Abstract
To investigate the SDHAF2 gene and its effect on primary hyperparathyroidism. Parathyroid tumors causing primary hyperparathyroidism (pHPT) are one of the more common endocrine neoplasias. Loss of heterozygosity at chromosome 11q13 is the most common chromosomal aberration in parathyroid tumors occurring in about 40% of sporadic tumors. Only 15–19% display somatic mutations in the MEN1 gene, which suggest that this chromosomal region may harbor additional genes of importance in parathyroid tumor development. The SDHAF2 (formerly SDH5) gene is a recently identified neuroendocrine tumor suppressor gene at this locus, and inherited mutations of the SDHAF2 gene has been linked to familial paraganglioma. We demonstrate that the SDHAF2 gene is expressed in parathyroid tissue using RT-PCR. Because detection of inactivating mutations is the major criterion for validating a candidate tumor suppressor, we used automated sequencing of the coding region and intron/exon boundaries in 80 sporadic parathyroid adenomas from patients with pHPT. A known polymorphisms (A to G substitution; rs879647) was identified in 9/80 parathyroid tumors but no tumor-specific somatic mutational aberrations, such as nonsense, frameshift, or other inactivating mutations were identified. The SDHAF2 gene is expressed in parathyroid tissue. However, somatic mutations of the SDHAF2 tumor suppressor gene are unlikely to frequently contribute to parathyroid tumor development in sporadic pHPT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There exist common genetic etiologies of tumor development among the endocrine glands, which is exemplified by inherited tumor-susceptibility syndromes such as multiple endocrine neoplasia (MEN) type 1 and 2, causing tumors of e.g., the parathyroid, and adrenal medulla (pheochromocytoma) [1]. Parathyroid tumors causing primary hyperparathyroidism (pHPT) is one of the more common endocrine tumors with a 2.3% prevalence in postmenopausal females [2]. Studies have so far identified genetic alterations in the cyclin D1 oncogene, the tumor suppressor genes MEN1 (located at chromosome 11q13), and HRPT2 (located at chromosome 1q25-q32), as pathogenically important for development of sporadic parathyroid tumors [3–6]. LOH at chromosome 11q13 is the most common chromosomal aberration in parathyroid tumors occurring in about 40% of sporadic tumors. However, only about 15–19% of cases display somatic mutations in the MEN1 gene [7–9]. This has lead to the speculation that another, yet identified, tumor suppressor gene on chromosome 11q13 is involved in parathyroid tumor development [10].
Recently, a novel putative neuroendocrine tumor suppressor gene located in the vicinity of the MEN1 gene was isolated. The SDHAF2 gene (also known as SDH5 or PGL2) encodes succinate dehydrogenase complex assembly factor 2 (SDHAF2), a highly conserved cofactor of flavin adenine dinucleotide (FAD) [11]. A missense mutation of the SDHAF2 gene was identified in a Dutch kindred with neuroendocrine paraganglioma of the head and neck. Functional analyses of the inactivating mutation (232G → A; Gly78Arg) showed complete loss of both flavination of SDHA and activity of the succinate dehydrogenase complex [11]. This SDHAF2 gene mutation also displayed parent-of-origin expression phenotype, with onset of tumor development only via the paternal line. SDHAF2 seems to have a role in flavination of SDHA, and correct flavination of SDHA is essential for a functional succinate dehydrogenase complex. Germline mutations in genes encoding succinate dehydrogenase subunits (SDHD, SDHC, or SDHB; formerly known as PGL1, PGL3, and PGL4) cause familial paraganglioma of the head and neck, as well as the thorax and abdomen (termed pheochromocytoma when occurring in the adrenal medulla) [12–15]. The enzyme complex plays a central role in cellular energy metabolism as both a mitochondrial tricarboxylic acid (TCA) cycle enzyme and as the complex II component of the electron transport chain. The role of TCA enzymes as tumor suppressors has broadened since the identification of the SDHD gene in 2000 [14], with mutations of fumarate hydratase reported as the cause of hereditary renal-cell cancer and leiomyomatosis [16], and the identification of somatic genetic aberrations of isocitrate dehydrogenase genes in glioblastoma [17].
In recent years, some groups have focused their attention toward mitochondrial DNA (mtDNA) and its role in the predisposition of cancer, especially among slowly progressing neoplasms. Costa-Guda et al. [18] analyzed and proved that within a majority of sporadic parathyroid adenomas there was indeed mutations present in the mtDNA. The mutations of this DNA have been implicated in the malfunction of the respiratory chain within the mitochondrial complex, particularly complex I. The chain can and is directly affected by reactive oxygen species (ROS), which have been implicated in the damage of DNA especially in slower growing tumors, such as breast, parathyroid, and papillary thyroid carcinoma [19]. The SDHAF2 gene through its role of flavination of SDHA is intricately involved within the electron transport chain of mitochondria [12–15].
In order to examine the role of SDHAF2 gene also in parathyroid tumorigenesis, we demonstrate that the gene is expressed in parathyroid tissue. Mutational analysis, however, failed to identify somatic genetic alteration of the gene, suggesting that mutations of the SDHAF2 tumor suppressor gene are unlikely to frequently contribute to parathyroid tumor development in sporadic pHPT.
Results
SDHAF2 gene expression in human parathyroid tissues
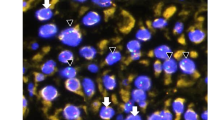
In order to determine whether the SDHAF2 gene is expressed in parathyroid tissue, total RNA was isolated from snap-frozen normal parathyroid cells and adrenal medulla (control). Reverse-transcriptase PCR of the cDNA revealed the expected size fragment in cDNA from normal parathyroid tissue and adrenal medulla (Fig. 1a), and verified by automated sequencing. Additionally, we demonstrated SDHAF2 gene expression in another cohort of 14 sporadic parathyroid adenomas from patients with PHPT and three normal parathyroid tissues (Fig. 1b).
a The novel endocrine tumor suppressor gene, SDHAF2, is expressed in parathyroid cells. Total RNA (10 μg) was isolated from snap-frozen parathyroid tissue and adrenal medulla (control). The expected product is visualized on a 1% agarose gel. Lanes 1 and 8, marker; lane 2, reverse transcriptase; lane 3, cDNA from normal parathyroid cells; lane 4, negative control (H20); lane 5, reverse transcriptase; lane 6, cDNA from adrenal medulla; and lane 7, negative control (H20). b. The novel endocrine tumor suppressor gene, SDHAF2, is expressed in parathyroid cells. Total RNA (10 μg) was isolated from snap-frozen parathyroid tissue both diseased and normal. The expected product is visualized on a 1% agarose gel. Lanes 1 through 14 represent parathyroid Adenomas, and lanes 15–17 are normal parathyroid tissue. Lanes marked “L” denote the DNA Ladder and the “N” is the negative control lane
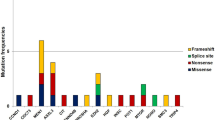
Direct sequence analysis of SDHAF2 in parathyroid tumors
Eighty patients with biochemically proven pHPT due to a single parathyroid adenoma were included in the study to examine whether tumor-specific somatic mutations were present in the SDHAF2 gene. The clinical characteristics of the patients are presented in Table 1. Automated sequencing of all coding regions identified an annotated SNP, rs879647 (A to G substitution in intron 2) in 9/80 parathyroid tumors, as well as in the germline DNA of these patients (Fig. 2). The frequency with which the various alleles were observed was as follows, the G allele was observed in 0.127 of the patients which is not significantly different from the 0.161 allele frequency reported in the HapMap CEU European cohort of 112 individuals (http://www.ncbi.nlm.nih.gov/projects/SNP/snp_ref.cgi?rs=879647). Similarly, the A allele had a similar observed frequency of 0.873 compared to 0.839 in the HapMap CEU European cohort (non significant). No tumor-specific somatic mutational aberrations, such as nonsense, frameshift, or other inactivating mutations were identified.
Discussion
Allelic loss at chromosome 11q13 is one of the most common genetic alterations in parathyroid tumors of pHPT, occurring in approximately 40% of tumors. However, only about 15–19% of parathyroid tumors exhibit somatic mutations in the MEN1 gene of likely importance to parathyroid tumorigenesis [7–9]. A yet to be identified tumor suppressor gene located on chromosome 11q13 also involved in parathyroid tumor development has thus been postulated [10]. The SDHAF2 gene is a novel putative endocrine tumor suppressor gene in the vicinity of the MEN1 gene (Fig. 3). Based on its function in regulating succinate dehydrogenase and the presence of a missense germline mutation in a family with cervical paragangliomas, SDHAF2 may represent an endocrine tumor suppressor [11]. We demonstrate within our study that the SDHAF2 gene is expressed in parathyroid cells; however, the role of its presence within parathyroid tissue has yet to be defined. We believe that the SDHAF2 gene may be an important candidate tumor suppressor gene that could acquire loss of function mutations specifically in the parathyroid tumor genome, leading to a selective advantage and parathyroid tumor development.
Our approach was designed to rigorously test the possibility that SDHAF2 serves as a classic tumor suppressor in the parathyroid glands. Only recurrent inactivating mutations can provide this critical evidence for a driving role of tumorigenesis [20]. We explored the mutational status of the SDHAF2 gene and failed to identify somatic mutations in any of the 80 parathyroid tumors studied. Although our study did not examine the possibility of epigenetic changes or mutations in non-protein coding regions of the gene, it would be unprecedented if inactivating alterations in an authentic tumor suppressor gene were to be found exclusively in these regions without ever appearing in the coding region.
In conclusion, our observations suggest that SDHAF2 acts infrequently, if at all, as a tumor suppressor gene in the molecular pathogenesis of parathyroid adenomas of pHPT.
Materials and methods
Subjects and tumor samples
Biopsies of normal human parathyroid glands were obtained from normocalcemic patients operated for atoxic goiter. These were biopsied due to macroscopic ambiguity of the microscopic diagnosis. Eighty patients with operatively verified, non-familial pHPT due to a single adenoma were included into the study. All the tumors were carefully evaluated by an experienced endocrine pathologist prior to use in the study. Tumors were dissected prior to processing to minimize contamination by normal cells. The tissue was snap frozen in liquid nitrogen and stored at −80°C. None of the patients demonstrated signs of familial hypercalcemia, clinical, and biochemical signs of multiple endocrine neoplasia syndromes nor had a history of previous neck irradiation. Blood was collected after an overnight fast and serum (s-) calcium (reference range 2.20–2.60 mmol/l) and intact s-PTH (reference range 10–65 ng/l) were determined preoperatively. All the patients had postoperatively reversed hypercalcemia during follow-up for at least 6 months. Informed consent was obtained and the study was approved by the institutional review board.
DNA, Total RNA, cDNA synthesis
High-molecular-weight genomic DNA from whole blood, and tumor tissue was isolated by standard methods as previously described [21]. Total RNA from snap-frozen tumor and normal tissue was isolated using the Nucleobond AX RNA Isolation Protocol (Machney-Nagel, Bethlehem, PA) [22]. RNA was not treated with DNAase during the extraction process. cDNA synthesis was performed using the iScript cDNA synthesis kit (Biorad, Hercules, CA).
RT-PCR
PCR reactions were performed using the mRNA specific primers 5′-CAGTGTTCTCGACTTCGTCGC-3′ and 5′-AGCGTCTGAATGATGTCACAC-3′. The PCR conditions were: one cycle of activation at 95°C followed by 30 cycles of amplifications at 95°C for 20 s, 60°C for 20 s, and 72°C for 20 s and a final elongation step at 72°C for 7 min using 50 ng of parathyroid cDNA and 15 pmol of each primer. The PCR products were analyzed on a 1% agarose gel to control the quality of products and exclude unspecific PCR reactions. PCR products were then purified using QIAquick PCR purification kit (Qiagen, Valencia CA) and sequenced by direct sequencing methods.
DNA sequencing of the SDHAF2 gene
The coding regions of the SDHAF2 gene were amplified using the primers in Table 2. The PCR conditions were: one cycle of activation at 95°C followed by 35 cycles of amplifications at 95°C for 20 s, 60°C for 20 s, and 72°C for 20 s and a final elongation step at 72°C for 7 min using 2.5 ng genomic DNA and 15 pmol of each primer. The PCR products were visualized on agarose gel to control the quality of products and exclude unspecific PCR reactions. The PCR products were then purified using QIAquick PCR purification kit (Qiagen, Valencia CA). Each sample (40 ng of DNA) was prepared for submission in 96-well Eppendorf twin tec plates (Eppendorf, Westbury, NY) in accordance with the high volume plate submission policies and procedures at the Yale Cancer Center/W.M. Keck Foundation Biotechnology Resource Laboratory. The sequencing reactions utilized fluorescently-labeled dideoxynucleotides (Big Dye Terminators) and Taq FS DNA polymerase in a thermal cycling protocol. The sequence analysis is carried out on 3,730 capillary instruments (Applied Biosystems Foster City, CA).
Data analysis
Data are analyzed with the use of Sequencing Analysis and AutoAssembler software (Applied Biosystems Foster City, CA), and publically available web based resources (NCBI, GenBank). Statistical analysis was done using SPSS 16 (SPSS Inc, Chicago, IL).
References
T. Carling, Multiple endocrine neoplasia syndrome: genetic basis for clinical management. Curr. Opin. Oncol. 17, 7–12 (2005)
E. Lundgren, J. Rastad et al., Population-based health screening for primary hyperparathyroidism with serum calcium and parathyroid hormone values in menopausal women. Surgery 121, 287–294 (1997)
S.C. Chandrasekharappa, S.C. Guru et al., Positional cloning of the gene for multiple endocrine neoplasia-type 1. Science 276, 404–407 (1997)
J.D.R.C. Carpten, A. Villablanca et al., HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat. Genet. 32, 676–680 (2002)
A. Arnold, H.G. Kim, Clonal loss of one chromosome 11 in a parathyroid adenoma. J. Clin. Endocrinol. Metab. 69, 496–499 (1989)
A. Arnold, H.G. Kim et al., Molecular cloning and chromosomal mapping of DNA rearranged with the parathyroid hormone gene in parathyroid adenoma. J. Clin. Invest. 83, 2034–2040 (1989)
C. Heppner, M.B. Kester et al., Somatic mutations of the MEN1 gene in parathyroid tumours. Nat. Genet. 16, 375–378 (1997)
T. Carling, P. Correa et al., Parathyroid MEN1 gene mutations in relation to clinical characteristics of nonfamilial primary hyperparathyroidism. J. Clin. Endocrinol. Metab. 83, 2960–2963 (1998)
F. Farnebo, B.-T. Teh, S. Kytölä et al., Alterations of the MEN1 gene in sporadic parathyroid tumors. J. Clin. Endocrinol. Metab. 83, 2627–2630 (1998)
T. Carling, Molecular pathology of parathyroid tumors. Trends Endocrinol. Metab. 12, 53–58 (2001)
H.X. Hao, O. Khalimonchuk et al., SDH5, a gene required for flavination of succinate dehydrogenase, is mutated in paraganglioma. Science 325, 1139–1142 (2009)
H.P. Neumann, B. Bausch et al., Germ-line mutations in nonsyndromic pheochromocytoma. N. Engl. J. Med. 346, 1459–1466 (2002)
B.E. Baysal, Clinical and molecular progress in hereditary paraganglioma. J. Med. Genet. 45, 689–694 (2008)
B.E. Baysal, R.E. Ferrell et al., Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 287, 848–851 (2000)
J.P. Bayley, H.P. Kunst et al., SDHAF2 mutations in familial and sporadic paraganglioma and phaeochromocytoma. Lancet Oncol. 11, 366–372 (2010)
I.P. Tomlinson, N.A. Alam et al., Germline mutations in FH predispose to dominantly inherited uterine fibroids, skin leiomyomata and papillary renal cell cancer. Nat. Genet. 30, 406–410 (2002)
H. Yan, D.W. Parsons et al., IDH1 and IDH2 mutations in gliomas. N. Engl. J. Med. 360, 765–773 (2009)
J. Costa-Guda, T. Tokura, S.I. Roth et al., Mitochondrial DNA mutations in oxyphilic and chief cell parathyroid adenomas. BMC Endocr. Disord. 7, 8 (2007)
J.J. Yeh, K.L. Lunetta et al., Somatic mitochondrial DNA (mtDNA) mutations in papillary thyroid carcinomas and differential mtDNA sequence variants in cases with thyroid tumours. Oncogene 19(16), 2060–2066 (2000)
T. Carling, A. Kindmark et al., Vitamin D receptor genotypes in primary hyperparathyroidism. Nat. Med. 1, 1309–1311 (1995)
T. Carling, J. Rastad et al., Reduced vitamin D receptor mRNA levels in parathyroid glands of primary and secondary hyperparathyroidism. J. Clin. Endocrinol. 85, 2000–2003 (2000)
E.R. Fearon, C.V. Dang, Cancer genetics: tumor suppressor meets oncogene. Curr. Biol. 9, R62–R65 (1999)
Acknowledgments
This study was in part supported by the Ohse Research Award (to T.C.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Starker, L.F., Delgado-Verdugo, A., Udelsman, R. et al. Expression and somatic mutations of SDHAF2 (SDH5), a novel endocrine tumor suppressor gene in parathyroid tumors of primary hyperparathyroidism. Endocr 38, 397–401 (2010). https://doi.org/10.1007/s12020-010-9399-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-010-9399-0