Abstract
The goal of the present study was to investigate changes on glucose homoeostasis and of the insulin receptor (IR) and insulin receptor substrate-1 (IRS-1) signalling in pancreatic islets from MSG-obese mice submitted to or not submitted to swim training. Swim training of 90-day-old MSG mice was used to evaluate whether signalling pathways of the IR and IRS-1 in islets are involved with the insulin resistance and glucose intolerance observed in this obese animal model. The results showed that IR tyrosine phosphorylation (pIR) was reduced by 42 % in MSG-obese mice (MSG, 6.7 ± 0.2 arbitrary units (a.u.); control, 11.5 ± 0.4 a.u.); on the other hand, exercise training increased pIR by 76 % in MSG mice without affecting control mice (MSG, 11.8 ± 0.3; control, 12.8 ± 0.2 a.u.). Although the treatment with MSG increased IRS-1 tyrosine phosphorylation (pIRS-1) by 96 % (MSG, 17.02 ± 0.6; control, 8.7 ± 0.2 a.u.), exercise training also increased it in both groups (control, 13.6 ± 0.1; MSG, 22.2 ± 1.1 a.u.). Current research shows that the practice of swim training increases the tyrosine phosphorylation of IRS-1 which can modulate the effect caused by obesity in insulin receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is becoming one of the most important increasing physiopathological conditions worldwide. Insufficient physical activity and excessive caloric intake are the causes for increasing body weight [1, 2]. The obesity produced by neonatal treatment with monosodium l-glutamate (MSG) is a major tool to study the effects of obesity on different metabolic parameters. This model is characterised by hyperinsulinaemia and higher insulin secretion [3] or early hyperglycaemia in MSG-treated mice [4, 5].
MSG-obese rodents present a severe tissue insulin resistance, which is observed as a dysfunction of the insulin receptor (IR) as well as in internal signal transduction pathways [6, 7]. When activated by insulin, the IR stimulates several intracellular substrates, such as insulin receptor substrate-1 (IRS-1), which play a key role in transmitting signals to intracellular pathways [8, 9]; multiple tyrosine residues of IRS-1 themselves are then phosphorylated by these receptors, which plays an important role in their biological function. Besides the insulin effect on peripheral tissues, mostly adipose and muscle, islet cells are directly influenced by insulin.
In recent years, autocrine effects of insulin on beta cells have remained controversial. Recently, however, a variety of new methods have been utilised to demonstrate the strong clinical importance of the autocrine actions of insulin [10, 11]. It is accepted that insulin also possesses auto- and paracrine actions in pancreatic islets cells [12]. While most of the metabolic actions of insulin are exerted in the peripheral tissues, few studies have attempted to clarify the early events in the insulin-signalling pathways. In 1995, Velloso et al. [12] showed glucose and insulin-induced phosphorylation of IRS-1 and IRS-2 in rat pancreatic islets. However, the mechanisms involved in insulin signalling in the islets are currently unknown.
Studies have shown that defects in glucose homoeostasis in obese rodents and humans are improved by exercise training [13–16]. Glucose transport stimulated by insulin in the peripheral tissues during exercise training is not increased by the expression of components of the insulin-signalling cascade but is rather due to insulin activating other insulin transduction pathways [17]. It was also reported that exercise training improves beta cell function and mass by enhancing IRS-2 expression in the islets of diabetic rats [18]. However, it is not known exactly which mechanisms of insulin signalling are involved in these effects.
In this study, we used a well-established hyperglycaemic and hyperinsulinaemic obese and insulin-resistant experimental model, MSG mice, to determine whether the signalling pathways of IR and IRS-1 in the pancreatic beta cell are involved. Swim training of MSG-induced obese mice was used to observe changes in glycaemic homoeostasis as well as insulin signalling in pancreatic islets.
Materials and methods
Animals and obesity treatment
All animal protocols were approved by the Animal Ethics Committee of the State University of Minas Gerais. Neonate male Mus musculus Swiss mice were subcutaneously injected during the first 5 days of life with MSG at a dose of 4 mg/g body mass (BM). Control animals received a saline solution. Both animal groups (15 mice from 3 litters of each group) were weaned at the 21st day of life. All animals were housed under controlled conditions in a 12 h light–dark cycle of (07:00–19:00 h) and temperature (21 ± 2 °C). Water and standard rodent chow (Nuvital–Curitiba–Brazil) were offered ad libitum.
At weaning, only males were selected for the experimental procedures. Control and MSG-obese mice were randomly chosen for exercise training.
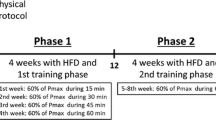
Swimming training
Control (Cont EXE) and MSG-obese (MSG EXE) mice were trained by free swimming in a glass tank (30 × 35 × 30 cm) filled with water at 32 ± 3 °C as reported by Scomparin et al. [19]. Mice were exercised for 15 min/day, three times per week over a period of 69 days. Four mice from each group were placed simultaneously into the pool at (2:00 p.m.). Additional animal groups, sedentary control and MSG-obese, did not swim (Cont SED and MSG SED, respectively).
The swimming programme should be considered a light exercise when compared to a previously reported moderate training programme in which mice freely swam for 60 min, 5 days a week, for 18 weeks [20]. After each exercise, mice were dried with paper towels and returned to their respective cages until the next swimming session as described by Andreazzi et al. [5].
Intraperitoneal glucose tolerance test (ipGTT)
ipGTT was performed by injecting glucose (2 g/kg BM) i.p. in overnight-fasted mice. Blood glucose levels were determined prior (0) to injection and 30, 60, 90, and 120 min after injection. Blood samples were obtained from the tail vein and plasmas were used to measure glucose concentration by the glucose oxidase method.
The total area-under-the-curve of ipGTT was calculated.
Assessment of obesity
All animals were weighed weekly and were killed at 90 days of age by cervical dislocation after being anaesthetised with thiopental (45 mg/kg BM). Obesity was assessed by BM and nasoanal length to calculate the rodent body mass index or Lee index. The Lee index was calculated from the ratio [BM1/3 (g)/nasoanal length (cm)] [21]. The epididymal fat was removed and weighed only for being used as a simple and reliable parameter of body fat in normal and obese rodents [22].
Pancreatic islet isolation
Isolation of pancreatic islets from mice was performed with a method adapted from one previously described [23]. Animals were deprived of food the evening before 12 h they were used for islet preparation. After anaesthesia as previously described, the abdominal wall of intact mice of all groups was cut open. A 10 ml Hank’s buffered saline solution (HBSS) containing 0.1 % collagenase type XI (Sigma Chemical Co., St. Louis, MO) was injected into the common bile duct. The pancreas, swollen with the collagenase solution, was quickly excised and incubated in a plastic culture bottle for 16 min at 37 °C. After that, 4 continuous washings were made in HBSS containing 0.12 % bovine serum albumin fraction V (BSA). Islets were collected with the aid of a microscope.
Insulin secretion stimulation
Isolated islets adapted to a baseline glucose concentration (5.6 mmol/l) were pre-incubated in 1 ml of normal Krebs–Ringer solution [(mmol/l): NaCl, 115; NaHCO3, 24; KCl, 1.6; MgCl·6H2O, 1; CaCl2·2H2O, 1; BSA, 15] containing 5.6 mmol/l glucose, for 60 min. This solution was gassed with (O2, 95 % + CO2, 5 % mixed) to maintain pH 7.4. After adaptation to low glucose concentration, islets were incubated for a further 60 min in glucose 5.6 and 16.7 with Krebs–Ringer solution. The origin of islets was from at least ten different mice to each experimental group. Aliquots from incubations were used to measure insulin concentration by RIA.
Western blotting
After isolation, groups of islets were pelleted by centrifugation at 12,000 rpm at 4 °C for 20 min and resuspended in 50–100 μl of homogenisation buffer containing protease inhibitors [24, 25]. The islets were sonicated and the total protein content was determined by the Bradford method (Bio-Rad®). Samples containing 100 mM DTT and 90 μg of protein were treated with Laemmli buffer (1 M sodium phosphate/l, pH 7.0, 0.1 % bromophenol blue, 50 % glycerol, 10 % SDS and water) and then electrophoresed on an 8 % SDS-polyacrylamide gel at 200–400 mA for 90 min. (Mini-Protein Bio-Rad®).
Electrotransfer of proteins to nitrocellulose membranes was performed in a buffer containing 25 mM Tris–Base, 192 mM glycine, 20 % methanol and SDS 0.02 % in sufficient quantity water to 1,000 ml for 2 h. After checking the transfer efficiency by Ponceau S staining, the membranes were blocked with 5 % skimmed milk in Tween-Tris buffered saline (TTBS; 10 ml of 1 M Tris–base; 30 ml of 5 M NaCl, 500 μl of Tween 20 and 1,000 ml water). The membrane was incubated with primary antibodies epitope corresponding to phosphorylated Tyr IR (pIR) and IRS-1 (pIRS-1) (both from Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA; diluted 1:1,000 in TTBS containing 1 % dry skimmed milk) overnight at 4 °C and then incubated with a horseradish peroxidase-conjugated secondary antibody for 1 h (Amersham-Pharmacia Biotech, Buckingham Shire, UK; diluted 1:10,000 in TTBS containing 1 % dry skimmed milk). The results were visualised by fluorescent immunodetection in combination with the Molecular Dynamics™ Storm™ imaging system. Band intensities were quantified by optical densitometry (Hoefer Scientific Instruments, GS300). The β-actin protein (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA; diluted 1:1,000 in TTBS containing 1 % dry skimmed milk) was used for normalisation.
Statistical analysis
Results are reported as mean ± SEM and were analysed with Student’s t tests or one-way analysis of variance (ANOVA), followed by Bonferroni’s post hoc tests. p values less than 0.05 were considered statistically significant. Tests were performed using GraphPad Prism version 5.0 for Windows (GraphPad Software®).
Results
The evolution of BM from 21 to 90 days of age, the Lee index and epididymal fat pads show that the neonatal MSG treatment was effective at inducing obesity in mice, as shown in Fig. 1A–C, respectively. Area-under-the-curve (AUC) analysis shows that the MSG SED group was 28 % smaller than the Cont SED group, whereas the MSG EXE group was 27 % smaller when compared to the MSG SED group (inset of Fig. 1A, p < 0.001). The MSG-treated SED group shows increase in epididymal fat pad, twofold more than CON SED group (p < 0.0001).
Assessment of obesity: symbols represent mean ± SEM of BM (A), Lee index (B) from weaning to adulthood and epididymal fat (C), of sedentary and training MSG-obese and control mice obtained with 15 animals for each group. Inset in (A) represents the area-under-the-curve of BM from 21 to 90 days of age. Letters over the bars represent statistical differences (p < 0.001) by one-way ANOVA among a control SED, b MSG SED, c control EXE, d MSG EXE
Figure 2 shows the effect of swim training on fasting plasma glucose (Fig. 2A) and insulin (Fig. 2B) concentrations. MSG treatment leads to increases in basal glucose (140.0 ± 1.8 mg/dl, MSG SED) and insulin (2.3 ± 0.1 ng/ml, MSG SED) of 9 and 139 %, respectively, when compared to the Cont SED group, basal glucose (127.9 ± 1.2 mg/dl) and insulin (0.9 ± 0.04 ng/ml). While exercise did not change fasting glucose levels of MSG-untreated mice, it decreased fasting glycaemia by 22 % (109.2 ± 0.9 mg/dl, MSG EXE) and fasting insulin by 39 % (13.9 ± 0.2 ng/ml, MSG EXE) in trained MSG mice compared to sedentary MSG mice (p < 0.001). Cont EXE group showed that basal glucose (125.4 ± 1.04 mg/dl) and fast insulin (0.89 ± 0.05 ng/dl) compared with the Cont SED group decrease of 1.95 and 6.08 %, respectively, were not significant.
Assessment of glucose homoeostasis: fasting glucose (A) and fasting insulin (B) from sedentary and swimming MSG-treated and control mice at 90 days of age for 15 animals in each group. Letters over the bars represent statistical differences (p < 0.001) by one-way ANOVA among a control SED, b MSG SED, c control EXE, d MSG EXE
Glucose concentrations during the ipGTT were not significantly affected by exercise training in lean animals (Cont EXE, 391 ± 14.42 mg/dl−120 min; Fig. 3a) when compared to sedentary animals (AUC of Cont SED, 369.1 ± 7.96 mg/dl−120 min). AUC during the ipGTT from the MSG SED group was 56.5 % higher than that of Cont SED group; nevertheless, exercise training reduced it by 42 % (exercised MSG mice, 335.5 ± 13.13 mg/dl−120 min, p < 0.001), when compared to untrained MSG mice, (Fig. 3b).
Glucose tolerance test: symbols represent mean ± SEM of glycaemia during the ipGTT from sedentary and training control mice (a) and MSG-obese mice (b) for 15 animals in each group. Insets in the each figure represent the respective areas-under-the-curve of glycaemia. *p < 0.001 from Student’s t test
When the islets were stimulated with low concentrations of glucose, insulin release was lower in Cont SED group compared to other groups, as shown in Fig. 4. When glucose concentration was increased from 5.6 to 16.7 mM, islets from all groups responded by secreting more insulin. While islets from Cont and MSG sedentary mice do not show different response to high glucose (16.7 mM), exercise training induced 128 % increase in insulin release only to MSG islets (p < 0.001).
Effect of MSG treatment and swimming on insulin secretion stimulated by low (5.6 mM) and high (16.7 mM) glucose concentration. Islets were obtained from a pool of 10 mice for each group. Bars represent mean of 20–40 batches of islets. Letters over the bars represent statistical differences (p < 0.001) by one-way ANOVA among a control SED, b MSG SED, c control EXE, d MSG EXE. Asterisk represents significant differences between insulin secretion induced by 5.6–16.7 mM for each group
While MSG treatment reduced pIR by 42 %, pIRS-1 was increased by 95 % compared to value of control mice (11.5 ± 0.4 and 8.7 ± 0.2 arbitrary units (a.u.), respectively), as shown in Fig. 5A and B. Exercise training was able to increase pIR by 76 % in MSG mice; on other hand, pIRS-1 was increased by 30 % in exercised MSG mice (p < 0.001). While swim training did not change pIR in control mice, pIRS-1 was enhanced by 55 % (13.6 ± 0.1 a.u., p < 0.001).
Expression of phosphorylated IR and IRS-1 in islets from mice: bars represent mean ± SEM of the density of expression of phosphorylated IR (A) and IRS-1 (B) by IB in pancreatic islets from sedentary and training control and MSG-obese mice isolated from 15 animals for each group. Letters over the bars represent statistical differences (p < 0.001) by one-way ANOVA among a control SED, b MSG SED, c control EXE, d MSG EXE. IB immunoblotting
Discussion
Biometric results confirm that MSG treatment was able to induce obesity in mice in adult life. As shown previously by our laboratory [4, 5, 19] and others [26, 27], fasting glucose and insulin were higher in MSG-mediated obese mice. Exercise training normalised both insulinaemia and glycaemia as previously reported [5, 21–28]. Sedentary MSG-obese mice were highly glucose intolerant, which is attributed to impaired insulin tissue sensitivity. It has been shown that insulin resistance is an important factor in development of type 2 diabetes, as observed in the MSG experimental model [29]. Peripheral insulin resistance in obesity demands an extreme effort of β-cells to produce and release increasing amounts of insulin despite ineffective normalisation of glycaemia.
Glycaemia of the lean exercised mice during the glucose tolerance test was not altered; however in MSG-obese mice, the fasting values were reduced by swim training. In this study, we showed that swim training is effective in the maintenance of glucose homoeostasis; as has been reported previously, insulin resistance and glucose tolerance are improved by exercise training on rodents [19, 30, 31].
In this study, the exercise effect confirms what was recently shown by our laboratory, i.e. a low-intensity swimming programme is effective at inhibiting MSG-mediated obesity in adult mice [4, 5, 19]. It is well documented that human beings and animals with metabolic syndrome undergoing physical exercise improve their blood insulin and glucose levels [32–34]. Nevertheless, with regard to the benefits of physical exercise, the mechanisms involved in the improvement of metabolism are still unclear. Although many studies have attempted to explain the mechanisms underlying exercise effects on insulin action in peripheral tissues, the effect of autocrine insulin action has not been studied. We suggest that the reduction of insulin plasma levels in MSG-trained mice is due to both improved insulin sensitivity in peripheral tissues and effect on beta cells by increasing IR phosphorylation. Insulin binds to pancreatic islet cells [35], including beta cells [36]. IR phosphorylation was observed in beta cells [12], as well as other steps of the insulin-signalling pathway [6, 37, 38]. IR phosphorylation and downstream signal transduction in pancreatic beta cells induces activation of several genes such as mammalian target of rapamycin (mTOR), which is involved in protein biosynthesis [39]. Our data do not allow us to support the discussion about insulin biosynthesis and/or β-cell mass regulation in the MSG-obese mice, but suggest that there is an adaptation on activity of IR which down regulated the IR activity to guarantee the MSG-obese β-cell survival/preservation because its hyperinsulaemia associated to strong demand due to glucose intolerance, peripheral insulin resistance [40–43] and the high cholinergic stimulation by the parasympathetic tonus observed in this model [4, 44, 45]. In islets from MSG-obese mice, we find low pIR; however, pIRS-1 was increased. These results indicate that MSG-obese mice have lower insulin sensitivity in islets, which could be due to high activation of the intracellular signalling cascade of insulin because it was shown that protein c-Jun N-terminal kinase (JNK) was elevated in tissues from obese rodents [46]. The dysfunction in the insulin-signalling cascade could impair the insulin-induced IRS-1 phosphorylation thereby attenuating insulin sensitivity [47, 48]. It has been shown that in the obesity, insulin resistance is associated with higher phosphorylation of serine residues of IRS-1 [49, 50]. Insulin resistance in obese rodents is accompanied by hyperinsulinaemia in combination with glucose intolerance and defective insulin secretion [3, 5, 26, 51–53]. Besides a possible metabolic adaptation to preserve the β-cell in pancreatic islets suggested by our data, we do not exclude that the possibility of the lower tyrosine phosphorylated IR in islets from MSG-obese mice may be due to a higher serine phosphorylation by inflammatory processes caused by high fat accumulation [54, 55].
In type 2 diabetes, the pancreatic islets become unable to respond to increased insulin demand, secreting more and more insulin to overcome the prevailing insulin resistance [56]. However, the swim training increases pIR from MSG-obese mice compared to control mice, which maintains normal pancreatic islet sensitivity to insulin action, thereby allowing the β-cells to respond properly to the stimuli to secrete insulin. The suggested mechanism can explain, at least in part, how exercise improves and/or protects pancreatic β-cell function. Despite the exercise effect on the insulin secretion and/or biosynthesis, the glucose also exerts a positive effect on this mechanism. We speculate that there is an opposite metabolic adaptation, in which glucose has any role on overcoming the downstream signals of IRS-1 for maintaining the storage of insulin to guarantee the high plasma insulin demand, once it is known that glucose per se in elevated concentrations has a regulatory effect on insulin secretion/biosynthesis [12, 56, 57]. Furthermore, we know the MSG-obese rats are very long hyperglycaemic which allow us to suggest that the high glucose levels exert any programmed stimulatory effect on IRS-1 activation in β-cell to maintain the insulin levels needed to peripheral glucose uptake. In this situation the exercise training has no beneficial impact on β-cell preservation, once it rises the phosphorylation of IRS-1.
Recently, we showed that glucose intolerance and insulin secretion in MSG-obese mice is improved by swim training [4, 5, 26]. It has been well established either in humans and experimental animals with type 2 diabetes that regular physical exercise enhances glucose-stimulated insulin secretion [14, 16, 58, 59] by improving peripheral insulin sensitivity [60, 61]. Beyond the peripheral effect of exercise, it has been shown that physical exercise improves β-cell function and mass by enhanced IRS-2 expression in islets of diabetic rats [18]. Although the magnitude of the increased pIRS-1 from exercised control mice was higher than MSG mice, we have shown that exercise was effective at improving pIRS-1 in isolated islets from both experimental groups, which suggests that exercise training can ameliorate pancreatic β-cell function, including insulin biosynthesis [62]. It is not surprising that insulin secretion stimulated by glucose is enhanced in islets isolated from control and exercised mice [5]. It may explain the higher pIRS-1 in the sedentary MSG-obese as a protective modulation to guarantee the insulin stores by a positive feedback mechanism [63]. In fact, it was reported that high IRS-1 activation is a protective mechanism for insulin stores from β-cells to guarantee that insulin would be synthesised and/or secreted [10]. Indeed, our results showed that exercise training used in the current work induced extra insulin release from islets of MSG mice. It must highlight that sedentary MSG mice have difficulty in secreting insulin when islets were stimulated by high glucose concentration. It has been shown that poor insulin secretion in postprandial situation is a signal to type 2 diabetes [56]. The data from insulin secretion can be associated to protein expression of IRS-1 which improves glucose-induced insulin secretion process. To our knowledge, this is the first time that results, presented in the current work, state that there is a positive effect produced by exercise on the correlation between insulin transduction in β-cells and insulin secretion. We conclude that obesity has harmful effects on the IRs of pancreatic islets by reducing their tyrosine phosphorylation, and exercise training can modulate this effect. We suggest that further studies must be performed to clarify what mechanisms in pancreatic β-cells are underlying the insulin deregulation in obesity and how the exercise training effects are involved with these mechanisms.
References
R.A. Winett, D.F. Tate, E.S. Anderson, J.R. Wojcik, S.G. Winett, Long-term weight gain prevention: a theoretically based internet approach. Prev. Med. 41, 629–641 (2005)
S.M. Phillips, L.G. Bandini, E.N. Naumova, H. Cyr, S. Colclough, W.H. Dietz, A. Must, Energy-dense snack food intake in adolescence: longitudinal relationship to weight and fatness. Obes. Res. 12, 461–472 (2004)
S. Grassiolli, C. Gravena, P.C. de Freitas Mathias, Muscarinic m2 receptor is active on pancreatic islets from hypothalamic obese rat. Eur. J. Pharmacol. 556, 223–228 (2007)
D.X. Scomparin, R.M. Gomes, S. Grassiolli, W. Rinaldi, A.G. Martins, J.C. de Oliveira, C. Gravena, P.C. de Freitas Mathias, Autonomic activity and glycemic homeostasis are maintained by precocious and low intensity training exercises in msg-programmed obese mice. Endocrine 36, 510–517 (2009)
A.E. Andreazzi, D.X. Scomparin, F.P. Mesquita, S.L. Balbo, C. Gravena, J.C. De Oliveira, W. Rinaldi, R.M. Garcia, S. Grassiolli, P.C. Mathias, Swimming exercise at weaning improves glycemic control and inhibits the onset of monosodium l-glutamate-obesity in mice. J. Endocrinol. 201, 351–359 (2009)
H. Tilg, A.R. Moschen, Inflammatory mechanisms in the regulation of insulin resistance. Mol. Med. 14, 222–231 (2008)
K.E. Wellen, G.S. Hotamisligil, Inflammation, stress, and diabetes. J. Clin. Invest. 115, 1111–1119 (2005)
X.J. Sun, P. Rothenberg, C.R. Kahn, J.M. Backer, E. Araki, P.A. Wilden, D.A. Cahill, B.J. Goldstein, M.F. White, Structure of the insulin receptor substrate irs-1 defines a unique signal transduction protein. Nature 352, 73–77 (1991)
M.G. Myers Jr., M.F. White, The new elements of insulin signaling. Insulin receptor substrate-1 and proteins with sh2 domains. Diabetes 42, 643–650 (1993)
C.A. Aspinwall, W.J. Qian, M.G. Roper, R.N. Kulkarni, C.R. Kahn, R.T. Kennedy, Roles of insulin receptor substrate-1, phosphatidylinositol 3-kinase, and release of intracellular Ca2+ stores in insulin-stimulated insulin secretion in beta-cells. J. Biol. Chem. 275, 22331–22338 (2000)
H. Gazzano, P. Halban, M. Prentki, R. Ballotti, D. Brandenburg, M. Fehlmann, E. Van Obberghen, Identification of functional insulin receptors on membranes from an insulin-producing cell line (rinm5f). Biochem. J. 226, 867–872 (1985)
L.A. Velloso, E.M. Carneiro, S.C. Crepaldi, A.C. Boschero, M.J. Saad, Glucose- and insulin-induced phosphorylation of the insulin receptor and its primary substrates irs-1 and irs-2 in rat pancreatic islets. FEBS Lett. 377, 353–357 (1995)
J.A. Houmard, C.J. Tanner, C.A. Slentz, B.D. Duscha, J.S. McCartney, W.E. Kraus, Effect of the volume and intensity of exercise training on insulin sensitivity. J. Appl. Physiol. 96, 101–106 (2004)
P.A. Farrell, A.L. Caston, D. Rodd, Changes in insulin response to glucose after exercise training in partially pancreatectomized rats. J. Appl. Physiol. 70, 1563–1568 (1991)
F. Dela, K.J. Mikines, B. Tronier, H. Galbo, Diminished arginine-stimulated insulin secretion in trained men. J. Appl. Physiol. 69, 261–267 (1990)
C.R. Bruce, A.D. Kriketos, G.J. Cooney, J.A. Hawley, Disassociation of muscle triglyceride content and insulin sensitivity after exercise training in patients with type 2 diabetes. Diabetologia 47, 23–30 (2004)
B.B. Yaspelkis 3rd, S.J. Lessard, D.W. Reeder, J.J. Limon, M. Saito, D.A. Rivas, I. Kvasha, J.A. Hawley, Exercise reverses high-fat diet-induced impairments on compartmentalization and activation of components of the insulin-signaling cascade in skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 293, E941–E949 (2007)
S. Park, S.M. Hong, S.R. Sung, Exendin-4 and exercise promotes beta-cell function and mass through irs2 induction in islets of diabetic rats. Life Sci. 82, 503–511 (2008)
D.X. Scomparin, S. Grassiolli, A.C. Marcal, C. Gravena, A.E. Andreazzi, P.C. Mathias, Swim training applied at early age is critical to adrenal medulla catecholamine content and to attenuate monosodium l-glutamate-obesity onset in mice. Life Sci. 79, 2151–2156 (2006)
C. Napoli, S. Williams-Ignarro, F. De Nigris, L.O. Lerman, L. Rossi, C. Guarino, G. Mansueto, F. Di Tuoro, O. Pignalosa, G. De Rosa, V. Sica, L.J. Ignarro, Long-term combined beneficial effects of physical training and metabolic treatment on atherosclerosis in hypercholesterolemic mice. Proc. Natl. Acad. Sci. USA 101, 8797–8802 (2004)
L. Bernardi, B. Patterso, Correlation between lee index and carcass fat content in weanling and adult female rats with hypothalamic lesions. J. Endocrinol. 40, 527 (1968)
P. Rogers, G.P. Webb, Estimation of body fat in normal and obese mice. Br. J. Nutr. 43(1), 83–86 (1980)
C. Gravena, P.C. Mathias, S.J.H. Ashcroft, Acute effects of fatty acids on insulin secretion from rat and human islets of langerhans. J. Endocrinol. 173, 73–80 (2002)
M.E.C. Amaral, M. Ueno, J.B. Carvalheira, E.M. Carneiro, L.A. Velloso, M.J.A. Saad, A.C. Boschero, Prolactin-signal transduction in neonatal rat pancreatic islets and interaction with the insulin-signaling pathway. Horm. Metab. Res. 35, 282–289 (2003)
G.G. Kelley, K.C. Zawalich, W.S. Zawalich, Synergistic interaction of glucose and neurohumoral agonists to stimulate islet phosphoinositide hydrolysis. Am. J. Physiol. 269, E575–E582M (1995)
J.E. Barnhart, W.J. Pizzi, The monosodium l-glutamate (msg) syndrome in mice develops independently of housing condition. Neurobehav. Toxicol. Teratol. 4, 549–556 (1982)
L. Maletinska, R.S. Toma, Z. Pirnik, A. Kiss, J. Slaninova, M. Haluzik, B. Zelezna, Effect of cholecystokinin on feeding is attenuated in monosodium glutamate obese mice. Regul. Pept. 136, 58–63 (2006)
N. Musi, L.J. Goodyear, Insulin resistance and improvements in signal transduction. Endocrine 29, 73–80 (2006)
J.F. Morrison, S. Shehab, R. Sheen, S. Dhanasekaran, M. Shaffiullah, E. Mensah-Brown, Sensory and autonomic nerve changes in the monosodium glutamate-treated rat: a model of type ii diabetes. Exp. Physiol. 93, 213–222 (2008)
M.A. de Mello, C.T. de Souza, L.R. Braga, J.W. dos Santos, I.A. Ribeiro, C.A. Gobatto, Glucose tolerance and insulin action in monosodium glutamate (msg) obese exercise-trained rats. Physiol. Chem. Phys. Med. NMR 33, 63–71 (2001)
G.P. Nassis, K. Papantakou, K. Skenderi, M. Triandafillopoulou, S.A. Kavouras, M. Yannakoulia, G.P. Chrousos, L.S. Sidossis, Aerobic exercise training improves insulin sensitivity without changes in body weight, body fat, adiponectin, and inflammatory markers in overweight and obese girls. Metabolism 54, 1472–1479 (2005)
A.J. Scheurink, A.B. Steffens, B. Roossien, B. Balkan, Sympathoadrenal function in genetically obese zucker rats. Physiol. Behav. 52, 679–685 (1992)
W.M. Sherman, J.E. Friedman, J.P. Gao, M.J. Reed, C.W. Elton, G.L. Dohm, Glycemia and exercise training alter glucose transport and glut4 in the zucker rat. Med. Sci. Sports Exerc. 25, 341–348 (1993)
R. Ross, I. Janssen, J. Dawson, A.M. Kungl, J.L. Kuk, S.L. Wong, T.B. Nguyen-Duy, S. Lee, K. Kilpatrick, R. Hudson, Exercise-induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes. Res. 12, 789–798 (2004)
E.J. Verspohl, H.P. Ammon, Binding of insulin to rat pancreatic islets: comparison between pancreatic human insulin and biosynthetic human insulin. Diabetes Care 4, 252–253 (1981)
Y.C. Patel, M. Amherdt, L. Orci, Quantitative electron microscopic autoradiography of insulin, glucagon, and somatostatin binding sites on islets. Science 217, 1155–1156 (1982)
P. Bevan, Insulin signalling. J. Cell Sci. 114, 1429–1430 (2001)
J.E. Pessin, A.R. Saltiel, Signaling pathways in insulin action: molecular targets of insulin resistance. J. Clin. Invest. 106, 165–169 (2000)
E. Jacinto, M.N. Hall, Tor signalling in bugs, brain and brawn. Nat. Rev. Mol. Cell Biol. 4, 117–126 (2003)
L.A. Campfield, F.J. Smith, J.E. Settle, R. Sohaey, Effect of the order of application of neural inputs on insulin secretion. Adv. Exp. Med. Biol. 211, 343–349 (1986)
T. Yamamoto, S. Matsuo, Y. Ueshima, F. Inoue, A. Kinugasa, T. Sawada, Plasma levels of insulin-like growth factor-i are reduced at one week of age in monosodium l-glutamate-treated mice. Endocr. J. 40, 461–465 (1993)
S.C. Blair, I.D. Caterson, G.J. Cooney, Insulin response to an intravenous glucose load during development of obesity in gold thioglucose-injected mice. Diabetes 42, 1153–1158 (1993)
A.E. Hirata, I.S. Andrade, P. Vaskevicius, M.S. Dolnikoff, Monosodium glutamate (msg)-obese rats develop glucose intolerance and insulin resistance to peripheral glucose uptake. Braz. J. Med. Biol. Res. 30, 671–674 (1997)
S.L. Balbo, M.L. Bonfleur, E.M. Carneiro, M.E. Amaral, E. Filiputti, P.C. Mathias, Parasympathetic activity changes insulin response to glucose and neurotransmitters. Diabetes Metab. 28, 3S13–3S17 (discussion 13S108-112) (2002)
D.X. Scomparin, S. Grassiolli, R.M. Gomes, R. Torrezan, J.C. de Oliveira, C. Gravena, C.C. Pera, P.C. Mathias, Low-intensity swimming training after weaning improves glucose and lipid homeostasis in msg hypothalamic obese mice. Endocr. Res. 36, 83–90 (2011)
B.L. Bennett, Y. Satoh, A.J. Lewis, Jnk: a new therapeutic target for diabetes. Curr. Opin. Pharmacol. 3, 420–425 (2003)
J. Hirosumi, G. Tuncman, L. Chang, C.Z. Gorgun, K.T. Uysal, K. Maeda, M. Karin, G.S. Hotamisligil, A central role for jnk in obesity and insulin resistance. Nature 420, 333–336 (2002)
V. Aguirre, T. Uchida, L. Yenush, R. Davis, M.F. White, The c-jun nh(2)-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of ser(307). J. Biol. Chem. 275, 9047–9054 (2000)
F. Tremblay, S. Brule, S. Hee Um, Y. Li, K. Masuda, M. Roden, X.J. Sun, M. Krebs, R.D. Polakiewicz, G. Thomas, A. Marette, Identification of irs-1 ser-1101 as a target of s6k1 in nutrient- and obesity-induced insulin resistance. Proc. Natl. Acad. Sci. USA 104, 14056–14061 (2007)
J. Zhang, Z. Gao, J. Yin, M.J. Quon, J. Ye, S6k directly phosphorylates irs-1 on ser-270 to promote insulin resistance in response to tnf-(alpha) signaling through ikk2. J. Biol. Chem. 283, 35375–35382 (2008)
L. Macho, M. Fickova, D. Jezova, S. Zorad, Late effects of postnatal administration of monosodium glutamate on insulin action in adult rats. Physiol. Res. 49, S79–S85 (2000)
S.K. Lee, E.C. Opara, R.S. Surwit, M.N. Feinglos, O.E. Akwari, Defective glucose-stimulated insulin release from perifused islets of c57bl/6j mice. Pancreas 11, 206–211 (1995)
R.S. Surwit, C.M. Kuhn, C. Cochrane, J.A. Mccubbin, M.N. Feinglos, Diet-induced type-ii diabetes in c57bl/6j mice. Diabetes 37, 1163–1167 (1988)
P. Huang, S. Li, M. Shao, Q. Qi, F. Zhao, J. You, T. Mao, W. Li, Z. Yan, Y. Liu, Calorie restriction and endurance exercise share potent anti-inflammatory function in adipose tissues in ameliorating diet-induced obesity and insulin resistance in mice. Nutr. Metab. Lond. 7, 59 (2010)
G.S. Hotamisligil, Inflammation and metabolic disorders. Nature 444, 860–867 (2006)
I.B. Leibiger, B. Leibiger, P.O. Berggren, Insulin signaling in the pancreatic beta-cell. Annu. Rev. Nutr. 28, 233–251 (2008)
K.L. Lipson, S.G. Fonseca, S. Ishigaki, L.X. Nguyen, E. Foss, R. Bortell, A.A. Rossini, F. Urano, Regulation of insulin biosynthesis in pancreatic beta cells by an endoplasmic reticulum-resident protein kinase ire1. Cell Metab. 4, 245–254 (2006)
T.P. Solomon, J.M. Haus, C.M. Marchetti, W.C. Stanley, J.P. Kirwan, Effects of exercise training and diet on lipid kinetics during free fatty acid-induced insulin resistance in older obese humans with impaired glucose tolerance. Am. J. Physiol. Endocrinol. Metab. 297, E552–E559 (2009)
S.B. Choi, J.S. Jang, S. Park, Estrogen and exercise may enhance beta-cell function and mass via insulin receptor substrate 2 induction in ovariectomized diabetic rats. Endocrinology 146, 4786–4794 (2005)
J.O. Holloszy, Exercise-induced increase in muscle insulin sensitivity. J. Appl. Physiol. 99, 338–343 (2005)
M.P. Corcoran, S. Lamon-Fava, R.A. Fielding, Skeletal muscle lipid deposition and insulin resistance: effect of dietary fatty acids and exercise. Am. J. Clin. Nutr. 85, 662–677 (2007)
I.B. Leibiger, B. Leibiger, T. Moede, P.O. Berggren, Exocytosis of insulin promotes insulin gene transcription via the insulin receptor/pi-3 kinase/p70 s6 kinase and cam kinase pathways. Mol. Cell 1, 933–938 (1998)
I.B. Leibiger, B. Leibiger, P.O. Berggren, Insulin feedback action on pancreatic beta-cell function. FEBS Lett. 532, 1–6 (2002)
Acknowledgments
This work was supported by the Brazilian Federal Foundation, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and the Paraná Science Foundation (Fundação Araucária).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miranda, R.A., Branco, R.C.S., Gravena, C. et al. Swim training of monosodium l-glutamate-obese mice improves the impaired insulin receptor tyrosine phosphorylation in pancreatic islets. Endocrine 43, 571–578 (2013). https://doi.org/10.1007/s12020-012-9798-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9798-5