Abstract
Insulin resistance is getting important in the course of type 1 diabetes mellitus. Visceral fat depot is associated with insulin resistance and assessment of epicardial fat thickness is a way of measuring visceral fat. The aim of the study was to measure epicardial adipose tissue (EAT) thickness and to determine its relationship with waist-hip-ratio (WHR) and estimated glucose disposal rate (eGDR) in adult type 1 diabetic patients. Thirty-six type 1 diabetic patients (aged 31 ± 8 years; Female/Male: 22/14) and 43 age, gender and BMI matched healthy controls were included. Fasting blood glucose (FBG), hemoglobin A1c, and lipid profiles were measured. Waist-hip-ratio (WHR) was calculated. Daily insulin dose/kg of patients were recorded and eGDR of all subjects was calculated. Epicardial adipose tissue (EAT) thickness was evaluated by echocardiography. EAT thickness of the type 1 diabetic patients was significantly higher than controls (3.30 ± 1.06 vs. 2.30 ± 0.34 mm, P < 0.0001). EAT thickness was correlated with age (P = 0.05; r = 0.35), WHR (P = 0.003; r = 0.67), daily insulin dose/kg (r = 0.45, P = 0.005), and eGDR (r = −0.55, P = 0.0004). Multivariate analysis revealed WHR and eGDR to be related to EAT among age, WHR, daily insulin dose/kg, eGDR, FBG, and hemoglobin A1c (r2 of the model = 0.64). Epicardial adipose tissue thickness is increased in type 1 diabetic patients compared to controls and is related to WHR and eGDR in this group of patients. This measurement may point to the presence of insulin resistance in type 1 diabetic patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is the leading cause of death in the type 1 diabetic population [1, 2]. Insulin resistance is known to contribute to the development of cardiovascular disease in type 2 diabetes mellitus (DM) [3, 4]. The influence of insulin resistance on the macrovascular complications in type 1 diabetic patients has been pointed out previously [5–7].
Recent data indicate that the prevalence of obesity has increased during the course of type 1 DM [5, 8]. Visceral obesity is an established risk factor for the appearance of insulin resistance and is related to the development of cardiovascular disease in the general population [9–11]. Iacobelis et al. have proposed epicardial adipose tissue (EAT) determination as a surrogate for visceral fat [12]. EAT is the visceral fat tissue deposited between the myocardium and the pericardium [13].
EAT detection by echocardiography is correlated with anthropometric measurements and MRI determination of visceral fat, which is the gold standard [12]. EAT was demonstrated to be related to anthropometric and metabolic components of the metabolic syndrome [14]. EAT has also been found to be correlated with atrial enlargement and diastolic dysfunction in obese people [15, 16]. We recently showed that it was related to decreased flow-mediated dilatation in patients with metabolic syndrome [17]. EAT has also been correlated with the severity of coronary artery disease, assessed by coronary angiography [18]. Thus, EAT thickness has been considered to be a possible cardiovascular risk indicator [19, 20].
Considering metabolic syndrome a clinical surrogate for insulin resistance, the prevalence of metabolic syndrome in type 1 DM has been reported to be around 20%. [8, 21, 22]. Therefore, determination of EAT thickness by echocardiography, which is a simple measurement in an experienced hand, may give a clue as to the presence of insulin resistance in this population of patients.
The aim of our study was to determine EAT thickness in type 1 diabetic patients and determine its relationship with anthropometric measurements and estimated glucose disposal rate (eGDR), another method of measuring insulin sensitivity in type 1 diabetic patients.
Materials and methods
Patients
Thirty-six type 1 diabetic patients, having this diagnosis for at least 1 year, were consecutively included in the study. The control group consisted of 43 sex and age-matched healthy people. The study protocol was approved by the local research ethics committee and was carried out in accordance with the declaration of Helsinki. All subjects gave written informed consent.
Medical history was obtained and physical examination was performed in all patients and controls. Electrocardiogram was recorded. Blood was withdrawn from all subjects following 12 h of fasting. Two or more timed overnight urine collections were used to measure urinary albumin excretion. Fundoscopic eye examinations were performed to assess retinopathy. Patients were evaluated for neuropathy by medical history and neurologic examination. Daily insulin dose/kg of patients were recorded.
Subjects with ischemic heart disease, valvular heart disease, congestive heart failure, any other systemic disease, such as inflammatory diseases, patients with cardiac symptoms, and abnormal ECG were excluded.
Anthropometric measurements
Anthropometric measurements of body weight, height, waist circumference, and hip circumference were made with the patient dressed in underwear. BMI was calculated as body weight divided by the square of the height. Waist circumference was measured at the midpoint between the lateral iliac crest and lowest rib. Hip circumference was measured at the level of the greater trochanter. Waist-hip-ratio (WHR) was calculated as the ratio of waist circumference to hip circumference.
Assessment of epicardial adipose tissue thickness
Each subject underwent transthoracic 2-dimensional M-mode echocardiography. Echocardiograms were performed with a GE Vingmed, System Five (Horten, Norway) by standard techniques with subjects in the left lateral decubitus position at end-diastole. The echocardiographer was blinded to whether the subject had diabetes or was a control. Epicardial adipose tissue thickness was measured on the free wall of right ventricle from both parasternal long- and short-axis views, with optimal cursor beam orientation at each view. Epicardial adipose tissue appeared as an echo-free or hyperechoic space, if it was massive. The maximum values at each site were measured and the mean of the measures obtained at both views was also taken.
Biochemical measurements
Hemoglobin A1c (HbA1c) levels were measured by high pressure liquid chromatography (HPLC) with a Thermo system. Fasting blood glucose (FBG), total cholesterol, HDL cholesterol, LDL cholesterol, and triglycerides were measured by enzymatic colorimetric assays (Roche Diagnostics GmbH, Mannheim, Germany). Estimated glucose disposal rate (eGDR) was calculated as defined before [23].
Statistical analysis
Statistical analysis was performed with a SPSS software package. Categorical variables were expressed as number while continuous variables were expressed as mean ± standard deviation. Pearson chi-square (χ 2) test was used to compare groups regarding categorical variables. Continuous variables were compared with Student T-test (while comparing parametric variables between diabetic patients and controls) or Mann–Whitney U test (while comparing nonparametric variables between diabetic patients and controls).
Correlation analysis was performed using Pearson or Spearman tests where appropriate to determine the relationship between EAT thickness and age, BMI, duration of diabetes, WHR, FBG, hemoglobin A1c, total cholesterol, triglycerides, HDL, and LDL cholesterol. Linear regression analysis was used to explore the independent determinants of EAT. Levels of statistical significance were set at a P value < 0.05.
Results
The demographic findings and laboratory values of the study groups are shown on Table 1. Fasting blood glucose and hemoglobin A1c levels were higher in the diabetic group compared to controls. Two patients had retinopathy, five patients had microalbuminuria, and no patients had neuropathy. Daily insulin doses and estimated glucose disposal rate (eGDR) of the patients were presented on Table 1. None of the patients had a stigmata of insulin resistance such as acanthosis nigricans.
EAT thickness, measured on the long axis, short axis and their average were all increased in the patients group in comparison to the control group (Table 2).
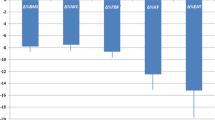
The mean EAT thickness was correlated with age (P = 0.05; r = 0.35); WHR (P = 0.003; r = 0.67) (Fig. 1), daily insulin dose/kg of the patients (P = 0.005, r = 0.45), negatively with eGDR (P = 0.0004, r = −0.55) (Fig. 2) and at a borderline significance with FBG (P = 0.06; r = 0.41). On the other hand, no correlation of EAT was observed with body mass index (BMI), duration of diabetes, hemoglobin A1c, total cholesterol, triglycerides, HDL, and LDL cholesterol. In the control group, the mean EAT was correlated with age (P = 0.05; r = 0.35), whereas no correlation was observed with WHR (Fig. 1), BMI, FBG, total cholesterol, triglycerides, HDL, and LDL cholesterol levels.
When linear regression analysis was performed with EAT as the dependent variable and age, WHR, FBG, and hemoglobin A1c as the independent ones, only WHR was related to EAT (r2 of the model = 0.54). When a second model was created with EAT as the dependent variable and age, WHR, daily insulin dose/kg, eGDR, HbA1c, and FBG as the independent variables, WHR and eGDR had significant association (r2 of the model = 0.64).
Discussion
This study shows that epicardial fat thickness is increased in type 1 diabetic patients and is correlated with the clinical surrogate of insulin resistance, WHR and eGDR, another method of determining insulin sensitivity.
EAT is a form of visceral adipose tissue. Epicardial, mesenteric, and omental fat all share the same origin from the splanchnopleuric mesoderm [24]. Similar to visceral fat, epicardial fat has been suggested to be a metabolic and cardiovascular risk indicator [19, 20, 25]. EAT is demonstrated to play role in adiposity-related inflammation and atherosclerosis, through paracrine secretion of pro- and anti-inflammatory cytokines [26]. EAT determined by echocardiography has been found to be correlated with coronary artery disease proven by angiography [18, 27–29].
Increased EAT thickness has been previously determined in type 2 diabetic patients [30], patients with metabolic syndrome, obese patients with insulin resistance [14, 31], and impaired fasting glucose [32].
The presence of metabolic syndrome in type 1 DM has been investigated. Since the prevalence of obesity in the general population has increased [33], the same increase may be anticipated in type 1 diabetic patients. In the DCCT population, the prevalence of metabolic syndrome was 15.5% in the conventionally treated group and 13.7% in the intensively treated group and these figures increased to 27.2 and 45.4%, respectively, during 9 years of follow-up [5]. This rise was attributed to weight gain observed during the study period. A recent study from Hungary reported the prevalence of metabolic syndrome in type 1 diabetics to be 31.1% according to ATP-III criteria and 36.2% according to IDF criteria [34].
Several studies have demonstrated an association between clinical surrogates of insulin resistance and vascular complications in type 1 DM. In the Pittsburg Epidemiology of Diabetes Complications Study [6] and EURODIAB PCS trials [7], insulin resistance has been shown to be an independent risk factor for micro and macrovascular complications of the disease. The FinnDiane group revealed metabolic syndrome to be a risk factor for cardiovascular disease, mortality, and progression of diabetic nephropathy in type 1 diabetic patients [21].
The assessment of insulin resistance in type 1 diabetic patients has been done through the measurement of anthropometric parameters and through the determination of eGDR, besides the labor-intensive and invasive euglycemic-hyperinsulinemic clamp [25, 26]. Anthropometric measurements are clinical tools, but euglycemic-hyperinsulinemic clamp is the gold standard method, although being difficult to perform. eGDR calculation is correlated with insulin resistance determined by the clamp method [23]. Since EAT has been suggested to be a marker of visceral adiposity, consequently of insulin resistance, determination of EAT may be a simpler measure in type 1 diabetic patients. As for our relatively well controlled type 1 diabetic group, EAT determined by echocardiography was increased in comparison to age and weight matched controls. This is in keeping with the previous reports of increased prevalence of obesity and insulin resistance in type 1 diabetic patients [5–8, 21, 34].
Our results showed EAT thickness was correlated with age, WHR, daily insulin dose/kg and eGDR and at a borderline significance with FBG, but when multiple regression analysis was performed only WHR and eGDR seemed to be related. This finding is not surprising, since EAT has been previously shown to be correlated with abdominal visceral fat measurements [14], for which WHR is a clinical marker. Our results are in agreement with some of the previous findings. In patients with metabolic syndrome, EAT was correlated with waist, BMI, and fat mass, while no correlation was shown with age [14]. EAT was correlated with fasting plasma glucose and waist circumference in patients with impaired fasting glucose [32]. Right ventricular EAT has also been shown to be related to waist circumference, diastolic blood pressure, and high levels of insulin in some other populations [12, 15]. Moreover, the fact that EAT thickness is related to eGDR, which itself is correlated with the clamp method [23], may suggest that EAT determination is a suitable method for determination of insulin resistance in type 1 diabetic patients.
In conclusion, EAT thickness, which is a simple method for determination of visceral fat, was increased in type 1 diabetic patients compared to controls. EAT thickness was related to WHR and eGDR. The results from this limited population of patients may suggest using EAT determination as a marker for insulin resistance in type 1 diabetics. Future studies with larger populations are needed to confirm these findings and demonstrate the efficacy of EAT measurements in determining cardiovascular risk in type 1 diabetic patients.
References
S.S. Soedamah-Muthu, J.H. Fuller, H.E. Mulnier, V.S. Raleigh, R.A. Lawrenson, H.M. Colhoun, All-cause mortality rates in patients with type 1 diabetes mellitus compared with a non-diabetic population from the UK general practice research database, 1992–1999. Diabetologia 49, 660–666 (2006)
G. Pambianco, T. Costacou, D. Ellis, D.J. Becker, R. Klein, T.J. Orchard, The 30-year natural history of type 1 diabetes complications: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes 55, 1463–1469 (2006)
E. Bonora, G. Formentini, F. Calcaterra, S. Lombardi, F. Marini, L. Zenari, F. Saggiani, M. Poli, S. Perbellini, A. Raffaelli, V. Cacciatori, L. Santi, G. Targher, R. Bonadonna, M. Muggeo, HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care 25, 1135–1141 (2002)
A.J. Hanley, K. Williams, M.P. Stern, S.M. Haffner, Homeostasis model assessment of insulin resistance in relation to the incidence of cardiovascular disease: the San Antonio Heart Study. Diabetes Care 25, 1177–1184 (2002)
E.S. Kilpatrick, A.S. Rigby, S.L. Atkin, Insulin resistance, the metabolic syndrome, and complication risk in type 1 diabetes: “double diabetes” in the DiabetesControl and Complications Trial. Diabetes Care 30, 707–712 (2007)
T.J. Orchard, J.C. Olson, J.R. Erbey, K. Williams, K.Y. Forrest, L. Smithline Kinder, D. Ellis, D.J. Becker, Insulin resistance-related factors, but not glycemia, predict coronary artery disease in type 1 diabetes: 10-year follow-up data from the Pittsburgh Epidemiology of Diabetes Complications Study. Diabetes Care 26, 1374–1379 (2003)
S.S. Soedamah-Muthu, N. Chaturvedi, M. Toeller, B. Ferriss, P. Reboldi, G. Michel, C. Manes, J.H. Fuller, EURODIAB Prospective Complications Study Group: risk factors for coronary heart disease in type 1 diabetic patients in Europe: the EURODIAB Prospective Complications Study. Diabetes Care 27, 530–537 (2004)
M. McGill, L. Molyneaux, S.M. Twigg, D.K. Yue, The metabolic syndrome in type 1 diabetes: does it exist and does it matter? J. Diabetes Complicat. 22, 18–23 (2008)
K.M. Rexrode, J.E. Buring, J.E. Manson, Abdominal and total adiposity and risk of coronary heart disease in men. Int. J. Obes. Relat. Metab. Disord. 25, 1047–1056 (2001)
K.M. Rexrode, V.J. Carey, C.H. Hennekens, E.E. Walters, G.A. Colditz, M.J. Stampfer, W.C. Willett, J.E. Manson, Abdominal adiposity and coronary heart disease in women. JAMA 280, 1843–1848 (1998)
A.N. Peiris, M.S. Sothmann, R.G. Hoffmann, M.I. Hennes, C.R. Wilson, A.B. Gustafson, A.H. Kissebah, Adiposity, fat distribution, and cardiovascular risk. Ann. Intern. Med. 110, 867–872 (1989)
G. Iacobellis, F. Assael, M.C. Ribaudo, A. Zappaterreno, G. Alessi, U. Di Mario, F. Leonetti, Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes. Res. 11, 304–310 (2003)
J. Shirani, K. Berezowski, W.C. Roberts, Quantitative measurement of normal and excessive (cor adiposum) subepicardial adipose tissue, its clinical significance, and its effect on electrocardiographic QRS voltage. Am. J. Cardiol. 76, 414–418 (1995)
G. Iacobellis, M.C. Ribaudo, F. Assael, E. Vecci, C. Tiberti, A. Zappaterreno, U. Di Mario, F. Leonetti, Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J. Clin. Endocrinol. Metab. 88, 5163–5168 (2003)
A.E. Malavazos, F. Ermetici, C. Coman, M.M. Corsi, L. Morricone, B. Ambrosi, Influence of epicardial adipose tissue and adipocytokine levels on cardiac abnormalities in visceral obesity. Int. J. Cardiol. 121, 132–134 (2007)
G. Iacobellis, F. Leonetti, N. Singh, A.M. Sharma, Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. Int. J. Cardiol. 115, 272–273 (2007)
H. Aydin, A. Toprak, O. Deyneli, D. Yazici, O. Tarçin, S. Sancak, D. Yavuz, S. Akalin, Epicardial fat tissue thickness correlates with endothelial dysfunction and other cardiovascular risk factors in patients with metabolic syndrome. Metab. Syndr. Relat. Disord. 8, 229–234 (2010)
R. Taguchi, J. Takasu, Y. Itani, R. Yamamoto, K. Yokoyama, S. Watanabe, Y. Masuda, Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis 157, 203–209 (2001)
G. Iacobellis, A.M. Sharma, Epicardial adipose tissue as new cardio-metabolic risk marker and potential therapeutic target in the metabolic syndrome. Curr. Pharm. Des. 13, 2180–2184 (2007)
A.M. de Vos, M. Prokop, C.J. Roos, M.F. Meijs, Y.T. van der Schouw, A. Rutten, P.M. Gorter, M.J. Cramer, P.A. Doevendans, B.J. Rensing, M.L. Bartelink, B.K. Velthuis, A. Mosterd, M.L. Bots, Peri-coronary epicardial adipose tissue is related to cardiovascular risk factors and coronary artery calcification in post-menopausal women. Eur. Heart J. 29, 777–783 (2008)
L.M. Thorn, C. Forsblom, J. Fagerudd, M.C. Thomas, K. Pettersson-Fernholm, M. Saraheimo, J. Wadén, M. Rönnback, M. Rosengård-Bärlund, C.G. Björkesten, M.R. Taskinen, P.H. Groop, FinnDiane Study Group: metabolic syndrome in type 1 diabetes: association with diabetic nephropathy and glycemic control (the FinnDiane study). Diabetes Care 28, 2019–2024 (2005)
G. Pambianco, T. Costacou, T.J. Orchard, The prediction of major outcomes of type 1 diabetes: a 12-year prospective evaluation of three separate definitions of the metabolic syndrome and their components and estimated glucose disposal rate: the Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes Care 30, 1248–1254 (2007)
K.V. Williams, J.R. Erbey, D. Becker, S. Arslanian, T.J. Orchard, Can clinical factors estimate insulin resistance in type 1 diabetes? Diabetes 49, 626–632 (2000)
E. Ho, Y. Shimada, Formation of the epicardium studied with the scanning electron microscope. Dev. Biol. 66, 579–585 (1978)
J.M. Marchington, C.A. Mattacks, C.M. Pond, Adipose tissue in the mammalian heart and pericardium: structure, foetal development and biochemical properties. Biochem. Physiol. B. 94, 225–232 (1989)
G. Iacobellis, G. Barbaro, The double role of epicardial adipose tissue as pro- and anti-inflammatory organ. Horm. Metab. Res. 40, 442–445 (2008)
N. Chaowalit, V.K. Somers, P.A. Pellikka, C.S. Rihal, F. Lopez-Jimenez, Subepicardial adipose tissue and the presence and severity of coronary artery disease. Atherosclerosis 186, 354–359 (2006)
R. Djaberi, J.D. Schuijf, J.M. Van Werkhoven, G. Nucifora, J.W. Jukema, J.J. Bax, Relation of epicardial adipose tissue to coronary atherosclerosis. Am. J. Cardiol. 102, 1602–1607 (2008)
S. Eroglu, L.E. Sade, A. Yildirir, U. Bal, S. Ozbicer, A.S. Ozgul, H. Bozbas, A. Aydinalp, H. Muderrisoglu, Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr. Metab. Cardiovasc. Dis. 19, 211–217 (2009)
C.P. Wang, H.L. Hsu, W.C. Hung, T.H. Yu, Y.H. Chen, C.A. Chiu, L.F. Lu, F.M. Chung, S.J. Shin, Y.J. Lee, Increased epicardial adipose tissue (EAT) volume in type 2 diabetes mellitus and association with metabolic syndrome and severity of coronary atherosclerosis. Clin. Endocrinol. (Oxf.) 70, 876–882 (2009)
G. Iacobellis, F. Leonetti, Epicardial adipose tissue and insulin resistance in obese subjects. J. Clin. Endocrinol. Metab. 90, 6300–6302 (2005)
G. Iacobellis, G. Barbaro, H.C. Gerstein, Relationship of epicardial fat thickness and fasting glucose. Int. J. Cardiol. 128, 424–426 (2008)
N. Mattsson, T. Rönnemaa, M. Juonala, J.S. Viikari, O.T. Raitakari, The prevalence of the metabolic syndrome in young adults. The Cardiovascular Risk in Young Finns Study. J. Intern. Med. 261, 159–169 (2007)
J. Nádas, Z. Putz, J. Fövényi, Z. Gaál, A. Gyimesi, T. Hídvégi, N. Hosszúfalusi, G. Neuwirth, T. Oroszlán, P. Pánczél, G. Széles, G. Vándorfi, G. Winkler, I. Wittmann, G. Jermendy, Cardiovascular risk factors characteristic for the metabolic syndrome in adult patients with type 1 diabetes. Exp. Clin. Endocrinol. Diabetes 117, 107–112 (2009)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yazıcı, D., Özben, B., Yavuz, D. et al. Epicardial adipose tissue thickness in type 1 diabetic patients. Endocrine 40, 250–255 (2011). https://doi.org/10.1007/s12020-011-9478-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-011-9478-x