Abstract
Brain and muscle ARNT-like protein 1 (BMAL1) is necessary for fertility and has been found to be essential to follicle growth and steroidogenesis. Sirtuin1 (SIRT1) has been reported to interact with BMAL1 and function in a circadian manner. Evidence has shown that SIRT1 regulates aromatase expression in estrogen-producing cells. We aimed to ascertain if there is a relationship between polycystic ovary syndrome (PCOS) and BMAL1, and whether and how BMAL1 takes part in estrogen synthesis in human granulosa cells (hGCs). Twenty-four women diagnosed with PCOS and 24 healthy individuals undergoing assisted reproduction were studied. BMAL1 expression in their granulosa cells (GCs) was observed by quantitative real-time polymerase chain reaction (qRT-PCR). The level of expression in the PCOS group was lower than that of the group without PCOS (p < 0.05). We also analyzed estrogen synthesis and aromatase expression in KGN cell lines. Both were downregulated after BMAL1 and SIRT1 knock-down and, conversely, upregulated after overexpression treatments of these two genes in KGN cells. Both BMAL1 and SIRT1 had a mutually positive regulation, as did the phosphorylation of JNK. Furthermore, JNK overexpression increased estrogen synthesis activity and the expression levels of aromatase, BMAL1, and SIRT1. In KGN and hGCs, estrogen synthesis and aromatase expression were downregulated after treatment with JNK and SIRT1 inhibitors. In addition, BMAL1, SIRT1, and JNK expression levels were all downregulated. Our results demonstrate the effects of BMAL1 on estrogen synthesis in hGCs and suggest a BMAL1–SIRT1–JNK positive feedback cycle in this process, which points out an important role of BMAL1 in the development of PCOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine and metabolic disorders in women of reproductive age. It is characterized by polycystic ovaries, amenorrhea, and hyperandrogenism [1]. The adverse effects of PCOS on a woman’s endocrine system and metabolism damage her reproductive health leading to infertility [2]. Studies have also demonstrated that PCOS patients have an increased abortion and preterm birth rate after in vitro fertilization and embryo transfer (IVF–ET) [3]. This may be the result of hypothalamic–pituitary–ovarian (HPO) axis disorders, theca cell or granulosa cells (GC) dysfunction, and abnormal metabolism, including hyperinsulinemia, insulin resistance, and hyperandrogenism. Studies have shown that women with PCOS have a lower follicle-stimulating hormone (FSH) level during the follicular phase of the menstrual cycle [4, 5]. PCOS is thought to represent a high rate of follicular atresia. It has been demonstrated that the activity of FSH is blocked in ovaries, and its negative feedback inhibition of FSH leads to the abnormal atresia and anovulation [6, 7]. Studies have reported that the GCs normally respond to FSH stimulation with the increase in estrogen [8]. It has also been shown that estradiol production and P450AROM mRNA expression are lower in PCOS follicles, despite no evidence of mutation of the P450 gene [9, 10].
Brain and muscle ARNT-like protein 1 (BMAL1), a cell-autonomous circadian clock oscillator, a member of Circadian family (CLOCK, Cry, BMAL1, Per1, and Per2), provides an internal mechanism by which temporal order is maintained in a rhythmic environment, such as during sleep–wake and feeding cycles, body temperature and blood pressure regulation, release of endocrine hormones, and metabolism. BMAL1 regulates homeostasis commonly in liver, heart, brain, and adipose tissues [11–13], and in the mammalian reproductive system. The circadian clock protein BMAL1 is necessary for fertility and normal testosterone production in Leydig cells of mice, and studies have shown that loss of BMAL1 in ovarian steroidogenic cells results in implantation failure in female mice [14, 15]. It has been demonstrated that FSH induces the circadian oscillator in rat GCs [16–18]. Also, studies have found that the circadian clock protein CLOCK siRNA treatment inhibits the production of estrogen and expression of P450AROM mRNA in cow and heifer GCs [19].
Sirtuin1 (SIRT1) is a nicotinamide adenine dinucleotide(+) (NAD(+))-dependent protein deacetylase which functions in a circadian manner [20, 21]. SIRT1 has been found to take part in regulating metabolism such as obesity and insulin sensitivity [22, 23]. Moreover, it participates in the porcine follicular atresia process, improving the developmental ability of porcine oocytes and promoting the expression of StAR in GCs [24–26]. It has been reported to take a relationship between FSH and steroidogenesis in GCs, which has pointed out its involvement in control of secretory activity of ovarian cells [27].
Previous studies have shown that SIRT1 regulates the expression of aromatase in estrogen-synthesizing cells including human breast epithelial cells and rat ovarian GCs [26, 28]. Reports have also indicated that SIRT1 is a component of the CLOCK/BMAL1 transcription complex and affects the expression of clock genes [20, 29, 30]. However, whether BMAL1 regulates the production of estrogen in human granulosa cells (hGCs), how it carries out this regulation, and what role SIRT1 plays in this process have not been studied. In addition, the role of BMAL1 in the development of PCOS is still unclear. In this study, we examined the differences in BMAL1 levels between PCOS and non-PCOS patients undergoing treatment for infertility. The research also further studied the functional roles of BMAL1 on estrogen synthesis in hGCs in vitro.
Materials and methods
Subjects
A total of 48 women were recruited from the Center for Reproductive Medicine, Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University between September 2014 and September 2015. Twenty-four of the participants were 20- to 35-year-old women undertaking IVF–ET who were diagnosed as PCOS according to the Rotterdam criteria [31] (oligo- and/or anovulation; clinical and/or biochemical signs of hyperandrogenism; and polycystic ovaries with exclusion of other causes of hyperandrogenism, such as hyperprolactinemia, androgen-secreting tumors, Cushing’s syndrome, and non-classical congenital adrenal hyperplasia). The diagnosis of PCOS was satisfied when two or more of the three criteria were met. The remaining 24 participants, forming the non-PCOS group, were healthy women recruited through routine physical examination, tubal factor infertility, or husband’s factor infertility, with regular menstrual cycles (26–35 days) and normal ovarian morphology. Endocrine parameters were measured in the non-PCOS women to exclude hyperandrogenism. None of the participants had used hormonal therapy for at least 3 months before the study. All subjects underwent GnRHa long protocol (decapeptyl 0.05 mg; Gn for 8–12 days) with human chorionic gonadotropin (hCG) trigger, and all women were of Han ethnicity. The study was approved by the ART Ethics Committee of Ren Ji Hospital, School of Medicine, Shanghai Jiao Tong University. All subjects had been given written informed consent to participate in this study. The clinical characteristics of PCOS and non-PCOS group women are shown in Table 1.
Cell culture
We used hGCs and the human granulosa cell line KGN for cell models. hGCs were collected from PCOS and non-PCOS subjects undergoing their first IVF/intracytoplasmic sperm injection cycles at our center. 36 h after hCG trigger, oocytes were retrieved via transvaginal ultrasound-guided aspiration. The follicular fluid (FF) that was not heavily blood-stained was pooled from the patients. The GC isolation protocol was modified slightly from the method as described previously [32]. KGN cells (provided by Shandong University) and hGCs were maintained in phenol red-free DMEM/F12 (Gibco, Grand Island, NY) supplemented with 10 % charcoal-stripped FBS in 6-well plastic dishes (Sigma Chemical Co., St. Louis, MO) at a density of 105 cells/well for 24 h at 37 °C in 5 % CO2 and then washed with PBS to remove unattached cells. For FSH stimulation, the culture medium was replaced with a medium supplemented with rFSH 10 ng/ml refer to the study [33] for 12 h. For the inhibition experiment, we added JNK inhibitor (Selleckchem, Houston, TX) or SIRT1 inhibitor (Selleckchem, Houston, TX) for 24 h.
Transfection experiment
Synthetic siRNAs (GenePharma, Shanghai, China) were delivered into KGN cells using the Lipofectamine RNAiMAX transfection kit (Invitrogen, Carlsbad, CA). The nucleotide sequences of the siRNA were 5′-CCACCAACCCAUACACAGAAGCAAA-3′ (BMAL1) and 5′-CCACCAAAUACACACGAAGCCCAAA-3′ (SIRT1). DNA transfection reagent (Biotool, Houston, TX) and the gene construct BMAL1 (pENTER-BMAL1, Transheep, Shanghai, China), JNK (pcDNA3.1-SIRT1, Transheep, Shanghai, China), and SIRT1 cDNA (pcDNA3 Flag-SIRT1, provided by Huixing Huang, Fudan University, China) were used for the overexpression experiment. Transfection was processed according to the manufacturer’s instructions.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA samples from hGCs were extracted using a total RNA isolation kit (FOREGENE, Chengdu, China) and stored at −80 °C until analysis. The RNA concentration in each sample was determined by measuring the optical density at 260 nm (OD260) and determining the OD260/OD280 ratio using an ultramicro spectrophotometer (Thermo Fisher Scientific, Carlsbad, CA). A total of 500 ng RNAs were used for cDNA synthesis using the PrimeScript RT Master Mix Perfect Real Time kit (TaKaRa, Dalian, China). The primers’ (Sangon, Shanghai, China) sequences were as follows: BMAL1, forward 5′-TGCAAGGGAAGCTCACAGTC-3′ and reverse 5′-GATTGGTGGCACCTCTTAATG-3′; SIRT1, forward 5′-GTAGCACTAATTCCAAGTTCC-3′ and reverse 5′-AAGCTTTACAGGGTTACAGC-3′; β-actin, forward 5′-GGGAAATCGTGCGTGACATTAAG-3′ and reverse 5′-TGTGTTGGCGTACAGGTCTTTG-3′; CLOCK, forward 5′- TGCGAGGAACAATAGACCCAA-3′ and reverse 5′- ATGGCCTATGTGTGCGTTGTA-3′.
Western blot analysis
Samples of ovarian protein extracts were mixed with sodium dodecyl sulfate (SDS) sample buffer and boiled for 10 min. Then, 30 μg proteins from each sample were loaded onto an SDS polyacrylamide gel for electrophoresis and subsequently transferred to polyvinylidene fluoride membranes. The membranes were blocked in 5 % non-fat milk for 60 min at room temperature before being incubated overnight at 4 °C with the following primary antibodies: anti-BMAL1 (Abcam, Cambridge, UK), anti-SIRT1 (Cell Signaling, Danvers, MA), anti-pSIRT1 (Cell Signaling, Danvers, MA), anti-JNK (Cell Signaling, Danvers, MA), anti-pJNK (Cell Signaling, Danvers, MA), anti-AROM (Abcam, Cambridge, UK), and anti-β-actin (Santa Cruz Biotechnology, Santa Cruz, CA). Samples were then incubated for 90 min at room temperature with secondary antibodies (Cell Signaling, Danvers, MA). Chemiluminescence reagent (Thermo Fisher Scientific, Carlsbad, CA) was used to visualize the blots. All experiments were repeated on three separate occasions.
Steroid assays
Testosterone (Sigma Chemical Co., St. Louis, MO) 10−7 ng/mL was added as the substrate for estrogen synthesis. After 3 h, the levels of estrogen in the spent media were measured using the ECLIA (electrochemiluminescence immunoassay) kits (Roche, Indianapolis, IN) according to the manufacturer’s instructions.
Statistical analysis
Results were expressed as mean ± SEM. Differences between groups were determined using a t test or one-way ANOVA test followed by the Newman–Keuls multiple comparison test. Significance was defined as p < 0.05. All analyses were conducted using SPSS 21.0 for Windows (IBM, Chicago, IL, USA).
Results
BMAL1 mRNA expression in GCs was lower in PCOS patients than that in non-PCOS group
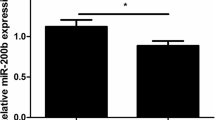
To determine if the expression of BMAL1 was altered in PCOS, a qRT-PCR assay was developed to measure human BMAL1 mRNA levels of GC samples. In Table 1, the average BMI of non-PCOS group (21.01 ± 2.74) was lower than that of PCOS group (23.10 ± 3.64) (p < 0.05). In order to exclude the influence of BMI on the expression of BMAL1, we additionally examined BMAL1 mRNA levels between PCOS group and non-PCOS group with normal BMI. As shown in Fig. 1a, BMAL1 mRNA levels were lower in PCOS patients than in the non-PCOS group (p < 0.05), among which, BMAL1 mRNA levels in PCOS (normal BMI) group were significantly lower than in the non-PCOS (normal BMI) group (p < 0.05). These suggested that low levels of BMAL1 expression in GCs took part in the occurrence and development of PCOS. It is well established that BMAL1 forms a protein complex with CLOCK and SIRT1 [23, 30]. In this study, CLOCK and SIRT1 expression in PCOS or non-PCOS groups were also determined. And as shown in Fig. 1, CLOCK mRNA levels in PCOS group were lower compared to the other group (p < 0.05). However, CLOCK mRNA levels had no significance between the PCOS (normal BMI) group and non-PCOS (normal BMI) group (Fig. 1c). Meanwhile, SIRT1 mRNA levels had no significance between the compared groups (Fig. 1b).
BMAL1, SIRT1, and CLOCK mRNA levels of hGCs in PCOS patients (n = 24), non-PCOS patients (n = 24) including PCOS with normal BMI patients (n = 14), non-PCOS with normal BMI patients (n = 18). a BMAL1 mRNA levels were analyzed by qRT-PCR. b SIRT1 mRNA levels were analyzed by qRT-PCR. c CLOCK mRNA levels were analyzed by qRT-PCR. The data are given as the mean ± SEM. * indicates significance (p < 0.05)
BMAL1 regulated estrogen synthesis and SIRT1 expression in GCs
The mechanism of BMAL1’s contribution to the pathogenesis of PCOS was still unclear. To evaluate the function of BMAL1 in hGCs, KGN cells were exposed to BMAL1 siRNA and then treated with FSH (Fig. 2a). siRNA knock-down of BMAL1 suppressed the levels of CYP19a1, aromatase, and estradiol production (p < 0.05) in human granulosa cell line KGN with FSH stimulation (Fig. 2b–d). Meanwhile, loss of BMAL1 function was associated with the downregulated expression levels of both T-SIRT1 and p-SIRT1 (Fig. 2c), which revealed that SIRT1 might be a potential downstream protein between BMAL1 and aromatase. To give additional support for this theory, we overexpressed BMAL1 in KGN cells, and as expected, the levels of estrogen (p < 0.05), aromatase, and SIRT1 expression were upregulated (Fig. 2f, g). Therefore, BMAL1 may regulate aromatase by SIRT1 under FSH stimulation.
Steroid assays, protein expression, and mRNA levels by BMAL1 regulation in KGN cells. a BMAL1 knock-down efficiency (0.84 ± 0.04) was ascertained by qRT-PCR analysis of BMAL1. b Estrogen levels were measured after BMAL1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h. c Expression of the proteins aromatase, SIRT1, and BMAL1 after BMAL1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h was detected by Western blot analysis. d CYP19a1 mRNA levels were measured after BMAL1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h. e BMAL1 overexpression efficiency was ascertained by qRT-PCR analysis of BMAL1. f Estrogen levels were measured after BMAL1 overexpression for 48 h. g Protein expression of aromatase, SIRT1, and BMAL1 after BMAL1 overexpression for 48 h in KGN cells was determined. For Western blot, three independent experiments were performed, and a representative result is shown. At left, a typical Western blot is shown; at right, the immunoreactive bands (left panel) were densitometrically quantified and the intensities shown relative to the siRNA-negative control (*) or the siRNA-BMAL1+FSH group (#) (c) and relative to vector group (*) (g). Bars represent mean ± SEM from three independent experiments. * or # indicates significance (p < 0.05), **(p < 0.01)
SIRT1 exerted a positive feedback on BMAL1 expression
To determine whether SIRT1 is required in estrogen synthesis and regulated by BMAL1, SIRT1 were knocked down or overexpressed in KGN cells with FSH. As before, we observed that siRNA knock-down of SIRT1 suppressed levels of CYP19a1, aromatase and estradiol production (p < 0.05) after FSH stimulation in KGN cells (Fig. 3b–d). Meanwhile, loss of SIRT1 function was associated with downregulated expression levels of BMAL1 (Fig. 3c), which revealed that SIRT1 might have a positive feedback effect on BMAL1. To give an additional support, we overexpressed SIRT1 in KGN cells and, as expected, observed the heightened levels of estrogen (p < 0.05), aromatase, and BMAL1 expression (Fig. 3f, g). These results showed that SIRT1 regulated aromatase and estradiol production under FSH stimulation. Because of the positive change in BMAL1 expression after the increase in SIRT1, we concluded that SIRT1 had a positive feedback effect on BMAL1.
Steroid assays, protein expression, and mRNA levels by SIRT1 regulation in KGN cells. a SIRT1 knock-down efficiency (0.87 ± 0.01) was ascertained by qRT-PCR analysis of SIRT1. b Estrogen levels were measured after SIRT1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h. c Expression of the proteins aromatase, SIRT1, and BMAL1 after SIRT1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h was detected by Western blot analysis. d CYP19a1 mRNA levels were measured after SIRT1 knock-down in KGN cells with or without FSH (10 ng/mL) for 12 h. e SIRT1 overexpression efficiency was ascertained by qRT-PCR analysis of SIRT1. f Estrogen levels were measured after SIRT1 overexpression for 48 h. g Expression of the proteins aromatase, SIRT1, and BMAL1 after SIRT1 overexpression for 48 h in KGN cells was analyzed. For Western blot, 3 independent experiments were performed and a representative result is shown. At left, a representative Western blot is shown; at right, the immunoreactive bands (left panel) were densitometrically quantified and the intensities shown relative to the siRNA-negative control (*) or the siRNA-SIRT1+FSH group (#) (c) and relative to vector group (*) (g). Bars represent mean ± SEM from three independent experiments. * or # Indicates significance (p < 0.05), ** (p < 0.01)
BMAL1–SIRT1 regulated aromatase expression and estrogen production through JNK activation
The c-Jun N-terminal kinase (JNK) pathway has been shown to be essential for cell cycle progression and mitosis in GCs of follicles [34]. Studies have also shown that JNK is involved in FSH-induced estradiol production in GCs and also takes part in the regulation of estrogen synthesis in breast cells [35–37]. To study its role in the BMAL1 and SIRT1 pathway, we examined JNK expression after knock-down or overexpression of BMAL1 and SIRT1. The knock-down of BMAL1 and SIRT1 led to reduced phosphorylation of JNK (Fig. 4a, b), while the overexpressed BMAL1 and SIRT1 led to increased phosphorylation of JNK (Fig. 4c). In addition, overexpressed JNK showed an upregulated estrogen level (p < 0.05) as well as aromatase and SIRT1 expression levels (Fig. 4d, e). In addition, positive regulation of BMAL1 indicated the existence of a positive feedback cycle in this regulation process (Fig. 4d).
Estrogen assays and JNK expression in KGN cells after BMAL1 and SIRT1 knock-down. a, b JNK expression levels were detected in KGN cells after BMAL1 or SIRT1 knock-down with or without FSH (10 ng/mL) for 12 h. c JNK expression levels were detected after BMAL1 or SIRT1 overexpression for 48 h. d, e Aromatase and estrogen levels after JNK overexpression for 48 h were determined by Western blot analysis and electrochemiluminescence immunoassay (ECLIA.) For Western blot, three independent experiments were performed and a representative result is shown. The immunoreactive bands (left panel) were densitometrically quantified and the intensities shown relative to the siRNA-negative control (*) or the siRNA-positive+FSH group (#) (a, b) and relative to vector group (*) (c, d). Bars represent mean ± SEM from three independent experiments. * or # Indicates significance (p < 0.05), **(p < 0.01)
BMAL1 and SIRT1 created a positive feedback cycle
To strengthen these findings, we treated KGN cells with FSH using inhibitors of JNK and SIRT1. As expected, we observed the suppression of estradiol production (p < 0.05) (Fig. 5a) and the reduction of aromatase expression levels (Fig. 5b). At the same time, JNK and SIRT1 inhibitors significantly inhibited the phosphorylation and protein expression of both JNK and SIRT1, and downregulated the expression of BMAL1 (Fig. 5b). We then used hGCs from healthy control women, adding JNK and SIRT1 inhibitors, and observed similar results (p < 0.05) (Fig. 5c, d). These results indicated that the inhibition of both JNK and SIRT1 activation decreased the estradiol production possibly through a BMAL1–JNK–SIRT1-positive feedback cycle.
Estrogen assays and protein expression in KGN cells and hGCs with JNK or SIRT1 inhibitors for 24 h. a Estrogen levels were measured after exposure with or without JNK inhibitor (1, 5 μM) and SIRT1 inhibitor (5, 10 μM) in KGN cells by ECLIA. b Aromatase, BMAL1, JNK, and SIRT1 expression levels were detected after exposure with or without JNK inhibitor (1, 5 μM) and SIRT1 inhibitor (5, 10 μM) in KGN cells by Western blot analysis. c Estrogen levels were measured after exposure with or without JNK inhibitor (1, 5 μM) and SIRT1 inhibitor (5, 10 μM) in hGCs by ECLIA. d Aromatase, BMAL1, JNK, and SIRT1 expression levels were determined after exposure with or without JNK inhibitor (1, 5 μM) and SIRT1 inhibitor (5, 10 μM) in hGCs. For Western blot, three independent experiments were performed, and a representative result is shown. Bars represent mean ± SEM from the three experiments. The immunoreactive bands (right panel) were densitometrically quantified and the intensities shown relative to the control group without inhibitor. * Indicates significance (p < 0.05), ** (p < 0.01)
Discussion
The molecular circadian clock, BMAL1, found in steroidogenic cells, is crucial for normal female reproduction, especially during embryonic implantation [15, 38]. Previous studies have shown that BMAL1−/− females are infertile. The BMAL1−/− mice showed significantly lower progesterone levels due to decreased expression of steroidogenic acute regulatory protein in corpora lutea. The regulation of steroidogenic acute regulatory by BMAL1 has been well established in vivo and vitro. Mice with deletion of BMAL1 in ovarian GCs or theca cells show different phenotype. Conditional KO of BMAL1 in ovarian theca cells abolished the rhythm of ovarian sensitivity to LH, but not in mice with conditional deletion of BMAL1 in GCs. These results imply the role of BMAL1 involved in LH response and progesterone synthesis [15, 38, 39]. SIRT1 has been reported to function in a circadian manner, interacting with BMAL1 in most cell nuclei and forming a component of CLOCK/BMAL1 transcription complexes, thereby affecting the expression of clock genes [20, 29, 30]. In this study, we found that BMAL1 took part in the process of estrogen production in hGCs. Moreover, we have shown that BMAL1 may regulate aromatase expression through the BMAL1–SIRT1–JNK cycle. Both BMAL1 and SIRT1 exerted positive feedback on each other. Meanwhile, our results illustrate that the SIRT1–BMAL1-dependent activation of aromatase and estrogen production relies on JNK signaling activation (Fig. 4). Our study for the first time demonstrates a BMAL1–SIRT1 unit that regulates the mechanism of estrogen synthesis in GCs (Figs. 2, 3, 4, 5). To our knowledge, we are the first to find this positive feedback cycle. SIRT1 has previously been shown to regulate the activity of non-histone proteins such as ERRα [40] and β-catenin [41], which have been implicated in the regulation of aromatase transcription [42]. Also, evidence exists that SIRT1 is physically associated with aromatase promoters [28]. Our experimental data demonstrate that either SIRT1 knock-down or with inhibitor treatment could reduce the activity of aromatase (Figs. 3, 5). The precise mechanism of aromatase regulation by SIRT1 in hGCs requires further study.
Additionally, the similar effects of BMAL1 and SIRT1 knock-down on aromatase activity and estrogen synthesis with FSH stimulation were shown in our data. However, the data showed that at baseline, siRNA for either BMAL1 or SIRT1 had less affect on estrogen synthesis without FSH, and these results imply that BMAL1 and SIRT1 might exert their function through regulating FSHR. Meanwhile, data from other investigator showed that FSHR was expressed in a feeble rhythmic fashion in mouse ovary, and the rhythms were disrupted in the ovary with BMAL1 conditional knockout in mice GCs [43]. We hypothesize that FSHR expression might be under the control of BMAL1–SIRT1 cycle. Moreover, our experiments have found that the knock-down of BMAL1 or SIRT1 by small interference RNA could downregulated the mRNA level of FSHR (data not shown), which might imply that BMAL1–SIRT1 cycle exerts its function of estrogen synthesis via regulating FSHR and revealed the important role of this cycle played in PCOS. Further studies need to be done to elucidate this hypothesis.
Anovulation in PCOS is characterized by the arrest of antral follicle development, which results in failure to enter the preovulatory phase of the menstruation cycle. It has been established that estrogen biosynthesis by GCs is under the control of FSH and requires testosterone from theca cells. The developing follicle secretes increasing amounts of estradiol, which leads to the midcycle surge of LH that triggers ovulation. It is known that estradiol production is low in PCOS follicles. Women with PCOS have lower FSH in the follicular phase. PCOS thought to have an FSH blocked ovaries has a negative feedback inhibition of FSH [6, 7, 9, 10]. Importantly, it is the first time to show that the expression of BMAL1 is lower in PCOS patients compared to non-PCOS women (Fig. 1). We hypothesize that low levels of BMAL1 in hGCs underlie the development of PCOS, because it is involved in the inhibition of FSH stimulation in the ovaries. FSH is not high enough in PCOS to produce an estrogenic microenvironment, which eventually leads to low follicular estrogen levels, antral follicle arrest, and anovulation. Implantation depends on the mutual interaction between a receptive endometrium and a blastocyst, and is essential for successful pregnancy. It is regulated by exposure to estrogen and progesterone, which allows follicular development, ovulation, blastocyst formation, and preparation of a receptive endometrium. Estrogen and progesterone drive the proliferation and differentiation of the endometrial tissue to prepare it for blastocyst implantation. Their downstream genes (LIF, Hoxa-10, HSD17B1, etc.) stimulate a crosstalk between the endometrial stroma and epithelium to increase endometrial receptivity [44–46]. Imbalances in the homeostasis of these processes may become a pathogenic factor for infertility. Women with PCOS are reported to have a high prevalence of infertility [2]. Endometrial stromal fibroblasts have an abnormal decidualization response to estrogen and progesterone in PCOS [47]. Evidence also exists that BMAL1 regulates the production of progesterone in GCs [15, 48]. We hypothesize that lower expression of BMAL1 in PCOS causes an estrogen–progesterone imbalance which may take part in the pathogenesis of infertility in PCOS. Further studies need to be undertaken to confirm this hypothesis.
To strengthen the evidence and determine if there was a significant difference in SIRT1 expression between PCOS and non-PCOS individuals, we used qRT-PCR to measure human SIRT1 mRNA levels in GC samples. As shown in Fig. 1b, SIRT1 mRNA levels were lower in PCOS individuals but with no significance (p > 0.05), which indicated the existence of other complex mechanism of estrogen synthesis in hGCs. What is more, our results have shown that CLOCK mRNA levels in PCOS group were lower compared to the other group (p < 0.05), but the levels had no significance between PCOS group and non-PCOS group with normal BMI (Fig. 1c). More clinical cases need to be studied in order to find out the role of CLOCK for the future research.
PCOS is characterized by endocrine and metabolic disorders. Numerous studies have demonstrated that obese, normal weight or thin women with PCOS have form of insulin resistance. Hyperinsulinemia resulting from insulin resistance plays an important role in PCOS by stimulating ovarian testosterone production and impeding ovulation. Studies have also shown that insulin stimulates steroidogenesis in both granulosa and theca cells in the human ovary [49–51]. BMAL1 and SIRT1 have been found to regulate the circadian change in insulin sensitivity [23, 52]. We hypothesize that a BMAL1–SIRT1 cycle may be involved in the development of insulin resistance in PCOS. More details such as average HOMA-IR and more clinical cases need to be studied to analyze the precise relationship between insulin resistance in PCOS and the BMAL1–SIRT1 cycle.
Previous studies have shown the rhythmical character of BMAL1 in transiently cultured rat GCs in vitro after FSH or LH stimulation [18, 48]. We have determined the mRNA level of BMAL1 and SIRT1 in KGN cells at 0, 12, 24, 36, 48 h cultured after cell-autonomous period, which shows no disparity at different time (data not shown). Due to the decades of culture in vitro, the KGN cells may have loss the characters of auto-rhythmic regulation, and we hypothesize that the auto-rhythm of BMAL1–SIRT1 could have been disrupted for the sake of long time culture, which may show us a potentially “clock-independent” role of BMAL1–SIRT1 in regulating steroid biosynthesis and FSHR signaling in hGCs.
Our findings may update our understanding of BMAL1 in hGCs, especially its role in regulating estrogen synthesis. In addition, our study is the first to demonstrate a role for BMAL1–SIRT1 positive cycle in the development of PCOS, which may help offer an instruction of diagnosis, treatment, and prognosis for the clinic in the future.
References
D.A. Ehrmann, Polycystic ovary syndrome. N. Engl. J. Med. 352(12), 1223–1236 (2005). doi:10.1056/NEJMra041536
X. Xu, Y. Shi, Y. Cui, J. Ma, L. Che, Z.J. Chen, Endocrine and metabolic characteristics of polycystic ovary syndrome in Chinese women with different phenotypes. Clin. Endocrinol. 76(3), 425–430 (2012). doi:10.1111/j.1365-2265.2011.04194.x
X. Yan, Y.H. Shi, Y. Sheng, R. Tang, L.H. Xu, Y. Li, Z.J. Chen, Pregnancy outcomes of patients with polycystic ovary syndrome undergoing in vitro fertilization and embryo transfer. Zhonghua fu chan ke za zhi 46(12), 923–927 (2011)
R. Rebar, H.L. Judd, S.S. Yen, J. Rakoff, G. Vandenberg, F. Naftolin, Characterization of the inappropriate gonadotropin secretion in polycystic ovary syndrome. J. Clin. Investig. 57(5), 1320–1329 (1976). doi:10.1172/jci108400
D.T. Baird, C.S. Corker, D.W. Davidson, W.M. Hunter, E.A. Michie, P.F. Van Look, Pituitary–ovarian relationships in polycystic ovary syndrome. J. Clin. Endocrinolo. Metab. 45(4), 798–801 (1977). doi:10.1210/jcem-45-4-798
S. Franks, J. Stark, K. Hardy, Follicle dynamics and anovulation in polycystic ovary syndrome. Hum. Reprod. Update. 14(4), 367–378 (2008). doi:10.1093/humupd/dmn015
A. Chavez-Ross, S. Franks, H.D. Mason, K. Hardy, J. Stark, Modelling the control of ovulation and polycystic ovary syndrome. J. Math. Biol. 36(1), 95–118 (1997)
S. Franks, N. Gharani, D. Waterworth, S. Batty, D. White, R. Williamson, M. McCarthy, Current developments in the molecular genetics of the polycystic ovary syndrome. Trends Endocrinol. Metab. 9(2), 51–54 (1998)
A.J. Jakimiuk, S.R. Weitsman, P.R. Brzechffa, D.A. Magoffin, Aromatase mRNA expression in individual follicles from polycystic ovaries. Mol. Hum. Reprod. 4(1), 1–8 (1998)
D. Soderlund, P. Canto, S. Carranza-Lira, J.P. Mendez, No evidence of mutations in the P450 aromatase gene in patients with polycystic ovary syndrome. Hum. Reprod. (Oxford) 20(4), 965–969 (2005). doi:10.1093/humrep/deh690
M.H. Hastings, A.B. Reddy, E.S. Maywood, A clockwork web: circadian timing in brain and periphery, in health and disease. Nat. Rev. Neurosci. 4(8), 649–661 (2003). doi:10.1038/nrn1177
K.F. Storch, O. Lipan, I. Leykin, N. Viswanathan, F.C. Davis, W.H. Wong, C.J. Weitz, Extensive and divergent circadian gene expression in liver and heart. Nature 417(6884), 78–83 (2002). doi:10.1038/nature744
S. Shimba, T. Ogawa, S. Hitosugi, Y. Ichihashi, Y. Nakadaira, M. Kobayashi, M. Tezuka, Y. Kosuge, K. Ishige, Y. Ito, K. Komiyama, Y. Okamatsu-Ogura, K. Kimura, M. Saito, Deficient of a clock gene, brain and muscle Arnt-like protein-1 (BMAL1), induces dyslipidemia and ectopic fat formation. PLoS One 6(9), e25231 (2011). doi:10.1371/journal.pone.0025231
J.D. Alvarez, A. Hansen, T. Ord, P. Bebas, P.E. Chappell, J.M. Giebultowicz, C. Williams, S. Moss, A. Sehgal, The circadian clock protein BMAL1 is necessary for fertility and proper testosterone production in mice. J. Biol. Rhythm. 23(1), 26–36 (2008). doi:10.1177/0748730407311254
Y. Liu, B.P. Johnson, A.L. Shen, J.A. Wallisser, K.J. Krentz, S.M. Moran, R. Sullivan, E. Glover, A.F. Parlow, N.R. Drinkwater, L.A. Schuler, C.A. Bradfield, Loss of BMAL1 in ovarian steroidogenic cells results in implantation failure in female mice. Proc. Natl. Acad. Sci. U.S.A. 111(39), 14295–14300 (2014). doi:10.1073/pnas.1209249111
G. Chu, I. Misawa, H. Chen, N. Yamauchi, Y. Shigeyoshi, S. Hashimoto, M.A. Hattori, Contribution of FSH and triiodothyronine to the development of circadian clocks during granulosa cell maturation. Am. J. Physiol. Endocrinol. Metab. 302(6), E645–E653 (2012). doi:10.1152/ajpendo.00470.2011
P.J. He, M. Hirata, N. Yamauchi, S. Hashimoto, M.A. Hattori, Gonadotropic regulation of circadian clockwork in rat granulosa cells. Mol. Cell. Biochem. 302(1–2), 111–118 (2007). doi:10.1007/s11010-007-9432-7
H. Chen, L. Zhao, G. Chu, G. Kito, N. Yamauchi, Y. Shigeyoshi, S. Hashimoto, M.A. Hattori, FSH induces the development of circadian clockwork in rat granulosa cells via a gap junction protein Cx43-dependent pathway. Am. J. Physiol. Endocrinol. Metab. 304(6), E566–E575 (2013). doi:10.1152/ajpendo.00432.2012
T. Shimizu, Y. Hirai, C. Murayama, A. Miyamoto, H. Miyazaki, K. Miyazaki, Circadian clock genes Per2 and clock regulate steroid production, cell proliferation, and luteinizing hormone receptor transcription in ovarian granulosa cells. Biochem. Biophys. Res. Commun. 412(1), 132–135 (2011). doi:10.1016/j.bbrc.2011.07.058
Y. Nakahata, M. Kaluzova, B. Grimaldi, S. Sahar, J. Hirayama, D. Chen, L.P. Guarente, P. Sassone-Corsi, The NAD+ -dependent deacetylase SIRT1 modulates CLOCK-mediated chromatin remodeling and circadian control. Cell 134(2), 329–340 (2008). doi:10.1016/j.cell.2008.07.002
Y. Nakahata, S. Sahar, G. Astarita, M. Kaluzova, P. Sassone-Corsi, Circadian control of the NAD+ salvage pathway by CLOCK-SIRT1. Science (New York) 324(5927), 654–657 (2009). doi:10.1126/science.1170803
S. Mariani, D. Fiore, S. Basciani, A. Persichetti, S. Contini, C. Lubrano, L. Salvatori, A. Lenzi, L. Gnessi, Plasma levels of SIRT1 associate with non-alcoholic fatty liver disease in obese patients. Endocrine 49(3), 711–716 (2015). doi:10.1007/s12020-014-0465-x
B. Zhou, Y. Zhang, F. Zhang, Y. Xia, J. Liu, R. Huang, Y. Wang, Y. Hu, J. Wu, C. Dai, H. Wang, Y. Tu, X. Peng, Y. Wang, Q. Zhai, CLOCK/BMAL1 regulates circadian change of mouse hepatic insulin sensitivity by SIRT1. Hepatology (Baltimore) 59(6), 2196–2206 (2014). doi:10.1002/hep.26992
F. Zhao, W. Zhao, S. Ren, Y. Fu, X. Fang, X. Wang, B. Li, Roles of SIRT1 in granulosa cell apoptosis during the process of follicular atresia in porcine ovary. Anim. Reprod. Sci. 151(1–2), 34–41 (2014). doi:10.1016/j.anireprosci.2014.10.002
N. Itami, K. Shirasuna, T. Kuwayama, H. Iwata, Resveratrol improves the quality of pig oocytes derived from early antral follicles through sirtuin 1 activation. Theriogenology 83(8), 1360–1367 (2015). doi:10.1016/j.theriogenology.2015.01.029
Y. Morita, O. Wada-Hiraike, T. Yano, A. Shirane, M. Hirano, H. Hiraike, S. Koyama, H. Oishi, O. Yoshino, Y. Miyamoto, K. Sone, K. Oda, S. Nakagawa, K. Tsutsui, Y. Taketani, Resveratrol promotes expression of SIRT1 and StAR in rat ovarian granulosa cells: an implicative role of SIRT1 in the ovary. Reprod. Biol. Endocrinol. 10, 14 (2012). doi:10.1186/1477-7827-10-14
A.V. Sirotkin, P. Dekanova, A.H. Harrath, S.H. Alwasel, D. Vasicek, Interrelationships between sirtuin 1 and transcription factors p53 and NF-kappaB (p50/p65) in the control of ovarian cell apoptosis and proliferation. Cell Tissue Res. 358(2), 627–632 (2014). doi:10.1007/s00441-014-1940-7
K.R. Holloway, A. Barbieri, S. Malyarchuk, M. Saxena, A. Nedeljkovic-Kurepa, M. CameronMehl, A. Wang, X. Gu, K. Pruitt, SIRT1 positively regulates breast cancer associated human aromatase (CYP19A1) expression. Mol. Endocrinol. (Baltimore) 27(3), 480–490 (2013). doi:10.1210/me.2012-1347
G. Asher, D. Gatfield, M. Stratmann, H. Reinke, C. Dibner, F. Kreppel, R. Mostoslavsky, F.W. Alt, U. Schibler, SIRT1 regulates circadian clock gene expression through PER2 deacetylation. Cell 134(2), 317–328 (2008). doi:10.1016/j.cell.2008.06.050
I. Park, Y. Lee, H.D. Kim, K. Kim, Effect of resveratrol, a SIRT1 activator, on the interactions of the CLOCK/BMAL1 complex. Endocrinol. Metab. (Seoul) 29(3), 379–387 (2014). doi:10.3803/EnM.2014.29.3.379
E.S. Rotterdam, ASRM-Sponsored PC, Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. (Oxford) 19(1), 41–47 (2004)
H. Matsubara, K. Ikuta, Y. Ozaki, Y. Suzuki, N. Suzuki, T. Sato, K. Suzumori, Gonadotropins and cytokines affect luteal function through control of apoptosis in human luteinized granulosa cells. J.Clin. Endocrinol. Metab. 85(4), 1620–1626 (2000). doi:10.1210/jcem.85.4.6509
I. Foldesi, M. Breckwoldt, J. Neulen, Oestradiol production by luteinized human granulosa cells: evidence of the stimulatory action of recombinant human follicle stimulating hormone. Hum. Reprod. (Oxford) 13(6), 1455–1460 (1998)
O. Oktem, E. Buyuk, K. Oktay, Preantral follicle growth is regulated by c-Jun-N-terminal kinase (JNK) pathway. Reprod. sci. (Thousand Oaks) 18(3), 269–276 (2011). doi:10.1177/1933719110385709
T. Miyoshi, F. Otsuka, M. Yamashita, K. Inagaki, E. Nakamura, N. Tsukamoto, M. Takeda, J. Suzuki, H. Makino, Functional relationship between fibroblast growth factor-8 and bone morphogenetic proteins in regulating steroidogenesis by rat granulosa cells. Mol. Cell. Endocrinol. 325(1–2), 84–92 (2010). doi:10.1016/j.mce.2010.04.012
J. Guo, Y. Yuan, D. Lu, B. Du, L. Xiong, J. Shi, L. Yang, W. Liu, X. Yuan, G. Zhang, F. Wang, Two natural products, trans-phytol and (22E)-ergosta-6,9,22-triene-3beta,5alpha,8alpha-triol, inhibit the biosynthesis of estrogen in human ovarian granulosa cells by aromatase (CYP19). Toxicol. Appl. Pharmacol. 279(1), 23–32 (2014). doi:10.1016/j.taap.2014.05.008
F. Li, L. Ye, S.M. Lin, L.K. Leung, Dietary flavones and flavonones display differential effects on aromatase (CYP19) transcription in the breast cancer cells MCF-7. Mol. Cell. Endocrinol. 344(1–2), 51–58 (2011). doi:10.1016/j.mce.2011.06.024
H. Chen, G. Chu, L. Zhao, N. Yamauchi, Y. Shigeyoshi, S. Hashimoto, M.A. Hattori, Rev-erbalpha regulates circadian rhythms and StAR expression in rat granulosa cells as identified by the agonist GSK4112. Biochem. Biophys. Res. Commun. 420(2), 374–379 (2012). doi:10.1016/j.bbrc.2012.02.164
C.K. Ratajczak, K.L. Boehle, L.J. Muglia, Impaired steroidogenesis and implantation failure in Bmal1−/− mice. Endocrinology 150(4), 1879–1885 (2009). doi:10.1210/en.2008-1021
B.J. Wilson, A.M. Tremblay, G. Deblois, G. Sylvain-Drolet, V. Giguere, An acetylation switch modulates the transcriptional activity of estrogen-related receptor alpha. Mol. Endocrinol.(Baltimore) 24(7), 1349–1358 (2010). doi:10.1210/me.2009-0441
K.R. Holloway, T.N. Calhoun, M. Saxena, C.F. Metoyer, E.F. Kandler, C.A. Rivera, K. Pruitt, SIRT1 regulates Dishevelled proteins and promotes transient and constitutive Wnt signaling. Proc. Natl. Acad. Sci. USA 107(20), 9216–9221 (2010). doi:10.1073/pnas.0911325107
T.N. Parakh, J.A. Hernandez, J.C. Grammer, J. Weck, M. Hunzicker-Dunn, A.J. Zeleznik, J.H. Nilson, Follicle-stimulating hormone/cAMP regulation of aromatase gene expression requires beta-catenin. Proc. Natl. Acad. Sci. USA 103(33), 12435–12440 (2006). doi:10.1073/pnas.0603006103
A.L. Mereness, Z.C. Murphy, A.C. Forrestel, S. Butler, C. Ko, J.S. Richards, M.T. Sellix, Conditional deletion of bmal1 in ovarian theca cells disrupts ovulation in female mice. Endocrinology 157(2), 913–927 (2016). doi:10.1210/en.2015-1645
L. Aghajanova, A. Hamilton, J. Kwintkiewicz, K.C. Vo, L.C. Giudice, Steroidogenic enzyme and key decidualization marker dysregulation in endometrial stromal cells from women with versus without endometriosis. Biol. Reprod. 80(1), 105–114 (2009). doi:10.1095/biolreprod.108.070300
H. Lim, L. Ma, W.G. Ma, R.L. Maas, S.K. Dey, Hoxa-10 regulates uterine stromal cell responsiveness to progesterone during implantation and decidualization in the mouse. Mol. Endocrinol. (Baltimore) 13(6), 1005–1017 (1999). doi:10.1210/mend.13.6.0284
C.L. Stewart, P. Kaspar, L.J. Brunet, H. Bhatt, I. Gadi, F. Kontgen, S.J. Abbondanzo, Blastocyst implantation depends on maternal expression of leukaemia inhibitory factor. Nature 359(6390), 76–79 (1992). doi:10.1038/359076a0
T.T. Piltonen, J.C. Chen, M. Khatun, M. Kangasniemi, A. Liakka, T. Spitzer, N. Tran, H. Huddleston, J.C. Irwin, L.C. Giudice, Endometrial stromal fibroblasts from women with polycystic ovary syndrome have impaired progesterone-mediated decidualization, aberrant cytokine profiles and promote enhanced immune cell migration in vitro. Hum. Reprod. (Oxford) 30(5), 1203–1215 (2015). doi:10.1093/humrep/dev055
H. Chen, L. Zhao, M. Kumazawa, N. Yamauchi, Y. Shigeyoshi, S. Hashimoto, M.A. Hattori, Downregulation of core clock gene Bmal1 attenuates expression of progesterone and prostaglandin biosynthesis-related genes in rat luteinizing granulosa cells. Am. J. Physiol. Cell Physiol. 304(12), C1131–C1140 (2013). doi:10.1152/ajpcell.00008.2013
R.S. Legro, C.L. Gnatuk, A.R. Kunselman, A. Dunaif, Changes in glucose tolerance over time in women with polycystic ovary syndrome: a controlled study. J. Clin. Endocrinol. Metab. 90(6), 3236–3242 (2005). doi:10.1210/jc.2004-1843
D.K. Panidis, D.H. Rousso, I.M. Matalliotakis, A.I. Kourtis, G.D. Vlassis, E.E. Koumantakis, Hyperinsulinemia does not influence androgens/estrogens ratio in patients with polycystic ovarian syndrome. Int. J. Fertil Women’s Med. 44(6), 301–306 (1999)
J.E. Nestler, D.J. Jakubowicz, A.F. de Vargas, C. Brik, N. Quintero, F. Medina, Insulin stimulates testosterone biosynthesis by human thecal cells from women with polycystic ovary syndrome by activating its own receptor and using inositolglycan mediators as the signal transduction system. J. Clin. Endocrinol. Metab. 83(6), 2001–2005 (1998). doi:10.1210/jcem.83.6.4886
J.H. Lee, M.Y. Song, E.K. Song, E.K. Kim, W.S. Moon, M.K. Han, J.W. Park, K.B. Kwon, B.H. Park, Overexpression of SIRT1 protects pancreatic beta-cells against cytokine toxicity by suppressing the nuclear factor-kappaB signaling pathway. Diabetes 58(2), 344–351 (2009). doi:10.2337/db07-1795
Acknowledgments
This work was supported in part by grants from the National Natural Science Foundation (81490743 and 81370687) and Shanghai Municipal Education Commission–Gaofeng Clinical Medicine (20152510).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, J., Liu, J., Zhu, K. et al. Effects of BMAL1–SIRT1-positive cycle on estrogen synthesis in human ovarian granulosa cells: an implicative role of BMAL1 in PCOS. Endocrine 53, 574–584 (2016). https://doi.org/10.1007/s12020-016-0961-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-0961-2