Abstract
The purpose of this study was to determine the correlation between human adrenocortical carcinoma (ACC) and the proteins involved in tumor angiogenesis, and to evaluate the angiogenic status of ACC. The expression of heparanase-1 (HPA-1), vascular endothelial growth factor (VEGF), and vascular endothelial growth factor receptor-2 (VEGFR-2) as well as microvessel density (MVD) were measured in a series of tissue samples from 44 human sporadic adrenocortical tumors by immunohistochemistry. These specimens were classified as adenomas (n = 20) and carcinomas (n = 24) according to the histological criteria defined by Weiss. A total of 22 of 24 (91.67%) malignant cases showed positive staining for HPA-1 and 3 of 20 (15%) benign cases showed positive, the difference of HPA-1 expression between ACA and ACC was statistically significant (P < 0.001). Similarly, VEGF staining was seen in 70.83% (17/24) of the malignant cases versus 25% (5/20) of the benign, the difference of VEGF expression among two groups was statistically significant (P = 0.002). VEGFR-2 expressed highly in the ACC group (79.17%, 19/24) and lowly in the benign group (25%, 5/20), the two groups had extremely significant difference (P < 0.001). Malignant cases showed higher MVD compared to benign tumors (84.70 ± 12.44 vs. 21.05 ± 8.07, P < 0.001). HPA-1 and VEGF expression were positively correlated with MVD in all specimens (r_s = 0.812, P = 0.001; r_s = 0.834, P < 0.001). In conclusion, these results suggest that angiogenesis of human ACC maybe mediated by these proteins and they could represent selective targets for the molecularly targeted treatments of ACC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adrenocortical carcinoma (ACC), derived from adrenal cortex, is a rare heterogeneous neoplasm with an incompletely understood pathogenesis and a poor prognosis [1]. Operation remains the only potentially curative option for ACC until recently; however, about half of all patients present with disseminated diseases at the time of primary diagnosis, and they were less likely to receive radical excision [2]. Up to 85% of patients develop recurrent disease even after seemingly complete removal of tumor, adjuvant mitotane treatment based on the individual risk status should be considered [3]. The 2nd Annual International Adrenal Cancer Symposium unanimously stated that patients with potential residual disease (R1 or Rx resection) and/or Ki67 more than 10% should be offered adjuvant mitotane, whereas adjuvant therapy is not considered mandatory in patients fulfilling all of the following criteria: stages I or II disease (based on the ENSAT stage); histologically proven R0 resection; and Ki67 expressed in ≤10% of neoplastic cells [4]. Although, the combination of cytotoxic drug and mitotane is recommended to be the first-line therapy in advanced ACC, the overall prognosis is still very limited [5]. No effective treatment has been developed yet, and the incomplete understanding of molecular features of ACC might be one of the reasons for this situation of unsatisfied clinical efficacy and dismal prognosis.
Angiogenesis, defined as new blood capillaries formed from pre-existing microvessels and venules, is connected with cancer growth and its metastasis [6]. Vascular endothelial growth factor (VEGF) has been proposed to be the most important endogenous factor which has a stimulate effect on angiogenesis. VEGF binds to vascular endothelial growth factor receptor (VEGFR), which usually is vascular endothelial growth factor receptor-2 (VEGFR-2), activates receptor tyrosine kinase, causes a series of signal transduction which induces endothelial cell (EC) proliferation and promotes EC migration. All these actions eventually lead to neovascularization [7]. Microvessel density (MVD) is considered as golden standard in evaluating tumor angiogenesis [8]. To quantify the angiogenic status, markers of ECs, as such as Factor VIII, CD31 and CD34, have been used.
The relationship between angiogenesis and tumor aggressiveness has been reported in various forms of human cancer. At the early stage of angiogenesis, EC sprouting is based on the extracellular matrix (ECM) enzymatic degradation. Those aggressive tumor features, including invasion of adjacent structures and metastasis to distant organs, are also mediated by degradation of ECM and basement membrane (BM). ECM and BM degradation allows tumor cells to penetrate through tissue barrier and begin the process of metastasis, while angiogenesis promotes the process of sprouting and branching of new vessels from the pre-existing capillaries and post-capillary venules [9]. Heparan sulfate proteoglycans (HSPGs), as important structural elements in the ECM and BM, are responsible for the self-assembly and integrity of the ECM and BM multimolecular structure [10]. Heparanase-1 (HPA-1) is an endo-β-d-glucuronidase capable of degrading heparan sulfate (HS) which is a functional component of HSPG, enzymatic degradation of HS by HPA-1 leads to disassembly of the ECM and BM, therefore results in biological phenomena associated with tissue remodeling and cell movement, including cancer progression, metastasis, and angiogenesis [11, 12].
Human HPA-1, MVD, VEGF, and VEGFR-2 were found to be upregulated in tissue specimens derived from various tumors [13–15], and encouraging results of anti-angiogenic substances were published showing significant prolongation of survival and good tolerance in advanced renal [16], lung [17], and breast [18] cancer. However, the preliminary results of anti-angiogenic therapy in ACC have been largely disappointing. In ten patients, no response was found with a combination of the anti-VEGF antibody bevacizumab plus capecitabine given as salvage treatment [19]. Expression of HPA-1, MVD, and VEGFR-2 in ACC and the association between angiogenesis and HPA-1 in ACC have not been comprehensively studied until recently. In this study, we examined the impact on the oncogenetic process through investigating the expression of HPA-1, VEGF, and VEGFR-2, as well as quantitatively examined MVD in our collection of adrenocortical adenomas (ACAs) and ACCs, further seek the molecularly targeted treatments directed at inhibiting angiogenesis of ACC.
Materials and methods
Patients and tissue samples
Approved by institutional ethics review board, pathology specimens and medical records were reviewed from database. The preoperative diagnosis was based on the clinical history, symptoms, signs, endocrine evaluation, and imagine examination (e.g., MRI, CT). Histological features, including high mitotic rate, atypical mitoses, high nuclear grade, low percentage of clear cells, necrosis, diffuse architecture of tumor, capsular invasion, sinusoidal invasion, and venous invasion, are carefully analyzed according to the method of Weiss [20]. The pathological diagnosis of ACC was based on Weiss’s criteria with its score ≥3 [21]. Forty-four patients of sporadic adrenocortical tumors (ACTs), who underwent adrenalectomy at Ruijin hospital between October 1986 and March 2010, were classified as ACAs (N = 20) and ACCs (N = 24). Forty-four adrenocortical tumor tissues, collected from surgical specimens of 44 patients, were divided into two groups: 20 benign adrenal cortical tumors and 24 ACCs. Besides clinical diagnosis, histopathologic slides were classified by two pathologists independently and no discrepancy exists between them.
Immunohistochemistry staining
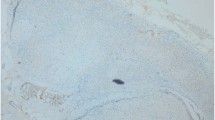
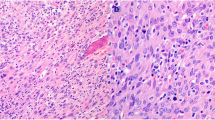
Specimens were fixed in 10% neutral buffered formalin, embedded in paraffin, and cutted into serial sections at a thickness of 3 μm. Paraffin-embedded tissues were dewaxed in xylene, rehydrated by serial concentrations of ethanol, and then rinsed in phosphate buffer solution (PBS) followed by treated with 3% H2O2 to refrain endogenous peroxidase. After being heated in a microwave at 750 W for 15 min for antigen retrieval, the sections were incubated with 10% goat serum at room temperature for 10 min to block non-specific reactions. Sections were incubated with polyclonal rabbit antihuman HPA-1 antibody (GenScript, USA) diluted to 1:100 for 12 h at 4°C. The slides were followed by a PBS wash and incubated by antirabbit EnVisionTM kit (DAKO, USA) for 30 min at 37°C. After a PBS wash, the sections were developed in diaminobenzidine (DAB) substrate. The sections were then counter-stained in hematoxylin and then dehydrated in ethanol and xylene before being mounted. Sections were re-prepared by EnVision immunohistochemical staining. VEGF was polyclonal rabbit anti-human antibody (Santa Cruz, USA), diluted to 1:50. VEGFR-2 was rabbit anti-human antibody (Maixin, China, 1:150 dilution). CD34 was monoclonal mouse anti-human antibody (Novocastra, USA), diluted to 1:200. The positive controls were gastric carcinoma, pancreatic carcinoma, and colon carcinoma with positive expressions of HPA-1, VEGF, VEGFR-2, and CD34. PBS instead of primary antibodies was as negative control.
Evaluation of immunohistochemical results
Immunohistochemical analysis demonstrates positive for HPA-1, VEGF, and VEGFR-2, if purple-brown granules located diffusely in the cytoplasm of the tumor cells. Lack of any obvious purple-brown or brown-red pigmentation in the cytoplasm of tumor cell was considered negative [22, 23]. For VEGF semi-quantitative immunoanalysis, the percentage of positive staining tumor cells was studied. Five representative high-power fields were chosen, and the number of positive-staining cells was calculated. The following categories were used: negative (−); weak (+) = 1–10%; moderate (++) = 11–50%; strong (+++) ≥51%. The results were scored by two independent pathologists who were blinded to the subtype of the tumors. A single microvessel was defined as any brown or brownish yellow CD34-immunostained ECs. We evaluated MVD following the method mentioned by Weider [8]: high vascular density area was selected under low power objective and counted the numbers of vascular stained by CD34 in three visual fields under high-power microscope (400×), and average value was regarded as the MVD value of the tumor.
Statistical analysis
Data analyses were performed using SPSS statistical package 15.0. The χ2 test was used to compare VEGF, VEGFR-2, and HPA-1 expressions in ACAs and ACCs. The average size of primary tumor of two groups was also examined. MVD result was expressed as mean ± SD, and Wilcoxon combined test was used to compare MVD expression between two groups. Spearman rank correlation analysis was used to determine the relationship between VEGF and HPA-1 expressions, and MVD. A P value less than 0.05 was considered significant.
Results
Twenty patients of ACA, consisting of 3 Cushing’s syndrome, 7 aldosteronomas, and 10 non-functional adenomas, are 12 females and 8 males, ranging from 28 to 59 years of age (mean age of 44.95 years at presentation). Twenty-four ACCs consisted of 13 females and 11 males, ranging from 38 to 74 years of age (mean age of 58.21 years). Fourteen patients of ACC have endocrine symptoms and signs that indicated excess secretion of cortisols (in 7 patients), cortisols and androgens concomitantly (in 6 patients), or estrogens (in 1 male patient). Eighteen patients had a left adrenal neoplasm and 26 had a right one. The mean primary tumor largest diameter in ACAs and ACCs group was 3.8 ± 2.5 and 7.5 ± 2.1 cm, respectively, (P < 0.001). The mean postsurgery follow-up of patients was 151.5 month (range, 102–264 months) and 47.2 months (range, 6–113 months), respectively. All of these characteristics were obtained from patient medical records and summarized in Table 1.
Positive staining for HPA-1 was observed in 15% (3/20) of the benign group and 91.67% (22/24) of the ACC group. The difference of HPA-1 expression between ACA and ACC was statistically significant (P < 0.001). VEGF staining was seen in 25% (5/20) of the benign versus 70.83% (17/24) of the malignant cases. The difference of VEGF expression among two groups was statistically significant (P = 0.002). VEGFR-2 expressed highly in the ACC group (79.17%, 19/24) and lowly in the benign group (25%, 5/20), the two groups had extremely significant difference (P < 0.001). The mean value of MVD was 84.70 ± 12.44/field in ACC group and 21.05 ± 8.07/field in ACAs, statistically significance was observed between them (P < 0.001).
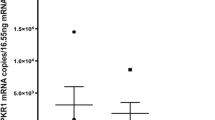
Sixteen out of 24 ACCs (66.67%) were stained positive for both HPA-1 and VEGF, while only two out of 20 ACAs (10%) were positive. Two of ACCs (8.33%) stained negative by both HPA-1 and VEGF, compared to 70% of benign tumors (n = 14). The mean value of MVD was 89.40 ± 15.64/field in sections which positivity for both HPA-1 and VEGF, and 13.10 ± 3.54 in sections which negative by both HPA-1 and VEGF, statistically significance was observed between them (P < 0.001), these staining data and value of MVD are summarized in Table 2. HPA-1 and VEGF expression in benign and malignant adrenal neoplasm were positively correlated with MVD (r_s = 0.812, P = 0.001; r_s = 0.834, P < 0.001) (Figs. 1, 2, 3, and 4).
Discussion
Unlike ACA that occurs frequently, ACC is a rare malignancy characterized by dismal prognosis and lacking efficacious therapeutic regimens. For patients with localized ACC, recurrent or metastasized ACC, complete surgical removal should be first considered. After ACC resection, the role of adjuvant treatment with mitotane is controversial. Veytsman et al. [24] point out that evidence on the efficacy of adjuvant mitotane in patients with ACC is based only on retrospective studies, however, no randomized prospective trials have so far been published, and no data from randomized clinical trials on adjuvant treatment in ACC will be available in the near future. The option of long-term monotherapy is restricted to patients who tolerate mitotane and either experiences a clinical response or are at high risk for recurrence. A preferable administration schedule is to start with 1–2 g/d and to increase the daily dose by 1 to at most 2 g every 1–2 weeks to the maximum-tolerated dose (never >6–10 g/d). Four to six grams is usually sufficient. Mitotane levels should be monitored by using a gas chromatography-flame ionization detection assay initially at 4–8 weeks intervals until a level of 10–14 mg/l is reached and subsequently at 3-month intervals [3, 24, 25]. For patients with metastasized ACC and not amenable to complete resection, mitotane in combination with cytotoxic drugs are promising treatment regimens. Despite of the treatment, the German ACC Registry demonstrated an overall survival of 47% after 5 years and 41% after 10 years, and in patients with metastases (stage IV) median survival is <15 months [26]. The overall prognosis is limited indicating the need for improved therapies directed at potential molecular targets, the molecular pathogenesis of ACC has thus attracted growing attention during the last decade [27, 28]. To the best of our knowledge, however, the angiogenic status of ACC and the correlation of HPA-1 and VEGF with MVD as indicator of angiogenesis in ACC have not been studied to date. In this study, we evaluated HPA-1, VEGF, and VEGFR-2 expression to clarify their usefulness as candidate molecular targets and determine if they correlate with angiogenesis in ACC.
Angiogenesis, an indispensable step in the progression of a variety of solid tumors, is related to tumor growth and may be a prognostic factor involved in tumor metastasis. MVD has been regarded as a golden standard that assess significant angiogenesis in tumors [8]. The microvessel count in tumor was made by highlighting the tumor-derived vascular ECs using monoclonal antibodies CD-31, CD-34, VIII factor, etc. [29]. There has been no further study on angiogenic status in ACC since Diaz-Cano SJ and his colleagues first published their article in 2001 [30], now we adopted CD34 immunostaining to assess MVD in our study and calculated the mean value of the CD34-positive vessel counts in the three selected hot spots per section. Our results demonstrated that expression of MVD was higher in malignant cases than benign tumors (84.70 ± 12.44 vs. 21.05 ± 8.07).
VEGF, an important and powerful stimulant of angiogenesis, binds and activates VEGFR2 to induce EC proliferation and promote EC migration [31]. Two VEGF receptors are present on ECs, VEGF receptor-1 (VEGFR-1), and VEGFR-2. Only VEGFR-2 is capable of mediating angiogenesis [7]. VEGF also increases the permeability of the endothelium of blood vessels, which in turn allows for cancerous cells to penetrate the vessel walls and become metastasis. Overexpression of VEGF has been reported in a number of tumor types and appears of significant prognostic value in various malignant tumors, including ACC [14]. Zacharieva and de Fraipont et al. [32, 33] demonstrated VEGF is significantly elevated in tumor tissue and circulating blood in patients with ACC. Our results are in line with previous studies that demonstrate ACCs appeared to have high angiogenic potential because they showed increased VEGF expression (70.83%, 17/24) in comparison to that observed in adenomas (25%, 5/20). There are few researches on VEGFR2 expression in tumor tissue of ACC and the relationship between VEGF expression and the degree of angiogenesis which expressed as MVD. We observed that VEGFR-2 strongly expressed in the majority of ACCs (79.17%, 19/24) and lowly in the ACA group (25%, 5/20). VEGF expression also showed the positive correlation with MVD count in ACC, that was, the stronger the expression of VEGF, the higher the MVD (r_s = 0.834, P < 0.001).
The nucleotide sequence of HPA-1 gene has been cloned and identified in mammals including human beings since 1999. HPA-1 is an endo-β-d-glucuronidase, which specifically degrades heparin sulfate side chains of heparin sulfate proteoglycans in the ECM and BM. Human HPA-1 protein expression were found to be upregulated in various types of primary tumors and were thought to facilitate metastasis by enabling tumor cells to invade tissue stroma and blood vessels, allowing tumor spread to surrounding tissues and distant organs [34, 35]. There has been no further study on HPA-1 expression in ACC, and we found that positive staining for HPA-1 was observed in 15% of ACA and 91.67% of ACC. Studies by Elkin et al. [36] have confirmed HPA-1’s role as a mediator in angiogenesis, specifically by freeing basic fibroblast growth factor (bFGF), VEGF, and HS degradation fragments that promote bFGFR binding and signaling. In this study, we found that expressions of HPA-1 in ACAs and ACCs were directly correlated with MVD (r_s = 0.812, P = 0.001), which confirmed the important role of HPA-1 in angiogenesis. Moreover, the MVD counts were increased in VEGF or HPA-1 positive tumors, and significantly upregulated in both VEGF and HPA-1 positive tumors. The ability of HPA-1 to promote angiogenesis and its involvement in metastasis make it to be a promising target for therapy of ACC.
In conclusion, our data show that HPA-1, VEGF, and VEGFR-2 expressions are higher in ACCs than ACAs. We find a statistically significant correlation among HPA-1 and VEGF, and MVD. Accordingly we presume that these proteins involved in angiogenesis may be potential molecular targets for the treatment of ACC, and prospective studies are needed to confirm whether they may be used as biomarkers to identify the patients who gain benefit from anti-angiogenic agents and to monitor the prognosis of ACCs.
References:
M. Fassnacht, R. Libe, M. Kroiss et al., Adrenocortical carcinoma: a clinician’s update. Nat. Rev. Endocrinol. 7, 323–335 (2011)
B. Allolio, M. Fassnacht, Clinical review: adrenocortical carcinoma: clinical update. J. Clin. Endocrinol. Metab. 91, 2027–2037 (2006)
M. Fassnacht, B. Allolio, What is the best approach to an apparently nonmetastatic adrenocortical carcinoma? Clin. Endocrinol. (Oxf) 73, 561–565 (2010)
A. Berruti, M. Fassnacht, E. Baudin et al., Adjuvant therapy in patients with adrenocortical carcinoma: a position of an international panel. J. Clin. Oncol. 28, 401–403 (2010)
D.E. Schteingart, G.M. Doherty, P.G. Gauger et al., Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr. Relat. Cancer 12, 667–680 (2005)
I.J. Fidler, L.M. Ellis, The implications of angiogenesis for the biology and therapy of cancer metastasis. Cell 79, 185–188 (1994)
N. Ferrara, Role of vascular endothelial growth factor in regulation of physiological angiogenesis. Am. J. Physiol. Cell. Physiol. 280, C1358–C1366 (2001)
N. Weidner, Intratumor microvessel density as a prognostic factor in cancer. Am. J. Pathol. 147, 9–19 (1995)
H. Sawai, Y. Okada, H. Funahashi et al., Basement membrane proteins play an important role in the invasive processes of human pancreatic cancer cells. J. Surg. Res. 144, 117–123 (2008)
M. Bernfield, M. Gotte, P.W. Park et al., Functions of cell surface heparan sulfate proteoglycans. Annu. Rev. Biochem. 68, 729–777 (1999)
C.R. Parish, C. Freeman, M.D. Hulett, Heparanase: a key enzyme involved in cell invasion. Biochim. Biophys. Acta 1471, M99–M108 (2001)
I. Vlodavsky, Y. Friedmann, Molecular properties and involvement of heparanase in cancer metastasis and angiogenesis. J. Clin. Invest. 108, 341–347 (2001)
H. Wang, J.L. Si, X.Z. Zhang et al., Expression and clinical significance of syndecan-1 mRNA and HPA-1 mRNA in colorectal cancer detected with real-time fluorescent quantitative polymerase chain reaction. Chin. J. Cancer 29, 288–293 (2010)
K.S. Rohrberg, B.G. Skov, U. Lassen et al., Markers of angiogenesis and epidermal growth factor receptor signalling in patients with pancreatic and gastroesophageal junction cancer. Cancer Biomark. 7, 141–151 (2010)
U. Yildirim, H. Erdem, A. Kayikci et al., Cyclooxygenase-2 and survivin in superficial urothelial carcinoma of the bladder and correlation with intratumoural microvessel density. J. Int. Med. Res. 38, 1689–1699 (2010)
J.C. Yang, L. Haworth, R.M. Sherry et al., A randomized trial of bevacizumab an anti-vascular endothelial growth factor antibody for metastatic renal cancer. N. Engl. J. Med. 349, 427–434 (2003)
A. Sandler, R. Gray, M.C. Perry et al., Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N. Engl. J. Med. 355, 2542–2550 (2006)
B. Ramaswamy, A.D. Elias, N.T. Kelbick et al., Phase II trial of bevacizumab in combination with weekly docetaxel in metastatic breast cancer patients. Clin. Cancer Res. 12, 3124–3129 (2006)
S. Wortmann, M. Quinkler, C. Ritter et al., Bevacizumab plus capecitabine as a salvage therapy in advanced adrenocortical carcinoma. Eur. J. Endocrinol. 162, 349–356 (2010)
L.M. Weiss, L.J. Medeiros Jr, A.L. Vickery, Pathologic features of prognostic significance in adrenocortical carcinoma. Am. J. Surg. Pathol. 13, 202–206 (1989)
R. Kouyama, K. Hiraishi, T. Sugiyama et al., Clinicopathological features, biochemical and molecular markers in 5 patients with adrenocortical carcinoma. Endocr. J. 2011 Apr 27. [Epub ahead of print]
Y. Kitadai, K. Haruma, T. Tokutomi et al., Significance of vessel count and vascular endothelial growth factor in human esophageal carcinomas. Clin. Cancer Res. 4, 2195–2200 (1998)
Y. Zhu, H.C. He, F. Yuan et al., Heparanase-1 and cyclooxygenase-2: prognostic indicators of malignancy in pheochromocytomas. Endocrine 38, 93–99 (2010)
I. Veytsman, L. Nieman, T. Fojo, Management of endocrine manifestations and the use of mitotane as a chemotherapeutic agent for adrenocortical carcinoma. J. Clin. Oncol. 27, 4619–4629 (2009)
I.G. Hermsen, M. Fassnacht, M. Terzolo et al., Plasma concentrations of o, p′DDD, o, p′DDA, and o, p′DDE as predictors of tumor response to mitotane in adrenocortical carcinoma: results of a Retrospective ENS@T Multicenter Study. J. Clin. Endocrinol. Metab. 96, 1844–1851 (2011)
M. Fassnacht, S. Johanssen, M. Quinkler et al., Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: proposal for a revised TNM classification. Cancer 115, 243–250 (2009)
T.J. Giordano, R. Kuick, T. Else et al., Molecular classification and prognostication of adrenocortical tumors by transcriptome profiling. Clin. Cancer Res. 15, 668–676 (2009)
A. de Reynies, G. Assie, D.S. Rickman et al., Gene expression profiling reveals a new classification of adrenocortical tumors and identifies molecular predictors of malignancy and survival. J. Clin. Oncol. 27, 1108–1115 (2009)
J.B. Laforga, F.I. Aranda, Angiogenic index: a new method for assessing microvascularity in breast carcinoma with possible prognostic implications. Breast J. 6, 103–107 (2000)
S.J. Diaz-Cano, M. de Miguel, A. Blanes, H. Galera, H.J. Wolfe, Contribution of the microvessel network to the clonal and kinetic profiles of adrenal cortical proliferative lesions. Hum. Pathol. 32, 1232–1239 (2001)
R.S. Kerbel, Tumor angiogenesis. N. Engl. J. Med. 358, 2039–2049 (2008)
S. Zacharieva, I. Atanassova, M. Orbetzova et al., Circulating vascular endothelial growth factor and active renin concentrations and prostaglandin E2 urinary excretion in patients with adrenal tumours. Eur. J. Endocrinol. 150, 345–349 (2004)
F. de Fraipont, M. El Atifi, C. Gicquel et al., Expression of the angiogenesis markers vascular endothelial growth factor-A, thrombospondin-1, and platelet-derived endothelial cell growth factor in human sporadic adrenocortical tumors: correlation with genotypic alterations. J. Clin. Endocrinol. Metab. 85, 4734–4741 (2000)
M.D. Hulett, C. Freeman, B.J. Hamdorf et al., Cloning of mammalian heparanase, an important enzyme in tumor invasion and metastasis. Nat. Med. 5, 803–809 (1999)
K. Gohji, H. Hirano, M. Okamoto et al., Expression of three extracellular matrix degradative enzymes in bladder cancer. Int. J. Cancer 95, 295–301 (2001)
M. Elkin, N. Ilan, R. Ishai-Michaeli et al., Heparanase as mediator of angiogenesis: mode of action. FASEB. J. 15, 1661–1663 (2001)
Acknowledgments
This study was supported by Shanghai Municipal Natural Science Foundation (No. 09ZR1418500) and Innovation Program of Shanghai Municipal Education Commission (No. 11YZ58).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, Yz., Zhu, Y., Shen, Zj. et al. Significance of heparanase-1 and vascular endothelial growth factor in adrenocortical carcinoma angiogenesis: potential for therapy. Endocrine 40, 445–451 (2011). https://doi.org/10.1007/s12020-011-9502-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-011-9502-1