Abstract
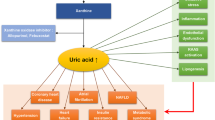
For more than 200 years initially seen as a cause of gout, speaking in a politically correct 21st century term, a disease of the rich and very well nourished people, many experimental and epidemiological studies have associated increased levels of serum uric acid (UA) with the classical components of the metabolic syndrome (MS), type 2 diabetes, and cardiovascular disease [1]. This association with components of the MS is seen even in children and adolescents [2]. The topic of increased UA concentrations, its consequences or associations is getting more important nowadays due to the increments in the prevalence of obesity and the MS in both developed and developing countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Uric acid as a cause and not as consequence of the metabolic syndrome, is this possible?
Indeed if we see the metabolic syndrome (MS) as an entity where insulin resistance predominates, and considering that excess insulin concentrations increase sodium and uric acid (UA) reabsorption by the kidney, this association could have been easily explained [3]. However, not everything that glitters is gold and the picture is not so clear for this simple and elegantly proven explanation. Excess UA reduces nitric oxide (NO) bioavailability [4], NO on its hand is essential for insulin action [5]; therefore hyperuricemia could induce or increase insulin resistance by itself.
Previous evidence also associated increased serum UA concentrations with elevated visceral adipose tissue mass [6]. One possible explanation for this finding is that increased free fatty acid flux to the liver, as seen in visceral obesity, not only increases triglyceride-rich VLDL production but also stimulates UA synthesis [7]. This would occur due to de novo purine synthesis by NADPH produced in the pentose phosphate pathway. However, to complicate more, this metabolic charade, evidence from one experimental animal study suggests that elevated UA may not be a consequence but might be one of the causes of the MS [8]. Putting it in more clear words, elevated serum UA might cause the onset of some of the components of the MS and not just be a consequence of it! If insulin resistance is the link between UA and the MS, we could say that UA might participate in a vicious cycle that is associated with the onset of some components of the MS, like increased blood pressure, raising triglyceride levels, reduction of HDL-C, and high fasting glucose levels [9]. Indeed previous prospective studies found a positive and independent association between serum UA concentrations and the risk of developing type 2 diabetes [10–12].
In this number of endocrine, Gonçalves et al. [13], found in a well-designed study performed in 1,054 Portuguese subjects an independent association of UA concentrations with the onset of the MS as whole and more specifically with some of its individual components. The association was found in both a cross-sectional investigation and in a prospective average 5-year follow-up. Most importantly, in the latter evaluation hyperuricemic subjects (UA >6.0 and 7.0 mg/dL, respectively for men and women) presented a 1.73 (95 % CI 1.08–2.76) greater chance of developing the MS. When measured as a continuous variable 1 standard deviation in UA concentrations (1.2 mg/dL) was associated with a 1.22-fold increase in the risk of developing the MS (95 % CI; 1.05–1.42). The strongest associations were seen with the prevalence and onset of increased plasma triglycerides (>150 mg/dL) in respectively the cross-sectional and the prospective study and in the onset of elevated waist circumference values (>94 cm in women and >102 cm in men) in the latter. Indeed this association with increased plasma triglyceride levels might reflect the increased insulin resistance state seen in these circumstances [14]. Despite the findings of the Portuguese group, this association of UA with the onset of the MS is not totally clear in the literature. Yang et al. [15] in a prospective study done in 3,857 Chinese subjects found and independent association of serum UA with the MS onset in women but not in men after a 5.8 years prospective follow-up. This controversy might be explained by ethnical factors, like different fat distributions between oriental subjects and Caucasians [16]. However, despite all the care taken by Gonçalves et al. [13] in their study the authors were not able to avoid the possible reverse causality in the relation between UA and the MS.
In the animal model where the MS was induced by fructose feeding, the use of UA lowering medications was associated with reductions in blood pressure, triglyceride, and insulin levels as well as in excess body weight [8]. This was a good hint of a causal effect of UA in the metabolic changes associated with the MS. However, to prove the real role of UA on the genesis of this pathologic condition, we need a long term randomized prospective trial testing the effects of serum UA lowering on the components of the MS. Without that the Koch’s postulates showing the cause and effect association of one agent over disease cannot be proven.
Uric acid, metabolic syndrome and cardiovascular events, does uric acid have a role?
Finally, a few words on the possible independent association of UA with cardiovascular disease especially in the MS set. I’m totally convinced that raised UA levels are associated with an increased risk of cardiovascular disease [1, 17]. This is clear by both cross-sectional studies evaluating subclinical atherosclerotic disease as well as by prospective data [18–22]. However, many of these studies are confounded by lack in adjustment for reduced kidney function, a very important risk factor for both increased UA levels and vascular disease [23]. Moreover, when we think about the MS, we would have to consider that UA per se is another player in an environment polluted by so many unquestionable risk factors for atherosclerotic vascular disease like hypertension, low HDL-cholesterol levels, and inflammation [9]. In this scenario, we also have the contribution of insulin resistance and the consequent increased oxidative stress and its proliferative effects. On the other hand, there is a theory suggesting that increased UA levels are a compensation for the increased oxidative stress found in these situations [24], meaning a possible protective role of UA counterbalancing pro-atherogenic mechanisms.
In conclusion, putting all these facts together it’s hard to prove, even if we perform a very well conducted epidemiological trial, that increased serum UA concentrations have an independent role in the atherogenic process in subjects with the MS. However, if we consider that serum UA has something to do with the genesis of MS, and that if it aggravates many pathophysiological mechanisms associated with the risk of cardiovascular disease we do need to have a definitive answer for this charade. Again the much-awaited randomized controlled trial of UA reduction is necessary to clarify this foggy scenario.
References
A.C. Gagliardi, M.H. Miname, R.D. Santos, Uric acid: a marker of increased cardiovascular risk. Atherosclerosis 202, 11–17 (2009)
E.S. Ford, C. Li, S. Cook, H.K. Choi, Serum concentrations of uric acid and the metabolic syndrome among US children and adolescents. Circulation 115, 2526–2532 (2007)
A.Q. Galvan, A. Natali, S. Baldi et al., Effect of insulin on uric acid excretion in humans. Am. J. Physiol. 268, E1–E5 (1995)
U.M. Khosla, S. Zharikov, J.L. Finch et al., Hyperuricemia induces endothelial dysfunction and vasoconstriction. Kidney Int. 67, 1739–1742 (2005)
G. Wu, C.J. Meininger, Nitric oxide and vascular insulin resistance. BioFactors 35, 21–27 (2009)
F. Matsuura, S. Yamashita, T. Nakamura, M. Nishida, S. Nozaki, T. Funahashi, Y. Matsuzawa, Effect of visceral fat accumulation on uric acid metabolism in male obese subjects: visceral fat obesity is linked more closely to overproduction of uric acid than subcutaneous fat obesity. Metabolism 47, 929–933 (1998)
I. Fabregat, E. Revilla, A. Machado, Short-term control of the pentose phosphate cycle by insulin could be modulated by the NADPH/NADP ratio in rat adipocytes and hepatocytes. Biochem. Biophys. Res. Commun. 146, 920–925 (1987)
T. Nakagawa, H. Hu, S. Zharikov, K.R. Tuttle, R.A. Short, O. Glushakova, X. Ouyang, D.I. Feig, E.R. Block, J. Herrera-Acosta, J.M. Patel, R.J. Johnson, A causal role for uric acid in fructose-induced metabolic syndrome. Am. J. Physiol. Renal. Physiol. 290, F625–F631 (2006)
G. Reaven, Why a cluster is truly a cluster: insulin resistance and cardiovascular disease. Clin. Chem. 54, 785–787 (2008)
K.L. Chien, M.F. Chen, H.C. Hsu, W.T. Chang, T.C. Su, Y.T. Lee, F.B. Hu, Plasma uric acid and the risk of type 2 diabetes in a Chinese community. Clin. Chem. 54, 310–316 (2008)
V. Bhole, J.W. Choi, S.W. Kim, M. de Vera, H. Choi, Serum uric acid levels and the risk of type 2 diabetes: a prospective study. Am. J. Med. 123, 957–961 (2010)
T. Wang, Y. Bi, M. Xu, Y. Huang, Y. Xu, X. Li, W. Wang, G. Ning, Serum uric acid associates with the incidence of type 2 diabetes in a prospective cohort of middle-aged and elderly Chinese. Endocrine 40, 109–116 (2011)
J.P. Gonçalves, A. Oliveira, M. Severo, A.C. Santos, C. Lopes, Cross-sectional and longitudinal associations between serum uric acid and metabolic syndrome. Endocrine. (2012). Epub ahead of print
M.Y. Desai, R.D. Santos, D. Dalal, J.A. Carvalho, D.R. Martin, J.A. Flynn, K. Nasir, R.S. Blumenthal, Relation of serum uric acid with metabolic risk factors in asymptomatic middle-aged Brazilian men. Am. J. Cardiol. 95, 865–868 (2005)
T. Yang, C.H. Chu, C.H. Bai, S.L. You, Y.C. Chou, W.Y. Chou, K.L. Chien, L.C. Hwang, T.C. Su, C.H. Tseng, C.A. Sun, Uric acid level as a risk marker for metabolic syndrome: a Chinese cohort study. Atherosclerosis 220, 525–531 (2012)
S.H. Boutcher, S.L. Dunn, T.E. Gail, J. Freund, Regional adiposity distribution and insulin resistance in young Chinese and European Australian women. Scand. J. Clin. Lab. Invest. 71, 653–657 (2011)
R.D. Santos, Uric acid and cardiovascular disease: how to solve another chicken or egg puzzle. Cardiology 114, 298–299 (2009)
C. Iribarren, A.R. Folsom, J.H. Eckfeldt, P.G. McGovern, F.J. Nieto, Correlates of uric acid and its association with asymptomatic carotid atherosclerosis: the ARIC study. Atherosclerosis risk in communities. Ann. Epidemiol. 6, 331–340 (1996)
R.D. Santos, K. Nasir, R. Orakzai, R.S. Meneghelo, J.A. Carvalho, R.S. Blumenthal, Relation of uric acid levels to presence of coronary artery calcium detected by electron beam tomography in men free of symptomatic myocardial ischemia with versus without the metabolic syndrome. Am. J. Cardiol. 99, 42–45 (2007)
A.D. Liese, H.W. Hense, H. Löwel et al., Association of serum acid with all-cause and cardiovascular disease and incident myocardial infarction in the MONICA Augsburg cohort. World Health Organization monitoring trends and determinants in cardiovascular diseases. Epidemiology 10, 391–397 (1999)
M.J. Bos, P.J. Koudstaal, A. Hofman, J.C.M. Witteman, M.M.B. Breteker, Uric acid is a risk factor for myocardial infarction and stroke. Stroke 37, 1503–1507 (2006)
A. Strasak, E. Ruttmann, L. Brant et al., Serum uric acid and risk of cardiovascular mortality: a prospective long-term study of 83 683 Austrian men. Clin. Chem. 54, 273–284 (2008)
R.J. Johnson, D.H. Kang, D. Feig et al., Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension 416, 1183–1190 (2003)
F.J. Nieto, C. Iribarren, M.D. Gross, G.W. Cosmotock, R.G. Cutler, Uric acid and serum antioxidant capacity: a reaction to atherosclerosis? Atherosclerosis 148, 131–139 (2000)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santos, R.D. Elevated uric acid, the metabolic syndrome and cardiovascular disease: cause, consequence, or just a not so innocent bystander?. Endocrine 41, 350–352 (2012). https://doi.org/10.1007/s12020-012-9657-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-012-9657-4