Abstract
Increasing evidence suggests that 25-hydroxyvitamin D [25(OH)D] and parathyroid hormone (PTH) levels are associated with metabolic syndrome (MetS). In 2010, we explored the association of serum 25(OH)D and PTH levels with MetS in 1,390 Chinese participants, aged 20–83 years. Anthropometric phenotypes, blood pressure, and the incidence of MetS were evaluated. In addition, serum lipids, 25(OH)D, and PTH were measured. The median concentration of 25(OH)D and PTH were 55.3 nmol/l and 2.8 pmol/l, respectively. The prevalence of vitamin D deficiency (<50 nmol/l) was 39.9 %, with 34.5 % in men and 47.8 % in women. After accounting for confounding factors and serum PTH, a 10 nmol/l higher serum 25(OH)D level was associated with a 10 % lower risk of MetS (OR = 0.90, 95 % CI 0.84–0.96, P = 0.0007). Furthermore, participants with vitamin D sufficiency had a 35 % lower risk of MetS than those with vitamin D deficiency (OR = 0.65, 95 % CI 0.51–0.84, P = 0.0009). PTH was not associated with the risk of MetS after adjustment for confounding factors. These results were confirmed in both men and women. Thus in this cohort of Chinese individuals, vitamin D deficiency is common and optimal vitamin D level is inversely associated with MetS, independent of several confounders and PTH level. The clinical significance of these findings warrants further study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome (MetS) is characterized by a set of cardiovascular risk factors, including abdominal obesity, raised blood pressure, atherogenic dyslipidemia, insulin resistance, and glucose intolerance. MetS is associated with an increased risk of diabetes, cardiovascular diseases, and mortality [1–4]. Vitamin D, a fat-soluble vitamin produced in skin following sun exposure and retrieved from diet and supplementation, has been widely related to insulin resistance, obesity, hypertension, MetS, dyslipidemia, diabetes mellitus, and mortality [5–9]. Increasing evidence suggests that vitamin D deficiency may be a novel risk factor for MetS. Although recent studies have shown that 25(OH)D level is inversely associated with MetS components or risk of MetS in obese subjects or general population [9–16], other studies have produced conflicting results [17–19]. In addition, some studies showing significant association between vitamin D and risk of MetS have failed to adjust for serum PTH [10, 11, 15], an important calcium-regulating hormone. Actually, some studies have indicated that serum PTH is positively correlated with MetS components and risk of MetS, even in normal PTH range [12, 17, 19–21]. However, other studies report no significant association between PTH and MetS [9, 13, 14, 16, 18]. Furthermore, no epidemiologic study of MetS has examined both serum vitamin D and PTH levels in the Chinese population.
With the rapid growth of economy and unfavorable lifestyle changes in its population during recent decades, China is experiencing MetS epidemic and increased incidence of related cardiovascular diseases. Data from the InterASIA study reveal that 64 million (or 13.7 %) Chinese adults aged 35–74 years have MetS as defined by the U.S. National Cholesterol Education Program’s Adult Treatment Panel III (ATP III) [22]; in addition, the age-standardized prevalence of MetS as defined by the International Diabetes Federation (IDF) and revised-ATP III definitions are 16.5 and 23.3 %, respectively [23]. We hypothesized that vitamin D deficiency and increased PTH level are associated with MetS in the Chinese population. We measured 25-hydroxyvitamin D [25(OH)D] level in our subjects since this is the main storage form of vitamin D in the body and the most commonly used marker to evaluate vitamin D status [24]. Then, we conducted this cross-sectional study to evaluate the association of serum 25(OH)D and PTH levels with MetS components and risk of MetS in the Chinese population.
Research design and methods
Population
The present analysis was based on a cross-sectional study involving comprehensive cardiovascular health examinations for all employees of a factory in Dali, Yunnan Province (latitude 25° north). We invited all employees and retired workers to take part in this study from March to May 2010. All employees and retired workers were in the same social class. We did not apply any inclusion or exclusion criteria for our study. Of the 1,643 eligible individuals, 1,443 (87.8 %) agreed to participate in the study. In addition, 53 participants were excluded because of inadequate blood sample to test for 25(OH)D or PTH levels, or lack of demographic data. Thus, a total of 1,390 participants were included in the present analysis. All subjects gave written informed consent. The study protocol was approved by the Ethics Committee of the Affiliated Hospital of Dali University.
Data collection
One physician measured each participant’s blood pressure three times consecutively using an automatic blood pressure monitor (Omron HEM 7011, Japan), after the subjects have rested for at least 5 min in the sitting position. The three blood pressure readings were averaged for analysis. The same observer also administered a standardized questionnaire to collect information on medical history, smoking habits, alcohol consumption, and the use of medications. Hypertension was defined as sitting systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, or current taking of antihypertensive drugs. Diabetes mellitus was defined as a fasting blood glucose ≥7.0 mmol/l, or as current use of oral hypoglycemic agents or insulin. Current smoking was defined as at least 1 cigarette smoked per day. Current alcohol intake was defined as consumption of at least 1 drink per week. A trained technician performed anthropometric measurements, including body height, body weight, and waist and hip circumferences. Body weight and body height were measured with the participant barefoot and wearing light clothes. Body mass index was calculated as body weight in kilograms divided by body height in meters. Waist-to-hip ratio (WHR) was defined as waist circumference divided by hip circumference. Overweight and obesity were defined as a body mass index of 25 kg/m2 and higher. Waist circumference was measured at the smallest circumference between the ribs and iliac crest, and hip circumference was measured at the maximum circumference between the iliac crest and crotch to the nearest 0.1 cm.
Laboratory methods
Venous blood samples were drawn after overnight fasting for biochemical measurements. Serum glucose was measured with a modified hexokinase enzymatic method using the Hitachi automatic clinical analyzer (Hitachi 7180, Japan). Concentrations of total cholesterol, triglycerides, and HDL cholesterol were assayed enzymatically with commercially available reagents. Serum was also stored at −30 °C for the measurement of 25(OH)D and PTH levels. Though it is recommended to store samples at −80 °C for the measurement of 25(OH)D level, studies have demonstrated the stability of 25(OH)D in serum samples under different conditions [25, 26]. Serum 25(OH)D was determined by radioimmunoassay (Diasorin Inc., Stillwater, Minnesota, USA) in the Clinical Laboratory of the Affiliated Hospital of Dali University in May, 2011. The intra- and interassay coefficients of variance were 6.0 and 5.6 %, respectively. Serum PTH was measured using the chemiluminescence method (DPC 2000, Siemens, Germany). The intra- and interassay coefficients of variance were 3.9 and 6.0 %, respectively. The analytic sensitivity of the assays for measuring serum 25(OH)D and PTH levels were 3.8 nmol/l and 0.32 pmol/l, respectively. Vitamin D deficiency was defined as having serum 25(OH)D <50 nmol/l [27]. Glomerular filtration rate (GFR) was calculated using the modification of diet in renal disease (MDRD) Study equation: GFR = 186 × (serum creatinine, mg/dl)−1.154 × (age, years)−0.203 × (0.742 if female) [28].
Definition of metabolic syndrome
Metabolic syndrome was defined according to the updated ATP III criteria for Asian Americans [29] as the presence of three or more of the following components: (1) waist circumference ≥90 cm for men or ≥80 cm for women; (2) blood pressure ≥130/85 mmHg or currently using of antihypertensive drugs; (3) triglyceride ≥1.7 mmol/l; (4) HDL cholesterol <1.03 mmol/l for men or <1.29 mmol/l for women; (5) fasting glucose ≥5.6 mmol/l or if currently using drugs to treat hyperglycemia.
Statistical analysis
For database management and statistical analysis, we used the SAS software (version 9.1.3, SAS Institute, Cary, NC). The extent of departure from normality was evaluated by Shapiro–Wilk’s test. Participant characteristics were compared by gender using the independent sample Student’s t test for continuous variables and Fisher’s exact test for categorical variables, respectively. Multivariable adjusted linear regression models were used to calculate the coefficients for MetS components with a 10 nmol/l and a 1 pmol/l increase in serum 25(OH)D and PTH levels, respectively. Unadjusted and multivariable adjusted logistic regression models were used to estimate the odds ratios (ORs) and 95 % confidence intervals (CI) for MetS. Linear regression analyses were stratified by gender; logistics regression analyses were stratified by gender and body weight status (normal weight vs. overweight/obesity). P values were two-sided, and P ≤ 0.05 was considered significant.
Results
Characteristics of the participants
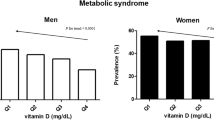
The 1,390 participants included 559 women (40.2 %), and 472 (34.0 %) hypertensive patients, of whom 211 (44.7 %) took antihypertensive drugs. Three hundred sixty six (26.3 %) individuals met the criteria for MetS, and the prevalence of MetS was similar between men and women (27.0 vs. 25.4 %, P = 0.52). The prevalence of vitamin D deficiency was 39.9 %, with 34.5 % in men and 47.8 % in women. The prevalence of MetS decreased significantly with increasing tertiles of serum 25(OH)D level in men (P = 0.004) and women (P = 0.01). However, the prevalence of MetS increased significantly with increasing tertiles of serum PTH level in women (P = 0.03) but not in men (P = 0.10) (Fig. 1).
Gender-specific prevalence of metabolic syndrome across tertiles of serum 25(OH)D and PTH levels black and gray bar represent prevalence of MetS for men and women, respectively, according to the tertiles of serum 25(OH)D (left panel) and PTH levels (right panel). P values for trends for each group are given. T1 tertile 1, T2 tertile 2, T3 tertile 3
Because vitamin D is a fat-soluble vitamin, fat distribution might be associated with vitamin D status. We also analyzed differences in serum 25(OH)D and PTH levels in subjects with android (WHR >0.9 for men and >0.85 for women, n = 563) and gynecoid fat distribution (WHR ≤0.9 for men and ≤0.85 for women, n = 827). There were significant differences in serum 25(OH)D (54.6 vs. 58.2 nmol/l, P = 0.001) and PTH (3.4 vs. 3.0 pmol/l, P = 0.001) levels between subjects with android and gynecoid fat distribution.
Table 1 shows the population characteristics by gender. Men exhibited higher values for the following parameters than women: age, body mass index, waist circumference, hip circumference, waist-to-hip ratio, systolic and diastolic blood pressure, fasting triglyceride, fasting glucose, 25(OH)D, and proportion of individuals currently consuming alcohol or cigarettes and with hypertension (P ≤ 0.04). However, men had lower HDL cholesterol, GFR and lower proportion of individuals with vitamin D deficiency (P < 0.0001) than women. Men and women had similar total cholesterol, LDL cholesterol, PTH, and similar proportion of individuals with diabetes mellitus and MetS (Table 1).
Association of serum 25(OH)D and PTH levels with MetS components
Gender-specific association of serum 25(OH)D and PTH levels with MetS components are shown in Table 2. In men, a 10 nmol/l higher serum 25(OH)D level was negatively associated with waist circumference (P = 0.02) and fasting triglyceride (P < 0.0001), and positively associated with HDL cholesterol (P = 0.004) after accounting for age, current alcohol intake, current smoking, working status, day of blood sampling, GFR, and serum PTH. A one unit higher PTH level was positively associated with diastolic blood pressure (P = 0.02) and waist circumference (P = 0.03) in multivariable adjusted analyses. In women, a 10 nmol/l higher serum 25(OH)D level was negatively associated with triglyceride level (P = 0.0002) and positively associated with HDL cholesterol level (P = 0.03), while a one unit higher PTH level was positively associated with systolic (P = 0.002) and diastolic blood pressure (P = 0.02), and negatively associated with triglyceride level (P = 0.02) in multivariable adjusted analyses.
Association of serum 25(OH)D and PTH levels with the risk of MetS
Gender-specific association of serum 25(OH)D and PTH levels with the risk of MetS are shown in Table 3. A 10 nmol/l higher serum 25(OH)D level was associated with a 10 % lower risk of MetS after adjusting for age, current alcohol intake, current smoking, working status, day of blood sampling, GFR, and serum PTH. Adjusting additionally for body mass index did not affect the strength of the association (OR = 0.88, 95 % CI 0.82–0.94, P = 0.0004). The results were confirmed in both men and women. Furthermore, participants with vitamin D sufficiency had a 35 % (OR = 0.65, 95 % CI 0.51–0.84, P = 0.0009) lower risk of MetS after multivariable adjustment than those with vitamin D deficiency. The odds ratios of MetS increased significantly with one unit increase of serum PTH level in men and women when no adjustment was applied. However, after further adjustment for covariates in the models, these associations were attenuated significantly and became statistically nonsignificant (Table 3).
We further analyzed the association of serum 25(OH)D and PTH levels with the risk of MetS according to weight status. Interestingly, a higher level of serum 25(OH)D was only associated with a lower risk of MetS in overweight/obese women (P = 0.02), but not in men or women of normal weight. A higher level of serum PTH was not associated with a higher risk of MetS in either normal weight or overweight/obese subjects (Table 4).
Discussions
Our results reveal the prevalence of vitamin D deficiency, and the negative and independent association of a higher serum 25(OH)D level with specific MetS components and the risk of MetS in the Chinese population. Though a number of MetS components were associated with serum PTH level after multivariable adjustment, there was no evidence of an association between serum PTH level and the risk of MetS. We also observed a significant gender-related difference in the association of 25(OH)D and PTH levels with MetS components.
Our finding that a higher 25(OH)D level is associated with a lower risk of MetS is consistent with most previous population studies. Among the 8,421 participants aged ≥20 years in NHANES III [10], the odds ratio for MetS among participants with the highest quintile of vitamin D compared with those in the lowest quintile was 0.49 (95 % CI 0.37–0.66) after multivariate adjustment. Among the 3,262 middle-aged and elderly Chinese enrolled from Beijing and Shanghai, Lu et al. [15] also found that vitamin D deficiency is common, and that a low 25(OH)D level is significantly associated with an increased risk of developing MetS and insulin resistance. In a study of 1,330 middle-aged Korean participants, Kim et al. [9] also found a strong inverse association of 25(OH)D with MetS.
We calculated the prevalence of MetS to be 26.3 %, which is higher than what is reported in the InterASIA study. In China, the prevalence of MetS and its major components have been rapidly rising, largely reflecting the transition in lifestyle and nutrition in the last two decades. MetS and related cardiovascular diseases have been major public health problems in China. In our study, subjects were recruited in the summer months and from low latitude areas. Thus, we expected less subjects with vitamin D deficiency due to more exposure to sun. However, vitamin D deficiency was still common in this population, especially in women and obese subjects. This is consistent with a previous Chinese study reporting poor vitamin D status in middle-aged and elderly Chinese [15]. Although little is known regarding to what extent vitamin D deficiency in our population could be explained by skin color, latitude, and/or genetic factors, plausible explanations might include: (1) use of vitamin D supplementation is rare among Chinese; (2) unlike in the western countries, Chinese people have not been exposed to vitamin D fortified food; (3) less sun exposure as the result of less outdoor activity, more air pollution, and increased sunscreen use especially for women; (4) increasing prevalence of obesity. Hence, attention should be paid to the vitamin D status of females and of individuals who are old, obese, and less physically active.
Vitamin D may modulate the risk of developing MetS and its components through several potential mechanisms. Active vitamin D can inhibit the proliferation of preadipocytes, and suppress the expression of several differentiation markers and adipogenic-related genes [30]. Meanwhile, it is known that vitamin D promotes general activation of protein synthesis in pancreatic β-cells, enhances Ca2+ influx into β-cells and stimulates the conversion of proinsulin to insulin [31, 32]. The effect of vitamin D on lipids could be via suppression of PTH secretion as PTH has been reported to reduce lipolysis at least in vitro [33]. In addition, vitamin D could influence on the lipids through an increased calcium level which may reduce hepatic triglyceride formation and/or secretion [34, 35]. Indeed, our finding that a higher 25(OH)D level is associated with a favorable lipid profile, an observation not confounded by obesity, is consistent with previous studies. Jorde et al. [36] found a significant increase in serum HDL-C level and a significant decrease in serum triglyceride level across increasing serum 25(OH)D quartiles. In a longitudinal study, an increase in serum 25(OH)D level over 14 years is associated with a significant decrease in serum triglyceride [36]. Furthermore, in a prospective study of 4,330 subjects with a 5-year follow-up, a 10 nmol/l higher baseline level of vitamin D is associated with a decrease in triglyceride and very low density lipoprotein cholesterol levels by 0.52 and 0.66 %, respectively [7].
Given that vitamin D is believed to be sequestered in fat tissue as a result of its hydrophobic nature and to not be as readily available for 25-hydroxylation as in lean individuals, some studies have corrected for body mass index in multivariable analysis of the association with MetS [12, 37]. Because central obesity is a major component of MetS, it is somewhat controversial to account for adiposity in multivariable analysis. Even if we additionally adjusted for body mass index in logistic analyses, the association between 25(OH)D and MetS did not change substantially. Thus, we confirmed that the association between 25(OH)D and MetS is independent of adiposity. We further conducted subgroup analyses according to weight status. However, a higher serum 25(OH)D level only inversely associated with MetS in overweigh/obese women, but not in men or women of normal weight.
The reason for gender difference in the prevalence of MetS across increasing tertiles of serum PTH is unknown. Although we showed that serum PTH level is significantly associated with a number of components of MetS in men or women, we could not find an independent association between serum PTH level and risk of MetS after multivariable adjustment in both men and women. Previous studies that investigated the association between PTH level and MetS provided conflicting results [12, 17–20]. Moreover, previous studies with a positive association of PTH level with MetS have been conducted in populations restricted to elderly [12, 17, 20] or obese subjects [19]. Our present study was conducted in relatively young and lean subjects, which may partly account for the difference observed in the association between PTH level and MetS. In addition, the lack of independent association between serum PTH and MetS in our study is consistent with a report in middle-aged Korean subjects [9]. Given the present inconsistencies in the literature, further study in this area is warranted.
To our knowledge, this is the first study to investigate the association of both 25(OH)D and PTH levels with MetS in the Chinese population. A strength of our study is its rapid completion, which minimized the seasonal variation of serum 25(OH)D and PTH levels. In addition, there was only one participant under calcium supplementation and none received vitamin D supplementation. However, our study has to be interpreted within the context of its limitations. First, we did not collect information on physical activity, dietary vitamin D intake, and sunlight exposure. However, we directly measured serum 25(OH)D level, an indicator of vitamin D status in the body and can reflect the cumulative effect of sunlight exposure and dietary intake of vitamin D. Second, the participants were not selected randomly from the general population. Therefore, the results may not be generalized to the general population. Third, we measured serum 25(OH)D level at only one timepoint; thus, our findings are not indicative of vitamin D status over the lifetime of the participant. Finally, our study was cross-sectional, and hence no causal inference could be taken.
Despite its limitations, our population study found that 25(OH)D is significantly and inversely associated with MetS. There is no association detected between PTH and MetS. Considering the high prevalence of MetS and vitamin D deficiency in the Chinese population, our results may have important implication for public health interventions. However, further research is needed to verify our findings.
Abbreviations
- 25(OH)D:
-
25-hydroxyvitamin D
- PTH:
-
Parathyroid hormone
- MetS:
-
Metabolic syndrome
- GFR:
-
Glomerular filtration rate
- OR:
-
Odds ratio
- 95 % CI:
-
95 % Confidence interval
References
B. Isomaa, P. Almgren, T. Tuomi, B. Forsen, K. Lahti, M. Nissen, M.R. Taskinen, L. Groop, Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 24, 683–689 (2001)
H.M. Lakka, D.E. Laaksonen, T.A. Lakka, L.K. Niskanen, E. Kumpusalo, J. Tuomilehto, J.T. Salonen, The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288, 2709–2716 (2002)
E.S. Ford, Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 28, 1769–1778 (2005)
P.W. Wilson, R.B. D’Agostino, H. Parise, L. Sullivan, J.B. Meigs, Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 112, 3066–3072 (2005)
N. Vilarrasa, J. Vendrell, J. Maravall, I. Elio, E. Solano, J.P. San, I. Garcia, N. Virgili, J. Soler, J.M. Gomez, Is plasma 25(OH)D related to adipokines, inflammatory cytokines and insulin resistance in both a healthy and morbidly obese population. Endocrine 38, 235–242 (2010)
E. Kamycheva, V. Berg, R. Jorde, Insulin-like growth factor I, growth hormone, and insulin sensitivity: the effects of a one-year cholecalciferol supplementation in middle-aged overweight and obese subjects. Endocrine (2012). [Epub ahead of print]
T. Skaaby, L.L.N. Husemoen, C. Pisinger, T. Jorgensen, B.H. Thuesen, M. Fenger, A. Linneberg, Vitamin D status and changes in cardiovascular risk factors: a prospective study of a general population. Cardiology 123, 62–70 (2012)
T. Skaaby, L.L. Husemoen, C. Pisinger, T. Jorgensen, B.H. Thuesen, M. Fenger, A. Linneberg, Vitamin D status and incident cardiovascular disease and all-cause mortality: a general population study. Endocrine (2012). [Epub ahead of print]
M.K. Kim, K.M. Il, O.K. Won, H.S. Kwon, J.H. Lee, W.C. Lee, K.H. Yoon, H.Y. Son, The association of serum vitamin D level with presence of metabolic syndrome and hypertension in middle-aged Korean subjects. Clin. Endocrinol. (Oxf) 73, 330–338 (2010)
E.S. Ford, U.A. Ajani, L.C. McGuire, S. Liu, Concentrations of serum vitamin D and the metabolic syndrome among US adults. Diabetes Care 28, 1228–1230 (2005)
J.I. Botella-Carretero, F. Alvarez-Blasco, J.J. Villafruela, J.A. Balsa, C. Vazquez, H.F. Escobar-Morreale, Vitamin D deficiency is associated with the metabolic syndrome in morbid obesity. Clin. Nutr. 26, 573–580 (2007)
J.P. Reis, D. von Mühlen, E.R. Miller III, Relation of 25-hydroxyvitamin D and parathyroid hormone levels with metabolic syndrome among US adults. Eur. J. Endocrinol. 159, 41–48 (2008)
E.S. Ford, G. Zhao, C. Li, W.S. Pearson, Serum concentrations of vitamin D and parathyroid hormone and prevalent metabolic syndrome among adults in the United States. J Diabetes 1, 296–303 (2009)
D.M. Lee, M.K. Rutter, T.W. O’Neill, S. Boonen, D. Vanderschueren, R. Bouillon, G. Bartfai, F.F. Casanueva, J.D. Finn, G. Forti, A. Giwercman, T.S. Han, I.T. Huhtaniemi, K. Kula, M.E. Lean, N. Pendleton, M. Punab, A.J. Silman, F.C. Wu, Vitamin D, parathyroid hormone and the metabolic syndrome in middle-aged and older European men. Eur. J. Endocrinol. 161, 947–954 (2009)
L. Lu, Z. Yu, A. Pan, F.B. Hu, O.H. Franco, H. Li, X. Li, X. Yang, Y. Chen, X. Lin, Plasma 25-hydroxyvitamin D concentration and metabolic syndrome among middle-aged and elderly Chinese individuals. Diabetes Care 32, 1278–1283 (2009)
S. Kayaniyil, R. Vieth, S.B. Harris, R. Retnakaran, J.A. Knight, H.C. Gerstein, B.A. Perkins, B. Zinman, A.J. Hanley, Association of 25(OH)D and PTH with metabolic syndrome and its traditional and nontraditional components. J. Clin. Endocrinol. Metab. 96, 168–175 (2011)
J.P. Reis, D. von Mühlen, D. Kritz-Silverstein, D.L. Wingard, E. Barrett-Connor, Vitamin D, parathyroid hormone levels, and the prevalence of metabolic syndrome in community-dwelling older adults. Diabetes Care 30, 1549–1555 (2007)
S. Rueda, C. Fernandez–Fernandez, F. Romero, J. de Martínez Osaba, J. Vidal, Vitamin D, PTH, and the metabolic syndrome in severely obese subjects. Obes. Surg. 18, 151–154 (2008)
J. Hjelmesaeth, D. Hofso, E.T. Aasheim, T. Jenssen, J. Moan, H. Hager, J. Roislien, J. Bollerslev, Parathyroid hormone, but not vitamin D, is associated with the metabolic syndrome in morbidly obese women and men: a cross-sectional study. Cardiovasc Diabetol 8, 7 (2009)
T. Ahlstrom, E. Hagstrom, A. Larsson, C. Rudberg, L. Lind, P. Hellman, Correlation between plasma calcium, parathyroid hormone (PTH) and the metabolic syndrome (MetS) in a community-based cohort of men and women. Clin. Endocrinol. (Oxf) 71, 673–678 (2009)
R. Jorde, J. Svartberg, J. Sundsfjord, Serum parathyroid hormone as a predictor of increase in systolic blood pressure in men. J. Hypertens. 23, 1639–1644 (2005)
D. Gu, K. Reynolds, X. Wu, J. Chen, X. Duan, R.F. Reynolds, P.K. Whelton, J. He, Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 365, 1398–1405 (2005)
W. Yang, K. Reynolds, D. Gu, J. Chen, J. He, A comparison of two proposed definitions for metabolic syndrome in the Chinese adult population. Am. J. Med. Sci. 334, 184–189 (2007)
M.F. Holick, Resurrection of vitamin D deficiency and rickets. J. Clin. Invest. 116, 2062–2072 (2006)
J.P. Wielders, F.A. Wijnberg, Preanalytical stability of 25(OH)-vitamin D3 in human blood or serum at room temperature: solid as a rock. Clin. Chem. 55, 1584–1585 (2009)
M.C. Ocke, J. Schrijver, B.G.L. Obermann-de, B.P. Bloemberg, G.R. Haenen, D. Kromhout, Stability of blood (pro)vitamins during four years of storage at −20 degrees C: consequences for epidemiologic research. J. Clin. Epidemiol. 48, 1077–1085 (1995)
A.C. Ross, J.E. Manson, S.A. Abrams, J.F. Aloia, P.M. Brannon, S.K. Clinton, R.A. Durazo-Arvizu, J.C. Gallagher, R.L. Gallo, G. Jones, C.S. Kovacs, S.T. Mayne, C.J. Rosen, S.A. Shapses, The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J. Clin. Endocrinol. Metab. 96, 53–58 (2011)
A.S. Levey, J. Coresh, E. Balk, A.T. Kausz, A. Levin, M.W. Steffes, R.J. Hogg, R.D. Perrone, J. Lau, G. Eknoyan, National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann. Intern. Med. 139, 137–147 (2003)
S.M. Grundy, J.I. Cleeman, S.R. Daniels, K.A. Donato, R.H. Eckel, B.A. Franklin, D.J. Gordon, R.M. Krauss, P.J. Savage, S.C. Smith Jr, J.A. Spertus, F. Costa, Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112, 2735–2752 (2005)
H. Zhuang, Y. Lin, G. Yang, Effects of 1,25-dihydroxyvitamin D3 on proliferation and differentiation of porcine preadipocyte in vitro. Chem. Biol. Interact. 170, 114–123 (2007)
P.M. Bourlon, B. Billaudel, A. Faure-Dussert, Influence of vitamin D3 deficiency and 1,25 dihydroxyvitamin D3 on de novo insulin biosynthesis in the islets of the rat endocrine pancreas. J. Endocrinol. 160, 87–95 (1999)
M. Kajikawa, H. Ishida, S. Fujimoto, E. Mukai, M. Nishimura, J. Fujita, Y. Tsuura, Y. Okamoto, A.W. Norman, Y. Seino, An insulinotropic effect of vitamin D analog with increasing intracellular Ca2+ concentration in pancreatic beta-cells through nongenomic signal transduction. Endocrinology 140, 4706–4712 (1999)
M.B. Zemel, H. Shi, B. Greer, D. Dirienzo, P.C. Zemel, Regulation of adiposity by dietary calcium. FASEB J. 14, 1132–1138 (2000)
A. Zittermann, S. Frisch, H.K. Berthold, C. Gotting, J. Kuhn, K. Kleesiek, P. Stehle, H. Koertke, R. Koerfer, Vitamin D supplementation enhances the beneficial effects of weight loss on cardiovascular disease risk markers. Am. J. Clin. Nutr. 89, 1321–1327 (2009)
H.J. Cho, H.C. Kang, S.A. Choi, Y.C. Ju, H.S. Lee, H.J. Park, The possible role of Ca2+ on the activation of microsomal triglyceride transfer protein in rat hepatocytes. Biol. Pharm. Bull. 28, 1418–1423 (2005)
R. Jorde, Y. Figenschau, M. Hutchinson, N. Emaus, G. Grimnes, High serum 25-hydroxyvitamin D concentrations are associated with a favorable serum lipid profile. Eur. J. Clin. Nutr. 64, 1457–1464 (2010)
J. Wortsman, L.Y. Matsuoka, T.C. Chen, Z. Lu, M.F. Holick, Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 72, 690–693 (2000)
Acknowledgments
The Chinese Ministry of Science and Technology (30960137) supported this research. The authors gratefully acknowledge the voluntary participation of all study subjects and the technical assistance of Xue-Yan Li, Xiao Dong, Xiao-Ping Wang, Yong-Lin Yang, and Shu-Huai Xu.
Conflict of interest
None of the authors have a conflict of interest with regard to the data presented in this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, LH., Yin, XY., Yao, CY. et al. Serum 25-hydroxyvitamin D, parathyroid hormone, and their association with metabolic syndrome in Chinese. Endocrine 44, 465–472 (2013). https://doi.org/10.1007/s12020-013-9885-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-013-9885-2