Abstract
The aim of this study was to assess the effects of genistein (G) and daidzein (D) on the histological, hormonal, and functional parameters of the pituitary-ovarian axis in middle-aged female rats, and to compare these effects with the effects of estradiol (E), commonly used in the prevention and treatment of menopausal symptoms. Middle-aged (12 month old) Wistar female rats subcutaneously received 35 mg/kg of G, or 35 mg/kg of D, or 0.625 mg/kg of E every day for 4 weeks. Each of the treated groups had a corresponding control group. An intact control group was also established. G and D did not change the intracellular protein content within gonadotropic and lactotropic cells, but vacuolization was observed in all the cell types. In contrast, E caused an inhibition of gonadotropic and stimulation of lactotropic cells. Also, ovaries of middle-aged female rats exposed to G or D have more healthy primordial and primary follicles and less atretic follicles. E treatment in the ovaries had a mostly negative effect, which is reflected by the increased number of atretic follicles in all tested classes. G and D provoked decrease in CuZnSOD and CAT activity, while E treatment increased MnSOD and decreased CuZnSOD and GSHPx activity. All the treatments increased serum estradiol and decreased testosterone levels, while D and E increased the serum progesterone level. In conclusion, soy phytoestrogens exhibited beneficial effects on pituitary-ovarian function in middle-aged female rats, as compared to estradiol.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Menopause, as the culmination of reproductive aging, is characterized by depletion of ovarian follicles, cessation of ovarian hormone production down to gonadectomy levels, and elevated levels of serum gonadotropins from the pituitary [1]. Normally, menopause is a natural process, but the progressive loss of estrogens leads to typical menopausal symptoms like hot flushes, night sweats, vaginal dryness, and/or insomnia, which may seriously compromise the quality of life in menopausal women [2]. Many women thus want to extend their reproductive life due to collateral benefits, i.e., in order to delay the uncomfortable menopause-related symptoms. To alleviate these symptoms and to protect women against estrogen deficiency-related ailments like osteoporosis, hormone replacement therapy (HRT) used to be the treatment of choice [3]. Since studies have shown that the benefits of such therapy are outweighed in the long run due to the increased risk of breast cancer, stroke, thromboembolism, and dementia [4–6], HRT is no longer being prescribed [7]. As a consequence, consumer interest in the effective and preferably safe alternative treatment options is increasing. Therefore, soy phytoestrogens such as genistein and daidzein have been proposed as a possible alternative to treat the menopausal symptoms [8, 9].
Phytoestrogens represent a group of plant-derived, biologically active compounds with a chemical structure similar to 17β-estradiol, which allows them to bind to estrogen receptors (ERs) leading to estrogenic or antiestrogenic effects [10]. Additionally, genistein and daidzein have been reported to be more estrogenic than the other phytoestrogens, with preferential binding affinity for ER beta (ERβ) over ER alpha (ERα) [10]. Interestingly, their polyphenolic structure may enable their binding to either nuclear or membrane forms of ERs, which increases the range of their estrogen-like activities to cover both the slow, genomic, and the fast, signaling-related ones [11]. Phytoestrogens may also manipulate the endogenous hormone levels by interfering with sex hormone-binding globulin (SHBG) as well as with the enzymes involved in steroid biosynthesis [12]. Finally, they may affect the numerous oxidative stress pathways/molecules which imply significant anti-aging benefits [13]. Also, it has been suggested that consumption of soy phytoestrogens as a regular part of diet improves human health by reducing cardiovascular disease risk, diabetes, and osteoporosis [14]. However, information on the potential risks of their usage is lacking, particularly in view of the fact that purified soy phytoestrogens may also act as endocrine disruptors [15]. Namely, in vivo studies have demonstrated that genistein alters the development of a female reproductive system, including delaying of estrous cycles and induction of subfertility and infertility [15]. In addition, we have previously reported that genistein had an inhibitory effect on the initial phase of folliculogenesis and, at the same time, stimulated the pituitary gonadotropic cells in immature, estrogen-deprived animals [16, 17]. Still, whether the phytoestrogens would exert their effects on the pituitary-ovarian axis in a similar estrogen low hormonal milieu of middle-aged rats, fraught with other physiological challenges, remains unknown.
Based on the literature data and our previous results, we hypothesized that the pituitary-ovarian function in middle-aged female rats would be modulated by chronic exposure to soy phytoestrogens, namely genistein and daidzein. Therefore, the precise aim of this study was to examine the effects of subcutaneous genistein or daidzein treatment on the immunofluorescence characteristics of pituitary gonadotropic and lactotropic cells, on the ovarian follicular development as well as on anti-oxidative system operativeness in the ovaries of middle-aged female Wistar rats. We also aimed to make an objective and critical parallel between these effects and the effects of estradiol, commonly used in the prevention and treatment of menopausal symptoms [18, 19].
Considering the numerous similarities of the endocrine milieu in middle-aged female rats and in menopausal women [20], we have used an ovary-intact middle-aged rat model. Furthermore, the existing literature data mostly elaborate the effects of phytoestrogens, as nutritional supplements or alternative therapy, in ovariectomized (ovx) rats, so the present study attempts to be a step forward.
Materials and methods
Animals, diet, and experimental design
Middle-aged female Wistar rats (12 month old) were housed in the unit for experimental animals at the Institute for Biological Research ‘‘Siniša Stanković’’, Belgrade, Serbia. The animals were housed in groups of two per cage, maintained on a constant photoperiod (12 h light:dark cycles) and temperature (22 ± 2 °C), with freely available food and water. All middle-aged females were in constant diestrus (as determined by daily obtained vaginal smears) for at least 2 weeks prior to the start of the experiment.
Two weeks prior to the start of the experiment, the animals were fed a soy-free diet prepared in cooperation with the Department of Animal Nutrition and Botany, Faculty of Veterinary Medicine, Belgrade, Serbia, and INSHRA PKB, Belgrade, Serbia, according to previously described procedures [21]. The soy-free diet is required because the potential presence of phytoestrogens in the soy portion of commercial non-purified diets could confound the experimental results.
Middle-aged (12 month old) female rats subcutaneously (s.c.) received 0.625 mg/kg of estradiol dipropionate (E; Galenika, Belgrade, Serbia), or 35 mg/kg of genistein (G; LC Laboratories, MA, USA), or 35 mg/kg of daidzein (D; LC Laboratories, MA, USA), every day for 4 weeks. Each of the treated groups had a corresponding control group. Genistein and daidzein were dissolved in a mixture of sterile olive oil and absolute ethanol (ratio 9:1), while their control group (CP) received this vehicle only. The applied doses of soy phytoestrogens provide the circulating levels of genistein or daidzein that are in line with the ones in the blood of people consuming greater amounts of phytoestrogens, including their use for therapeutic purposes [22]. The s.c. route of administration was chosen to precisely regulate the dosage of soy phytoestrogens and to avoid metabolism of dietary daidzein to equol (by intestinal microflora), which has stronger estrogenic properties than both G and D [23]. The applied dose of estradiol is equivalent to the dose commonly used in clinical practice for estrogen replacement in postmenopausal women and was used in previous experimental designs [19, 24]. Estradiol was dissolved in sterile olive oil, and hence females of the appropriate control group (CE) received the sterile olive oil only. The dosing volume for all groups was 5 ml/kg b.w./day. An intact control group (C) was also established. Each group consisted of six animals, while all animals were sacrificed 24 h after the last injection. Pituitaries and one of the ovaries were excised, fixed in 4 % paraformaldehyde solution for 24 h, and dehydrated in increasing concentrations of ethanol and xylene. After embedding in Histowax (Histolab Product Ab, Göteborg, Sweden), each tissue block was serially sectioned at 3 µm thickness. Pituitary sections were immunofluorescently stained, while the ovary sections were stained with hematoxylin and eosin (H&E). After decapitation, one of the ovaries from control and one from the treated females were immediately frozen using liquid nitrogen and then stored at -80 °C until the analysis of anti-oxidative enzyme activities. The tissues from control and treated females were processed contemporaneously. Blood was collected from the trunk and the sera were stored at −80 °C.
All animal procedures were in compliance with Directive 2010/63/EU on the protection of animals used for experimental and other scientific purposes and were approved by the Ethical Committee for the Use of Laboratory Animals of the Institute for Biological Research “Siniša Stanković”, University of Belgrade, Serbia.
Immunofluorescence analyses and confocal microscopy
For the evaluation of FSH, LH, and PRL intracellular protein (hormonal) content, pituitary sections were immunofluorescently stained. Prior to the staining procedure, sections were washed in PBS and pretreated for 1 h with blocking normal donkey serum (Dako, Denmark), diluted in PBS (1:10). After blocking, sections were incubated for 2 h at room temperature with: polyclonal anti-rat βFSH antibody (National Institutes of Health, Bethesda, Md., USA, 1:300); polyclonal anti-rat βLH antibody (National Institutes of Health, Bethesda, Md., USA, 1:500); polyclonal anti-rat PRL antibody (National Institutes of Health, Bethesda, Md., USA, 1:300).
Antisera were obtained from Dr. A.F. Parlow, National Hormone Peptide Program (NHPP), Harbor-UCLA Medical Centre, Carson, CA, USA. The usable dilution was determined empirically for each antiserum. After rinsing in PBS, the sections were incubated for 2 h at room temperature with a secondary antibody, Alexa Fluor 488 donkey anti-rabbit IgG (Molecular Probes, Inc., USA, 1:200). The sections were then washed in PBS five times for 5 min and cover slipped with Mowiol 4–88 (Sigma-Aldrich Co., St. Louis, MO, USA). Images were obtained using a confocal laser scanning microscope Leica TCS SP5 II Basic (Leica Microsystems CMS GmbH; Germany). An Ar-ion 488-nm laser was used for excitation of fluorescence. Analysis of confocal microscopy images was performed using the Quantify option in LAS AF Lite software (Leica Application Suite Advanced Fluorescence Lite/1.7.0 build 1240, Leica Microsystems CMS GmbH; Germany). Relative intensity of fluorescence (RIF) in the cytoplasm of pituitary gonadotropes or lactotropes was evaluated according to previously described procedures [25, 26].
Morphometry and classification of the ovarian follicles
The follicles were classified into two groups: small follicles measuring <275 µm in the largest cross section (LCS) and large follicles measuring >275 µm in the LCS. Additionally, the small follicles were divided into classes as follows: (1) primordial follicles containing an oocyte surrounded by a layer of three to six flattened pregranulosa cells; (2) primary follicles consisting of an oocyte surrounded by a single layer of cuboidal granulosa cells in part or in entirety; (3) secondary follicles containing more than one layer of cuboidal granulosa cells, with no visible antrum. The diameters of the follicles were measured (two diameters at right angles) in the LCS (that contained the oocyte nucleolus). Primordial and primary follicles that contained an oocyte with a pycnotic nucleus and/or a highly irregularly shaped nucleus were classified as atretic. Secondary and antral follicles were classified as atretic if more than one pycnotic granulosa cell was present in the granulosa layer and/or if degeneration of the oocyte was observed. The follicle number was determined by exact counts obtained from digital images of every fourth section encompassing whole cross sections of the ovary. Oocyte nuclear number was equated to follicular number. The number of corpus luteum (CL) at different phases of development (newly formed, mature, and regressive) was determined per ovary.
Stereological estimation of ovary volume
Total ovary volume (mm3), the volume of ovarian tissue phases (follicular parenchyma (V fp ), ovarian stroma (V os ), and corpus luteum (V cl ); mm3), and volume densities (%) of ovarian tissue phases determined using Cavalieri’s principle [27] with a new CAST stereological software package (VIS Visiopharm Integrator System, version 3.2.70; Visiopharm; Denmark). Every 10th section from each of the tissue blocks was analyzed as previously described [17]. Follicular parenchyma included follicles in different stages of folliculogenesis, whereas ovarian stroma contained interstitial glands, blood vessels, and ovary connective tissue. Luteal phase included corpus at different phases of development. The volume of different ovarian tissue phases was calculated using the formula:
where a (p) is the area associated with each sampling point, (\(\bar{d}\)) is the mean distance between two consecutively studied Sections (30 µm), n is the number of sections studied for each ovary, and ΣP i is the sum of points hitting a given target.The volume of the ovary (V ov ) was then estimated as: V ov = V fp + V os + V cl.
Quantification of granulosa lutein cell number and volume within mature corpus luteum (mCL)
A physical disector was used to estimate the number of granulosa lutein cells within a mature corpus luteum (mCL) in the ovaries of control and treated animals [28, 29].
The planar rotator was used as an unbiased local estimator [30] at an objective magnification of 100X, and the average granulosa lutein cell volume was measured on cells sampled by the physical dissector, applying unique counting rules (only the granulosa lutein cells with a clearly visible nucleus that appeared within the unbiased counting frame of the reference mCL and did not appear in the “look up” mCL, which were not intersected by exclusion boundaries, were analyzed).
Determination of anti-oxidative enzyme activities
Ovaries were homogenized at 0–4 °C in five volumes of ice-cold 0.25 M sucrose, 1 mM EDTA, and 0.05 M Tris–HCl buffer, pH 7.4. All procedures were performed on ice. The homogenates were centrifuged for 60 min at 105,000×g, 4 °C and the resulting supernatants were used for determining total protein concentration and enzyme activities (using a Shimadzu UV-160 spectrophotometer, Shimadzu Scientific Instruments, Kyoto, Japan). Superoxide dismutase (SOD) activities were determined by the adrenaline method [31]. One unit of activity is defined as the amount of enzyme necessary to decrease by 50 % the rate of adrenalin autooxidation at pH 10.2. Manganese SOD (MnSOD) activity was determined by incubating the samples with 8 mM KCN. Copper–zinc SOD (CuZnSOD) activity was calculated as the difference between total SOD and MnSOD activities. The activity of catalase (CAT) was determined by the rate of H2O2 disappearance measured at 240 nm, according to Claiborne [32]. One unit of CAT activity is defined as the amount of enzyme that decomposes 1 mmol H2O2 per min at 25 °C and pH 7.0. The activity of glutathione peroxidase (GSHPx) was determined by the GSH-dependent reduction of t-butyl hydroperoxide, using a modification of the assay described by Paglia and Valentine [33]. One unit of GSHPx activity is defined as the amount needed to oxidize 1 nmol NADPH per min at 25 °C and pH 7.0. Glutathione reductase (GR) activity was determined using the method of Glatzle et al. [34]. This assay is based on NADPH oxidation concomitant with GSH reduction. One unit of GR activity is defined as the oxidation of 1 nmol NADPH per min at 25 °C and pH 7.4. All enzyme activities were expressed as units per mg of protein. Soluble protein concentration was determined using the method of [35] with bovine serum albumin used as standard.
Hormonal analysis
Serum estradiol levels were measured using a electrochemiluminescent immunoassay (ECLIA) on a Roche Cobas 6000 (c501) automated analyzer (Roche Diagnostics, Mannheim, Germany) in duplicate samples within a single assay, with a coefficient of variation (CV) of 6.2 %. Analytical sensitivity of this assay is 5 pg/ml. Serum testosterone and progesterone levels were measured using a chemiluminescent microparticle immunoassay (CMIA) on an Architect i2000SR instrument (Abbott Diagnostics, Wiesbaden, Germany). Sensitivity of the testosterone immunoassay is typically less than 0.3 nmol/ml, with a CV of 20 %. Sensitivity of the progesterone immunoassay is typically less than 0.25 nmol/ml, with a CV of 6.8 %.
Statistical analysis
STATISTICA® version 6.0 (StatSoft, Inc., USA) was used for the statistical analysis. All the results were expressed as means for six animals per group ± SD. The data were tested for normality of distribution by the Kolmogorov–Smirnov test. One way analysis of variance (ANOVA) followed by a Newman–Keuls test was used for comparison of differences between the groups. A probability value of 5 % or less was considered statistically significant.
Results
Pituitary hormone producing cells
Immunofluorescence analyses of gonadotropic (FSH and LH) and lactotropic (PRL) cells
The gonadotropic (FSH and LH) cells of middle-aged females were polygonal, oval, or polyhedral in shape, with prominent, often eccentrically located nuclei, and also exerting a strong immunofluorescence signal located in the cytoplasm. Immunofluorescently labeled lactotropes (PRL cells) of middle-aged females were polygonal, elongated in shape, with spherical, centrally located nuclei surrounded by relatively small portions of pronounced immunofluorescent cytoplasm (Fig. 1a).
a Representative micrographs of immunofluorescently labeled FSH, LH, and PRL cells in the pituitary pars distalis of control (C), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. After estradiol treatment, FSH and LH cells were smaller in size and irregularly shaped, while PRL cells were more numerous. After genistein and daidzein treatment, pituitary cells were larger and with unstained parts of cytoplasm (arrows). Scale bar 50 µm. b The relative intensity of fluorescence (RIF) of FSH, LH, and PRL cells in the pituitary pars distalis of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6. *Significantly different from the corresponding control (C, CE, and CP) (P < 0.05)
After estradiol treatment, both types of gonadotropes were smaller (Fig. 1a) and the relative intensity of fluorescence (RIF) of FSH and LH cells was significantly (P < 0.05) decreased by 56.7 and 72.3 %, respectively, compared to the controls (Fig. 1b). At the same time, PRL cells were more numerous after estradiol treatment (Fig. 1a). Their shape was irregular, with a more pronounced prolactin content within their cytoplasm, which was reflected by 1.6-fold increase (P < 0.05) of RIF in comparison to the control group (Fig. 1b).
In contrast to estradiol, genistein and daidzein did not change the RIF of gonadotropic or lactotropic cells (Fig. 1b). However, changes in cell morphology were observed after treatments with both phytoestrogens. All the types of examined pituitary cells were changed in shape, with unevenly stained cytoplasm, where the immunolabeled parts of cytoplasm were separated by unstained regions, giving the cells the appearance of vacuolization (Fig. 1a).
Ovary
Histological findings
Hyperplasia and hypertrophy of the ovarian stroma appear to be a common feature of ovarian atrophy, observed in our middle-aged control rats. Pale-stained, plump stromal cells were arranged in variably sized islands and clusters. The follicles at all stages of folliculogenesis and several generations of CL were present, as well as numerous atretic follicles at different stages of degeneration (Fig. 2a). Cystic anovulatory follicles and CL were also observed (Fig. 2a). The granulosa lutein cells within mCL in the control middle-aged rat ovary were plump, polygonal, and contained moderate amounts of foamy eosinophilic cytoplasm (Fig. 3a).
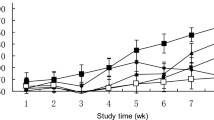
a Representative ovarian micrographs of control (C), estradiol (E)-, genistein (G)-, and daidzein (D)-treated middle-aged female rats. After estradiol treatment, ovaries were larger in size and atretic follicles were more abundant. Ovaries of larger size were observed in the groups of genistein- and daidzein-treated rats but with numerous healthy follicles and corpora lutea. (H&E) Scale bar 400 µm. b The volume densities of follicular parenchyma, ovarian stroma, and luteal phase of ovaries from control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats, as well as their ratio. The number of healthy follicles in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. The number of atretic follicles in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. The number of CL in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6. *Significantly different from the corresponding control (C, CE, and CP) (P < 0.05)
a Representative granulosa lutein cell micrographs of control (C), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. (H&E) Scale bar 10 µm. b The number and volume of granulosa lutein cells within mature corpus luteum (mCL) in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6; *Significantly different from the corresponding control (C, CE, and CP) (P < 0.05)
Light microscopic examination revealed that the ovaries of estradiol-treated rats were larger in size, with prominently dilated blood vessels compared to those of the corresponding controls (Fig. 2a). Numerous CL, follicular and luteal cysts were also present. Granulosa lutein cells within mCL were less numerous, but larger in size, with brighter cytoplasm, in comparison to the corresponding control (Fig. 3a).
Genistein-treated rats revealed numerous, healthy follicles at different stages of folliculogenesis and considerably fewer follicular and CL cysts, without observable changes at the level of ovary size. Granulosa lutein cells within mCL were similar in respect to size and appearance to those seen in control ovaries (Fig. 3a). The ovaries of daidzein-treated rats were larger than those of the corresponding controls and were characterized by prominently dilated blood vessels (Fig. 2a). Daidzein treatment changed the healthy to cystic follicle ratio in favor of healthy follicles, as compared to corresponding controls. In addition, light microscopy examination revealed slightly enlightened granulosa lutein cells within mCL after daidzein treatment (Fig. 3a).
Stereological measurements
The ovary volume of middle-aged female rats treated with estradiol was significantly (P < 0.05; Fig. 4a) increased by 7.1 % compared to the corresponding control. Follicular parenchyma volume remained unchanged (Fig. 4b), whereas the volume of ovarian stroma decreased by 5.7 % (P < 0.05; Fig. 4c). The estradiol treatment led to an increase in the CL volume by 25.9 % (P < 0.05; Fig. 4d) in comparison with the corresponding control. The volume density of follicular parenchyma remained unchanged, whereas volume densities of ovarian stroma and CL increased by 18.7 % (P < 0.05) and 8.9 % (P < 0.05), respectively (Fig. 2b).
The average volume of a ovaries, b follicular parenchyma, c ovarian stroma, and d corpus luteum of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6. *Significantly different from corresponding control (C, CE, and CP) (P < 0.05)
Genistein treatment did not change the ovary volume as well as CL volume (Fig. 4a, d). The volume of follicular parenchyma was 38.3 % greater (P < 0.05; Fig. 4b), whereas ovarian stroma volume was 9.9 % smaller (P < 0.05; Fig. 4c) in comparison to the corresponding control values. Treatment with daidzein induced a significant increase in the ovary volume (by 4.1 %; P < 0.05; Fig. 4a) and follicular parenchyma volume (by 34.6 %; P < 0.05; Fig. 4b) compared to the corresponding control values.
Volume density of follicular parenchyma after genistein and daidzein treatment increased (P < 0.05) by 36.4 and 29.1 %, respectively (Fig. 2b). This was accompanied by a decrease in the volume density of ovarian stroma after both treatments. Thus, genistein induced a 21.1 % decrease (P < 0.05), and daidzein caused a 25.2 % decrease (P < 0.05) in comparison with the corresponding control values (Fig. 2b).
Follicular number
Estradiol induced a significant decrease in the number of healthy (by 37.4 %; P < 0.05) and atretic (by 20.3 %; P < 0.05) small growing (secondary) follicles. In addition, estradiol led to a significant increase in the number of atretic primordial (by 89.9 %; P < 0.05), primary (by 86.2 %; P < 0.05) and antral follicles (by 71.7; P < 0.05), when compared to the corresponding control values (Fig. 2b). After estradiol treatment, the number of mature and regressive CL was increased 1.4-fold (P < 0.05) and 4.1-fold (P < 0.05), respectively. Therefore, the total number of healthy CL was significantly higher (91.4 %; P < 0.05) in comparison with the control values (Fig. 2b). Estradiol led to a decrease in the number of granulosa lutein cells within mCL (by 22.4 %; P < 0.05), accompanied by a 3.2-fold (P < 0.05) increase in the cell volume (Fig. 3b).
The number of non-growing primordial follicles after genistein treatment was 2.4-fold and after daidzein treatment 3.3-fold greater (P < 0.05) than for the corresponding control group. In addition, the number of primary follicles was also significantly greater (P < 0.05) after genistein and daidzein treatment (1.2-fold and 1.6-fold, respectively; Fig. 2b). The number of atretic primordial follicles was unchained after both treatments (Fig. 2b). However, the number of atretic primary follicles after genistein and daidzein treatment decreased (P < 0.05) by 32.6 and 23.5 %, respectively. The number of healthy and atretic secondary follicles, as well as healthy antral follicles remained unchanged, while the number of atretic antral follicles was reduced after both treatments. Thus, genistein induced a 22.6 % decrease (P < 0.05), and daidzein caused a 32.3 % decrease (P < 0.05), when compared to the corresponding control values (Fig. 2b). Genistein treatment did not change the number of individual classes of CL, or their total number. In contrast, daidzein increased the number of mCL (by 86.8 %; P < 0.05), which resulted in an increase in their total number (by 33.7 %; P < 0.05; Fig. 2b). Genistein and daidzein did not cause changes in the number or volume of granulosa lutein cells within mCL (Fig. 3b).
Antioxidant enzyme activities
Higher MnSOD (P < 0.05; Fig. 5a) and lower GSHPx activity (P < 0.05; Fig. 5b) were noted in the ovaries of estradiol-treated female rats. However, estradiol had no significant effect on CuZnSOD, CAT, and GR activity, when compared to the corresponding control values.
a The changes in CuZnSOD, MnSOD, and CAT anti-oxidative enzyme activity in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6. *Significantly different from the corresponding control (C, CE, and CP) (P < 0.05). b The changes in GSHPx and GR anti-oxidative enzyme activity in the ovaries of control (C, CE, and CP), estradiol-(E), genistein-(G), and daidzein-(D) treated middle-aged female rats. All values are given as mean ± SD; n = 6. *Significantly different from the corresponding control (C, CE, and CP) (P < 0.05)
Both genistein and daidzein treatments significantly decreased CuZnSOD (P < 0.05; Fig. 5a) and CAT (P < 0.05; Fig. 5a) activity in the ovaries of middle-aged females, but the difference was more pronounced after daidzein treatment. On the other hand, there were no significant changes in MnSOD, GSHPx, and GR activity in comparison with the corresponding control values.
Serum hormone analysis
The serum hormone levels of control and treated animals and the significance of the value differences are summarized in Table 1.
The applied estradiol induced a 510-fold (P < 0.05) elevation in serum estradiol concentration when compared to the corresponding control. Furthermore, estradiol led to an increase in serum progesterone concentration (1.3-fold; P < 0.05), followed by a 36.1 % (P < 0.05) decrease in testosterone serum levels.
Genistein treatment increased the serum estradiol level by 20.3 % (P < 0.05) and decreased the testosterone concentration by 42.8 % (P < 0.05), without affecting the progesterone serum level. After daidzein treatment, serum estradiol and progesterone concentrations increased by 51.6 % (P < 0.05) and 34.3 % (P < 0.05) respectively, while testosterone was reduced by 48.9 % (P < 0.05) compared to the corresponding control values.
Discussion
Recent years have witnessed a growing research focus on soy phytoestrogens, claimed by pharmaceutical companies to be a potential alternative to the classic hormone replacement therapy. As a consequence, many women aged 45–60 years have been exposed to high doses of phytoestrogens in purified form for the first time in their lives [36]. Although no harmful effects of soy phytoestrogens have been described so far, if consumption occurs as a regular part of diet (in the form of soy flour or crude soy extracts), the effects of isolated and high-dosed soy phytoestrogens could be controversial [37–39]. Therefore, the aim of this study was to assess the effects of genistein and daidzein on the histological, hormonal, and functional parameters of pituitary-ovarian axis in middle-aged female rats, and to compare them with the effects of estradiol, commonly used in the prevention and treatment of menopausal symptoms.
Considering the fact that gonadotropin levels represent an established indirect marker of follicular activity and their elevation is often associated with the development of menopause [1, 40], we performed a morphological and immunofluorescent characterization of estrogen-sensitive, gonadotropic as well as lactotropic pituitary cells in middle-aged female rats. Namely, analysis of the relative intensity of fluorescent signal, which quantifies intracellular protein content (the specific hormonal storage), showed that neither genistein nor daidzein changed the tested parameter. However, alterations in cell morphology were observed after treatment with both phytoestrogens. In fact, gonadotropic and lactotropic pituitary cells were changed in shape, with unevenly stained cytoplasms which gave cells the appearance of vacuolization. Considering the presence of various forms of ERs (with the serious potential of phytoestrogen sensitivity) in the pituitary gonadotropic and lactotropic cells, not only in the nucleus and cytoplasm but also in the membrane of rough endoplasmic reticulum and secretory vesicles [41], and keeping in mind that vesicular trafficking crucially defines cell mechanical status [12, 42], we can assume that the observed changes in cell morphology may be mediated by both genomic and non-genomic pathways.
It has been reported that during the female reproductive life primordial follicles are continuously recruited to grow into developing follicles, a few of which are selected to mature until ovulation, while the vast majority undergo atresia at various developmental stages [43]. In fact, when the available pool of primordial follicles is depleted, female reproductive function ceases and women enter menopause and to the menopausal syndrome and diseases associated with aging [1, 40]. Additionally, oxidative stress plays an integral part of the ovary aging and results from the overproduction of free radicals such as the reactive oxygen species (ROS) [44]. Namely, ROS have an important role in modulating the entire spectrum of female reproductive functions including oocyte maturation, ovarian steroidogenesis, CL progesterone production, and luteolysis [45], and the processes inter alia being driven by the appropriate balance between free radical species generation and antioxidant mechanism activation. By contrast, overabundance of ROS disrupts the ovarian niche and induces follicular atresia, which is observed during the menopausal period [44]. Therefore, in the next step within our experiment, we examined the follicular differentiation and anti-oxidative enzyme activity in the middle-aged rat ovary. A significant finding of this study was that ovaries from middle-aged female rats exposed to genistein or daidzein had more healthy primordial and primary follicles and less atretic follicles. Our study revealed that genistein and daidzein increased the ovarian follicular reserve in middle-aged rats by stepping down the transition from primordial to primary follicle and by depressing follicular atresia. The mechanisms may be explained by the suppression of cellular proliferation through the inhibition of key steps in the signal transduction pathways [46] and cell cycle progression [47, 48], indicating that genistein and daidzein may play a role in suppressing the process of follicular development by scavenging and suppressing intracellular reactive oxygen intermediates. Therefore, we presume that phytoestrogens may protect follicles from atresia due to the decrease of oxidative stress in the ovary. This assumption has gained importance through our results. We observed that genistein and daidzein significantly decreased the activities of CuZnSOD (superoxide dismutase that reduces the superoxide anion radicals to H2O2) and CAT (catalase that converts H2O2 into water), indicating that the soy phytoestrogens may decrease the pool of ROS in the ovary directly due to their polyphenolic structures. Namely, genistein and daidzein act as free radical scavengers, while their structures at least partly enable the antioxidant properties. The hydroxyl group at position 4′ is the active center for scavenging peroxyl radicals, and was shown to be crucial in protecting against superoxide anion and H2O2 formation [12, 49]. Therefore, the observed decreases in antioxidant enzyme activities in the ovary caused by phytoestrogens supposedly could highlight their direct antioxidant potential. Moreover, our results indicated that daidzein exhibits stronger anti-oxidative potential than genistein, although genistein owns one hydroxyl group more (in general, the more hydroxyl group substitutions, the stronger the free radical scavenging activity). A possible explanation might be the effective metabolic conversion of daidzein to 8-hydroxydaidzein, which is the most potent free radical scavenger, in parallel with daidzein increased tissue penetrability due to its more pronounced hydrophobicity [12, 49]. Finally, daidzein has been shown to induce de novo synthesis of mitochondria [50], which may reduce oxidative stress and prevent cell apoptosis, potentially protecting the follicles from atresia. Also, in our experimental conditions both phytoestrogens reduced the number of antral atretic follicles and ovarian cysts, which might also be the consequence of anti-oxidative stress reduction. Alternatively, it may be that the molecular effects of phytoestrogens on depressing follicular atresia and development of follicular cysts occur through estrogen receptor mediated pathways [51]. Due to the preservation of ovarian healthy follicles function in the middle-aged female rats, phytoestrogens increased the volume density of follicular parenchyma and reduced the volume density of ovarian stroma, which in our study resulted in an increase in estradiol as well as reduction of the testosterone concentration in serum. However, only rats in the daidzein-treated group exhibited a larger number and volume of mCL than those in the control group. This observation suggested that daidzein may affect the conservation of CL, which due to its secretory activity increased the level of progesterone in serum.
Our results clearly show that treatment with estradiol implies a number of negative effects on the rat’s pituitary-ovarian axis. Namely, they confirmed the already existing evidence on the harmful effects of estradiol-based HRT. As expected, chronic administration of estradiol caused an increase of estradiol in serum, which inhibited pituitary gonadotropic cells in our study, causing an adverse effect on the ovarian function. At the same time, we showed that estradiol-stimulated PRL cells, supposedly through the reported changes in the concentration of bFGF (basic Fibroblast Growth Factor) and VEGF (Vascular Endothelial Growth Factor), increased sensitivity to TRH (Thyrotropin-releasing hormone) and reduced sensitivity to dopamine [52], all of which could result in prolactinoma development [53].
In the present study, estradiol also had an extremely negative effect on the ovaries of middle-aged females, evident in the increased number of atretic follicles in all tested classes. Estradiol is able to increase follicular atresia either indirectly, through the inhibition of gonadotropins [54], or directly through the increase of oxidative stress, as indicated in our results obtained by determining the anti-oxidative enzyme activity. Because of its maturing effect [55], through the PRL synthesis and secretion affirmation, estradiol increased not only the number, but also the activity of mCL, which resulted in an increase of progesterone concentration in serum. At the same time, the number of regressive corpora lutea was also increased, causing an increase in the volume of the ovary.
In summary, we have observed that in our experimental model: (1) genistein and daidzein did not change the hormonal content in gonadotropic and lactotropic pituitary cells and thus exhibited a positive effect on the maintenance of ovarian function, unlike estradiol, which due to the inhibition of gonadotropic cells induced an atretic process in the ovaries, while due to the stimulation of lactotropic cells could also increase the risk of pituitary prolactinoma development; (2) both the examined phytoestrogens can step down follicular development, significantly improving the ovarian follicular reserve. Furthermore, genistein and daidzein affected the follicle survival by inhibiting atresia, while estradiol caused acceleration of the atretic process. Bearing in mind that menopause is caused by reduced ovarian function, our data suggest that genistein and daidzein may prolong the lifespan of the ovary in aging women. Despite the beneficial effects of genistein and daidzein observed in our study, it is very important to rule out some potential side effects of purified soy phytoestrogens including cell proliferation and increased carcinogenesis risk, which leaves this field of investigation open.
References
M. Guida, F. Zullo, B. Buonomo, M.L. Marra, V. Palatucci, R. Pascale, F. Visconti, G. Guerra, M. Spinelli, A. Di Spiezio Sardo, Estrogens and neuropeptides in postmenopausal women, un update. Transl. Med. UniSa 3, 25–41 (2012)
A. Cagnacci, M. Cannoletta, F. Palma, R. Zanin, A. Xholli, A. Volpe, Menopausal symptoms and risk factors for cardiovascular disease in postmenopause. Climacteric 15, 157–162 (2012)
A.J. Welton, M.R. Vickers, J. Kim, D. Ford, B.A. Lawton, A.H. Maclennan, S.K. Meredith, J. Martin, T.W. Meade, Health related quality of life after combined hormone replacement therapy randomised controlled trial. BMJ 337, a1190 (2008)
J.E. Rossouw, G.L. Anderson, R.L. Prentice, A.Z. LaCroix, C. Kooperberg, M.L. Stefanick, R.D. Jackson, S.A. Beresford, B.V. Howard, K.C. Johnson, J.M. Kotchen, J. Ockene, Writing Group for the Women’s Health Initiative Investigators, Risks and benefits of estrogen plus progestin in healthy postmenopausal women, principal results. From the Women’s Health Initiative randomized controlled trial. JAMA 288, 321–333 (2002)
L.L. Schierbeck, L. Rejnmark, C.L. Tofteng, L. Stilgren, P. Eiken, L. Mosekilde, L. Køber, J.E. Jensen, Effect of hormone replacement therapy on cardiovascular events in recently postmenopausal women, randomised trial. BMJ 345, e6409 (2012)
J.E. Manson, R.T. Chlebowski, M.L. Stefanick, A.K. Aragaki, J.E. Rossouw, Anderson G. PrenticeRL, B.V. Howard, C.A. Thomson, A.Z. LaCroix, J. Wactawski-Wende, R.D. Jackson, M. Limacher, K.L. Margolis, S. Wassertheil-Smoller, S.A. Beresford, J.A. Cauley, C.B. Eaton, M. Gass, J. Hsia, K.C. Johnson, C. Kooperberg, L.H. Kuller, C.E. Lewis, S. Liu, L.W. Martin, J.K. Ockene, M.J. O’Sullivan, L.H. Powell, M.S. Simon et al., Menopausal hormone therapy and health outcomes during theintervention and extended poststopping phases of the Women’s HealthInitiative randomized trials. JAMA 310, 1353–1368 (2013)
A. Lagro-Janssen, M.W. Knufing, L. Schreurs, C. van Weel, Significant fall in hormone replacement therapy prescription in general practice. Fam. Pract. 27, 424–429 (2010)
M. Bedell, The pros and cons of plant estrogens for menopause. J. Steroid Biochem. Mol. Biol. 139, 225–236 (2014)
V.S. Lagari, S. Levis, Phytoestrogens for menopausal bone loss and climacteric symptoms. J. Steroid Biochem. Mol. Biol. 139, 294–301 (2014)
G.G. Kuiper, J.G. Lemmen, B. Carlsson, J.C. Corton, S.H. Safe, P.T. Van Der Saag, B. Van Der Burg, J. Gustafsson, Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor β. Endocrinology 139, 4252–4263 (1998)
V. Ajdžanović, I. Medigović, J. Zivanović, M. Mojić, V. Milošević, Membrane steroid receptor-mediated action of soy isoflavones, tip of the iceberg. J. Membr. Biol. 248, 1–6 (2015)
V.Z. Ajdžanović, I.M. Medigović, J.B. Pantelić, V.L.J. Milošević, Soy isoflavones and cellular mechanics. J. Bioenerg. Biomembr. 46, 99–107 (2014)
L. Pilšáková, I. Riečanský, F. Jagla, The physiological actions of isoflavone phytoestrogens. Physiol. Res. 59, 651–664 (2010)
E. Poluzzi, C. Piccinni, E. Raschi, A. Rampa, M. Recanatini, P.F. De, Phytoestrogens in postmenopause, the state of the art from a chemical, pharmacological and regulatory perspective. Curr. Med. Chem. 21, 417–436 (2014)
W.N. Jefferson, E. Padilla-Banks, R.R. Newbold, Disruption of the developing female reproductive system by phytoestrogens, genistein as an example. Mol. Nutr. Food Res. 51, 832–844 (2007)
I. Medigović, M. Manojlović-Stojanoski, S. Trifunović, N. Ristić, V. Milošević, D. Zikić, N. Nestorović, Effects of genistein on gonadotropic cells in immature female rats. Acta Histochem. 114, 270–275 (2012)
I. Medigović, N. Ristić, S. Trifunović, M. Manojlović-Stojanoski, V. Milošević, D. Zikić, N. Nestorović, Genistein affects ovarian folliculogenesis, a stereological study. Microsc. Res. Tech. 75, 1691–1699 (2012)
J. Hsia, R.D. Langer, J.E. Manson, L. Kuller, K.C. Johnson, S.L. Hendrix, M. Pettinger, S.R. Heckbert, N. Greep, S. Crawford, C.B. Eaton, J.B. Kostis, P. Caralis, R. Prentice, Conjugated equine estrogens and coronary heart disease: the Women’s Health Initiative. Women’s Health Initiative Investigators. Arch. Intern. Med. 166, 357–365 (2006)
M.M. Abdel-Dayem, M.S. Elgendy, Effects of chronic estradiol treatment on the thyroid gland structure and function of ovariectomized rats. BMC Res. Notes 30, 173 (2009)
G. Neal-Perry, E. Nejat, C. Dicken, The neuroendocrine physiology of female reproductive aging, an update. Maturitas 67, 34–38 (2010)
I. Medigović, N. Ristić, J. Živanović, B. Šošić-Jurjević, B. Filipović, V. Milošević, N. Nestorović, Diosgenin does not express estrogenic activity, a uterotrophic assay. Can. J. Physiol. Pharmacol. 92, 292–298 (2014)
D. Doerge, D. Sheehan, Goitrogenic and estrogenic activity of soy isoflavones. Environ. Health Perspect. 110, 349–353 (2002)
J.H. Mitchell, P.T. Gardner, D.B. McPhail, P.C. Morrice, A.R. Collins, G.G. Duthie, Antioxidant efficacy of phytoestrogens in chemical and biological model systems. Arch. Biochem. Biophys. 360, 142–148 (1998)
B. Sosic-Jurjevic, B. Filipovic, V. Milosevic, N. Nestorovic, M. Manojlovic-Stojanoski, B. Brkic, M. Sekulic, Chronic estradiol exposure modulates thyroid structure and decreases T4 and T3 serum levels in middle-aged female rats. Horm. Res. 63, 48–54 (2005)
S. Trifunović, M. Manojlović-Stojanoski, V. Ajdžanović, N. Nestorović, N. Ristić, I. Medigović, V. Milošević, Effects of genistein on stereological and hormonal characteristics of the pituitary somatotrophs in rats. Endocrine 47, 869–877 (2014)
M. Miler, B. Šošić-Jurjević, N. Nestorović, N. Ristić, I. Medigović, S. Savin, V. Milošević, Morphological and functional changes in pituitary-thyroid axis following prolonged exposure of female rats to constant light. J. Morphol. 275, 1161–1172 (2014)
H.J. Gundersen, E.B. Jensen, The efficiency of systematic sampling in stereology and its prediction. J. Microsc. 147, 229–263 (1987)
K.A. Dorph-Petersen, J.R. Nyengaard, H.J.G. Gundersen, Tissue shrinkage and unbiased stereological estimation of particle number and size. J. Microsc. 204, 232–246 (2001)
H.J. Gundersen, Stereology of arbitrary particles. A review of unbiased number and size estimators and the presentation of some new ones, in memory of William R. Thompson. J. Microsc. 143, 3–45 (1986)
M. Manojlović-Stojanoski, N. Nestorović, N. Ristić, S. Trifunović, B. Filipović, B. Šošić-Jurjević, M. Sekulić, Unbiased stereological estimation of the rat fetal pituitary volume and of the total number and volume of TSH cells after maternal dexamethasone application. Microsc. Res. Tech. 73, 1077–1085 (2010)
H.P. Misra, I. Fridovich, The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 247, 3170–3175 (1972)
A. Claiborne, Assay for catalase in handbook of methods for oxygen radical research (CRC Press, Boca Raton, 1985), pp. 283–284
D.E. Paglia, W.N. Valentine, Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J. Lab. Clin. Med. 70, 74–77 (1967)
D. Glatzle, J.P. Vuilleumier, F. Weber, K. Decker, Glutathione reductase test with whole blood a convenient procedure for the assessment of the riboflavin status in humans. Experientia 30, 665–668 (1974)
O.H. Lowry, N.L. Rosebrough, A.L. Farr, R.I. Randall, Protein measurement with Folin phenol reagent. J. Biol. Chem. 193, 265–275 (1951)
A. Ferrari, Soy extract phytoestrogens with high dose of isoflavones for menopausal symptoms. J. Obstet. Gynaecol. Res. 35, 1083–1090 (2009)
C.D. Allred, K.F. Allred, Y.H. Ju, T.S. Goeppinger, D.R. Doerge, W.G. Helferich, Soy processing influences growth of estrogen-dependent breast cancer tumors. Carcinogenesis 25, 1649–1657 (2004)
M. Du, X. Yang, J.A. Hartman, P.S. Cooke, D.R. Doerge, Y.H. Ju, W.G. Helferich, Low-dose dietary genistein negates the therapeutic effect of tamoxifen in athymic nude mice. Carcinogenesis 33, 895–901 (2012)
Y. Liu, L. Hilakivi-Clarke, Y. Zhang, X. Wang, Y.X. Pan, J. Xuan, S.C. Fleck, D.R. Doerge, W.G. Helferich, Isoflavones in soy flour diet have different effects on whole-genome expression patterns than purified isoflavone mix in human MCF-7 breast tumors in ovariectomized athymic nude mice. Mol. Nutr. Food Res. (2015). doi:10.1002/mnfr.201500028
C.R. Anzalone, L.S. Hong, J.K. Lu, P.S. LaPolt, Influences of age and ovarian follicular reserve on estrous cycle patterns, ovulation, and hormone secretion in the Long-Evans rat. Biol. Reprod. 64, 1056–1062 (2001)
M. González, R. Reyes, C. Damas, R. Alonso, A.R. Bello, Estrogen receptor alpha and beta in female rat pituitary cells, an immunochemical study. Gen. Comp. Endocrinol. 155, 857–868 (2008)
A. Asnacios, O. Hamant, The mechanics behind cell polarity. Trends Cell Biol. 22, 584–591 (2012)
E.A. McGee, A.J. Hsueh, Initial and cyclic recruitment of ovarian follicles. Endocr. Rev. 21, 200–214 (2000)
A. Agarwal, A. Aponte-Mellado, B.J. Premkumar, A. Shaman, S. Gupta, The effects of oxidative stress on female reproduction, a review. Reprod. Biol. Endocrinol. 10, 49 (2012)
S.B. Doshi, A. Agarwal, The role of oxidative stress in menopause. J. Midlife Health. 4, 140–146 (2013)
S.D. Wang, B.C. Chen, S.T. Kao, C.J. Liu, C.C. Yeh, Genistein inhibits tumor invasion by suppressing multiple signal transduction pathways in human hepatocellular carcinoma cells. BMC Complement. Altern. Med. 14, 26 (2014)
Y.H. Choi, W.H. Lee, K.Y. Park, L. Zhang, p53-independent induction of p21 (WAF1/CIP1), reduction of cyclin B1 and G2/M arrest by the isoflavone genistein in human prostate carcinoma cells. Jpn. J. Cancer Res. 91(2), 164–173 (2000)
M. Yamasaki, S. Fujita, E. Ishiyama, A. Mukai, H. Madhyastha, Y. Sakakibara, M. Suiko, K. Hatakeyama, T. Nemoto, K. Morishita, H. Kataoka, H. Tsubouchi, K. Nishiyama, Soy-derived isoflavones inhibit the growth of adult T-cell leukemia cells in vitro and in vivo. Cancer Sci. 98, 1740–1746 (2007)
G. Rimbach, S. De Pascual-Teresa, B.A. Ewins, S. Matsugo, Y. Uchida, A.M. Minihane, R. Turner, K. VafeiAdou, P.D. Weinberg, Antioxidant and free radical scavenging activity of isoflavone metabolites. Xenobiotica 33, 913–925 (2003)
K.A. Rasbach, R.G. Schnellmann, Isoflavones promote mitochondrial biogenesis. J. Pharmacol. Exp. Ther. 325, 536–543 (2008)
A.E. Drummond, P.J. Fuller, Ovarian actions of estrogen receptor-β, an update. Semin. Reprod. Med. 30, 32–38 (2012)
C. Spuch, Y. Diz-Chaves, D. Pérez-Tilve, F. Mallo, Fibroblast growth factor-2 and epidermal growth factor modulate prolactin responses to TRH and dopamine in primary cultures. Endocrine 29, 317–324 (2006)
A.P. Heaney, M. Fernando, S. Melmed, Functional role of estrogen in pituitary tumor pathogenesis. J. Clin. Invest. 109, 277–283 (2002)
V. Milošević, V. Ajdžanović, Pituitary hormone-producing cells after estradiol application in rat models of menopause. Serb. J. Exp. Clin. Res. 15, 115–120 (2014)
G.D. Niswender, J.L. Juengel, P.J. Silva, M.K. Rollyson, E.W. McIntush, Mechanisms controlling the function and life span of the corpus luteum. Physiol. Rev. 80, 1–29 (2000)
Acknowledgments
This work was supported by the Ministry of Education, Science and Technological Development of the Republic of Serbia, Grant Number 173009. The authors wish to express their sincere gratitude to Olympus d.o.o. Belgrade, Serbia, for technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Medigović, I.M., Živanović, J.B., Ajdžanović, V.Z. et al. Effects of soy phytoestrogens on pituitary-ovarian function in middle-aged female rats. Endocrine 50, 764–776 (2015). https://doi.org/10.1007/s12020-015-0691-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0691-x