diabetes Care. 38(2), 197–205 (2015). doi:10.2337/dc14-0327
P. McGowan, The relative effectiveness of self-management programs for type 2 diabetes. Can. J. Diabetes 39(5), 411–419 (2015). doi:10.1016/j.jcjd.2015.04.005
D. Edelman, R.J. Dolor, C.J. Coffman, K.C. Pereira, B.B. Granger, J.H. Lindquist, A.M. Neary, A.J. Harris, H.B. Bosworth, Nurse-led behavioral management of diabetes and hypertension in community practices: a randomized trial. J. Gen. Intern. Med. 30(5), 626–633 (2015). doi:10.1007/s11606-014-3154-9
S. Hamid, S. Dunsiger, A. Seiden, O. Nu’usolia, J. Tuitele, J.D. DePue, S.T. McGarvey, Impact of a diabetes control and management intervention on health care utilization in American Samoa. Chronic. Illn. 10(2), 122–134 (2014). doi:10.1177/1742395313502367
E.G. Eakin, E.A. Winkler, D.W. Dunstan, G.N. Healy, N. Owen, A.M. Marshall, N. Graves, M.M. Reeves, Living well with diabetes: 24-month outcomes from a randomized trial of telephone-delivered weight loss and physical activity intervention to improve glycemic control. Diabetes Care 37(8), 2177–2185 (2014). doi:10.2337/dc13-2427
L.M. Welschen, P. van Oppen, S.D. Bot, P.J. Kostense, J.M. Dekker, G. Nijpels, Effects of a cognitive behavioural treatment in patients with type 2 diabetes when added to managed care; a randomised controlled trial. J. Behav. Med. 36(6), 556–566 (2013). doi:10.1007/s10865-012-9451-z
J. Sperl-Hillen, S. Beaton, O. Fernandes, A. Von Worley, G. Vazquez-Benitez, A. Hanson, J. Lavin-Tompkins, W. Parsons, K. Adams, C.V. Spain, Are benefits from diabetes self-management education sustained? Am. J. Manag. Care. 19(2), 104–112 (2013)
U. Mons, E. Raum, H.U. Kramer, G. Ruter, D. Rothenbacher, T. Rosemann, J. Szecsenyi, H. Brenner, Effectiveness of a supportive telephone counseling intervention in type 2 diabetes patients: randomized controlled study. PLoS ONE. 8(10), e77954 (2013). doi:10.1371/journal.pone.0077954
J.J. Gagliardino, S. Lapertosa, G. Pfirter, M. Villagra, J.E. Caporale, C.D. Gonzalez, J. Elgart, L. Gonzalez, C. Cernadas, E. Rucci, C. Clark Jr., Clinical, metabolic and psychological outcomes and treatment costs of a prospective randomized trial based on different educational strategies to improve diabetes care (PRODIACOR). Diabetes Med. 30(9), 1102–1111 (2013). doi:10.1111/dme.12230
M.J. Crowley, B.J. Powers, M.K. Olsen, J.M. Grubber, C. Koropchak, C.M. Rose, P. Gentry, L. Bowlby, G. Trujillo, M.L. Maciejewski, H.B. Bosworth, The cholesterol, hypertension, and glucose education (CHANGE) study: results from a randomized controlled trial in African Americans with diabetes. Am. Heart J. 166(1), 179–186 (2013). doi:10.1016/j.ahj.2013.04.004
I.D. Blackberry, J.S. Furler, J.D. Best, P. Chondros, M. Vale, C. Walker, T. Dunning, L. Segal, J. Dunbar, R. Audehm, D. Liew, D. Young, Effectiveness of general practice based, practice nurse led telephone coaching on glycaemic control of type 2 diabetes: the patient engagement and coaching for health (PEACH) pragmatic cluster randomised controlled trial. BMJ. 347, f5272 (2013). doi:10.1136/bmj.f5272
L.O. Rygg, M.B. Rise, K. Gronning, A. Steinsbekk, Efficacy of ongoing group based diabetes self-management education for patients with type 2 diabetes mellitus. A randomised controlled trial. Patient Educ. Couns. 86(1), 98–105 (2012). doi:10.1016/j.pec.2011.04.008
K. Khunti, L.J. Gray, T. Skinner, M.E. Carey, K. Realf, H. Dallosso, H. Fisher, M. Campbell, S. Heller, M.J. Davies, Effectiveness of a diabetes education and self management programme (DESMOND) for people with newly diagnosed type 2 diabetes mellitus: three year follow-up of a cluster randomised controlled trial in primary care. BMJ. 344, e2333 (2012). doi:10.1136/bmj.e2333
B.J. Wakefield, J.E. Holman, A. Ray, M. Scherubel, M.R. Adams, S.L. Hillis, G.E. Rosenthal, Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed. J. E-Health. 17(4), 254–261 (2011). doi:10.1089/tmj.2010.0176
R.C. Andrews, A.R. Cooper, A.A. Montgomery, A.J. Norcross, T.J. Peters, D.J. Sharp, N. Jackson, K. Fitzsimons, J. Bright, K. Coulman, C.Y. England, J. Gorton, A. McLenaghan, E. Paxton, A. Polet, C. Thompson, C.M. Dayan, Diet or diet plus physical activity versus usual care in patients with newly diagnosed type 2 diabetes: the Early ACTID randomised controlled trial. Lancet. 378(9786), 129–139 (2011). doi:10.1016/S0140-6736(11)60442-X
G.A. Piatt, R.M. Anderson, M.M. Brooks, T. Songer, L.M. Siminerio, M.M. Korytkowski, J.C. Zgibor, 3-year follow-up of clinical and behavioral improvements following a multifaceted diabetes care intervention: results of a randomized controlled trial. Diabetes Educ. 36(2), 301–309 (2010). doi:10.1177/0145721710361388
D. Edelman, S.K. Fredrickson, S.D. Melnyk, C.J. Coffman, A.S. Jeffreys, S. Datta, G.L. Jackson, A.C. Harris, N.S. Hamilton, H. Stewart, J. Stein, M. Weinberger, Medical clinics versus usual care for patients with both diabetes and hypertension: a randomized trial. Ann. Intern. Med. 152(11), 689–696 (2010). doi:10.7326/0003-4819-152-11-201006010-00001
B.J. Thoolen, D. de Ridder, J. Bensing, K. Gorter, G. Rutten, Beyond good intentions: the role of proactive coping in achieving sustained behavioural change in the context of diabetes management. Psychol. Health 24(3), 237–254 (2009). doi:10.1080/08870440701864504
H. Cooper, K. Booth, G. Gill, A trial of empowerment-based education in type 2 diabetes--global rather than glycaemic benefits. Diabetes Res. Clin. Pract. 82(2), 165–171 (2008). doi:10.1016/j.diabres.2008.07.013
B. Thoolen, D. De Ridder, J. Bensing, C. Maas, S. Griffin, K. Gorter, G. Rutten, Effectiveness of a self-management intervention in patients with screen-detected type 2 diabetes. Diabetes Care 30(11), 2832–2837 (2007). doi:10.2337/dc07-0777
T. Shibayama, K. Kobayashi, A. Takano, T. Kadowaki, K. Kazuma, Effectiveness of lifestyle counseling by certified expert nurse of Japan for non-insulin-treated diabetic outpatients: a 1-year randomized controlled trial. Diabetes Res. Clin. Pract. 76(2), 265–268 (2007). doi:10.1016/j.diabres.2006.09.017
E.T. Adolfsson, M.L. Walker-Engstrom, B. Smide, K. Wikblad, Patient education in type 2 diabetes: a randomized controlled 1-year follow-up study. Diabetes Res. Clin. Pract. 76(3), 341–350 (2007). doi:10.1016/j.diabres.2006.09.018
J.A. Fornos, N.F. Andres, J.C. Andres, M.M. Guerra, B. Egea, A pharmacotherapy follow-up program in patients with type-2 diabetes in community pharmacies in Spain. Pharm. World Sci. 28(2), 65–72 (2006). doi:10.1007/s11096-006-9003-0
R.L. Rothman, R. Malone, B. Bryant, A.K. Shintani, B. Crigler, D.A. Dewalt, R.S. Dittus, M. Weinberger, M.P. Pignone, A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. Am. J. Med. 118(3), 276–284 (2005). doi:10.1016/j.amjmed.2004.09.017
A. Sarkadi, U. Rosenqvist, Experience-based group education in Type 2 diabetes: a randomised controlled trial. Patient Educ. Couns. 53(3), 291–298 (2004). doi:10.1016/j.pec.2003.10.009
S.L. Krein, M.L. Klamerus, S. Vijan, J.L. Lee, J.T. Fitzgerald, A. Pawlow, P. Reeves, R.A. Hayward, Case management for patients with poorly controlled diabetes: a randomized trial. Am. J. Med. 116(11), 732–739 (2004). doi:10.1016/j.amjmed.2003.11.028
A.N. Goudswaard, R.P. Stolk, N.P. Zuithoff, H.W. de Valk, G.E. Rutten, Long-term effects of self-management education for patients with Type 2 diabetes taking maximal oral hypoglycaemic therapy: a randomized trial in primary care. Diabetes Med. 21(5), 491–496 (2004). doi:10.1111/j.1464-5491.2004.01153.x
M. Clark, S.E. Hampson, L. Avery, R. Simpson, Effects of a tailored lifestyle self-management intervention in patients with type 2 diabetes. Br. J. Health Psychol. 9(Pt 3), 365–379 (2004). doi:10.1348/1359107041557066
C.B. Taylor, N.H. Miller, K.R. Reilly, G. Greenwald, D. Cunning, A. Deeter, L. Abascal, Evaluation of a nurse-care management system to improve outcomes in patients with complicated diabetes. Diabetes Care 26(4), 1058–1063 (2003)
J.P. New, J.M. Mason, N. Freemantle, S. Teasdale, L.M. Wong, N.J. Bruce, J.A. Burns, J.M. Gibson, Specialist nurse-led intervention to treat and control hypertension and hyperlipidemia in diabetes (SPLINT): a randomized controlled trial. Diabetes Care 26(8), 2250–2255 (2003)
T.L. Gary, L.R. Bone, M.N. Hill, D.M. Levine, M. McGuire, C. Saudek, F.L. Brancati, Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev. Med. 37(1), 23–32 (2003)
J.D. Piette, M. Weinberger, F.B. Kraemer, S.J. McPhee, Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a Department of Veterans Affairs Health Care System: a randomized controlled trial. Diabetes Care 24(2), 202–208 (2001)
Y. Groeneveld, H. Petri, J. Hermans, M. Springer, An assessment of structured care assistance in the management of patients with type 2 diabetes in general practice. Scand. J. Prim. Health Care 19(1), 25–30 (2001)
J.D. Piette, M. Weinberger, S.J. McPhee, C.A. Mah, F.B. Kraemer, L.M. Crapo, Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am. J. Med. 108(1), 20–27 (2000)
M. Weinberger, M.S. Kirkman, G.P. Samsa, E.A. Shortliffe, P.B. Landsman, P.A. Cowper, D.L. Simel, J.R. Feussner, A nurse-coordinated intervention for primary care patients with non-insulin-dependent diabetes mellitus: impact on glycemic control and health-related quality of life. J. Gen. Intern. Med. 10(2), 59–66 (1995)
S.R. Heller, P. Clarke, H. Daly, I. Davis, D.K. McCulloch, S.P. Allison, R.B. Tattersall, Group education for obese patients with type 2 diabetes: greater success at less cost. Diabetes Med. 5(6), 552–556 (1988)
Z.T. Bloomgarden, W. Karmally, M.J. Metzger, M. Brothers, C. Nechemias, J. Bookman, D. Faierman, F. Ginsberg-Fellner, E. Rayfield, W.V. Brown, Randomized, controlled trial of diabetic patient education: improved knowledge without improved metabolic status. Diabetes Care. 10(3), 263–272 (1987)
R. Li, S.S. Shrestha, R. Lipman, N.R. Burrows, L.E. Kolb, S. Rutledge, Diabetes self-management education and training among privately insured persons with newly diagnosed diabetes--United States, 2011-2012. MMWR Morb. Mortal. Wkly. Rep. 63(46), 1045–1049 (2014)
M. Peyrot, K.K. Burns, M. Davies, A. Forbes, N. Hermanns, R. Holt, S. Kalra, A. Nicolucci, F. Pouwer, J. Wens, I. Willaing, S.E. Skovlund, Diabetes attitudes wishes and needs 2 (DAWN2): a multinational, multi-stakeholder study of psychosocial issues in diabetes and person-centred diabetes care. Diabetes Res. Clin. Pract. 99(2), 174–184 (2013). doi:10.1016/j.diabres.2012.11.016
M.E. Chomko, P.S. Odegard, A.B. Evert, Enhancing access to diabetes self-management education in primary care. Diabetes Educ. (2016). doi:10.1177/0145721716659147
A.C. Tricco, N.M. Ivers, J.M. Grimshaw, D. Moher, L. Turner, J. Galipeau, I. Halperin, B. Vachon, T. Ramsay, B. Manns, M. Tonelli, K. Shojania, Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. Lancet. 379(9833), 2252–2261 (2012). doi:10.1016/S0140-6736(12)60480-2
C.K. Wong, W.C. Wong, Y.F. Wan, A.K. Chan, K.L. Chung, F.W. Chan, C.L. Lam, Patient empowerment programme in primary care reduced all-cause mortality and cardiovascular diseases in patients with type 2 diabetes mellitus: a population-based propensity-matched cohort study. Diabetes Obes. Metab. 17(2), 128–135 (2015). doi:10.1111/dom.12397
E. Kornelius, J.Y. Chiou, Y.S. Yang, Y.L. Lu, C.H. Peng, C.N. Huang, The diabetes shared care program and risks of cardiovascular events in type 2 diabetes. Am. J. Med. 128(9), 977–985 e973 (2015). doi:10.1016/j.amjmed.2015.03.025
B.R. Shah, J. Hwee, K. Cauch-Dudek, R. Ng, J.C. Victor, Diabetes self-management education is not associated with a reduction in long-term diabetes complications: an effectiveness study in an elderly population. J. Eval. Clin. Pract. 21(4), 656–661 (2015). doi:10.1111/jep.12360
G. Perman, A. Beratarrechea, V. Aliperti, L. Litwak, S. Figar, A. Alvarez, E. Langlois, Mortality in an elderly type 2 diabetic patients’ cohort who attended a self-management educational workshop. Prim. Care Diabetes. 5(3), 175–184 (2011). doi:10.1016/j.pcd.2011.03.002
L. Blonde, J. Dempster, J.M. Gallivan, E. Warren-Boulton, Reducing cardiovascular disease risk in patients with diabetes: a message from the national diabetes education program. J. Am. Acad. Nurse Pract. 18(11), 524–533 (2006). doi:10.1111/j.1745-7599.2006.00171.x
C.K. Wong, W.C. Wong, E.Y. Wan, A.K. Chan, F.W. Chan, C.L. Lam, Macrovascular and microvascular disease in obese patients with type 2 diabetes attending structured diabetes education program: a population-based propensity-matched cohort analysis of patient empowerment programme (PEP). Endocrine 53(2), 412–422 (2016). doi:10.1007/s12020-015-0843-z
H.M. Hsieh, T.H. Lin, I.C. Lee, C.J. Huang, S.J. Shin, H.C. Chiu, The association between participation in a pay-for-performance program and macrovascular complications in patients with type 2 diabetes in Taiwan: a nationwide population-based cohort study. Prev. Med. 85, 53–59 (2016). doi:10.1016/j.ypmed.2015.12.013
E. Monninkhof, P. van der Valk, J. van der Palen, C. van Herwaarden, M.R. Partridge, G. Zielhuis, Self-management education for patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 58(5), 394–398 (2003)
J.M. Coffman, M.D. Cabana, H.A. Halpin, E.H. Yelin, Effects of asthma education on children’s use of acute care services: a meta-analysis. Pediatrics. 121(3), 575–586 (2008). doi:10.1542/peds.2007-0113
A. Warsi, P.S. Wang, M.P. LaValley, J. Avorn, D.H. Solomon, Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch. Intern. Med. 164(15), 1641–1649 (2004). doi:10.1001/archinte.164.15.1641
J.P. Brown, A.M. Clark, H. Dalal, K. Welch, R.S. Taylor, Patient education in the management of coronary heart disease. Cochrane Database Syst. Rev. 12, CD008895 (2011). doi:10.1002/14651858.CD008895.pub2
H.A. Shah, M. Abu-Amara, Education provides significant benefits to patients with hepatitis B virus or hepatitis C virus infection: a systematic review. Clin. Gastroenterol. Hepatol. 11(8), 922–933 (2013). doi:10.1016/j.cgh.2013.04.024
N.H. Jonkman, H. Westland, R.H. Groenwold, S. Agren, F. Atienza, L. Blue, P.W. Bruggink-Andre de la Porte, D.A. DeWalt, P.L. Hebert, M. Heisler, T. Jaarsma, G.I. Kempen, M.E. Leventhal, D.J. Lok, J. Martensson, J. Muniz, H. Otsu, F. Peters-Klimm, M.W. Rich, B. Riegel, A. Stromberg, R.T. Tsuyuki, D.J. van Veldhuisen, J.C. Trappenburg, M.J. Schuurmans, A.W. Hoes, Do self-management interventions work in patients with heart failure? An individual patient data meta-analysis. Circulation. 133(12), 1189–1198 (2016). doi:10.1161/CIRCULATIONAHA.115.018006
K. Ismail, K. Winkley, S. Rabe-Hesketh, Systematic review and meta-analysis of randomised controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 363(9421), 1589–1597 (2004). doi:10.1016/S0140-6736(04)16202-8
Acknowledgment
We thank Prof. Zhang from Huadong Hospital of Fudan University for her helpful advice on our study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
He, X., Li, J., Wang, B. et al. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine 55, 712–731 (2017). https://doi.org/10.1007/s12020-016-1168-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1168-2