Abstract
Glucagon-like peptide-1 (GLP-1) stimulates insulin secretion and inhibits glucagon secretion in the pancreatic islets of Langerhans under hyperglycaemia. In type 2 diabetes (T2DM), GLP-1 improves glycaemic control without a hypoglycaemia risk. GLP-1 receptors have also been found in extra-pancreatic tissues, e.g., the cardiovascular system, the gastrointestinal system, and the central nervous system. Since cardiovascular comorbidities and degenerative neurological changes are associated with T2DM, the interest in the extrapancreatic effects of GLP-1 has increased. GLP-1-based therapies with either GLP-1 receptor agonists (GLP-1 RA) or DPP-4 inhibitors (that delay the degradation of endogenous GLP-1) have become widely used therapeutic options in T2DM. In clinical studies, GLP-1 RA have demonstrated a significant lowering of blood pressure that is independent of body weight changes. Preclinical data and small short-term studies with GLP-1 and GLP-1 RA have shown cardioprotective effects in ischaemia models. GLP-1 as well as a treatment with GLP-1 RA also induces a stable body weight loss by affecting GLP-1 signaling in the hypothalamus and by slowing gastric emptying. Regarding neuroprotective actions in degenerative neurological disease models for Parkinson’s- or Alzheimer’s disease or neurovascular complications like stroke, animal studies have shown positive results. In this article, a summary of the extrapancreatic effects of GLP-1 and GLP-1-based therapies is presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes (T2DM) incidence is increasing at a fast rate with 382 million people affected in 2013 and expected 592 million patients by 2035 [1]. Poor metabolic control is associated with micro- and macrovascular complications and T2DM, and cardiovascular mortality is responsible for the diminished life expectancy in the majority of patients with T2DM [2, 3]. Apart from the glycaemic defects, T2DM is frequently associated with hypertension, dyslipidaemia, and obesity [4].
Efficacious and safe therapies are needed that avoid hypoglycaemia and further body weight gain and also facilitate treatment adherence. In this respect, incretin-based therapies with receptor agonists for glucagon-like peptide-1 (GLP-1 RA) as injectable agents and DPP-4 inhibitors (dipeptidyl peptidase-IV inhibitors) as oral agents have been an important addition to the treatment possibilities. An ideal antidiabetic therapy would also have a favorable impact on the above-mentioned comorbidities found in T2DM as well as on cardiovascular outcomes.
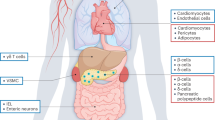
The incretin hormone glucagon-like peptide-1 (GLP-1) stimulates post-prandial insulin secretion under conditions of hyperglycaemia [5, 6]. It further inhibits glucagon secretion, increases insulin biosynthesis, and increases beta-cell function and -mass in rodent models [5, 6]. The GLP-1 receptor (GLP-1 R) is also widely expressed in extra-pancreatic tissues: the gastrointestinal tract, the brain, heart, kidney, and the lung [6]. Its tissue-specific functions are not completely characterized yet.
Native GLP-1 has been shown to have favorable effects on the gastrointestinal system, the cardiovascular system and the central nervous system (CNS) in various animal- and also human studies. Native GLP-1, however, is not practical for therapeutic use due to its short half-life caused by ubiquitous, fast, and effective in vivo degradation by the enzyme dipeptidyl peptidase-4 (DPP-4) [7, 8]. For this reason, GLP-1 RA and DPP-4 inhibitors have been introduced as two distinct treatment options for T2DM utilizing GLP-1 physiology and pharmacology [9].
The research area of the extra-pancreatic effects of the GLP-1 is busy and advancing in order to understand its non-glycaemic actions and develop novel strategies to utilize non-glycaemic effects with potential benefits in T2DM therapy. This article summarizes pre-clinical and clinical data, showing the effects of GLP-1-based therapy on the cardiovascular system, gastrointestinal system, and CNS. The search strategy for this review was using Embase, Medline, and Scopus screening for the terms “GLP-1”, “GLP-1 RA”, “DPP-4 inhibitor”, “extrapancreatic effects”, “cardiovascular effects”, “gastrointestinal”, “neuroprotection”, “inflammation”, “kidney”, and “liver”. Additional information from clinical trials was obtained from the clinical study register “ClinicalTrials.gov”. A summary of the effects and studies discussed within this review are shown in Table 1 [10–12].
Effects on the gastrointestinal system
Gastric emptying and gastrointestinal transit time
Pharmacological doses of GLP-1 slow gastric emptying in a dose dependent manner, causing sensations of fullness up to transient nausea and vomiting [13, 14]. Since therapy with GLP-1 RA raises levels of a GLP-1 receptor ligand ~8 to 10-fold, treatment with these agents is often associated with transient nausea and vomiting. This side effect is more pronounced with short acting GLP-1 RA that show distinct peak- and trough levels during therapy [15]. In rats, the effect of liraglutide (with a t 1/2 of 13 h in vivo) on gastric emptying appears to be transient, in contrast to that of exenatide (with a t 1/2 of 2.5–3 h in vivo) [16, 17]. The gastric-emptying effect observed with liraglutide at day 1 disappeared by day 14. In contrast, the gastric-emptying effect observed with exenatide in this study was still evident at the 14-day time-point [16, 17]. The different effects observed for liraglutide and exenatide are likely due to the different pharmacokinetic profiles of these agents and desensitization or tachyphylaxis. Consistent with this hypothesis is that gastric emptying also appears to be less pronounced with exenatide once weekly compared with exenatide twice daily [18] while lixisenatide (a short-acting GLP-1 RA t 1/2 of 3 h) provides sustained inhibition of gastric emptying [19]. As weight loss with short-acting GLP-1 RAs is not greater than with longer acting ones, inhibition of gastric emptying may also not represent the main mechanism by which GLP-1RAs reduce body weight [11].
Whether the gastrointestinal effects combined with the weight-loosing ones are direct effects of GLP-1R stimulation within the gastrointestinal system or are mediated by a mechanism in the central nervous system has not been fully elucidated yet [20]. In preclinical models GLP-1, RA-associated nausea (in accordance with the conditioned taste avoidance model, CTA model) was accompanied by diminished food intake [20]. In a clinical study with obese non-diabetic subjects, weight loss with liraglutide was greater in participants who had reported nausea or vomiting (9.2 kg) compared to those who did not report nausea or vomiting (9.2 vs. 6.3 kg, respectively) [21]. Clinical data have shown that the incidence of gastrointestinal adverse events may increase weight loss achieved with GLP-1 RA therapy, but this is probably not the most important and paramount mechanism, because treatment with GLP-1 RA without causing symptoms of nausea and vomiting still is associated with a significant weight loss in these subjects [21, 22]. In summary, while the gastrointestinal effects of GLP-1 RAs may contribute to the weight loss observed with therapy, they do not appear to be the main mechanism responsible. Such gastrointestinal effects may play a more important role in the reduction in postprandial hyperglycaemia observed with GLP-1RA therapy [11, 15, 23].
DPP-4 inhibitors that lead to much lower levels of GLP-1 concentrations, do not cause the above-mentioned gastrointestinal side effects and do not lead to an increase in gastrointestinal transit time [24, 25].
Effects on the brain (CNS)
Weight loss and central nervous effects
Receptors for GLP-1 are expressed in various brain regions, predominantly in the hypothalamus and brain stem, where the nuclei for the regulation of food intake and satiety are located. GLP-1 is able to cross the blood brain barrier; intracerebroventricular GLP-1 mediates satiety and inhibits food intake [26, 27]. Animal studies showed that the exendin-4-based GLP-1 RA exenatide and lixisenatide as well as the human GLP-1 analog liraglutide are also able to cross the blood brain barrier after peripheral administration [28–30]. The peripheral administration however has been shown to suppress food intake via vagus nerve-dependent and -independent pathways that result in direct CNS GLP-1 receptor activation [31].
Weight loss with GLP-1 RAs
With the exception of albiglutide, all GLP-1 RA tested in clinical studies so far have led to a significant loss of body weight in the magnitude of 1–3 kg in studies lasting for half a year [10, 12, 23, 32–38]. Albiglutide, a large fusion protein of two GLP-1 molecules with albumin designed for once weekly dosing appears to have less of an effect on body weight than other GLP-1 RAs, probably by not crossing the blood brain barrier due to its molecular size and charge [15]. However, dulaglutide, which is also a large fusion protein, has been reported to result in similar weight loss to exenatide, and therefore, the reduced effect of albiglutide may simply be due to reduced GLP-1R stimulation [12].
In subjects without diabetes and obesity, clinical studies are ongoing or have been performed with GLP-1 RA to observe the effects on body weight [39–43]. It is important to note, that GLP-1 RA do not have approval for this indication. In one study, liraglutide at high doses of either 2.4 or 3.0 mg once daily was significantly more effective than the lipase inhibitor orlistat or placebo in allowing weight loss in a study population with a BMI ≥30 and ≤40 kg/m2. The weight losses with 2.4 and 3.0 mg liraglutide were 6.3 and 7.2 kg for these doses, respectively, whereas patients on orlistat lost 4.1 kg and on placebo 2.8 kg [39]. Subjects treated with the maximal dose of 3.0 mg liraglutide had a weight loss of 10.3 ± 7.1 kg after 2 years [40]. In studies with exenatide at the doses used for diabetes therapy, body weight loss ranged 3.0–6.0 kg after 24 weeks in similar subjects with obesity, women with polycystic ovary syndrome (PCOS) or obese adolescents [41–43].
DPP-4 inhibitors in contrast to GLP-1 RA are considered body weight neutral and only lead to minor reductions in body weight in patients with T2DM [9, 24, 25].
Neuroprotective effects
T2DM is associated with a higher incidence of the neurodegenerative disorders of Alzheimer’s disease and Parkinson’s disease, suggesting a relationship between neuronal cell death and insulin dysregulation [11, 44, 45].
In preclinical studies, it was shown that exendin-4 diminished glutamate- or amyloid-beta peptide induced apoptosis of cultured rat hyppocampal neurons. Both, glutamate and amyloid-beta peptide are involved in the process of neurodegenaration [46, 47]. In models of diabetic polyneuropathy and peripheral nerve degeneration, exendin-4 also demonstrated favorable effects [48, 49]. More recently, it was reported that pretreatment with liraglutide dose-dependently protected rats against the impairment of spacial memory induced by an intrahippocampal injection of amyloid-beta protein [50]. Likewise, exendin-4 treatment protected mice with streptozotocin-induced hyperglycaemia against the cognitive dysfunction observed in saline-treated mice resulting from hyperglycaemia and/or LPS injection [11, 51]. Both GLP-1 RA, exenatide and liraglutide, have been shown to provide neuroprotective effects in animal models of diabetes, stroke, Parkinson’s disease, and Alzheimer’s disease [52–56]. Progenitor cell division and differentiation toward neurons were significantly enhanced in all models of diabetic mice treated with these GLP-1 RA [53].
Regarding the influence of DPP-4 inhibitors on the CNS, a recent study in a mouse model for T2DM indicated a linagliptin-mediated neuroprotection regarding ischaemic stroke that was glucose-independent and likely involved GLP-1 [57]. Ischemic brain damage was measured by determining stroke volume and by stereologic quantifications of surviving neurons in the striatum/cortex. Pronounced antistroke efficacy of linagliptin was demonstrated in normal mice as well as the diabetic mice, whereas the sulfonylurea glimepiride proved efficacious against stroke in normal mice only [57]. The benefit was independent of glycaemic control and was associated with marked increases in plasma levels of GLP-1. In the diabetic mice, the neuronal salvage was greater in the linagliptin-treated group compared with glimeperide-treated mice, despite less effective glucose control suggesting mechanisms distinct from glycaemic control alone. However, it was not possible, to clearly identify the putative mechanism of neuroprotection of DPP-4 inhibition in this study, especially since DPP-4 inhibition has potentially many other effects that do not directly involve GLP-1 [57, 58].
In summary, preclinical data have demonstrated that GLP-1 RAs can cross the blood brain barrier, enhance neuroneogenesis, and protect against the neurological damage commonly associated with diseases such as Alzheimer’s disease. However, the precise cellular mechanism by which GLP-1 exerts its neuroprotective effects is as yet unknown. GLP-1 RA therapy may also limit hippocampal atrophy in patients with T2DM, suggesting GLP-1 RAs may prove a valuable therapeutic agent for the future treatment of neurodegenerative diseases. To date, no study has described the effect of GLP-1 RA therapy in patients with T2DM who have such a specific coexistent neuropsychiatric condition, but such studies are planned [11]. Likewise, there are first indications from animal studies of potentially beneficial effects of a DPP-4 inhibitor in a diabetes/ischaemic stroke model in which the precise mechanism of the DPP-4 inhibitor action is also unknown. Whether the preclinical data will show corresponding results in the ongoing cardiovascular safety studies performed with incretin-based therapies (see Table 2), especially on “hard endpoints” like stroke, will be important to finally judge the importance of the preclinical findings described above [11, 58].
Effects on the cardiovascular system
An association between the higher incidence of cardiovascular disease in T2DM and insufficient glycaemic control has been shown in clinical studies [59, 60]. However, interventions with intensive therapy of T2DM with the classical antidiabetic treatment options (metformin, sulfonylurea, glitazones, and insulin) to normalize glycaemia only led to a moderate reduction in cardiovascular events without a significant reduction in all-cause mortality [61, 62]. A small short-term study investigated the safety and efficacy of 72-hour infusion of GLP-1 in patients with acute myocardial infarction (AMI) and left ventricular dysfunction [63]. The infusion of GLP-1 was well tolerated and improved left ventricular function significantly and independently of AMI location or history of diabetes. The GLP-1 RAs liraglutide and exenatide as well as the DPP-4 inhibitors have demonstrated various aspects of cardiac function in animal models and cardiovascular risk factors in subjects with T2DM and long-term cardiovascular outcome trials are now ongoing [11].
Effects on biomarkers for cardiovascular risk and dyslipidaemia
Significant reductions in biomarkers for cardiovascular risk (high sensitivity c-reactive protein [hsCRP], brain natriuretic protein [BNP], and plasminogen activator inhibitor-1 [PAI-1]) were observed in long-term studies with the GLP-1 RA exenatide and liraglutide [64, 65]. Data from the 3.5 years extension of the exenatide phase 3 programme showed a persistent and significant improvements in total cholesterol (TC), LDL-cholesterol (LDL-C), HDL-cholesterol (HDL-C), and triglycerides (TG) were observed [64]. Stratification of these data by body weight change revealed that patients who lost most weight had the greatest improvements in TG and HDL-C; a similar sub-analysis has not been published to date for liraglutide. The long-term EUREXA study (The European Exenatide Study) also reported a significantly greater improvement from baseline in serum hsCRP, TG, and HDL-C following 3 years of exenatide BID treatment compared with glimepiride use (p < 0.005 for all) [66]. Liraglutide treatment at the high dose of 1.8 mg resulted in significantly greater reductions in free fatty acids, TG and VLDL cholesterol compared to exenatide BID in a head-to-head trial, while liraglutide at this dose and the long-acting form of exenatide, exenatide QW allowed similar reductions in cholesterol, HDL, and LDL cholesterol [11, 37, 67].
In a metaanalysis on the effect of different oral antidiabetic agents on the lipid profile, DPP-4 inhibitors showed a favorable effect by lowering total cholesterol and triglycerides [68]. The difference-in-means for endpoint versus baseline total cholesterol in patients on DPP-4 inhibitors treatment in another metaanalysis was significantly higher in comparison with controls, meaning that treatment with DPP-4 inhibitors is associated with a significant reduction in total cholesterol (−0.18 [−0.29; −0.06] mmol/L (−7.0 [−11.2; −2.50] mg/dL); p = 0.002) [69]. DPP-4 inhibitors seem to have a more favorable effect on the lipid profile than sulfonylureas in these investigations. In a clinical study from Japan, it was shown that sitagliptin has the potential to lower markers for inflammation [70].
Effects on haemodynamics, blood pressure, and heart rate
In clinical trials with GLP-1 RA, a clinically meaningful reduction of the systolic blood pressure has been observed, whereby the reductions were generally greater in individuals with a higher baseline systolic blood pressure. In those phase III studies, the mean reductions ranged 2–7 mmHg [10, 11, 32, 33, 64, 71]. In a metaanalysis of clinical trials that used GLP-1 RA therapy in T2DM, a significantly greater reduction in systolic blood pressure was observed in the subjects that were treated with GLP-1 RA compared to those in the control arms of the respective studies (placebo, comparator oral antihyperglycaemic medications, or insulin) (weighted mean difference 3.57 mmHg, 95 % CI 5.49–1.66 mmHg) [72]. For the diastolic blood pressure, the findings in the metaanalysis were not as consistent as for the systolic blood pressure, while GLP-1 RA therapy provided a significantly greater reduction versus “control” treatments (p < 0.05), the effect may not be clinically relevant (weighted mean difference 1.38 mmHg, 95 % CI 2.02–0.73 mmHg), and it was not consistently observed across the studies included [11, 72]. The reduction in systolic blood pressure is independent from the weight loss that is also observed with GLP-1 RA therapy and is already present in early phases of treatment, when weight reduction has not occurred yet [73].
An increase in the heart rate of approximately 2–4 beats per minute was observed in the clinical studies with GLP-1 RA. This rise in pulse rate was persistent, but not dose dependent on the dose of the GLP-1 RA used [10, 11, 33, 74]. The exact molecular mechanisms behind the GLP-1 RA-associated decrease in systolic blood pressure and increase in heart rate have not yet been fully elucidated. Mechanistic studies investigating acute effects as well as long-term clinical studies on the effects of GLP-1 RAs on haemodynamics and autonomic nervous system activity will be important as to understand these changes. Furthermore, it is not clear yet, if these effects might be predictors of cardiovascular outcomes [11, 75].
In a small study in patients with T2DM and congestive heart failure, an acute intravenous infusion of exenatide was able to decrease the pulmonary capillary wedge pressure (PCWP) compared with placebo [76]. PCWP is often used as an indirect measure of left atrial pressure and is considered to be a marker of acute pulmonary oedema; therefore, the effects of exenatide on PCWP may be clinically beneficial, but further studies are required to assess the effect of the concomitant increase in cardiac index [11]. Regarding ECG changes and cardiac rhythm, there have been conflicting data, whether GLP-1 RA treatment causes changes of the QTc interval (as a risk marker for arrhythmias and sudden death). While one study showed an increase of the QTc interval with increasing doses of exenatide, other studies with either exenatide or liraglutide could not confirm this finding [77–79].
DPP-4 inhibition has also yielded positive results. For example, Shigeta et al. [80, 81] observed reversal of diastolic ventricular dysfunction in a rat model due DPP4 inhibition, via local actions on angiogenesis and inotropic effects. Similar results were reported by Gomez et al. [80, 82] who observed preservation of glomerular filtration rate, increase in stroke volume, and enhancement of the inotropic effect of exogenous brain natriuretic peptide due to DPP-4 inhibition.
Antihypertensive effects have also been observed for DPP-4 inhibitors. For example, Yanai et al. [80, 83] reported reduction of body weight, HbA1c levels, and blood pressure after 6-month treatment with sitagliptin. The antihypertensive effect of sitagliptin was confirmed by Ogawa, who showed that this effect was independent of BMI and blood glucose reduction [80, 84].
Effects on the endothelium
The endothelium plays an important role in the regulation of vasoconstriction, vasodilation, blood pressure, subclinical inflammation, and balance of coagulation. T2DM and hypertension are associated with endothelial dysfunction that later results in atherogenesis [85, 86]. In preclinical studies using either isolated endothelial cells, isolated perfused vasculature or animal models for endothelial dysfunction (ApoE−/− knockout mice), the GLP-1 RA exenatide, and liraglutide improved parameters of endothelial dysfunction and demonstrated anti-inflammatory or antioxidative effects as well as an inhibitoty effect on endothelial cell apoptosis [87–90].
In patients with T2DM and in obese subjects with prediabetes, the effects of exenatide on endothelial function were investigated, showing favorable effects on digital reactive hyperaemia, brachial artery flow, C-reactive protein (CRP), circulating oxidized LDL (oxLDL), and vascular cell adhesion molecule-1 (VCAM-1) [75, 86, 91]. Likewise, liraglutide was shown to improve surrogate markers of vascular and endothelial function in patients with T2DM like plasminogen activator inhibitor-1 (PAI-1), intact proinsulin and microvascular response to flicker light [65]. Treatment with liraglutide was also associated with an attenuation of atherosclerotic lesions in a mouse model as well as a reduction in carotid intima-media thickness (carotid IMT) in a clinical study, where the effect was independent of the glycaemic parameters and the development of body weight [11, 92, 93].
Effects of cardioprotection
In preclinical studies, the GLP-1 RA demonstrated cardioprotective effects. Liraglutide-reduced infarct size and increased survival after myocardial infarction (MI) in mice and reduced mortality from cardiac rupture, and improved cardiac output in a mouse model of MI [11, 94]. Exenatide was shown to reduce myocardial infarct size and to protect against deterioration of cardiac function in a porcine model of ischaemia and reperfusion injury [95]. Likewise, albuglutide had cadioprotective effects in a preclinical study showing an improvement of myocardial infarct size in an animal model of reperfusion ischaemia [11, 96]. Lixisenatide, on the other hand, revealed cardioprotective properties in a mouse model that may partly be mediated by GLP-1 receptor independent mechanisms [11, 97]. Therefore, further mechanistic studies need to be carried out to fully characterize and understand the cardiovascular effects of GLP-1 [11].
In isolated cardiomyocytes, GLP-1 RA improve glucose uptake and protect these cells from apoptosis by reducing hydrogen-peroxide-, palmitate-, and thapsigargin-mediated apoptotic mechanisms [11, 98].
In patients with myocardial infarction with ST-segment elevation (STEMI), the application of exenatide in clinical feasibility and pilot studies seems to be safe and associated with beneficial outcomes on infarct size or myocardial area at risk [11, 99–101].
DPP-4 inhibitors have also shown encouraging results in human studies. In a placebo-controlled trial conducted on patients with pre-existing coronary artery disease with preserved left ventricular function, an increase in GLP-1 levels caused by DPP-4 inhibition resulted in improvement of global and regional left ventricular function and amelioration of post-ischemic stunning [80, 102]. New horizons are being explored in this regard, with a recent study providing promising results in the combination trial (SITAGRAMI-Trial) of sitagliptin and G-CSF-based stem cell mobilization [80, 103].
Effects on cardiovascular outcomes in subjects with T2DM
Analyses of the major adverse cardiovascular events (MACE) have been obtained from the clinical studies with GLP-1 RA and DPP-4 inhibitors [11, 104–107]. With the GLP-1 RA exenatide and liraglutide, the incidence ratio of MACE was not increased (and tended to be lower) with liraglutide (0.7; 95 % CI 0.4–1.4) and exenatide BID (0.7; 95 % CI 0.4–1.3) compared with all comparator drugs pooled [11, 104, 105]. For all the incretin baes therapies, large prospective cardiovascular safety and -outcome trials are currently ongoing (see Table 2 for details).
Two of these prospective studies (for the DPP-4 inhibitors alogliptin and saxagliptin) have already been completed and have had neutral results concerning the predefined combined cardiovascular endpoints compared to the respective control arms [108, 109]. Both agents had data from pooled MACE analyses from the clinical development programmes that suggested a possible cardioprotective effect (saxagliptin: hazard ratio [HR] = 0.43 [95 % CI 0.23–0.80]; alogliptin: HR = 0.64 [95 % CI 0.0–1.41]) [110, 111], but the prosepective endpoint studies that were performed in a patient population with a higher cardiovascular comorbidity- or risk as well as with a longer diabetes duration did not confirm these preliminary data [109–112]. In the SAVOR-TIMI 53 study, 16,492 patients with T2DM and a history or at a high risk of cardiovascular disease were randomized to either saxagliptin or placebo [109]. After a median of 2.1 years of treatment, the incidence of the primary (composite of cardiovascular death, myocardial infarction, and ischaemic stroke) and secondary endpoint (cardiovascular death, myocardial infarction, stroke, hospitalization for unstable angina, coronary revascularisation, or heart failure) was very similar in both groups (primary endpoint: 7.3 % [saxagliptin] vs. 7.2 % [placebo], HR = 1.00 [95 % CI 0.89–1.12], p = 0.99) [109]. Similarly, in the EXAMINE study (5,380 people with T2D with recent acute coronary syndrome), 18 months’ treatment with alogliptin did not decrease the rates of major adverse cardiovascular events versus placebo (primary endpoint: 11.3 % [alogliptin] vs. 11.8 % [placebo], HR = 0.96 [95 % CI ≤ 1.16], p = 0.32) [11, 108].
The results of the remaining outcome studies need to be awaited, before definitive conclusions can be drawn on the advantages, benefits, or unfavorable outcomes in the long-term treatment with incretin-based therapies. Taken together, preliminary and short-term study results point to potential cardioprotective effects of exenatide and sitagliptin in patients with heart failure and myocardial infarction. Long-term randomized trials, on the other hand, showed no benefit of alogliptin, and an increase of hospital admissions due to heart failure associated with the use of saxagliptin [112].
Effects on other tissues and organs
Incretin-based therapies can also have effects on other tissues in the body, either directly through locally expressed GLP-1 receptors or indirectly by degradation products of either endogenous GLP-1, degradation products of the GLP-1 RA, or by DPP-4 effects. Effects on the kidneys are of particular interest due to the increased incidence of renal impairment in people with type 2 diabetes [113].
The kidneys
Microvascular complications of T2DM are a main cause of renal impairment; therefore, the tolerability of type 2 diabetes agents in people with renal impairment is of clinical interest [11, 113]. Regarding GLP-1 RA, a meta-analysis of six liraglutide phase 3 trials has reported that liraglutide use did not significantly alter creatinine clearance in people with mild renal impairment compared with the general study population [114]. Unlike liraglutide, exenatide is renaly excreted and its safety in people with renal impairment is less clear [11, 115, 116]. Due to very limited clinical experience, liraglutide and exenatide QW are currently not recommended for use in people with moderate or severe renal impairment. Exenatide BID can be used in people with moderate renal impairment but dose escalation from 5 to 10 μg should proceed conservatively. Generally, patients treated with GLP-1 RA should take precautions to avoid fluid depletion due to the potential risk of dehydration in relation to gastrointestinal side effects [11, 117].
All currently available DPP-inhibitors appear to be appropriate pharmacotherapeutic choices in patients with declining renal function, with linagliptin affording the added advantage of not requiring dose adjustment or periodic monitoring of drug-related kidney function [117].
Pancreatic safety
Concerns regarding pancreatic safety with incretin-based therapies have been raised by one study that analyzed the pancreata from organ donors with or without T2DM [118]. An increase in endocrine pancreatic mass and also an increase in exocrine duct cell proliferation and dysplasia were described in the organs of people with a history of treatment with incretin-based therapies. The authors also suggested an increased risk for the evolution of neuroendocrine tumors [118]. Meanwhile, in a statement released by the European Medicines Agency (EMA) following an investigation, a hearing by the Food and drugs Administration (FDA) as well as several other publications, concerns have been raised about the methodology and sample size of the study [119–122]. In particular the treatment groups appear poorly matched not only in terms of age (mean 58 years [incretin therapy] vs. 40 years [diabetic control]), gender (25 % female vs. 67 % female), diabetes duration (12 years vs. 8 years) and background medication (five subjects in diabetic control group were untreated), but also with respect to diabetes type. The subjects receiving sitagliptin/exenatide BID had type 2 diabetes, while the some of the “diabetic controls” appear to resemble people with type 1 diabetes (for example, two died of diabetic ketoacidosis); this is important as imaging studies have shown that pancreatic volume in subjects with type 1 diabetes is significantly reduced shortly after diagnosis and declines further as disease progresses [11, 122–124]. The general conclusions of the regulatory bodies EMA and FDA were that there should not be any substantial changes in clinical recommendations regarding the use of incretin-based therapies based on the study by Butler et al [11, 118]. Pooled analyses and meta-analyses of data from the clinical development programmes of individual or pooled DPP-4 inhibitors and individual or pooled GLP-1 RAs and analyses from claims databases have also reported no increased risk of pancreatitis with either class of agent compared to comparator therapies [11, 106, 125–129]. Likewise, there has been no signal for an increase in pancreatitis or other pancreatic pathologies in the recently completed endpoint studies with alogliptin ad saxagliptin [109, 111]. The remaining ongoing long-term cardiovascular safety studies carried out with incretin-based therapies will generate additional safety data on pancreatic safety in a large population of >60,000 patients.
Conclusions
Incretin-based therapies may have beneficial effects beyond the glycaemic effects by direct action on the endocrine pancreas due to the widespread expression of GLP-1 receptors. These may include cardiovascular effects, effects on lipid metabolism, neurological disorders, and (as already shown for the GLP-1 RA) beneficial effects on systolic blood pressure and body weight. These beneficial effects need to be counterweighed against possible side effects, e.g., the gastrointestinal side effects and the increase of pulse rate observed with GLP-1 RA therapy. Data from the ongoing long-term safety studies are needed to judge, if the beneficial effects seen in preclinical studies and in shorter clinical trials will also improve outcomes in the long run. In the future, GLP-1 RAs may also have potential to be used in treating obesity. Such use is not currently approved and substantial further research in people without diabetes is underway to test this hypothesis [11].
References
International Diabetes Federation (IDF): Diabetes Atlas, 6th edition 2013. http://www.idf.org/diabetesatlas. Accessed 15 Jan 2014
N.J. Morrish, S.L. Wang, L.K. Stevens, J.H. Fuller, H. Keen, Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 44(Suppl. 2), S14–S21 (2001)
R. Donnelly, A.M. Emslie-Smith, I.D. Gardner, A.D. Morris, Vascular compli-cations of diabetes. Brit. Med. J. 320, 1062–1066 (2000)
W.P.T. James, Overweight and obesity (high body mass index), in Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors, ed. by Ezzati (World Health Organization, Geneva, 2004), pp. 497–596
B. Ahrén, Incretin dysfunction in type 2 diabetes: clinical impact and future perspectives. Diabetes Metab. 39, 195–201 (2013)
J.J. Holst, The physiology of glucagon-like peptide 1. Physiol. Rev. 87, 1409–1439 (2007)
R. Mentlein, B. Gallwitz, W.E. Schmidt, Dipeptidyl-peptidase IV hydrolyses gastric inhibitory polypeptide, glucagon-like peptide-1(7-36)amide, peptide histidine methionine and is responsible for their degradation in human serum. Eur. J. Biochem. 214, 829–835 (1993)
C.F. Deacon, M.A. Nauck, M. Toft-Nielsen, L. Pridal, B. Willms, J.J. Holst, Both subcutaneously and intravenously administered glucagon-like peptide I are rapidly degraded from the NH2-terminus in type II diabetic patients and in healthy subjects. Diabetes 44, 1126–1131 (1995)
M.A. Nauck, T. Vilsbøll, B. Gallwitz, A. Garber, S. Madsbad, Incretin-based therapies: viewpoints on the way to consensus. Diabetes Care 32(Suppl 2), S223–S231 (2009)
M.J. Davies, R. Kela, K. Khunti, Liraglutide - overview of the preclinical and clinical data and its role in the treatment of type 2 diabetes. Diabetes Obes. Metab. 13, 207–220 (2011)
J. Seufert, B. Gallwitz, The extra-pancreatic effects of GLP-1 receptor agonists: a focus on the cardiovascular, gastrointestinal and central nervous systems. Diabetes Obes. Metab. (2013). doi: 10.1111/dom.12251
M.H. Muskiet, M.M. Smits, L.M. Morsink, M. Diamant, The gut-renal axis: do incretin-based agents confer renoprotection in diabetes? Nat Rev Nephrol. (2013). doi:10.1038/nrneph.2013.272
R. Ritzel, C. Orskov, J.J. Holst, M.A. Nauck, Pharmacokinetic, insulino-tropic, and glucagonostatic properties of GLP-1 [7-36 amide] after subcutaneous injection in healthy volunteers. Dose–response-relationships. Diabetologia 38, 720–725 (1995)
J.J. Meier, B. Gallwitz, S. Salmen, O. Goetze, J.J. Holst, W.E. Schmidt, M.A. Nauck, Normalization of glucose concentrations and deceleration of gastric emptying after solid meals during intravenous glucagon-like peptide 1 in patients with type 2 diabetes. J. Clin. Endocrinol. Metab. 88, 2719–2725 (2003)
J.J. Meier, GLP-1 receptor agonists for individualized treatment of type 2 dia-betes mellitus. Nat. Rev. Endocrinol. 8, 728–742 (2012)
J. Jelsing, N. Vrang, G. Hansen, K. Raun, M. Tang-Christensen, L.B. Knudsen, Liraglutide: Short lived effect on gastric emptying—long lasting effects on body-weight. Diabetes Obes. Metab. 14, 531–538 (2012)
M. Horowitz, A. Flint, K.L. Jones, C. Hindsberger, M.F. Rasmussen, C. Kapitza, S. Doran, T. Jax, M. Zdravkovic, I.M. Chapman, Effect of the once-daily human GLP-1 analogue liraglutide on appetite, energy intake, energy expenditure and gastric emptying in type 2 diabetes. Diabetes Res. Clin. Pract. 97, 258–266 (2012)
D.J. Drucker, J.B. Buse, K. Taylor, D.M. Kendall, M. Trautmann, D. Zhuang, L. Porter, DURATION-1 Study Group, Exenatide once weekly versus twice daily for the treatment of type 2 diabetes: a randomised, open-label, non-inferiority study. Lancet 372(9645), 1240–1250 (2008)
M. Lorenz, C. Pfeiffer, A. Steinsträßer, R.H. Becker, H. Rütten, P. Ruus, M. Horowitz, Effects of lixisenatide once daily on gastric emptying in type 2 diabetes—relationship to postprandial glycemia. Regul. Pept. 185, 1–8 (2013)
S.E. Kanoski, L.E. Rupprecht, S.M. Fortin, B.C. De Jonghe, M.R. Hayes, The role of nausea in food intake and body weight suppression by peripheral GLP-1 receptor agonists, exendin-4 and liraglutide. Neuropharmacology 62, 1916–1927 (2012)
M.E. Lean, R. Carraro, N. Finer, H. Hartvig, M.L. Lindegaard, S. Rössner, L. Van Gaal, A. Astrup, Tolerability of nausea and vomiting and associations with weight loss in a randomized trial of liraglutide in obese, non-diabetic adults. Int J Obes (Lond). (2013). doi:10.1038/ijo.2013.149
K. Niswender, X. Pi-Sunyer, J. Buse, K.H. Jensen, A.D. Toft, D. Russell-Jones, B. Zinman, Weight change with liraglutide and comparator therapies: an analysis of seven phase 3 trials from the liraglutide diabetes development programme. Diabetes Obes. Metab. 15, 42–54 (2013)
H. Linnebjerg, S. Park, P.A. Kothare, M.E. Trautmann, K. Mace, M. Fineman, I. Wilding, M. Nauck, M. Horowitz, Effect of exenatide on gastric empty-ing and relationship to postprandial glycemia in type 2 diabetes. Regul. Pept. 151, 123–129 (2008)
C.F. Deacon, J.J. Holst, Dipeptidyl peptidase-4 inhibitors for the treatment of type 2 diabetes: comparison, efficacy and safety. Expert Opin. Pharmacother. 14, 2047–2058 (2013)
M.A. Nauck, Incretin-based therapies for type 2 diabetes mellitus: properties, functions, and clinical implications. Am. J. Med. 124(1 Suppl), S3–S18 (2011)
M.D. Turton, D. O’Shea, I. Gunn, S.A. Beak, C.M. Edwards, K. Meeran, S.J. Choi, G.M. Taylor, M.M. Heath, P.D. Lambert, J.P. Wilding, D.M. Smith, M.A. Ghatei, J. Herbert, S.R. Bloom, A role for glucagon-like peptide-1 in the central regulation of feeding. Nature 379(6560), 69–72 (1996)
B. Gallwitz, Anorexigenic effects of GLP-1 and its analogues. Handb. Exp. Pharmacol. 209, 185–207 (2012)
A.J. Kastin, V. Akerstrom, Entry of exendin-4 into brain is rapid but may be limited at high doses. Int. J. Obes. Relat. Metab. Disord. 27, 313–318 (2003)
M. Punjabi, M. Arnold, N. Geary, W. Langhans, G. Pacheco-López, Peripheral glucagon-like peptide-1 (GLP-1) and satiation. Physiol. Behav. 105, 71–76 (2011)
K. Hunter, C. Hölscher, Drugs developed to treat diabetes, liraglutide and lixisenatide, cross the blood brain barrier and enhance neurogenesis. BMC Neurosci. 13, 33 (2012)
S.E. Kanoski, S.M. Fortin, M. Arnold, H.J. Grill, M.R. Hayes, Peripheral and central GLP-1 receptor populations mediate the anorectic effects of peripherally administered GLP-1 receptor agonists, liraglutide and exendin-4. Endocrinology 152, 3103–3112 (2011)
A. Stonehouse, B. Walsh, R. Cuddihy, Exenatide once-weekly clinical development: safety and efficacy across a range of background therapies. Diabetes Technol. Ther. 13, 1063–1069 (2011)
D. Russell-Jones, R.M. Cuddihy, M. Hanefeld, A. Kumar, J.G. González, M. Chan, A.M. Wolka, M.K. Boardman, DURATION-4 Study Group, Efficacy and safety of exenatide once weekly versus metformin, pioglitazone, and sitagliptin used as monotherapy in drug-naive patients with type 2 diabetes (DURATION-4): a 26-week double-blind study. Diabetes Care 35, 252–258 (2012)
J.B. Buse, R.R. Henry, J. Han, D.D. Kim, M.S. Fineman, A.D. Baron, Ex-enatide-113 Clinical Study Group, Effects of exenatide (exendin-4) on glyce-mic control over 30 weeks in sulfonylurea-treated patients with type 2 diabe-tes. Diabetes Care 27, 2628–2635 (2004)
R.A. DeFronzo, R.E. Ratner, J. Han, D.D. Kim, M.S. Fineman, A.D. Baron, Effects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetes. Diabetes Care 28, 1092–1100 (2005)
D.M. Kendall, M.C. Riddle, J. Rosenstock, D. Zhuang, D.D. Kim, M.S. Fineman, A.D. Baron, Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sul-fonylurea. Diabetes Care 28, 1083–1091 (2005)
J.B. Buse, M. Nauck, T. Forst, W.H. Sheu, S.K. Shenouda, C.R. Heilmann, B.J. Hoogwerf, A. Gao, M.K. Boardman, M. Fineman, L. Porter, G. Schernthaner, Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet 381(9861), 117–124 (2013)
L.J. Scott, Lixisenatide: a review of its use in patients with type 2 diabetes mellitus. BioDrugs 27, 509–523 (2013)
A. Astrup, S. Rossner, L. Van Gaal, A. Rissanen, L. Niskanen, M. Al Hakim, J. Madsen, M.F. Rasmussen, M.E. Lean, NN8022-1807 Study Group, Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet 374, 1606–1616 (2009)
A. Astrup, R. Carraro, N. Finer, A. Harper, M. Kunesova, M.E. Lean, L. Niskanen, M.F. Rasmussen, A. Rissanen, S. Rössner, M.J. Savolainen, L. Van Gaal, NN8022-1807 Investigators, Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond) 36, 843–854 (2012)
K. Elkind-Hirsch, O. Marrioneaux, M. Bhushan, D. Vernor, R. Bhushan, Comparison of single and combined treatment with exenatide and metformin on menstrual cyclicity in overweight women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 93, 2670–2678 (2008)
J. Rosenstock, L.J. Klaff, S. Schwartz, J. Northrup, J.H. Holcombe, K. Wilhelm, M. Trautmann, Effects of exenatide and lifestyle modification on body weight and glucose tolerance in obese subjects with and without pre-diabetes. Diabetes Care 33, 1173–1175 (2010)
A.S. Kelly, A.M. Metzig, K.D. Rudser, A.K. Fitch, C.K. Fox, B.M. Nathan, M.M. Deering, B.L. Schwartz, M.J. Abuzzahab, L.M. Gandrud, A. Moran, C.J. Billington, S.J. Schwarzenberg, Exenatide as a weight-loss therapy in extreme pediatric obesity: a randomized, controlled pilot study. Obesity 20, 364–370 (2012)
F. Irie, A.L. Fitzpatrick, O.L. Lopez, L.H. Kuller, R. Peila, A.B. Newman, L.J. Launer, Enhanced risk for Alzheimer disease in persons with type 2 dia-betes and APOE epsilon4: the Cardiovascular Health Study Cognition Study. Arch. Neurol. 65, 89–93 (2008)
J.A. Driver, A. Smith, J.E. Buring, J.M. Gaziano, T. Kurth, G. Logroscino, Prospective cohort study of type 2 diabetes and the risk of Parkinson’s disease. Diabetes Care 31, 2003–2005 (2008)
T. Perry, N.J. Haughey, M.P. Mattson, J.M. Egan, N.H. Greig, Protection and reversal of excitotoxic neuronal damage by glucagon-like peptide-1 and exendin-4. J. Pharmacol. Exp. Ther. 302, 881–888 (2002)
T. Perry, D.K. Lahiri, K. Sambamurti, D. Chen, M.P. Mattson, J.M. Egan, N.H. Greig, Glucagon-like peptide-1 decreases endogenous amyloid-β pep-tide (Aβ) levels and protects hippocampal neurons from death induced by Aβ and iron. J. Neurosci. Res. 72, 603–612 (2003)
T. Himeno, H. Kamiya, K. Naruse, N. Harada, N. Ozaki, Y. Seino, T. Shibata, M. Kondo, J. Kato, T. Okawa, A. Fukami, Y. Hamada, N. Inagaki, Y. Seino, D.J. Drucker, Y. Oiso, J. Nakamura, Beneficial effects of exendin-4 on experimental polyneuropathy in diabetic mice. Diabetes 60, 2397–2406 (2011)
W.J. Liu, H.Y. Jin, K.A. Lee, S.H. Xie, H.S. Baek, T.S. Park, Neuroprotec-tive effect of the glucagon-like peptide-1 receptor agonist, synthetic exendin-4, in streptozotocin-induced diabetic rats. Br. J. Pharmacol. 164, 1410–1420 (2011)
W.N. Han, C. Hölscher, L. Yuan, W. Yang, X.H. Wang, M.N. Wu, J.S. Qi, Liraglutide protects against amyloid-β protein-induced impairment of spatial learning and memory in rats. Neurobiol. Aging 34, 576–588 (2013)
H.J. Huang, Y.H. Chen, K.C. Liang, Y.S. Jheng, J.J. Jhao, M.T. Su, G.J. Lee-Chen, H.M. Hsieh-Li, Exendin-4 protected against cognitive dysfunction in hyperglycemic mice receiving an intrahippocampal lipopolysaccharide injection. PLoS One 7(7), e39656 (2012)
C. Hölscher, L. Li, New roles for insulin-like hormones in neuronal signalling and protection: new hopes for novel treatments of Alzheimer’s disease? Neurobiol. Aging 31, 1495–1502 (2010)
A. Hamilton, S. Patterson, D. Porter, V.A. Gault, C. Hölscher, Novel GLP-1 mimetics developed to treat type 2 diabetes promote progenitor cell prolifera-tion in the brain. J. Neurosci. Res. 89, 481–489 (2011)
P.L. McClean, V. Parthsarathy, E. Faivre, C. Hölscher, The diabetes drug li-raglutide prevents degenerative processes in a mouse model of Alzheimer’s disease. J. Neurosci. 31, 6587–6594 (2011)
S. Kim, M. Moon, S. Park, Exendin-4 protects dopaminergic neurons by in-hibition of microglial activation and matrix metalloproteinase-3 expression in an animal model of Parkinson’s disease. J. Endocrinol. 202, 431–439 (2009)
Y. Li, T. Perry, M.S. Kindy, B.K. Harvey, D. Tweedie, H.W. Holloway, K. Powers, H. Shen, J.M. Egan, K. Sambamurti, A. Brossi, D.K. Lahiri, M.P. Mattson, B.J. Hoffer, Y. Wang, N.H. Greig, GLP-1 receptor stimulation preserves primary cortical and dopaminergic neurons in cellular and rodent models of stroke and Parkinsonism. Proc. Natl. Acad. Sci. USA 106, 1285–1289 (2009)
V. Darsalia, H. Ortsäter, A. Olverling, E. Darlöf, P. Wolbert, T. Nyström, T. Klein, Å. Sjöholm, C. Patrone, The DPP-4 inhibitor linagliptin counteracts stroke in the normal and diabetic mouse brain: a comparison with glimepiride. Diabetes 62, 1289–1296 (2013)
R.P. Shannon, DPP-4 inhibition and neuroprotection: do mechanisms matter? Diabetes 62, 1029–1031 (2013)
R.C. Turner, H. Millns, H.A. Neil, I.M. Stratton, S.E. Manley, D.R. Matthews, R.R. Holman, Risk factors for coronary artery disease in non-insulin de-pendent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23). BMJ 316, 823–828 (1998)
Emerging Risk Factors Collaboration, S.R. Seshasai, S. Kaptoge, A. Thompson, E. Di Angelantonio, P. Gao, N. Sarwar, P.H. Whincup, K.J. Mukamal, R.F. Gillum, I. Holme, I. Njølstad, A. Fletcher, P. Nilsson, S. Lewington, R. Collins, V. Gudnason, S.G. Thompson, N. Sattar, E. Selvin, F.B. Hu, J. Danesh, Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364, 829–841 (2011)
ADVANCE Collaborative Group, A. Patel, S. MacMahon, J. Chalmers, B. Neal, L. Billot, M. Woodward, M. Marre, M. Cooper, P. Glasziou, D. Grobbee, P. Hamet, S. Harrap, S. Heller, L. Liu, G. Mancia, C.E. Mogensen, C. Pan, N. Poulter, A. Rodgers, B. Williams, S. Bompoint, B.E. de Galan, R. Joshi, F. Travert, Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358, 2560–2572 (2008)
Action to Control Cardiovascular Risk in Diabetes Study Group, H.C. Gerstein, M.E. Miller, R.P. Byington, D.C. Goff Jr, J.T. Bigger, J.B. Buse, W.C. Cushman, S. Genuth, F. Ismail-Beigi, R.H. Grimm Jr, J.L. Probstfield, D.G. Simons-Morton, W.T. Friedewald, Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358, 2545–2559 (2008)
L.A. Nikolaidis, S. Mankad, G.G. Sokos, G. Miske, A. Shah, D. Elahi, R.P. Shannon, Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 109, 962–965 (2004)
D.C. Klonoff, J.B. Buse, L.L. Nielsen, X. Guan, C.L. Bowlus, J.H. Holcombe, M.E. Wintle, D.G. Maggs, Exenatide effects on diabetes, obesity, cardiovascular risk factors and hepatic biomarkers in patients with type 2 diabetes treated for at least 3 years. Curr. Med. Res. Opin. 24, 275–286 (2008)
T. Forst, G. Michelson, F. Ratter, M.M. Weber, S. Anders, M. Mitry, B. Wilhelm, A. Pfützner, Addition of liraglutide in patients with Type 2 diabetes well controlled on metformin monotherapy improves several markers of vascular function. Diabet. Med. 29, 1115–1118 (2012)
R. Simo, B. Guerci, G. Schernthaner, B. Gallwitz, J. Guzman, F. Dotta, A. Festa, H. Sapin, S. Chen, J. Kiljanski, Long-term administration of ex-enatide and changes in body weight and markers of cardiovascular risk: a comparative study with glimepiride. Diabetologia 55(Suppl. 1), S332 (2012). (Abstract 781)
J. Buse, J. Rosenstock, G. Sesti, W.E. Schmidt, E. Montanya, J.H. Brett, M. Zychma, L. Blonde, LEAD-6 Study Group, Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet 374, 39–47 (2009)
M. Monami, V. Vitale, M.L. Ambrosio, N. Bartoli, G. Toffanello, B. Ragghianti, F. Monami, N. Marchionni, E. Mannucci, Effects on lipid profile of dipeptidyl peptidase 4 inhibitors, pioglitazone, acarbose, and sulfonylureas: meta-analysis of placebo-controlled trials. Adv. Ther. 29, 736–746 (2012)
M. Monami, C. Lamanna, C.M. Desideri, E. Mannucci, DPP-4 inhibitors and lipids: systematic review and meta-analysis. Adv. Ther. 29, 14–25 (2012)
N. Satoh-Asahara, Y. Sasaki, H. Wada, M. Tochiya, A. Iguchi, R. Nakagawachi, S. Odori, S. Kono, K. Hasegawa, A. Shimatsu, A dipeptidyl peptidase-4 inhibitor, sitagliptin, exerts anti-inflammatory effects in type 2 diabetic patients. Metabolism 62, 347–351 (2013)
B. Gallwitz, J. Guzman, F. Dotta, B. Guerci, R. Simó, B.R. Basson, A. Festa, J. Kiljański, H. Sapin, M. Trautmann, G. Schernthaner, Exenatide twice daily versus glimepiride for prevention of glycaemic deterioration in patients with type 2 diabetes with metformin failure (EUREXA): an open-label, randomised controlled trial. Lancet 379, 2270–2278 (2012)
T. Vilsbøll, M. Christensen, A.E. Junker, F.K. Knop, L.L. Gluud, Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ 344, d7771 (2012)
B. Gallwitz, Glucagon-like peptide-1 analogues for type 2 diabetes mellitus: current and emerging agents. Drugs 71, 1675–1688 (2011)
M. Diamant, L. Van Gaal, S. Stranks, J. Northrup, D. Cao, K. Taylor, M. Trautmann, Once weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes (DURATION-3): an open-label randomised trial. Lancet 375, 2234–2243 (2010)
P. Valensi, S. Chiheb, M. Fysekidis, Insulin- and glucagon-like peptide-1-induced changes in heart rate and vagosympathetic activity: why they matter. Diabetologia 56, 1196–1200 (2013)
D. Nathanson, B. Ullman, U. Löfström, A. Hedman, M. Frick, A. Sjöholm, T. Nyström, Effects of intravenous exenatide in type 2 diabetic patients with congestive heart failure: a double-blind, randomised controlled clinical trial of efficacy and safety. Diabetologia 55, 926–935 (2012)
H. Linnebjerg, M. Seger, P.A. Kothare, T. Hunt, A.M. Wolka, M.I. Mitchell, A thorough QT study to evaluate the effects of single dose exenatide 10 μg on cardiac repolarization in healthy subjects. Int. J. Clin. Pharmacol. Ther. 49, 594–604 (2011)
B. Darpö, P. Sager, L. Macconell, B. Cirincione, M. Mitchell, J. Han, W. Huang, J. Malloy, C. Schulteis, L. Shen, L. Porter, Exenatide at therapeutic and supratherapeutic concentrations does not prolong the QTc interval in healthy subjects. Br. J. Clin. Pharmacol. 75, 979–989 (2013)
D.J. Chatterjee, N. Khutoryansky, M. Zdravkovic, C.R. Sprenger, J.S. Litwin, Absence of QTc prolongation in a thorough QT study with subcutaneous liraglutide, a once-daily human GLP-1 analog for treatment of type 2 diabetes. J. Clin. Pharmacol. 11, 1353–1362 (2009)
A. Sheikh, Direct cardiovascular effects of glucagon like peptide-1. Diabetol. Metab. Syndr. 5, 47 (2013)
T. Shigeta, M. Aoyama, Y.K. Bando, A. Monji, T. Mitsui, M. Takatsu, X.W. Cheng, T. Okumura, A. Hirashiki, K. Nagata, T. Murohara, Dipeptidyl peptidase-4 modulates left ventricular dysfunction in chronic heart failure via angiogenesis-dependent and -independent actions. Circulation 126, 1838–1851 (2012)
N. Gomez, K. Touihri, V. Matheeussen, A. Mendes Da Costa, M. Mahmoudabady, M. Mathieu, L. Baerts, A. Peace, P. Lybaert, S. Scharpe, I. De Meester, J. Bartunek, M. Vanderheyden, K. Mc Entee, Dipeptidyl peptidase IV inhibition improves cardiorenal function in overpacing-induced heart failure. Eur J Heart Fail 14, 14–21 (2012)
H. Yanai, H. Adachi, H. Hamasaki, Y. Masui, R. Yoshikawa, S. Moriyama, S. Mishima, A. Sako, Effects of 6-month sitagliptin treatment on glucose and lipid metabolism, blood pressure, body weight and renal function in type 2 diabetic patients: a chart-based analysis. J. Clin. Med. Res. 4, 251–258 (2012)
S. Ogawa, M. Ishiki, K. Nako, M. Okamura, M. Senda, T. Mori, S. Ito, Sitagliptin, a dipeptidyl peptidase-4 inhibitor, decreases systolic blood pressure in Japanese hypertensive patients with type 2 diabetes. Tohoku J. Exp. Med. 223, 133–135 (2011)
N. Chhabra, Endothelial dysfunction—a predictor of atherosclerosis. Internet J. Med. Updat 4, 33–41 (2009)
A.S. Kelly, R.M. Bergenstal, J.M. Gonzalez-Campoy, H. Katz, A.J. Bank, Effects of exenatide vs. metformin on endothelial function in obese patients with pre-diabetes: a randomized trial. Cardiovasc. Diabetol. 11, 64 (2012)
T. Gaspari, H. Liu, I. Welungoda, Y. Hu, R.E. Widdop, L.B. Knudsen, R.W. Simpson, A.E. Dear, A GLP-1 receptor agonist liraglutide inhibits endothelial cell dysfunction and vascular adhesion molecule expression in an Ap-oE−/− mouse model. Diabetes Vasc. Dis. Res. 8, 117–124 (2011)
A. Shiraki, J. Oyama, H. Komoda, M. Asaka, A. Komatsu, M. Sakuma, K. Kodama, Y. Sakamoto, N. Kotooka, T. Hirase, K. Node, The glucagon-like peptide 1 analog liraglutide reduces TNF-α-induced oxidative stress and inflammation in endothelial cells. Atherosclerosis 221, 375–382 (2012)
Ö. Erdogdu, L. Eriksson, T. Nyström, Å. Sjöholm, Q. Zhang, Exendin-4 restores glucolipotoxicity-induced gene expression in human coronary artery endothelial cells. Biochem. Biophys. Res. Commun. 419, 790–795 (2012)
L. Han, Y. Yu, X. Sun, B. Wang, Exendin-4 directly improves endothelial dysfunction in isolated aortas from obese rats through the cAMP or AMPK-eNOS pathways. Diabetes Res. Clin. Pract. 97, 453–460 (2012)
C. Irace, S. De Luca, E. Shehaj, C. Carallo, A. Loprete, F. Scavelli, A. Gnasso, Exenatide improves endothelial function assessed by flow mediated dilation technique in subjects with type 2 diabetes: results from an observational research. Diab. Vasc. Dis. Res. 10, 72–77 (2013)
R.W. Simpson, T. Gaspari, I. Welungoda, R.E. Widdop, L.B. Knudsen, A.E. Dear, The GLP-1 receptor agonist liraglutide attenuates atherosclerotic lesion development and potentially enhances plaque stability in an ApoE−/− mouse model. Diabetes 61(Suppl 1), A486 (2012). (Abstract 1896-P)
M. Rizzo, A. Maria Patti, V. Di Bartolo, R. Vincenza Giglio, G. Montalto, A.A. Rizvi, Effect of liraglutide on carotid intima-media thickness in patients with type-2 diabetes: a 4-month prospective study. Diabetes 61(Suppl 1), A109 (2012). (Abstract 418-P)
M.H. Noyan-Ashraf, M.A. Momen, K. Ban, A.M. Sadi, Y.Q. Zhou, A.M. Riazi, L.L. Baggio, R.M. Henkelman, M. Husain, D.J. Drucker, GLP-1R agonist liraglutide activates cytoprotective pathways and improves outcomes after experimental myocardial infarction in mice. Diabetes 58, 975–983 (2009)
L. Timmers, J.P. Henriques, D.P. de Kleijn, J.H. Devries, H. Kemperman, P. Steendijk, C.W. Verlaan, M. Kerver, J.J. Piek, P.A. Doevendans, G. Pasterkamp, I.E. Hoefer, Exenatide reduces infarct size and improves cardiac function in a porcine model of ischemia and reperfusion injury. J. Am. Coll. Cardiol. 53, 501–510 (2009)
W. Bao, K. Aravindhan, H. Alsaid, T. Chendrimada, M. Szapacs, D.R. Citerone, M.R. Harpel, R.N. Willette, J.J. Lepore, B.M. Jucker, Albiglutide, a long lasting glucagon-like peptide-1 analog, protects the rat heart against is-chemia/reperfusion injury: evidence for improving cardiac metabolic efficiency. PLoS One 6, e23570 (2011)
P. Wohlfart, W. Linz, T. Hübschle, D. Linz, J. Huber, S. Hess, D. Crowther, U. Werner, H. Ruetten, Cardioprotective effects of lixisenatide in rat myocardial ischemia-reperfusion injury studies. J. Transl. Med. 11, 84 (2013)
J.R. Ussher, D.J. Drucker, Cardiovascular biology of the incretin system. Endocr. Rev. 33, 187–215 (2012)
J. Lønborg, H. Kelbæk, N. Vejlstrup, H.E. Bøtker, W.Y. Kim, L. Holmvang, E. Jørgensen, S. Helqvist, K. Saunamäki, C.J. Terkelsen, M.M. Schoos, L. Køber, P. Clemmensen, M. Treiman, T. Engstrøm, Exenatide reduces final infarct size in patients with ST-segment-elevation myocardial infarction and short-duration of ischemia. Circ. Cardiovasc. Interv. 5, 288–295 (2012)
J. Lønborg, N. Vejlstrup, H. Kelbæk, H.E. Bøtker, W.Y. Kim, A.B. Mathiasen, E. Jørgensen, S. Helqvist, K. Saunamäki, P. Clemmensen, L. Holmvang, L. Thuesen, L.R. Krusell, J.S. Jensen, L. Køber, M. Treiman, J.J. Holst, T. Engstrøm, Exenatide reduces reperfusion injury in patients with ST-segment elevation myocardial infarction. Eur. Heart J. 33, 1491–1499 (2012)
F.J. Bernink, L. Timmers, M. Diamant, M. Scholte, A.M. Beek, O. Kamp, K.M. Marques, R.N. Denham, W.J. Chen, P.A. Doevendans, A.C. van Rossum, N. van Royen, A.J. Horrevoets, Y. Appelman, Effect of additional treatment with EXenatide in patients with an acute myocardial infarction: the EXAMI study. Int. J. Cardiol. 167, 289–290 (2013)
P.A. Read, F.Z. Khan, P.M. Heck, S.P. Hoole, D.P. Dutka, DPP-4 inhibition by sitagliptin improves the myocardial response to dobutamine stress and mitigates stunning in a pilot study of patients with coronary artery disease/clinical perspective. Circ. Cardiovasc. Imaging. 3, 195–201 (2010)
H.D. Theiss, C. Brenner, M.G. Engelmann, M.M. Zaruba, B. Huber, V. Henschel, U. Mansmann, B. Wintersperger, M. Reiser, G. Steinbeck, W.M. Franz, Safety and efficacy of SITAgliptin plus GRanulocyte-colony-stimulating factor in patients suffering from acute myocardial infarction (SITAGRAMI-Trial)–rationale, design and first interim analysis. Int. J. Cardiol. 145, 282–284 (2010)
S.P. Marso, J.B. Lindsey, J.M. Stolker, J.A. House, G. Martinez Ravn, K.F. Kennedy, T.M. Jensen, J.B. Buse, Cardiovascular safety of liraglutide assessed in a patient-level pooled analysis of phase 2: 3 liraglutide clinical development studies. Diab. Vasc. Dis. Res. 8, 237–240 (2011)
S.P. Marso, N.R. Poulter, S.E. Nissen, M.A. Nauck, B. Zinman, G.H. Daniels, S. Pocock, W.M. Steinberg, R.M. Bergenstal, J.F. Mann, L.S. Ravn, K.B. Frandsen, A.C. Moses, J.B. Buse, Liraglutide effect and action in diabetes: evaluation of cardiovascular outcome and results (LEADER) trial design and methods. Am. Heart J. 166, 823–830 (2013)
M. Monami, I. Dicembrini, D. Martelli, E. Mannucci, Safety of dipeptidyl peptidase-4 inhibitors: a meta-analysis of randomized clinical trials. Curr. Med. Res. Opin. 27(Suppl 3), 57–64 (2011)
M. Monami, I. Dicembrini, C. Nardini, I. Fiordelli, E. Mannucci, Effects of glucagon-like peptide-1 receptor agonists on cardiovascular risk: a meta-analysis of randomized clinical trials. Diabetes Obes. Metab. 39–47, 109 (2014)
W.B. White, C.P. Cannon, S.R. Heller, Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl. J. Med. 369, 1327–1335 (2013)
B.M. Scirica, D.L. Bhatt, E. Braunwald, Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. M N Engl J Med 369, 1317–1326 (2013)
M.E. Cobble, R. Frederich, Saxagliptin for the treatment of type 2 diabetes mellitus: assessing cardiovascular data. Cardiovasc. Diabetol. 11, 6 (2012)
W.B. White, R. Pratley, P. Fleck, M. Munsaka, M. Hisada, C. Wilson, V. Me-non, Cardiovascular safety of the dipetidyl peptidase-4 inhibitor alogliptin in type 2 diabetes mellitus. Diabetes Obes. Metab. 15, 668–673 (2013)
N. Mikhail, Effects of incretin-based therapy in patients with heart failure and myocardial infarction. Endocrine. (2014) [Epub ahead of print]
R. Retnakaran, C.A. Cull, K.I. Thorne, A.I. Adler, R.R. Holman, UKPDS Study Group, Risk factors for renal dysfunction in type 2 diabetes: U.K. Prospective Diabetes Study 74. Diabetes 55, 1832–1839 (2006)
J.A. Davidson, J. Brett, A. Falahati, D. Scott, Mild renal impairment has no effect on the efficacy and safety of liraglutide. Endocr. Pract. 6, 1–31 (2010)
W.J. Weise, M.S. Sivanandy, C.A. Block, R.J. Comi, Exenatide-associated ischemic renal failure. Diabetes Care 32, e22–e23 (2009)
B. Kuehn, Exenatide and kidney function. JAMA 302, 2644 (2009)
C.B. Giorda, E. Nada, B. Tartaglino, Pharmacokinetics, safety, and efficacy of DPP-4 inhibitors and GLP-1 receptor agonists in patients with type 2 diabetes mellitus and renal or hepatic impairment. A systematic review of the literature. Endocrine. (2014) [Epub ahead of print]
A.E. Butler, M. Campbell-Thompson, T. Gurlo, D.W. Dawson, M. Atkin-son, P.C. Butler, Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes 62, 2595–2604 (2013)
EMA statement Investigation into GLP-1-based diabetes therapies con-cluded. http://www.ema.europa.eu/ema/index.jsp?curl=pages/news_and_events/news/2013/07/news_detail_001856.jsp&mid=WC0b01ac058004d5c1. Accessed 13 Sept 2013
NIDDK-NCI Workshop on Pancreatitis-Diabetes-Pancreatic Cancer. http://www2.niddk.nih.gov/News/Calendar/PDPC2013.htm. Accessed 13 Sept 2013
S.E. Kahn, Incretin therapy and islet pathology—a time for caution. Diabetes 62, 2178–2180 (2013)
S. Bonner-Weir, P. In’t Veld, G. Weir, Re-analysis of study of pancre-atic effects of incretin therapy: Methodological deficiencies. Diabetes Obes. Metab. (2014). doi:10.1111/dom.12257
A.J. Williams, S.L. Thrower, I.M. Sequeiros, A. Ward, A.S. Bickerton, J.M. Triay, M.P. Callaway, C.M. Dayan, Pancreatic volume is reduced in adult patients with recently diagnosed type 1 diabetes. J. Clin. Endocrinol. Metab. 97, E2109–E2113 (2012)
A.J. Williams, W. Chau, M.P. Callaway, C.M. Dayan, Magnetic resonance imaging: a reliable method for measuring pancreatic volume in type 1 diabetes. Diabet. Med. 24, 35–40 (2007)
S.S. Engel, E. Round, G.T. Golm, K.D. Kaufman, B.J. Goldstein, Safety and tolerability of sitagliptin in type 2 diabetes: pooled analysis of 25 clinical studies. Diabetes Ther. 4, 119–145 (2013)
C. Alves, F. Batel-Marques, A.F. Macedo, A meta-analysis of serious adverse events reported with exenatide and liraglutide: acute pancreatitis and cancer. Diabetes Res. Clin. Pract. 98, 271–284 (2012)
D.D. Dore, J.D. Seegerac, K.A. Chanac, Use of a claims-based active drug safety surveillance system to assess the risk of acute pancreatitis with exenatide or sitagliptin compared to metformin or glyburide. Curr. Med. Res. Opin. 25, 1019–1102 (2009)
E. Garg, W. Chen, M. Pendergrass, Acute pancreatitis in type 2 diabetes treated with exenatide or sitagliptin. A retrospective observational pharmacy claims analysis. Diabetes Care 33, 2349–2354 (2010)
M. Wenten, J.A. Gaebler, M. Hussein, E.M. Pelletier, D.B. Smith, P. Girase, R.A. Noel, D.K. Braun, G.L. Bloomgren, Relative risk of acute pancreatitis in initiators of exenatide twice daily compared with other anti-diabetic medication: a follow-up study. Diabet. Med. 29, 1412–1418 (2012)
Conflict of interests
The author has attended Advisory Boards for AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly & Co, Novartis, Novo Nordisk, Roche, Merck & Co; has received Research Support from AstraZeneca, Boehringer Ingelheim, Eli Lilly & Co, Novartis, Novo Nordisk; has attended Speaker’s Bureaux for AstraZeneca, Berlin Chemie AG, Bristol-Myers Squibb, Boehringer Ingelheim, Eli Lilly & Co, Merck & Co, Novartis, Novo Nordisk, Roche, Sanofi, and Takeda.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gallwitz, B. Extra-pancreatic effects of incretin-based therapies. Endocrine 47, 360–371 (2014). https://doi.org/10.1007/s12020-014-0223-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-014-0223-0