Abstract
The purpose of this study is to evaluate the distribution of thyrotropin (TSH) values in patients with autonomously functioning thyroid nodules and to set a TSH threshold above which thyroid scintigraphy would be obviated. Four hundred fifty one patients were included in the present study. Inclusion criteria were age > 18 years, TSH levels between 0.40 and 4.0 mIU/L, detection of a single solid or predominantly solid thyroid nodule >10 mm in the longest diameter. Thyroid ultrasound and thyroid scintigraphy with 99mTc-pertechnetate were performed concurrently in all patients. Among 451 enrolled patients, 173 (38 %) had an autonomously functioning thyroid nodules, of which 137 (79 %) with a normal TSH level. Demographic data and nodules’ volume were not significantly different in patients with autonomously functioning thyroid nodules and non-functioning nodules, respectively. However, TSH levels were nonetheless significantly lower in patients with autonomously functioning thyroid nodules compared to those with non-functioning nodules (p < 0.001). Adopting a TSH cutoff level at 2.38 mUI/L, all autonomously functioning thyroid nodules were correctly identified (i.e., 100 % sensitivity) with a 100 % negative predictive value. Our study showed a very high prevalence of autonomously functioning thyroid nodules in mildly iodine-deficient regions and confirmed that serum TSH is not an effective screening test to diagnose an autonomously functioning thyroid nodules. Our data add arguments in favor of the first-line use of thyroid scintigraphy to assess thyroid nodules, at least in iodine deficient areas. As all scintigraphically detected autonomously functioning thyroid nodules had a TSH level below 2.38 mUI/L, a thyroid scintigraphy should be omitted when higher TSH values are found in patients carrying a thyroid nodule.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Thyroid scintigraphy (ThyS) with either 99mTc-pertechnetate or 123I-natrium iodide is the only available tool to detect autonomously functioning thyroid nodules (AFTNs) [1]. In turn, AFTNs can be classified as benign with a very high accuracy rate [2]. Therefore, current clinical guidelines suggest refraining from fine needle aspiration cytology (FNA) of an AFTN [3]. In recent years, however, the use of ThyS in the management of thyroid nodules has been reduced due to the assumption that ThyS would only be useful in patients with a lowered or suppressed thyrotropin (TSH) level [4]. In contrast, the relationship between thyroid autonomy and TSH levels has not been established as there is a considerable influence of the degree of iodine sufficiency, which varies widely between different countries and regions. In geographic areas that formerly had or still show iodine deficiency, TSH may remain normal even if an AFTN is present because the low synthesis rate of thyroid hormones cannot suppress the TSH secretion, especially early in the disease [5, 6]. Furthermore, literature has shown that within 10 years more than 70 % of non-toxic AFTN will convert to causing hyperthyroidism [7]. Considerably, AFTNs are rarely if ever malignant and a large number of unnecessary FNA procedures, with associated rates of false positive or unclear findings necessitating surgery for histological analysis of the lesion, could be spared if patients with AFTNs are not subjected to FNA. The prevalence of AFTNs with normal TSH is about 50 %[5, 6, 8, 9] with higher rates reported in Europe where, although in several countries iodine prophylaxis programs are already operating, mild to moderate iodine deficiency still persist in many regions including Southern Switzerland and Sicily (Italy) [10–13]. Accordingly, in our centers ThyS is used on a routine basis, independently from TSH levels, to assess thyroid nodules. In this context, however, it is unclear if ThyS is necessary across all normal TSH values; then we undertook the present study (1) to evaluate the distribution of TSH values among patients with an AFTN and a TSH level within the normal reference range and (2) to set, if possible, a TSH threshold above which ThyS could be obviated.
Material and methods
Patients
Between 1 January 2014 and 1 May 2016 904 consecutive outpatients (213 males, 691 females, age 35.8 (18–84) years) affected by nodular goiter were referred to Bellinzona (n = 560) and Messina (n = 344) nuclear medicine outpatients services, respectively. These patients were visited by a board certified nuclear medicine physician and first submitted to thyroid ultrasound (ThyUS) and TSH measurement. ThyS was not performed in pregnant females (n = 5) and those with a history of iodide contamination and treatment by drugs interfering with thyroid function (e.g., antithyroid drugs, thyroid hormones, amiodarone, lithium) (n = 54). Among the remaining patients included in the present study were those patients fulfilling the following criteria: age >18 years, TSH levels between <0.4 and 4.0 mIU/L, detection of a single solid or predominantly solid thyroid nodule >10 mm in the main diameter. Excluded were those patients with age <18 years, increased TSH level, a purely or predominantly cystic nodule and those with multiple nodules.
Laboratory
Thyrotropin (TSH) was measured with chemiluminescence immunoassays (HYPERsensitive hTSH) on a UniCelDxI 800 automated platform (Beckman Coulter SA, Nyon, Switzerland). The HYPERsensitive hTSH assay is based on the 3rd International Standard (WHO) for human TSH (IRP 81/565) with analytical sensitivity of 0.003 mIU/L, functional sensitivity of 0.01 mIU/l and a range of linearity from 0.01 to 100 mIU/L, respectively. The TSH normal reference range is 0.40 to 4.00 mIU/L.
Thyroid ultrasound (ThyUS)
All ultrasound examinations were performed using an Acuson®S3000 sonograph equipped with a small-parts multifrequency (5–13 MHz) probe (Siemens, Erlangen, Germany). The longest diameter of the nodules was measured and expressed in mm; the volume of the nodules was estimated according to the formula: height × width × depth × 0.524 and expressed in mL. Patients with predominantly cystic nodules (i.e., >50 % of the volume) were excluded from the study.
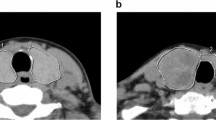
99mTc-pertechnetate ThyS
99mTc-pertechnetate scintigraphy was performed using a large-field-of-view γ-camera (Symbia-T2; Siemens, Erlangen, Germany) equipped with a ultra-high resolution parallel-hole low-energy collimator. Fifteen minutes after intravenous injection of 74 MBq of freshly eluted99mTc pertechnetate (Mallinkrodt, Petten, The Netherlands), a static image of the neck was acquired in the anterior view with a 128 × 128 matrix, using a digital zoom of 2 (pixel dimension, 2.4 mm). The acquisition time was set to 300 s with a 15 % window centered at 140 keV in all cases. Nodules were scored as hyperfunctioning (i.e., uptake of the nodule > normal thyroid tissue), isofunctioning (i.e., uptake of the nodule = normal thyroid tissue) or hypofunctioning (i.e., uptake of the nodule < normal thyroid tissue. The scintigraphic criteria for AFTNs was a solid nodule > 10 mm on ultrasound and hyperfunctioning on ThyS. Nodules with uptake ≤ normal thyroid tissue were classified as non-functioning ones (i.e., NFTNs).
Statistical evaluation
Statistical analysis was performed using GraphPad Prism, version 4.0 (GraphPad Prism Software, San Diego, CA, USA) and MedCalc Statistical Software version 16.4.3 (MedCalc Software, Ostend, Belgium). A p-value <0.05 was considered statistically significant. The normality of the distribution was assessed using the Shapiro–Wilk test for the results of TSH concentration and nodule diameter/volume. Since values were not normally distributed, data were reported as median and range (minimum-maximum). The degree of association between TSH concentrations and the nodule volume was assessed using Spearman’s rank correlation for non-normally distributed data. Mann–Whitney U-test was used to compare two samples of observations. The diagnostic performance of the TSH test to discriminate between AFTN and NFTN patients was evaluated using Receiver Operating Characteristic (ROC) curve analysis. Sensitivity/specificity pairs were graphically defined and determined by Youdens’s J index, respectively. Corresponding positive (+LR) and negative (−LR) likelihood ratios and positive (+PV) and negative (−PV) predictive values were also calculated.
Results
Among 845 patients who underwent ThyS, 394 patients (47 %) were excluded from the study due to age <18 years (19, 5 %), TSH levels exceeding 4 mUI/L (31, 8 %), purely or predominantly cystic nodules (69, 17 %) and multiple nodules (275, 70 %). Among 451(53 %) patients fulfilling inclusion criteria, 22(5 %) had symptomatic hyperthyroidism, 45(10 %) had incidentally detected reduced TSH and 384 (85 %) showed a clinically (95, 25 %) or incidentally (289, 75 %) detected thyroid nodule. The TSH level was subnormal (i.e., <0.40 mIU/L) in 45/451 (10 %) patients and between 0.40 and 4.00 mIU/L in the remaining 406/451 (90 %) patients. An AFTN was scintigraphically demonstrated in 36 of 45 (80 %) patients with reduced TSH and 137 of 406 (34 %) patients with normal TSH (Chi-square test, p < 0.0001). All in all, 173 of 451 (38 %) patients had a scintigraphically detected AFTN and 137 of them (79 %) had a normal TSH concentration. A weak relationship was found between TSH levels and AFTNs diameter (p 0.045) but not with the volume (Fig.1). Among patients with AFTNs, those with reduced TSH were older and had larger nodules than those with normal TSH levels (Table 1). Among patients with normal TSH and either AFTN or NFTN, neither demographic data nor nodules’ dimensions differed significantly. However, TSH levels were nonetheless significantly lower in patients with an AFTN compared to those with an NFTN (p < 0.001) (Table 2). The ROC curve analysis showed a good overall accuracy of TSH measurement [area under the ROC curve 0.804 (CI: 0.761–0.842)] (Fig.2). The best sensitivity/specificity pair was obtained by a cutoff of 1.49 mIU/L (i.e., sensitivity, specificity, +PV, −PV of 83 % (CI 76–89 %), 65 % (CI 59–70 %), 55 % and 88 %]. Furthermore, when positivity criterion was established farther right on the ROC curve to maximize –PV, a TSH threshold at 2.38 mIU/L correctly identified all AFTNs (i.e., sensitivity 100 %, specificity 21 % (CI 17–27 %), +PV 40 % and –PV 100 %). Finally, positive and negative LRs were 2.38/0.26 and 1.27/0 for a TSH threshold of 1.49 and 2.38 mUI/L, respectively.
Discussion
In our series of 451 patients carrying a thyroid nodule, 173 (38 %) had a scintigraphically detected AFTN challenging previous data reporting AFTNs in 5–10 % of thyroid nodules in dated reports [14,15]. The latters, however, were based on thyroid nodules’ detection by palpation while, combining high resolution ultrasound and systematic ThyS, we also detected non-palpable and non-toxic AFTNs. In all, our present epidemiological data further corroborate the systematic use of ThyS in patients with nodular goitre. Indeed, 137 of 173 (79 %) patients with an AFTN had a normal TSH concentration and demonstrated normal TSH values in our series, which is well in line with current literature [2, 5, 6, 8, 9]. In addition, 85 % of AFTNs were discovered during thyroid nodules work-up in our patients well conforming previous data reported by Chami et al. [8]. In fact, they found an increasing proportion of AFTNs with normal TSH in patients evaluated during a thyroid nodule work-up (71 %) compared to patients referred for any reason, including thyroid dysfunctions (49 %). A significant but weak inverse relationship was found between TSH levels and diameter of AFTNs but not volume. This apparent paradox is likely due to the wider variability in volume estimation by ellipsoid model (i.e., intra-observer variability 14.4 %, repeatability 84.8 %) than in diameter measurement (i.e., intra-observer variability 3.4 %, repeatability 96.5 %) [16]. Moreover, the wide dispersion of both AFTNs’ diameters and volumes around any TSH level strata precludes their role in predicting or excluding AFTNs in patients with normal TSH values. This is likely due to the heterogeneous cellular density from one nodule to another one, the difficulty of estimating the actual weight of the autonomous tissue within the nodule and the presence of an impaired iodide organification in AFTNs [8]. All in all, the diagnostic accuracy of TSH was likely unaffected by nodules’ dimensions. The best pair of sensitivity/specificity was found at a TSH cutoff of 1.49 mUI/L. Nevertheless, a threshold of 2.38 mIU/L correctly identified all AFTNs optimizing the −PV of TSH as yard-stick for ThyS. Our results are well in line with those obtained by Gorges et al. [5]; in fact, only 1.6 % of their 514 patients carrying an AFTN had TSH levels above 2.34 mUI/L.We used the traditional TSH reference range (0.4–4 mIU/L) to identify euthyroid patients. Interestingly, some authors support the reduction of the upper reference limit (URL) to 2.5 mIU/L in order to exclude patients with occult hypothyroidism while others suggest to increase the URL, especially in women and in old people [17]. Additionally, sex, age, race, body mass index, iodine intake were identified as independent factors influencing TSH reference intervals [18–20]. These factors unlikely affected our results as patients with either AFTNs or NFTNs showed similar demographic characteristics (Table 2). Briefly, the mean age was 54 and 51 years, respectively, with a good representation of all age classes and the proportion of females and males was comparable in AFTN and NFTN patients. Sometimes, however, a population-based reference range for TSH, even if well established, might fail to detect thyroid disfunctions at individual level, due to intra- and inter-individual variability [17].We attempted to limit such influences by excluding pregnant females [21] and hospitalized patients [22] and by standardizing the blood sample timing [23]. Indeed, we selected our cutoff in well-characterized patients using ThyS as benchmark [24]. As already demonstrated in patients with differentiated thyroid carcinoma, [25] a theranostic approach to radioiodine molecular imaging and therapy should be also usefully applied to patients with an AFTN. In fact, subjects with lower TSH still within the euthyroid range had an almost twofold increased risk of atrial fibrillation, compared with those in the highest quartile. Then, adopting an optimized TSH level as a yard-stick for ThyS may detect AFTNs requiring radioiodine ablation despite formally “normal” TSH values [26]. Finally, it should be noted that TSH results are not identical when different assay methods are employed and reference values may differ in different subject and patient populations [27]. As a consequence, caution is needed in translating our results when different assays are employed and different populations are evaluated. Clinicians and laboratory specialists are strongly advised to carefully evaluate the analytical and clinical performance of their TSH assay and to derive analytical cutoffs and clinical decision limits in their own patient populations.
Conclusions
Our present study confirms that serum TSH is not an effective screening test to diagnose an AFTN adding arguments in favor of the first-line use of ThyS in thyroid nodules assessment, at least in iodine deficient areas. Selecting patients with a thyroid nodule and a TSH level below 2.38 mUI/L allows a correct detection of an AFTN with a 100 % sensitivity while ThyS should be safely spared for higher TSH values with a 100 % −PV.
References
L. Giovanella, L. Ceriani, G. Treglia, Role of isotope scan, including positron emission tomography/computed tomography, in nodular goitre. Best. Pract. Res. Clin. Endocrinol. Metab. 28, 507–518 (2014)
H. Schicha, M. Hellmich, W. Lehmacher, W. Eschner, M. Schmidt, C. Kobe et al., Should all patients with thyroid nodules ≥ 1 cm undergo aspiration biopsy? Nuklearmedizin 48, 79–83 (2009)
B.R. Haugen, E.K. Alexander, K.C. Bible, J.M. Doherty, S.J. Mandel, Y.E. Nikiforov et al., 2015 American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 26, 1–133 (2016)
G. Popoveniuc, J. Jonklaas, Thyroid nodules. Med. Clin. North. Am. 96, 329–349 (2012)
R. Gorges, T. Kandror, S. Kuschnerus, M. Zimny, R. Pink, H. Palmedo et al., Scintigraphically “hot” thyroid nodules mainly go hand in hand with a normal TSH. Nuklearmedizin 50, 179–188 (2011)
D. Graf, B. Helmich-Kapp, S. Graf, F. Veit, N. Lehmann, K. Mann, Functional activity of autonomous adenoma in Germany. Dtsch. Med. Wochenschr. 137, 2089–2092 (2012)
D. Sandrock, T. Olbricht, D. Emrich, G. Benker, D. Reinwein, Longterm follow-up in patients with autonomous thyroid adenoma. Acta Endocrinol. 128, 51–55 (1993)
R. Chami, R. Moreno-Reyes, B. Corvilain, TSH measurement is not an appropriate screening test for autonomous functioning thyroid nodules: a retrospective study of 368 patients. Eur. J. Endocrinol. 170, 593–599 (2014)
G. Treglia, P. Trimboli, F.A. Verburg, M. Luster, L. Giovanella, Prevalence of normal TSH among patients with autonomously functioning thyroid nodules. Eur. J. Clin. Invest. 45, 739–744 (2015)
M. Olivieri, P. Vitti, Attività di monitoraggio del programma nazionale per la prevenzione dei disordini da carenza iodica. http://www.iss.it/binary/osna/cont/Rapporto_Istisan_2014.pdf (2014). Accessed 6 August 2016
M. Anderson, B. de Benoist, I. Darrnton-Hill, F. Delalonge, Iodine deficiency in Europe. A continuing public health problem. http://www.who.int/nutrition/publications/VMNIS_Iodine_deficiency_in_Europe.pdf (2007). Accessed 6 August 2016
M. Heinisch, G. Kumnig, D. Asböck, P. Mikosch, H.J. Gallowitsch, E. Kresnik et al., Goiter prevalence and iodine urinary excretion in a formerly iodine deficient region after introduction of statutory iodization of common salt. Thyroid 12, 809–814 (2002)
A.C. van de Ven, R.T. Netea-Maier, H.A. Ross, T.A. van Herwaarden, S. Holewijn, J. de Graaf et al., Longitudinal trends in thyroid function in relation to iodine intake: ongoing changes of thyroid function despite adequate current iodine status. Eur. J. Endocrinol. 170, 49–54 (2013)
J.I. Hamburger, The autonomously functioning thyroid nodule: Goetsch’s disease. Endocrine Reviews 8, 439–447 (1998)
L. Hegedus, S.J. Bonnema, F.N. Bennedbaek, Management of simple nodular goiter: current status and future perspectives. Endocr. Rev. 24, 102–132 (2003)
P. Andermann, S. Schlögl, U. Mäder, M. Luster, M. Lassmann, C. Reiners, Intra- and interobserver variability of thyroid volume measurements in healthy adults by 2D versus 3D ultrasound. Nuklearmedizin 46, 1–7 (2007)
P. Laurberg, S. Andersen, A. Carlé, J. Karmisholt, N. Knudsen, I.B. Pedersen, The TSH upper reference limit: where are we at? Nat. Rev. Endocrinol. 7, 232–239 (2011)
M.I. Surks, J.G. Hollowell, Age-specific distribution of serum thyrotropin and antithyroid antibobides in the US population: implications for the prevalence of subclinical hypothyroidism. J. Clin. Endocrinol. Metab. 92, 4575–4582 (2007)
B. Biondi, Thyroid and obesity: an intriguing relationship. J. Clin. Endocrinol. Metab. 95, 3614–3617 (2010)
J.G. Hollowell, N.W. Stehling, W.E. Flanders, Serum TSH, T4, and anthyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J. Clin. Endocrinol. Metab. 87, 489–499 (2002)
L. DeGroot, M. Abalovich, E.K. Alexander, Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J. Clin Endocrinol. Metab. 97, 2543–2565 (2012)
Kopp, P., Thyrotoxicosis of other ethiologies. In: De Groot L.J. (ed.) Endotext, http://www.thyroidmanager.org/chapter/thyrotoxicosis-of-other-etiologies/ (2000). Accessed 6 August 2016
J. Ehrenkranz, P.R. Bach, G.L. Snow, A. Schneider, J.L. Lee, S. Ilstrup, S.T. Bennett, S. Benvenga, Circadian and circannual rhythms in thyroid hormones: determining the TSH and free T4 reference intervals based upon time of day, age, and sex. Thyroid 25, 954–961 (2015)
M. Plebani, Biochemical and imaging biomarkers: the search for the Holy Grail. Clin. Chem. Lab. Med. 48, 1055–1056 (2010)
B.C. Ahn, Personalized medicine based on theranostic radioiodine molecular imaging for differentiated thyroid cancer. Biomed. Res. Int. 2016, 9(2016). doi: 10.1155/2016/1680464
G. Ronga, M. Filesi, R. D’Apollo, M. Toteda, A.D. Di Nicola, M. Colandrea et al., Autonomous functioning thyroid nodules and 131I in diagnosis and therapy after 50 years of experience: what is still open to debate? Clin. Nucl. Med. 38, 349–353 (2013)
G. Beckett, F. MacKenzie, Thyroid guidelines – are thyroid-stimulating hormone assays fit for purpose? Ann. Clin. Biochem. 44, 203–208 (2007)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the ethics board of Ente Ospedaliero Cantonale, Bellinzona (Switzerland) and Univerity Hospital of Messina (Italy). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals.
Informed consent
Informed consent was obtained from all individual participants included in the present study.
Rights and permissions
About this article
Cite this article
Giovanella, L., D’Aurizio, F., Campenni’, A. et al. Searching for the most effective thyrotropin (TSH) threshold to rule-out autonomously functioning thyroid nodules in iodine deficient regions. Endocrine 54, 757–761 (2016). https://doi.org/10.1007/s12020-016-1094-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1094-3