Abstract
The objective is to evaluate the association of arterial stiffness [brachial-ankle pulse wave velocity (ba-PWV)] with glycemic control and duration of type 2 diabetes in diabetic subjects with or without hypertension. One thousand Chinese diabetic patients (562 with hypertension, 438 without hypertension) were included in this study. All patients underwent ba-PWV and biochemical measurements. Ba-PWV was significantly higher in diabetic subjects with hypertension than those without hypertension (1779 ± 341 vs. 1691 ± 342 cm/s, P < 0.0001), and these subjects were under similar glycemic control (6.9 ± 1.5 vs. 6.9 ± 1.3, P = 0.86). In diabetic and hypertensive subjects, ba-PWV was positively associated with HbA1c (1715 ± 314 vs. 1851 ± 335 cm/s, in subjects with HbA1c < 6.5% and with HbA1c > 7.0%, respectively, P < 0.0001), as well as duration of diabetes (1671 ± 342 vs. 1791 ± 313 vs. 1861 ± 338 cm/s, in subjects with duration of diabetes <5 years, 5–10 years, and >10 years, respectively, P all < 0.05). In diabetic subjects without hypertension, ba-PWV was not associated with HbA1c (P = 0.47), but associated with duration of diabetes (1503 ± 272 vs. 1692 ± 354 cm/s, in subjects with duration of diabetes <5 years and >10 years, respectively, P = 0.0013). Ba-PWV was higher in diabetic subjects with hypertension than in diabetic subjects without hypertension, suggesting the independent effect of hypertension on arterial stiffness in diabetic subjects. Ba-PWV positively correlated with HbA1c and duration of diabetes in subjects with diabetes and hypertension, suggesting the importance of early glycemic control in the prevention of arterial stiffness and vascular complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atherosclerotic disease is the major complication of type 2 diabetes (T2D), and also, the leading cause of high morbidity and mortality in T2D. Atherosclerosis leads to the degeneration of arterial elasticity which is an important characteristic of the arteries and a direct reflection of their condition [1]. In diabetes, recent evidence indicates that increased arterial stiffness is a stronger risk factor for early mortality. Arterial wall stiffening is exacerbated with diabetes and hypertension, and the stiffening is also increased in common carotid and femoral arteries in diabetes. Arterial stiffness can be assessed non-invasively with measurement of pulse wave velocity (PWV) along the thoracoabdominal aortic pathway by a simple and reproducible method [2]. Previous studies have demonstrated that PWV is an independent predictor of cardiovascular and cerebrovascular mortality in hypertensive patients [3, 4]. A recent study showed that PWV, especially brachial-ankle PWV (ba-PWV) which can be measured within a few minutes, might be useful as a marker of atherosclerotic vascular damage [4]. However, few studies have been performed to investigate the association between PWV, glycemic control, and duration of diabetes. Therefore, the aim of the present study was to evaluate the association of arterial stiffness (ba-PWV) with glycemic control (HbA1c) and duration of diabetes in a large sample of Chinese diabetic subjects with or without hypertension.
Subjects and methods
Subjects
A total of 1,000 patients with T2D were recruited consecutively from the Outpatient Endocrine Clinic at Ruijin Hospital affiliated to Shanghai Jiao-Tong University School of Medicine, China from 2005 to 2007. Diabetes was defined according to the 1999 WHO criteria. The duration of T2D was confirmed by clinical records. The study protocol was approved by the Institutional Review Board of Ruijin Hospital. Signed informed consents were obtained from all study participants.
Clinical and biochemical measurements
Participants were questioned in detail by trained investigators using a structured questionnaire covering sociodemographic factors, smoking habits, alcohol consumption, and general use of medications. In addition, a detailed medical record review was performed. All measurements and procedures were taken with the patients in the fasted state and having refrained from food or drink for at least the previous 10 h. Height and weight were recorded, and body mass index (BMI) was calculated as weight/(height2) and expressed in kg/m2. Waist circumference was measured at the level of the umbilicus with the patient in the standing position. Hip circumference was measured at the level of the trochanter majors. WHR (Waist to Hip Ratio) was calculated as the ratio of the circumference of the waist to the hip. Blood pressure (BP) was measured twice in each patient by an experienced doctor with a standard mercury sphygmomanometer after 15 min resting in a sitting position from the non-dominant arm, and the mean value for systolic blood pressure (SBP) and diastolic blood pressure (DBP) was computed from two readings. The pulse pressure (PP) was calculated as the difference between SBP and DBP. Hypertension was diagnosed if the average of the blood pressure readings was greater than 140 mmHg for SBP or 90 mmHg for DBP or those who had been under treatment by anti-hypertension medications.
The HbA1c level was measured by HPLC (BIO-RAD Company, USA). Serum total cholesterol, triglyceride (TG), high-density lipoprotein (HDL) cholesterol, and low-density lipoprotein (LDL) were measured using an enzymatic colorimetric method (Beckman LX-20, Brea, CA, USA).
PWV measurement
Brachial-ankle pulse wave velocity (ba-PWV) indicates brachial to ankle PWV. It was determined by Colin VP-1000 (Model BP203RPE II, Form PWV/ABI) after patients had rested for 15–30 min. To determine the ba-PWV, pulse waves were measured simultaneously with cuffs placed on the right upper-arm and the right ankle. The difference in the times of the start of the pulse waves was corrected for distance to obtain the ba-PWV. The normal values of ba-PWV (cm/s) in healthy subjects were 1376 ± 373 cm/s (mean ± SD) in males and 1352 ± 222 cm/s in females [5].
Statistical analysis
Statistical analysis was performed using SAS 8.1 (SAS Institute, Cary, NC). All the numerical data were expressed as means ± standard deviations (S.D.) or geometrical mean (95% confidence interval). Comparisons of means were analyzed by one-way analysis of variance (ANOVA). P values <0.05 were considered to be statistically significant.
Results
Characteristics of subjects
Table 1 shows the baseline clinical and biochemical characteristics of diabetic subjects with and without hypertension. There were 438 diabetic patients without hypertension (194 males and 244 females; age, 56.8 ± 8.7 years) and 562 subjects with diabetes and hypertension (246 males and 316 females; age, 60.8 ± 7.8 years). Compared to subjects with diabetes and hypertension, diabetic subjects without hypertension were younger (56.8 ± 8.7 vs. 60.8 ± 7.8 years, P < 0.0001) and had a shorter duration of diabetes (4.9 vs. 6.0 years, P = 0.0024). They also had a lower BMI (23.8 ± 3.4 vs. 25.3 ± 3.4 kg/m2, P < 0.0001), lower waist circumference (85.6 ± 8.6 vs. 89.3 ± 9.2 cm, P < 0.0001), lower WHR (0.90 ± 0.06 vs. 0.92 ± 0.10, P < 0.0001), lower cholesterol (5.12 ± 1.10 vs. 5.30 ± 1.09 mmol/l, P = 0.035) and lower TG (1.21 vs. 1.41 mmol/l, P < 0.0001). Moreover, these diabetic subjects without hypertension had a significantly lower ba-PWV than subjects with diabetes and hypertension (1691 ± 342 vs. 1779 ± 341 cm/s, P < 0.0001). These two groups of subjects had similar glycemic controls (HbA1c), HDL, LDL, and gender ratios.
Correlation between ba-PWV and other variables
Simple correlation analysis revealed that HbA1c (r = 0.143, P < 0.0001), log duration of diabetes (r = 0.197, P < 0.0001) (Fig. 1a, b), age (r = 0.421, P < 0.0001), BMI (r = 0.0788, P = 0.014), waist circumference (r = 0.128, P < 0.0001), waist-to-hip ratio (r = 0.119, P = 0.0002), SBP (r = 0.397, P < 0.0001), DBP (r = 0.198, P < 0.0001), TC (r = 0.115, P = 0.0003), LDL (r = 0.110, P = 0.0005), log TG (r = 0.109, P = 0.006), creatinine (r = 0.0915, P = 0.0042), and log ACR (r = 0.237, P < 0.0001) were all positively and significantly associated with ba-PWV. Multiple linear regression also found that HbA1c (standardized β = 0.0819, P = 0.0046), log duration of diabetes (standardized β = 0.0742, P = 0.0095), age (standardized β = 0.328, P < 0.0001), SBP (standardized β = 0.263, P < 0.0001), and log ACR (standardized β = 0.116, P < 0.0001) were independent risk factors for ba-PWV.
Association of ba-PWV with glycemic control
To investigate the correlation between arterial stiffness (ba-PWV) and glycemic control (HbA1c), we divided subjects with diabetes and hypertension into 3 subgroups based on the level of HbA1c (HbA1c < 6.5%, 6.5% ≤ HbA1c < 7.0%, and HbA1c ≥ 7.0%). As shown in Fig. 2a, ba-PWV was significantly higher in subjects with HbA1c ≥ 7.0% that those with HbA1c < 6.5% (1851 ± 335 vs. 1715 ± 314 cm/s, P < 0.0001), suggesting that arterial stiffness was associated with glycemic control. In contrast, in diabetic subjects without hypertension, we did not observe the association between ba-PWV and HbA1c (1568 ± 307 vs. 1553 ± 279 vs. 1601 ± 331 cm/s, P = 0.31) (Fig. 2b).
Association of ba-PWV with duration of diabetes
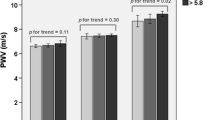
Brachial-ankle pulse wave velocity was positively associated with duration of diabetes in both 562 diabetic subjects with hypertension and 438 diabetic subjects without hypertension (P < 0.0001 and P = 0.0013). To find the cut-off point for duration of diabetes for ba-PWV, we divided the two groups of subjects into subgroups in terms of duration of diabetes (<5 year, 5–10 year, and ≥10 year). As shown in Fig. 3a, in subjects with diabetes and hypertension, ba-PWV of subjects with a duration of diabetes 5–10 years was significantly higher than that in those with a duration <5 years 1791 ± 313 vs. 1671 ± 342 cm/s, P = 0.0008). The ba-PWV of subjects with a duration >10 years was the highest among the three subgroups (Fig. 3a).
On the contrary, in subjects with diabetes but no hypertension, we did not observe a significant difference of ba-PWV between subjects with a duration of <5 years and of 5–10 years (1527 ± 286 vs. 1590 ± 331 cm/s, P = 0.077) nor a difference of ba-PWV between subjects with a duration of 5–10 years and of >10 years (1590 ± 331 vs. 1642 ± 318 cm/s, P = 0.18) (Fig. 3b). A significant difference of ba-PWV was shown in subjects with a duration of <5 years and of >10 years (1527 ± 286 vs. 1642 ± 318 cm/s, P = 0.0013), suggesting that 10 years may be the cut-off point of duration of diabetes for ba-PWV in diabetic subjects without hypertension.
Effect of duration of diabetes on the PWV in different HbA1c levels
The effect of duration of diabetes on the PWV in different HbA1c levels was compared (Fig. 4). PWV in hypertensive subjects was gradually increased according to duration of diabetes when HbA1c ≥ 7.0% (1680 ± 334 vs. 1865 ± 299 and 1897 ± 338 cm/s, P = 0.0062 and P = 0.0004, respectively) and was not different among those with 6.5% ≤ HbA1c < 7.0% and HbA1c < 6.5% (P > 0.05) (Fig. 4a).When HbA1c was more than 7.0%, the PWV in non-hypertensive subjects with duration of diabetes ≥10 years was significantly higher than those with duration of diabetes <5 years (1692 ± 354 vs. 1503 ± 272 cm/s, P = 0.0018). The difference persisted after adjusted for age (P < 0.05). However, when HbA1c was between 6.5–7.0%, the difference of PWV did not reach statistical significance among the three groups with different duration of diabetes (1441 ± 253 vs. 1571 ± 261 vs. 1625 ± 312 cm/s, P > 0.05) (Fig. 4b). Similarly,no significant difference was detected among the three groups when HbA1c was <6.5% (P > 0.05).
Discussion
Hyperglycemia in diabetes stimulates the formation of advanced glycation end products (AGEs). The AGE cross-links within the vascular wall further exacerbate vascular stiffness and large artery atherosclerosis [6–8]. PWV had been shown as an early and convenient index to measure the degree of arterial stiffness [4]. However, few studies have evaluated the value of PWV in diabetic patients with hypertension. In the present study, we observed that ba-PWV was positively associated with HbA1c as well as duration of diabetes in diabetic subjects with or without hypertension. We found that ba-PWV in diabetic and hypertensive patients with HbA1c < 6.5% was significantly lower than those with HbA1c ≥ 7.0%, suggesting that HbA1c ≥ 7.0% was the cut-off point and the importance of glycemic control in the prevention of arterial stiffness. The above finding was consistent with considerable clinical studies [9–14]. Besides HbA1c level, duration of diabetes is the other independent risk factor for vascular deficiency. Our study showed that ba-PWV increased with duration of diabetes in diabetic subjects with or without hypertension, suggesting that arterial stiffness was gradually worsened with a longer of duration of diabetes.
Previous studies have demonstrated that PWV was higher in patients with hypertension than those without hypertension. It is resulted from structural damage of the vessel wall by hypertension-augmented vascular tension [15–18]. Our present study observed that subjects with both diabetes and hypertension had higher arterial stiffness (ba-PWV) than those with diabetes but no hypertension. We also showed that cut-off point for duration of diabetes for arterial stiffness in subjects with diabetes but no hypertension was 10 years. However, the cut-off point for duration of diabetes for arterial stiffness was lowered to 5 years in subjects with hypertension and diabetes, suggesting that hypertension was an additive risk factor for arterial stiffness in diabetic subjects. It causes earlier and faster development of arthrosclerosis.
There are several limitations in our study. The inclusion of patients with pre-existing vascular disease and the coexistence of treatment for diabetes and hyperlipidemia may have affected the results. In addition, the present study was a cross-sectional study with limitation in the identification of causal factors of arterial stiffness.
In conclusion, arterial stiffness (ba-PWV) was more severe in diabetic subjects with hypertension than those without hypertension. Arterial stiffness was positively associated with HbA1c and duration of diabetes in subjects with diabetes and hypertension. These results suggest that early glycemic control is important in the prevention of development of vascular stiffness even in hypertensive diabetic subjects.
References
M.S. Kochkina, D.A. Zateishchikov, B.A. Sidorenko, Measurement of arterial stiffness and its clinical value. Kardiologiia 45, 63–71 (2005)
C.D.A. Stehouwer, R.M.A. Henry, I. Ferreira, Arterial stiffness in diabetes and the metabolic syndrome: a pathway to cardiovascular disease. Diabetologia 51, 527–539 (2008)
S. Laurent, P. Boutouyrie, R. Asmar, I. Gautier, B. Laloux, L. Guize, P. Ducimetiere, A. Benetos, Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 37, 1236–1241 (2001)
A. Yamashina, H. Tomiyama, T. Aria, Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens. Res. 26, 615–622 (2003)
J. Tayama, M. Munakata, K. Yoshinaga, T. Toyota, Higher plasma homocysteine concentration is associated with more advanced systemic arterial stiffness and greater blood pressure response to stress in hypertensive patients. Hypertens. Res. 29, 403–409 (2006)
P.V. Vaitkevicius, M. Lane, H. Spurgeon, D.K. Ingram, G.S. Roth, J.J. Egan, S. Vasan, D.R. Wagle, P. Ulrich, M. Brines, J.P. Wuerth, A. Cerani, E.G. Lakatta, A cross-link breaker has sustained effects on arterial and ventricular properties in older rhesus monkeys. Proc. Natl. Acad. Sci. USA 98, 1171–1175 (2001)
K. Shiina, H. Tomiyama, Y. Takata, Y. Usui, K. Asano, Y. Hirayama, T. Nakamura, A. Yamashina, Concurrent presence of metabolic syndrome in obstructive sleep apnea syndrome exacerbates the cardiovascular risk: a sleep clinic cohort study. Hypertens. Res. 29, 433–441 (2006)
Y. Naka, L.G. Bucciarelli, T. Wendt, L.K. Lee, L.L. Rong, R. Ramasamy, S.F. Yan, A.M. Schmidt, RAGE axis: animal models and novel insights into the vascular complications of diabetes. Arterioscler. Thromb. Vasc. Biol. 24, 1342–1349 (2004)
R.C. Turner, The U.K. prospective diabetes study. A review. Diabetes care 21(Suppl 3), C35–C38 (1998)
UK Prospective Diabetes Study (UKPDS) Group, Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352(9131), 837–853 (1998). Erratum in: Lancet 354(9178), 602 (1999)
Epidemiology of Diabetes Interventions and Complications (EDIC) Research Group, Effect of intensive diabetes treatment on carotid artery wall thickness in the epidemiology of diabetes interventions and complications. Diabetes 48(2), 383–390 (1999)
T. Mazzone, Strategies in ongoing clinical trials to reduce cardiovascular disease in patients with diabetes mellitus and insulin resistance. Am. J. Cardiol. 93(11A), 27C–31C (2004)
S.H. Kim, S.J. Lee, E.S. Kang, S. Kang, K.Y. Hur, H.J. Lee, C.W. Ahn, B.S. Cha, J.S. Yoo, H.C. Lee, Effects of lifestyle modification on metabolic parameters and carotid intima-media thickness in patients with type 2 diabetes mellitus. Metabolism 55, 1053–1059 (2006)
H. Yokoyama, N. Katakami, Y. Yamasaki, Recent advances of intervention to inhibit progression of carotid intima-media thickness in patients with type 2 diabetes mellitus. Stroke 37, 2420–2427 (2006)
B. Li, H. Gao, X. Li, X. Li, Y. Liu, M. Wang, Correlation between brachial-ankle pulse wave velocity and arterial compliance and cardiovascular risk factors in elderly patients with arteriosclerosis. Hypertens. Res. 29, 309–314 (2006)
H. Sasamura, Y. Kitamura, M. Nakamura, M. Ryuzaki, T. Saruta, Effects of the angiotensin receptor blocker candesartan on arterial stiffness and markers of extracellular matrix metabolism in patients with essential hypertension. Clin. Exp. Hypertens. 28, 511–520 (2006)
J. Ishikawa, K. Kario, Y. Matsui, K. Eguchi, M. Morinari, R. Kaneda, S. Hoshide, K. Eguchi, Y. Hojo, K. Shimada, Collagen metabolism in extracellular matrix may be involved in arterial stiffness in older hypertensive patients with left ventricular hypertrophy. Hypertens. Res. 28, 995–1001 (2005)
B. Athanase, A. Chris, M.B. Jeanne, T. Mohamed, L. Carlos, B. Kathryn, T. Frédérique, P. Bruno, A. Roland, Z. Mahmoud, S. Michel, G. Louis, Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circulation 105, 1202–1207 (2002)
Acknowledgments
We are indebted to all the patients and their family members who participated in this study. This study was partially supported by a grant from Shanghai Pujiang Program; a grant from PhD Program Foundation of Shanghai Jiaotong University School of Medicine and a grant from the Science Foundation of Shanghai health bureau (No. 2007121).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Yuhong Chen and Yun Huang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Chen, Y., Huang, Y., Li, X. et al. Association of arterial stiffness with HbA1c in 1,000 type 2 diabetic patients with or without hypertension. Endocr 36, 262–267 (2009). https://doi.org/10.1007/s12020-009-9221-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-009-9221-z