Abstract
The purpose of this study was to determine low-grade inflammation associated with obesity that is mediated partially by TNF-α, an adipocytokine which stimulates sphingomyelinase activity in adipocytes. Circulating ceramide (Cer) and sphingosine 1-phosphate (S1P) are elevated in genetically obese (ob/ob) mice. We aimed to determine whether serum sphingolipid concentrations correlate with measures of obesity, insulin resistance, and lipid profiles in overweight versus lean adolescents. This cross-sectional study recruited 30 healthy overweight (body mass index, BMI ≥ 85%) and 15 lean (BMI 10–84%) adolescents. Anthropometric measurements and fasting blood samples were collected at one clinic visit. Serum glucose, insulin, and fasting lipid profiles were measured. Serum adipocytokine concentrations were measured by ELISA or colorimetric assay and sphingolipids were measured by HPLC–mass spectrometry. Between group differences in serum sphingolipid concentrations were assessed. Correlations between sphingolipid concentrations and (i) body mass index, (ii) calculated homeostasis model assessment of insulin resistance (HOMA-IR), (iii) adipocytokines, and (iv) lipoproteins were determined. The results showed that significant differences in HOMA-IR (4.5 ± 3.2 vs. 1.2 ± 0.7), free fatty acids (0.8 ± 0.3 mmol/l vs. 0.4 ± 0.3 mmol/l), and adiponectin (6.4 ± 3.8 vs. 12.6 ± 9.9 μg/ml) were seen between groups (overweight vs. lean). There were significant correlations between Cer and TNF-α (r = 0.429), S1P and TNF-α (r = 0.288), Cer and adiponectin (r = 0.321), Cer:S1P and adiponectin (r = 0.324), Cer and HOMA-IR (r = 0.307), and Cer:S1P and LDL cholesterol (r = 0.453); these associations persisted after adjustment for BMI Z-score, sex, and Tanner stage. We concluded that elevated sphingolipid concentrations correlate with TNF-α, adiponectin, lipoprotein profiles, and HOMA-IR. Ceramide is associated with atherogenic lipid profiles and the development of insulin resistance in obese adolescents, similar to adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive weight gain in children and adolescents is a major health concern. Among school-aged adolescents, aged 12–19 years, the prevalence of obesity, defined as body mass index (BMI) ≥95th percentile, increased from 5.0% in 1976–1980 to 18.1% in 2007–2008 [1]. Obese children develop many of the comorbidities associated with the obese state, including insulin resistance, glucose intolerance, dyslipidemia, and hypertension [2, 3]. Metabolic syndrome, a compilation of these metabolic disturbances, is a significant risk factor for the development of Type 2 diabetes (T2DM) and atherosclerotic cardiovascular disease [4].
Inflammation is a major contributor to the insulin-resistant state that accompanies obesity. In obese adults, secretion of inflammatory mediators precedes the development of insulin resistance [5]. Population-based studies in overweight children have demonstrated elevated serum concentrations of inflammatory mediators and adipocytokines including C-reactive protein and interleukin-6 (IL-6) and decreased adiponectin concentrations [6]. Correlations between obesity and tumor necrosis factor-alpha (TNF-α) have been less consistent in children [7, 8]. However, in vitro studies in adipocytes have demonstrated a central role of TNF-α in insulin resistance both through inhibition of insulin signaling and activation of sphingomyelinase activity [9]. This has raised an interest in the role of sphingolipids in the development and pathogenesis of insulin resistance and the metabolic syndrome.
Sphingolipids help to maintain the structural integrity of the plasma membrane. In addition, sphingolipids mediate cellular processes including growth, differentiation, motility, and apoptosis [10, 11]. Activation of sphingomyelinases by cellular stress and cytokines increases ceramide (Cer) levels, stimulating apoptotic pathways [10]. Ceramide is converted to sphingosine (Sph) via ceramidases and subsequently metabolized to sphingosine 1-phosphate (S1P) via sphingosine kinase (SPHK). The role of circulating ceramide in development of insulin resistance and T2DM in human subjects has recently been demonstrated [12, 13]. Obese subjects with T2DM have elevated plasma concentrations of ceramide and its subspecies compared with healthy controls [12]. In addition, total ceramide concentrations decrease following gastric bypass surgery with decline in ceramide correlating with improved insulin sensitivity [13].
S1P is a major bioactive sphingolipid with dual roles as a cell surface ligand and intracellular second messenger. The regulation of S1P production may be altered in the insulin-resistant state. High glucose activates SPHK in vascular endothelial cells in vitro, producing S1P, which, in turn, promotes vascular endothelial cell growth [14]. Circulating platelets contain high concentrations of SPHK and release S1P in response to blood vessel injury, contributing to repair of the damaged vessel wall [15]. S1P is also a component of plasma lipoproteins, with the highest concentration present in the anti-atherogenic high-density lipoprotein (HDL) [16]. Finally, erythrocytes contain high levels of S1P, acting as a reservoir for circulating S1P [17]. It has been suggested that a balance between the sphingolipid metabolites ceramide and S1P may influence cell death and survival [18], thus raising an interest in these metabolites as potential moderators/regulators of insulin resistance and atherogenesis associated with the chronic inflammatory state of obesity.
A role for sphingolipids in the development of the metabolic syndrome has been demonstrated in animal models. Leptin deficient ob/ob mice develop severe obesity with hyperinsulinemia. Adipose tissues from these mice have decreased concentrations of ceramide, while serum concentrations of ceramide, Sph, and S1P are increased [19].
Although the role of sphingolipids in development of obesity-associated comorbidities has been demonstrated in adult subjects, studies in adolescents have yet to be performed. The overweight adolescent population provides a unique opportunity to examine the association between sphingolipids and insulin resistance, adipocytokines, and atherogenic lipoprotein profiles since it is less likely that the results will be confounded by chronic inflammatory conditions that affect older populations. This population also provides the opportunity to evaluate circulating sphingolipid concentrations earlier in the pathogenesis of metabolic disease. The primary objective of this study was to compare the serum concentrations of sphingolipids, specifically ceramide, Sph, and S1P in overweight versus lean adolescents to address whether obesity is associated with altered serum sphingolipid profiles in this population. An additional objective was to determine whether serum adipocytokines and serum sphingolipid concentrations are associated with early evidence of risk for development of atherosclerosis and progression to T2DM in adolescents by evaluating serum adipocytokines, insulin resistance, and fasting lipoprotein profiles.
Materials and methods
Study population
Adolescents (age 13–18 years) referred to the pediatric endocrinology division at the Women and Children’s Hospital of Buffalo (WCHOB) for management of overweight status (BMI ≥85th percentile) were recruited for the study group. This cross-sectional study was approved by the Institutional Review Board for Children and Youth at WCHOB and was in accordance with the ethical standards of the Helsinki Declaration of 1975. Normoglycemic, lean (BMI ≥10th percentile and <85th percentile), age-matched adolescents with no chronic illness followed at the clinic for non-pathological short stature (height ≥ 5th percentile; n = 12), pubertal gynecomastia (n = 2), or for autoimmune thyroiditis (n = 1) who were euthyroid for at least 6 months prior to enrollment, served as controls. The subject’s parent/guardian provided signed informed consent with assent provided by the subject.
Subjects were excluded from the study if they had an acute illness with fever, vomiting, or diarrhea within 5 days of the study, a history of a chronic inflammatory disease, bleeding disorders, recent surgery, or blood transfusion. Subjects were excluded if they took oral steroids within 2 months of study entry or if they were taking cholesterol-lowering, anti-hypertensive, or daily non-steroidal anti-inflammatory drugs. Subjects who were pre-pubertal or pregnant were excluded.
For all subjects, the following information was collected at one clinic visit: (1) participant’s current state of health, (2) anthropometry including height (nearest 0.1 cm), weight (nearest 0.1 kg), (3) waist circumference (WC), (4) heart rate and blood pressure, and (5) Tanner stage. Height was measured using a calibrated wall-mounted stadiometer, and weight was measured with an electronic scale. BMI was calculated as kg/m2 and BMI Z-scores, Ht Z-scores, and Wt Z-scores for age and sex were calculated using software based on the Center for Disease Control and Prevention (CDC) growth charts [20]. WC was measured to the nearest 0.1 cm with a flexible linen tape in triplicate with the average used for analysis. Heart rate and blood pressure were measured twice using a Welch Allyn Spot Vital Signs monitor by trained nurses. The average of the measurements was used for analysis.
Laboratory parameters
Fasting (10–12 h) blood samples for lipid profile, hemoglobin A1C (HbA1c), glucose, insulin, free fatty acids (FFAs), adipocytokines (TNF-α, IL-6, and adiponectin), and serum sphingolipids were drawn between 0730 and 1000 h. Samples for blood glucose were collected in a fluorinated tube and measured via glucose oxidase—O2 electrode method. Insulin was measured by Immulite Chemiluminescence assay, and HbA1c was measured using Bio-Rad Variant II (Bio-Rad Laboratories, Diagnostic Group, Hercules, CA). Total cholesterol was determined with the Beckman Coulter reagent (Beckman Coulter, Inc, Brea, CA) via enzymatic method. HDL cholesterol (HDL-C) was determined using a Beckman Coulter reagent via direct polyanion method using detergent and cholesterol esterase/oxidase. Triglyceride was determined enzymatically using glycerol phosphate oxidase without correction for free glycerol. LDL cholesterol (LDL-C) was calculated using the Friedewald equation [for triglyceride <400 mg/dl (4.5 mmol/l)]. These analyses were performed at the Kaleida Health Department of Pathology and Laboratory Medicine (Buffalo, NY) to assure inter-assay reliability. Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as follows: fasting glucose (mmol/l) × fasting insulin (μIU/ml)/22.5. This tool correlates with insulin resistance as measured by the euglycemic-hyperinsulinemic clamp method [21]. Metabolic syndrome was defined by the presence of three or more of the following criteria: blood pressure (BP) greater than 90th percentile for age, height, and sex [22]; WC greater than 90th percentile for age and sex [23]; triglyceride greater than 150 mg/dl (1.7 mmol/l), HDL-C less than 40 mg/dl (1.04 mmol/l), and blood glucose greater 100 mg/dl (5.5 mmol/l) [24].
Serum adipocytokine and sphingolipid measurements
Serum samples for adipocytokines and sphingolipids were centrifuged within 1–2 h after blood draw, labeled, aliquoted, and frozen at −80°C in non-stick Eppendorf tubes. Serum TNF-α was measured by ELISA using Quantikines® kit (R&D Systems, Minneapolis, MN) which has a sensitivity of 1.6 pg/ml and intra- and inter-assay coefficients of variation (CV) <10%. Serum IL-6 was measured by ELISA (Thermo-Scientific®, Rockford, IL) which has a sensitivity <1 pg/ml and intra- and inter-assay CV <10%. Serum adiponectin concentrations were measured by ELISA (Millipore®, Billerica, MA) which has a sensitivity of 0.78 ng/ml and intra- and inter-assay CV <10%. FFAs concentrations were measured by colorimetric assay (Zen-Bio, Inc®, Research Triangle Park, NC). Sphingolipid analysis was done by HPLC tandem mass spectrometry at the Hollings Cancer Center Analytical Lipidomics Core, Medical University of South Carolina, as described previously [19]. Data were expressed as picomoles per milliliter (pmol/ml) of serum.
Statistical analysis
Sample size was calculated a priori using data comparing ceramide concentrations in lean and ob/ob mice [19]. Based on these data, 30 subjects and 15 controls would give the study greater than 80% power, with an alpha-error of 0.05 to detect a difference in serum ceramide concentrations of 750 pmol/ml between the lean and obese adolescents. Data were expressed as mean ± standard deviation (SD) or median (25th, 75th percentile). Continuous data were assessed for normal distribution and were logarithmically transformed as appropriate. Data were compared using two-tailed Student’s t test for continuous variables and χ2 test or Fisher’s exact test for categorical variables. Correlations between serum sphingolipids, adipocytokines, HOMA-IR, and lipoprotein profiles were determined using Pearson’s correlation coefficient (r). A general linear regression model was created to determine the association between variables showing significant correlations after adjusting for BMI Z-score, sex, and pubertal stage (Tanner stage). All subjects were categorized into two Tanner stage groups for regression analysis, Tanner stages 2–4 or Tanner stage 5. P values (two-tailed) ≤0.05 were considered as statistically significant. Statistical analysis was done with SPSS 16.0 (Chicago, IL, USA).
Results
The study enrolled 30 obese (study group) and 15 lean (control group) adolescents. All subjects in the study group had exogenous obesity of variable duration ranging from 5 to 12 years. Age and sex distribution was similar between the two groups. The ethnic distribution was more diverse in the study group. The obese subjects had significantly higher Wt Z-score, BMI, BMI Z-score, WC, and median Tanner stage, while height was similar between groups (Table 1).
There was no significant difference in fasting blood glucose and HbA1c between the groups (Table 2). None of the subjects had impaired fasting glucose or elevated HbA1c levels. Despite normoglycemia in the study group, fasting insulin concentrations were significantly elevated and mean HOMA-IR was in the upper 2.5 percentile, consistent with significant insulin resistance [25]. In addition, HDL-C was significantly lower (P < 0.001) in the obese compared with lean subjects, while LDL-C and total cholesterol did not differ between the groups. In addition, fasting triglyceride concentrations were higher in obese adolescents (P = 0.001). Using parameters established by Cook et al. [24], 20% of obese subjects and none of lean subjects met the diagnostic criteria for metabolic syndrome (Table 2).
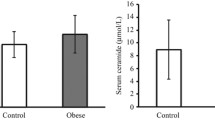
We also compared serum adipocytokine, FFA, and the major sphingolipid metabolite concentrations between the two groups. Our analysis confirms that obese adolescents have significantly lower adiponectin concentrations compared with controls (P = 0.004; Table 3). In addition, FFA concentrations were higher in obese subjects than in lean controls (P < 0.001). There was no significant difference in either IL-6 (P = 0.750) or TNF-α (P = 0.720) concentrations between the two groups. Sphingolipid concentrations of ceramide, Sph, and S1P were not significantly different between the two groups (Table 3). There was no difference in ceramide subspecies concentrations (C14:0, C16:0, C18:0, C20:0, C24:0, and C24:1) between the groups (data not shown). In addition, the ceramide:S1P ratio (Cer:S1P), an indicator of sphingolipid biochemical flux, was similar between the study and control groups (Table 3).
Although there were no significant differences in sphingolipid concentrations between the two populations, there were significant associations between sphingolipid metabolites and adipocytokines, atherogenic lipid levels, and measures of insulin resistance. Correlations between paired variables of interest are shown in Table 4. Total ceramide positively correlated with TNF-α and HOMA-IR, while S1P positively correlated with TNF-α and negatively correlated with LDL-C. Ceramide subspecies, C16:0 and C24:0 positively correlated with TNF-α; only ceramide C24:0 positively correlated with HOMA-IR. Interestingly, ceramide concentrations and Cer:S1P also positively correlated with adiponectin, although adiponectin concentrations were significantly lower in obese compared with lean subjects. Finally, Cer:S1P negatively correlated with IL-6 and positively correlated with LDL-C. No significant correlations were seen between BMI Z-score and sphingolipid metabolites (P > 0.05; Table 4). While significant correlations were demonstrated between BMI Z-score and HOMA-IR (P < 0.005), no associations were seen between either BMI Z-score or HOMA-IR and TNF-α (P > 0.05; data not shown).
General linear regression model was used to clarify the relationship between adipocytokine and sphingolipid concentrations, as well as the association between sphingolipid products and insulin resistance and atherogenic lipoproteins for all subjects, adjusting for BMI Z-score, gender, and Tanner stage categories (Table 5). These covariates are known to affect insulin resistance, lipoprotein profiles, and adipocytokine expression. Outcome variables were assessed for linear distribution, and HOMA-IR and ceramide were log-transformed to correct for non-linear distribution. TNF-α was positively associated with S1P (P = 0.03; β-coefficient = 83.45), Log10ceramide (P < 0.001; β = 0.0515), its subspecies, Log10ceramide C16:0 (P < 0.05; β = 0.034), and Log10ceramide C24:0 (P < 0.05; β = 0.025). Adiponectin was positively associated with Log10ceramide (P = 0.006; β = 0.012) and Cer:S1P (P = 0.003; β = 0.058). Associations between IL-6 and Cer:S1P were lost after adjusting for covariates (P = 0.07). Further, total ceramide and subspecies C16:0 were positively associated with insulin resistance represented by Log10HOMA-IR (P = 0.05; β-coefficient = 0.0000375 (Table 5) and 0.000047, respectively). While both S1P and Cer:S1P positively correlated with LDL-C, only the association between Cer:S1P and LDL-C remained after adjustment (P = 0.004; β-coefficient = 0.0097).
Discussion
Obesity in the adolescent population correlates with the development of insulin resistance [25] and T2DM and is associated with low-grade inflammation [2, 3]. Some studies have demonstrated that adipocytokines secreted from adipose tissue, e.g., IL-6 and TNF-α, are increased in overweight adolescents, and adipocytokine concentrations correlate with measurements of insulin resistance [6, 26]. Our data comparing 30 obese adolescents to lean controls demonstrate significant insulin resistance (HOMA-IR 4.5 ± 3.2; Table 2) in the obese group, with 20% of the obese adolescents meeting the diagnostic criteria for metabolic syndrome. Adiponectin concentrations are lower in obese subjects than in lean subjects, consistent with published results [6, 27]. Differences in IL-6 and TNF-α were not observed. Our study was not powered to detect differences in IL-6 concentrations between obese and lean adolescents, and relationships between obesity and TNF-α are inconsistent in the literature [7, 8].
Cytokines alter sphingolipid metabolism in some cell types, contributing to the pathology associated with cytokine secretion [28]. In vitro studies have shown that TNF-α increases sphingomyelinase activity in a wide variety of cell types, including adipose tissue, leading to increased ceramide production [9]. Our group previously demonstrated that TNF-α stimulates SPHK activity and S1P production in pancreatic β-cells in vitro [29]; by implication, serum concentrations of S1P may be increased as a result of increased TNF-α. Here, we show that serum ceramide and S1P positively correlate with TNF-α concentrations in adolescent subjects (Table 4).
While our study did not demonstrate an association between TNF-α and insulin resistance as measured by HOMA-IR, TNF-α does correlate with total serum ceramide concentrations in our subjects, similar to findings in obese adults with T2DM [12]. We also found the ceramide subspecies C:16 and C:24:0 positively correlate with TNF-α concentrations, although fewer ceramide subspecies show this correlation in adolescents than in adults [12]. Furthermore, we demonstrate that both total ceramide and the ceramide subspecies C:24:0 correlate with HOMA-IR, even after adjusting for parameters which are known to affect insulin resistance, including BMI, pubertal status, and gender (Tables 4, 5). Studies in obese adults with T2DM reported an inverse association between ceramide and its subspecies concentrations and insulin sensitivity [12]. Our findings support the hypothesis that ceramide contributes to insulin resistance in the inflammatory milieu associated with the obese state even before the development of glucose intolerance (Fig. 1). Interestingly, we identified a positive correlation between both serum ceramide and Cer:S1P and adiponectin, while adiponectin concentrations negatively correlate with BMI. Although our study did not detect a difference in the Cer:S1P between two groups, the correlation between Cer:S1P and adiponectin suggests that the balance between ceramide and S1P levels are altered in obesity similar to changes seen in adiponectin. These findings are in agreement with recent data demonstrating a positive correlation between adiponectin and ceramide concentrations in adipose tissue harvested from lean and obese adults with and without T2DM [30]. Perhaps adiponectin secretion is upregulated as ceramide concentrations rise in the adipocyte, while in the insulin-resistant state, adiponectin concentrations fail to compensate for ceramide accumulation. This hypothesis remains to be tested. The role of adiponectin in regulating ceramide biosynthesis, particularly in the insulin-resistant state, may aid in the understanding of the contribution of sphingolipids to metabolic disease.
Model for correlations between sphingolipids and metabolic syndrome. Obesity leads to altered concentrations of adipocytokines including IL-6, TNF-α, FFA, and adiponectin. This results in changes in sphingolipid profiles and influences insulin signaling, as well as atherogenic profiles of lipoproteins increasing the risk of atherosclerosis. IL-6 interleukin-6, TNF-α tumor necrosis factor α, FFA free fatty acid, LDL-C low density lipoprotein cholesterol, HDL-C high-density lipoprotein cholesterol, Sph sphingosine, S1P sphingosine 1 phosphate
HDL-C particles are the major lipoprotein carriers of S1P in blood, while LDL-C is not a significant contributor to S1P content in serum [31]. Our study demonstrates a significant association between Cer:S1P, a representation of sphingolipid metabolic flux, and LDL-C concentrations. The balance between ceramide and S1P as measured by the Cer:S1P may be a relevant corollary to lipoprotein profiles as a measure of atherosclerotic risk.
Our study showed no difference in sphingolipid concentrations between lean and obese adolescents. Various factors may have contributed to these differences to animal data. First, the a priori sample size calculation was based on an animal study in genetically obese mice [19]. In contrast to the animal data, serum sphingolipid concentrations from adolescents were more variable, which may have contributed to the failure to identify differences between the two groups. A larger study would address this issue. Second, we tested serum rather than plasma sphingolipid concentrations. S1P levels in serum are at least twofold higher than in plasma [31], due to release when platelets are activated during the clotting process. However, handling of plasma samples requires careful attention to volume collection and anti-coagulation in order to minimize inter-subject variability. Ceramide concentrations are not affected by sample collection procedures [31]. Thus, it is unlikely that assay of plasma samples would have impacted either the variability in absolute sphingolipid concentrations or the results related to sphingolipid concentrations between the two groups.
Obese adults with T2DM have elevated circulating ceramide concentrations [12]. The study presented here is the first to investigate whether obesity alone is associated with changes in serum sphingolipid concentrations in younger subjects. The failure to identify a difference in sphingolipids, in particular ceramide species, suggests that our subjects, in spite of the obesity and insulin resistance as measured by HOMA-IR, represent a healthier population than the adults previously studied. A future study involving adolescents with T2DM may reveal elevated ceramide concentrations as demonstrated in adults with T2DM [12]. However, our observation that serum ceramide concentrations correlate with both TNF-α and HOMA-IR supports the hypothesis that ceramide is associated with the insulin-resistant state, further elaborating the concept that the metabolic complications associated with obesity represent a disease spectrum. This is consistent with the observation that glucose intolerance is often unmasked in the face of a second-hit, such as severe illness or sepsis, when inflammatory cytokines upregulate sphingomyelinase activity increasing serum ceramide concentrations [32]. Future studies will address whether improving the inflammatory milieu of insulin resistance, either through weight loss or pharmacologic intervention alters serum sphingolipid concentrations.
References
C. Ogden, M. Carroll, NCHS health e-stat: prevalence of obesity among children and adolescents: United States, trends 1963–1965 through 2007–2008. http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_07_08.htm (2010). Accessed 12 December 2011
R. Sinha, G. Fisch, B. Teague, W.V. Tamborlane, B. Banyas, K. Allen, M. Savoye, V. Rieger, S. Taksali, G. Barbetta, R.S. Sherwin, S. Caprio, Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N. Engl. J. Med. 346(11), 802–810 (2002)
Y. Aggoun, Obesity, metabolic syndrome, and cardiovascular disease. Pediatr. Res. 61(6), 653–659 (2007)
P.W. Wilson, R.B. D’Agostino, H. Parise, L. Sullivan, J.B. Meigs, Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 112(20), 3066–3072 (2005)
J.C. Pickup, Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care 27(3), 813–823 (2004)
C. Herder, S. Schneitler, W. Rathmann, B. Haastert, H. Schneitler, H. Winkler, R. Bredahl, E. Hahnloser, S. Martin, Low-grade inflammation, obesity, and insulin resistance in adolescents. J. Clin. Endocrinol. Metab. 92(12), 4569–4574 (2007)
I. Aeberli, L. Molinari, G. Spinas, R. Lehmann, D. l’Allemand, M.B. Zimmermann, Dietary intakes of fat and antioxidant vitamins are predictors of subclinical inflammation in overweight Swiss children. Am. J. Clin. Nutr. 84(4), 748–755 (2006)
Y.S. Moon, D.H. Kim, D.K. Song, Serum tumor necrosis factor-alpha levels and components of the metabolic syndrome in obese adolescents. Metabolism 53(7), 863–867 (2004)
P. Peraldi, G.S. Hotamisligil, W.A. Buurman, M.F. White, B.M. Spiegelman, Tumor necrosis factor (TNF)-alpha inhibits insulin signaling through stimulation of the p55 TNF receptor and activation of sphingomyelinase. J. Biol. Chem. 271(22), 13018–13022 (1996)
Y.A. Hannun, The sphingomyelin cycle and the second messenger function of ceramide. J. Biol. Chem. 269(5), 3125–3128 (1994)
S. Spiegel, O. Cuvillier, L.C. Edsall, T. Kohama, R. Menzeleev, Z. Olah, A. Olivera, G. Pirianov, D.M. Thomas, Z. Tu, J.R. Van Brocklyn, F. Wang, Sphingosine-1-phosphate in cell growth and cell death. Ann. N. Y. Acad. Sci. 845, 11–18 (1998)
J.M. Haus, S.R. Kashyap, T. Kasumov, R. Zhang, K.R. Kelly, R.A. DeFronzo, J.P. Kirwan, Plasma ceramides are elevated in obese subjects with type 2 diabetes and correlate with the severity of insulin resistance. Diabetes 58(2), 337–343 (2009)
H. Huang, T. Kasumov, P. Gatmaitan, H.M. Heneghan, S.R. Kashyap, P.R. Schauer, S.A. Brethauer, J.P. Kirwan, Gastric bypass surgery reduces plasma ceramide subspecies and improves insulin sensitivity in severely obese patients. Obesity 19, 2235–2240 (2011)
L. Wang, X.P. Xing, A. Holmes, C. Wadham, J.R. Gamble, M.A. Vadas, P. Xia, Activation of the sphingosine kinase-signaling pathway by high glucose mediates the proinflammatory phenotype of endothelial cells. Circ. Res. 97(9), 891–899 (2005)
D. English, Z. Welch, A.T. Kovala, K. Harvey, O.V. Volpert, D.N. Brindley, J.G. Garcia, Sphingosine 1-phosphate released from platelets during clotting accounts for the potent endothelial cell chemotactic activity of blood serum and provides a novel link between hemostasis and angiogenesis. FASEB J. 14(14), 2255–2265 (2000)
N. Murata, K. Sato, J. Kon, H. Tomura, M. Yanagita, A. Kuwabara, M. Ui, F. Okajima, Interaction of sphingosine 1-phosphate with plasma components, including lipoproteins, regulates the lipid receptor-mediated actions. Biochem. J. 352(Pt 3), 809–815 (2000)
P. Hanel, P. Andreani, M.H. Graler, Erythrocytes store and release sphingosine 1-phosphate in blood. FASEB J. 21(4), 1202–1209 (2007)
O. Cuvillier, G. Pirianov, B. Kleuser, P.G. Vanek, O.A. Coso, S. Gutkind, S. Spiegel, Suppression of ceramide-mediated programmed cell death by sphingosine-1-phosphate. Nature 381(6585), 800–803 (1996)
F. Samad, K.D. Hester, G. Yang, Y.A. Hannun, J. Bielawski, Altered adipose and plasma sphingolipid metabolism in obesity: a potential mechanism for cardiovascular and metabolic risk. Diabetes 55(9), 2579–2587 (2006)
R.J. Kuczmarski, C.L. Ogden, S.S. Guo, L.M. Grummer-Strawn, K.M. Flegal, Z. Mei, R. Wei, L.R. Curtin, A.F. Roche, C.L. Johnson, 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 11(246), 1–190 (2002)
H. Yokoyama, M. Emoto, S. Fujiwara, K. Motoyama, T. Morioka, M. Komatsu, H. Tahara, T. Shoji, Y. Okuno, Y. Nishizawa, Quantitative insulin sensitivity check index and the reciprocal index of homeostasis model assessment in normal range weight and moderately obese type 2 diabetic patients. Diabetes Care 26(8), 2426–2432 (2003)
B. Rosner, R.J. Prineas, J.M. Loggie, S.R. Daniels, Blood pressure nomograms for children and adolescents, by height, sex, and age, in the United States. J. Pediatr. 123(6), 871–886 (1993)
C. Li, E.S. Ford, A.H. Mokdad, S. Cook, Recent trends in waist circumference and waist-height ratio among US children and adolescents. Pediatrics 118(5), e1390–e1398 (2006)
S. Cook, P. Auinger, C. Li, E.S. Ford, Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J. Pediatr. 152(2), 165–170 (2008)
J.M. Lee, M.J. Okumura, M.M. Davis, W.H. Herman, J.G. Gurney, Prevalence and determinants of insulin resistance among US adolescents. Diabetes Care 29(11), 2427–2432 (2006)
A. Gupta, S. Ten, H. Anhalt, Serum levels of soluble tumor necrosis factor-alpha receptor 2 are linked to insulin resistance and glucose intolerance in children. J. Pediatr. Endocrinol. Metab. 18(1), 75–82 (2005)
R. Weiss, J. Dziura, T.S. Burgert, W.V. Tamborlane, S.E. Taksali, C.W. Yeckel, K. Allen, M. Lopes, M. Savoye, J. Morrison, R.S. Sherwin, S. Caprio, Obesity and the metabolic syndrome in children and adolescents. N. Engl. J. Med. 350(23), 2362–2374 (2004)
M. Nikolova-Karakashian, E.T. Morgan, C. Alexander, D.C. Liotta, A.H. Merrill Jr., Bimodal regulation of ceramidase by interleukin-1beta. Implications for the regulation of cytochrome p450 2C11. J. Biol. Chem. 272(30), 18718–18724 (1997)
L.D. Mastrandrea, S.M. Sessanna, S.G. Laychock, Sphingosine kinase activity and sphingosine-1 phosphate production in rat pancreatic islets and INS-1 cells: response to cytokines. Diabetes 54(5), 1429–1436 (2005)
A.U. Blachnio-Zabielska, M. Pulka, M. Baranowski, A. Nikolajuk, P. Zabielski, M. Górska, J. Górski, Ceramide metabolism is affected by obesity and diabetes in human adipose tissue. J. Cell Physiol. 227, 550–557 (2012)
S.M. Hammad, J.S. Pierce, F. Soodavar, K.J. Smith, M.M. Al Gadban, B. Rembiesa, R.L. Klein, Y.A. Hannun, J. Bielawski, A. Bielawska, Blood sphingolipidomics in healthy humans: impact of sample collection methodology. J. Lipid Res. 51(10), 3074–3087 (2010)
G. Delogu, G. Famularo, F. Amati, L. Signore, A. Antonucci, V. Trinchieri, L. Di Marzio, M.G. Cifone, Ceramide concentrations in septic patients: a possible marker of multiple organ dysfunction syndrome. Crit. Care Med. 27(11), 2413–2417 (1999)
Acknowledgments
The authors would like to thank Kathleen Bethin, MD, PhD, Suzanne Laychock, PhD, and Joan Dorn, PhD for their thoughtful review and helpful comments concerning this manuscript. The authors would also like to thank Lisa B. Rafalson, PhD and Chang-Xing Ma, PhD for their assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Majumdar, I., Mastrandrea, L.D. Serum sphingolipids and inflammatory mediators in adolescents at risk for metabolic syndrome. Endocrine 41, 442–449 (2012). https://doi.org/10.1007/s12020-011-9589-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-011-9589-4