Abstract
The bone changes in hypothyroidism are characterized by a low bone turnover with a reduced osteoid apposition and bone mineralization rate, and a decreased osteoclastic resorption in cortical bone. These changes could affect the mechanical performance of bone. The evaluation of such changes was the object of the present investigation. Hypothyroidism was induced in female rats aged 21 days through administration of propylthiouracil in the drinking water for 70 days (HT group). Controls were untreated rats (C group). Right femur mechanical properties were tested in 3-point bending. Structural (load bearing capacity and stiffness), geometric (cross-sectional area and moment of inertia) and material (modulus of elasticity) properties were evaluated. The left femur was ashed for calcium content determination. Plasma T4 concentration was significantly decreased in HT rats. Body and femur weight and length in HT rats were also reduced. Femoral calcium concentration in ash was higher in HT than in C rats. However, the femoral calcium mass was significantly lower in HT than in C rats because of the reduced femoral size seen in the former. The stiffness of bone material was higher in HT than in C rats, while the bone geometric properties were significantly lower. The “load capacity” was between 30 and 50% reduced in the HT group, although, the differences disappeared when the values were normalized per 100-g body weight. The lowered biomechanical ability observed in the femoral shafts of HT rats seems to be the expression of a diminished rate of growth. Qualitative alterations in the intrinsic mechanical properties of bone tissue were observed in HT rats, probably because the mineral content and the modulus of elasticity were positively affected. The cortical bone of the HT rat thus appears as a bone with a higher than normal strength and stiffness relative to body weight, probably due to improvement of bone material quality due to an increased matrix calcification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During evolution, the skeleton of vertebrates developed an important property, the resistance to deformation, and indirectly to fracture, that was adapted to the physiological mechanical demands of the environment. The criterion for adequate support function is the formation and maintenance of sufficient quantity and quality of bone to support the body throughout life and to withstand ordinary stresses to which skeletal components are subjected.
It is assumed that the mechanical properties of bones integrated as organs (structural properties, e.g., load bearing capacity and stiffness) are directly related to both the amount (bone mass) and the architectural disposition of bone material (geometric properties, e.g., cross-sectional area, moment of inertia and cortical thickness) and to the mechanical quality of bone material (material properties, e.g., capacity to stand stress and modulus of elasticity). The structural stiffness (measurable as a load/deformation ratio) is usually kept high enough to withstand to everyday bone and bone tissue deformation to avoid damage, and hence fracture. The structural stiffness, and indirectly the strength of bones, is thought to be controlled by the “bone mechanostast” [1]. This is a feedback mechanism, which optimizes the bone’s design through a permanent re-distribution of the mineralized tissue. Bone shape accounts significantly for the whole bone strength regardless of bone calcification or mass.
Thyroid hormone (TH) has been recognized to play an important physiological role in skeletal development, linear growth and the maintenance of body mass [2]. The relation between TH and bone was first recognized in the 1890s, when von Recklinghausen [3] reported on a patient with hyperthyroidism and multiple fractures. Hyperthyroidism accelerates bone turnover [4] and shortens the normal bone remodelling cycle [5]. TH seems to be more detrimental to cortical bone than to trabecular bone [6].
In juvenile hypothyroid rats, growth plates are grossly disorganized, with defective hypertrophic chondrocyte differentiation, extracellular matrix production and angiogenesis [7]. In previously performed tomographic studies (pQCT) on rats, we found that experimental hypothyroidism resulted in a reduced bone mass and moment of inertia of the femoral diaphysis and a concomitant improvement of the material properties of cortical bone [8]. Recent studies performed on genetically modified mice demonstrated that TRα1+/mβ+/− adult mice, which express a mutant T3 receptor (TRα1) with dominant-negative properties due to reduced ligand-binding affinity, had osteosclerosis with increased bone mineralization even though juveniles had delayed ossification [9].
These and many other reported studies (for review see [2, 7, 10, 11]) indicate that TH regulates both skeletal development and adult bone maintenance, with euthyroid status during development being essential to establish normal adult bone structure and mineralization.
We have recently shown that [12], although, the femur size of the hypophysectomized rat does not enlarge with age, its weight and its calcium mass (femur bone mass) increase significantly. From the biomechanical point of view, the bone markedly increases its intrinsic and extrinsic stiffness. These findings are probably associated to the lack of pituitary hormones during growth and development. The present study was designed to estimate the effects of experimental hypothyroidism on biometric and biomechanics parameters, as assessed by a mechanical bending test, in an attempt to describe the biomechanical properties of the hypothyroid bone and to get insights into the possible contribution of secondary hypothyroidism on the genesis of the biomechanical bone effects of hypophysectomy.
Materials and methods
Female Sprague–Dawley rats aged 21 days were used throughout the experiments. They were housed in stainless-steel cages and maintained under local vivarium conditions (temperature 22–23°C, 12-h on/off light cycle). All animals were allowed free access to a standard pelleted chow diet that has been shown to meet all necessary requirements to allow normal growth rates [13].
Experiment 1: changes with time after weaning of femur diaphysis strength
By considering that (a) hypothyroidism in the rat diminishes body weight gain, and (b) a positive correlation exists between body weight and bone strength, a first experiment was set up in which groups of four normal rats were sacrificed at 55, 65, 75, 90, 120, 150 and 180 days of life. At each of these times, both body weight and femur diaphyseal strength (see below) were determined on each rat. The correlation between the parameters was estimated. This type of information would permit us the comparison of weight-associated bone mechanical parameters between animals of different weights.
Experiment 2: effect of hypothyroidism on biomechanical performance of femoral shaft
In the second experiment, rats were divided in two equal groups of 10 animals each: control (C) and hypothyroid (HT). They were grouped to ensure similar masses (C = 73.4 ± 6.5 g, HT = 70.2 ± 6.8 g; P > 0.05). Hypothyroidism was induced in HT rats through administration of propylthiouracil (PTU) in the drinking water (0.1% in 5% ammonia). Thus, drinking water containing 5% ammonia was freely offered to both C and HT rats. The experimental period lasted 70 days. Thus, experimental data were collected during adulthood.
At its end, animals were weighed and samples of blood were taken by cardiac puncture for estimation of plasma-free T4 concentration (Electrochemiluminescence immunoassay, Elecsys 2010, Roche). They were then sacrificed by ether overdose. Body length was taken as the distance between nose and rump. The femurs were dissected, cleaned of adhering soft tissue, weighed in a Mettler scale and stored at −20°C wrapped in gauze soaked with Ringer’s solution in sealed plastic bags, in accordance with Turner and Burr [14].
On the day of testing, each bone was thawed at room temperature before analysis. Femur length was measured directly using a digital caliper (Digginess, Geneva, Switzerland) with an accuracy of ±0.01 mm. To assess cortical bone mechanical properties, the right femur was tested in 3-point bending [15]. Each bone was placed with the posterior side on two lowers supports (L = 13-mm span) and central along its length. Load was applied perpendicularly to the long axis of the bone until fracture. The test machine (Instron model 4442, Instron Corp., Canton, MA, USA) was operated in stroke control at a constant rate of 5 mm/min, which is useful for describing the static properties of the bone structure.
Mechanical parameters are briefly defined as follows [16]: Deformation is the amount of deflection of the bone as a result of loading. The second moment of inertia (or amount of inertia) describes the distribution of the bone mass around the central axis, i.e., the geometry of the cross-sectional section. Stress is an expression of force per unit area of bone (i.e., tissue strength). The calculation of stress would take into account the geometric configuration of the cross-sectional area over which the force was applied (the distance between the supports). Stress is a material property rather than a structural property, being dependent of bone tissue composition. Strain refers to the deformation created by bending the bone and was reported as change in length per unit length. Modulus of elasticity is derived from the linear portion of the stress–strain curve and is an expression of force per unit area per unit of bending. This parameter was used as indicator of bone material stiffness.
Load/deformation curves showing both the elastic (Hookean behaviour) and the plastic (non-Hookean behaviour) phases separated by the yielding point, enabled graphic determination of the main structural mechanical properties of bone shafts as beams [14], which essentially measures the resistance to deformation (stiffness) and fracture (strength) and the ability of the structure to absorb energy by deforming. They are (a) Bone stiffness (N/mm)—the slope of the force/displacement curve (W/d curve) in the linear region of elastic behaviour that was calculated from the best-fit linear regression; it is generally proportional to diaphyseal bone stiffnessor bone beams rigidity; (b) elastic limit (load at the yielding point, Wy) (N)—the value of the force at the upper extent of the linear region (yielding point); (c) Ultimate load (load at fracture, Wf) (N)—the value of the force at fracture, which determines the structural bone strength; it expresses directly the resistance of the whole bone to fracture, incorporating both the elastic and the plastic behaviours; and (d) Elastic absorbing capacity (EAC) (N/mm)—the total energy absorbed by the specimen up to the yielding point that was calculated as the area under the force/displacement curve (Wy dy/2).
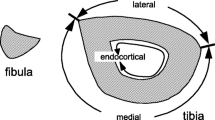
A representative indicator of bone material properties, the intrinsic bending stiffness of the cortical tissue (Elastic modulus [N/mm2]) was calculated from the following equation: E = W y · L 3 /48d y · I x (W y = load at the yielding point, L = distance between supports, d y = maximum elastic deflection, I x = second moment of inertia of the cross-section in relation to the horizontal axis). Using an Isomet low-speed diamond saw (Buehler, Lake Bluff, IL), a 2-mm cross-section slide was cut from the fracture section to perform regularized micromorphometrical determinations of the vertical (load direction) and horizontal (right angle to load direction) outer and inner diameters of the elliptic-shaped fracture sections. Measurements were taken with a digital caliper with the aid of a magnifier 40×. This procedure enabled calculation of the amount of diaphyseal bone mass (CSA) and the second moment of inertia of the cross-section in relation to the horizontal axis (xCSMI) (3.14[B 3 H − b 3 h]/64) (B = vertical outer diameter, H = horizontal outer diameter, b = vertical inner diameter, h = horizontal inner diameter) [17]. The volume of bone between supports (Lπ (HB − hb), the entire cross-sectional area (CSA) (π/4 BH), the medullary area (MA) (π/4 bh) and the cortical area (CtA) (CSA − CtA) were also calculated.
The left femur of each animal was ashed in a muffle furnace at 600°C for 18 h and the ash weight obtained. The bone ash was dissolved in 2-N HCl and calcium content determined by atomic energy absorption spectrophotometry [18]. In this study, femoral bone mass, or femoral calcium mass, refers to the milligram of calcium present in the ash of the left femur.
Results were summarized as means ± SD and were considered statistically significant at the level of P < 0.05. Comparisons between parameters were performed by Student’s t test. The curve that relates bone strength with age was fitted by nonlinear regression by applying the Boltzmann sigmoidal equation [Y = Bottom + (Top − Bottom)/(1 + exp (V50 − X)/Slope)]. The relationship between bone strength and body weight was analysed by linear regression. All analyses were performed by using GraphPad Prism Software (GraphPad Software Inc., San Diego, CA, USA).
The experiment was conducted in accordance with the principles and procedures outlined in the National Institute of Health Guide for the Care and Management of Laboratory Animals, and approved by the University of Buenos Aires Ethic Committee.
Results
Experiment 1
Analysis of the macroscopical growth of the femur in normal female rats indicates that the bone grew in a linear fashion from day 21 to approximately day 90 of postnatal life (data not shown). After day 90, the rate of growth showed a marked decline or deceleration. One-way analysis of variance indicated that no statistical significant differences were found between day 90 and day 120 values. A similar pattern of growth was observed in the femoral bone strength as derived from the ultimate load values (Fig. 1a). Extremely high positive correlation was found between femur diaphysis ultimate load (W f) and body weight (r = 0.9555, R 2 = 0.913, P < 0.0001) (Fig. 1b, triangles).
a Changes with age of ultimate load (Wf) of the femur diaphysis in normal rats, b correlation between ultimate load (Wf) of bone shafts and body weight in normal and hypothyroid rats, c correlation between ultimate load (Wf) and stiffness (Wy/dy ratio) of bone shafts in control and hypothyroid rats, considered as a whole group, d correlation between ultimate load (Wf) and moment of inertia (xCSMI) of bone shafts in control and hypothyroid rats, considered as a whole group, e correlation between stiffness (Wy/dy ratio) and moment of inertia (xCSMI) of bone shafts in control and hypothyroid rats considered as a whole group, f correlation of calcium concentration in ash and the elastic modulus (E) in control and hypothyroid rats considered as a whole group
Experiment 2
In controls, the mean plasma T4 was 5.1 ± 0.8 μg/dl at the end of the study period. The mean plasma T4 was very low (0.9 ± 0.4 μg/dl) in HT rats at the same time (P < 0.001), thus confirming the effectiveness of treatment.
As expected, HT rats (128.72 ± 3.31 g) failed to obtain normal weight gain (P < 0.001) compared with the age-matched C rats (283.35 ± 4.22 g) at the end of the experimental period (Table 1). This 55% reduction in body weight found in HT animals was accompanied by a significant, 26% diminution of body length. Similarly, femur weight and femur length were 50 and 23% reduced, respectively, in HT rats when compared to C ones (P < 0.001). Femoral calcium concentration in ash was higher in HT than in C rats (C = 364.5 ± 4.5 mg/g, HT = 384.2 ± 6.9 mg/g, P = 0.0002). However, the femoral bone mass (calcium mass) was significantly lower (P < 0.0001) in HT (59.2 ± 4.4 mg) than in C (118.7 ± 8.2 mg). When the femoral bone mass was normalized for 100-g femur, it was higher in HT (38.4 ± 0.69 g/100 g) than in C (36.5 ± 0.45 g/100 g) (P = 0.0002).
Changes in cross-sectional geometry of the femur diaphysis are summarized in Table 1. Cortical bone circumferential growth was reduced significantly in HT rats. The femur mid-diaphyseal total cross-sectional area and the medullary area were significantly less in the HT group compared with the control one. Absolute regional diameters (horizontal and vertical, inner and outer) were similarly affected. The cross-sectional moment of inertia was thus extremely reduced.
The “load capacity” extrinsic properties of the femoral diaphysis are also shown in Table 1. All of them were between 30 and 50% reduced in the HT group (P < 0.0001). However, when the values for ultimate load at fracture (W f) and stiffness were expressed in terms of 100-g body weight, the differences between groups disappeared. This concept is graphically shown in Fig. 1b. In the plot of femoral W f as a function of the body weight of the animals, those values corresponding to HT rats laid on the curve established for rats of different ages and body weights obtained in the Experiment 1. Figure 1a also shows that the fracture load of HT rats aged 90 days correspond to that of normal rats aged 50 days.
The bone material quality indicators, or pre-yield bending stiffness (elastic modulus E) is also shown in Table 1. They were about 70% higher in HT than in C rats (P < 0.05).
Discussion
The results of this study provide details on how hypothyroidism affects the mechanical properties of bones in young rats, as derived from determinations performed in early adulthood. Healthy bones in the adult are dependent on the development, during the younger years, of a healthy bone structure and an adequate bone mass. This is especially true for cortical bone whose primary function is strength and support. The femoral mid-diaphysis in the rat is primarily composed by cortical bone. The bone used in the present experiment seems thus appropriate to evaluate the real effect of hypothyroidism on cortical bone biomechanics.
The present study began with very young animals and the effects of treatment on bone biomechanics were assessed in adulthood. The extremely significant decrease in circulating T4 observed in experimental rats in relation to control ones demonstrates that treatment was efficient in the induction of hypothyroidism.
As expected, hypothyroidism caused marked growth retardation in immature rats, as derived from changes in both body weight and body length. Growth retardation associated with hypothyroidism has been previously reported [19, 20]. Hypothyroidism in rats causes longitudinal skeletal growth retardation due to growth plate dysgenesis in which hypertrophic chondrocyte differentiation fails to progress. There are gross abnormalities of growth plate structure with disorganized proliferating chondrocyte columns, abnormal cartilage matrix, reduced hypertrophic chondrocyte differentiation and impaired vascular invasion at the primary spongiosum [21, 22]. While the majority of these effects probably result directly from TH deficiency in TR-expressing chondrocytes, the hypothyroid growth plate is also relatively insensitive to the actions of growth hormone because of reduced local expression of IGF-1 [21]. Nevertheless, studies of T3 and GH interactions of the tibial growth plate in vivo showed that T3 is independently essential for the stimulation of resting zone cells to differentiate to proliferating chondrocytes, for hypertrophic chondrocyte differentiation, and for vascular invasion of the growth plate [22]. It was also reported that [23] growth plate dysgenesis is associated with altered expression of components of the Ihh-PTHrP feedback loop in hypothyroid growth plates. These findings reinforce the general importance of TH as a systemic factor that is required for endochondral ossification. However, it has to state that a major limitation in this type of studies is that in the rat hypothyroidism is well known to cause a profound reduction in pituitary GH production that is associated with major decreased in circulating GH and IGF-1 levels and growth retardation. Hypothyroidism is also associated with derangement of a multitude of other metabolic and physiological processes.
Both the weight and the length of the femur were undoubtedly affected by growth retardation, as was the bone volume. The diminished CSA and xCSMI indicate that the size of the bone, in term of mid-diaphysis cross-sections, was significantly affected.
These alterations were paralleled by a weakening of bone beams, shown by the correlative impairment of diaphyseal ultimate strength (W f) and stiffness (W y/d y ratio) (Fig. 1c). The other extrinsic mechanical properties were also adversely affected in HT rats. The body weight of animals is one of the most important factors which influence mechanical stresses applied to bone. A positive linear correlation between the load at fracture of the femur and the body weight of animals was established (Fig. 1b). Therefore, it appears that cortical bone tissues of the HT rats changed the load at fracture so as to adapt themselves to the decrease of the in vivo load developed by diminished rate of body weight gain. When the load at fracture, as well as the other parameters indicative of femoral extrinsic mechanical properties, was normalized for body weight, the differences between groups disappeared and the corresponding values were even higher in HT than in C rats, which support that hypothesis. This hypothesis could be expressed in other words by saying that HT rats had smaller bones due to growth retardation and their load at fracture was not different than that of similarly sized control rats (Fig. 1b). Under this concept, no adaptation appears to be evident; HT rats just did not grow. Hypothyroidism possibly had also an effect on the ways in which the whole bone load capacity increased over the time course of the study. This is graphically shown in Fig. 1a. Average W f value in 90-day-old HT rats was similar to the value found in normal rats aged 50 days.
The above results enable the discussion of whether the impaired performance of diaphyseal shafts of HT rats was the result of nothing other than the changes in the amount and/or spatial distribution of cortical bone mass or if some other variation in bone material ability was an additional causal factor.
The first of these propositions is supported by the high positive correlation found between both strength and stiffness of bone beams and their sectional moments of inertia in C and HT groups, about 60% of the variation in W f and 62% of that of W y/d y ratio may be statistically attributed to xCSMI changes, as shown by R 2 in Fig. 1d and E. However, the severe impairment in W f (a property closely related to the amount and/or spatial distribution of material in the diaphysis) contrasted with the increasing effect of HT on the modulus of elasticity E (intensive property of bone material, which depends on its constitution but not on its amount or spatial distribution), suggesting that the adverse effects evoked by treatment on diaphyseal bone load capacity may have been only quantitative in nature. The finding that the adverse effect of hypothyroidism disappears when parameters indicative of bone extrinsic mechanical properties are normalized for body mass, gives support to this concept. The natural stimuli for the bone mechanostat would be the strain of bone tissue, sensed by osteocytes that are induced by both gravitational forces and contractions of regional muscles [17]. Therefore, on a wearing-weight bone as the femur, different body weights will produce different loads and strains.
The significant increase in E in the presence of a significant reduction in both the amount and the spatial distribution of cortical bone mass indicates that bone strength is higher in HT rats than it should be expected by the reduced bone mass. Material properties are usually thought to depend on many factors, such as composition, amount of secondary mineralization, collagen cross-linking and the presence of microdamage. Because mineral composition, particle size and distribution are not always the same, the properties of the crystals should also be considered as one of the factors contributing to material properties, when discussing the ability of bone to resist fracture [24]. The femoral shaft of the hypophysectomized rat is characterized by its high mineral density and its unusual large modulus of elasticity in spite of cessation of linear growth [12]. Both collagen maturation and cross-linking and the degree of mineralization of bone have been found to be increased in the hypophysectomized rat femur [25].
The effect of hypothyroidism on E, not described elsewhere, although, seen in preliminary observations from our laboratory [8], was paralleled by an increment in bone calcium content, as expressed in mg Ca/g ash (Fig. 1f). The positive correlation between bone Ca concentration and E suggests a causal connection between treatment and rigidity of bone tissue. In fact, calcification of collagen matrix is a high-priority determinant of bone tissue intrinsic stiffness [26, 27].
The bone changes in hypothyroidism are characterized by a very low bone turnover with a reduced osteoid apposition and bone mineralization rate, an inactive osteoclastic resorption in trabecular bone and a decreased osteoclastic resorption in cortical bone [28]. In hypothyroid female patients, Eriksen et al. [29] have shown that the final resorption depth, the total resorption period and the resorption rate were lower than in the control group. The total bone formation period was prolonged and the matrix and mineral appositional rates were lowered. Interestingly, the mean completed wall thickness was increased in the hypothyroid group, which is evidence of a positive balance per remodelling cycle. It is thus conceivable that the very low bone turnover associated to a lowered remodelatory rate may be responsible for the increased matrix mineralization in the cortical bone of HT rats, as evidenced by the higher calcium concentration in ash found in the present study. It has been shown that the degree of mineralization of older bone tissue is greater than that of newly formed tissue, so that the amount of bone turnover can influence the average tissue degree of mineralization [30]. Our results agree with the finding of an increased bone mineralization in TRα1+/mβ+/− mice recently reported by Duncan Basset et al. [7].
In conclusion, we have described a number of alterations in both morphometrical and biomechanical variables in rat femur shafts resulting from PTU-induced hypothyroidism. The clear loss of strength and stiffness of bone beams seemed to be closely related to a net impairment in the amount and/or spatial distribution of bone mass. However, because strength and stiffness are positively correlated to body weight, on the one hand, and HT rats showed an important deficit in body weight gain, on the other hand, it is suggested that the lowered biomechanical ability observed in the femoral shafts of HT rats was the expression of a diminished rate of growth. When the parameters were normalized for body weight, the differences between HT and C rats disappeared and the corresponding values were even higher in the former than in the latter. Qualitative alterations in the intrinsic mechanical properties of bone tissue were induced by treatment, as the mineral content and the modulus of elasticity were positively affected. It is conceivable that these effects are associated with the already described very low bone remodelatory rate and the positive balance per remodelling cycle. The cortical bone of the HT rat thus appears as a bone with a higher than normal strength and stiffness relative to body weight, probably due to improvement of bone material quality. Similar conclusions have been arrived for cortical bone of hypophysectomized rats [12], which suggest that hypothyroidism and hypopituitarism may affect bone biomechanics through a common operative mechanism which is associated to growth retardation.
References
H.M. Frost, Anat. Rec. 219, 1–9 (1966)
C.B. Harvey, P.J. O’Shea, A.J. Scott, H. Robson, T. Siebler, S.M. Shalet, J. Samarut, O. Chassande, G.R. Williams, Mol. Gen. Metab. 75, 17–30 (2002)
F.C. von Recklinghausen, in: Festschrift Rudolpf Virchow, ed. by G. Reimer (Berlin, 1891), pp. 1–89
M. Mosekilde, E.F. Eriksen, P. Charles, Endocrinol. Metab. Clin. North Am. 19, 35–63 (1990)
E.F. Eriksen, Endocr. Rev. 7, 379–408 (1986)
D.S. Ross, Thyroid 4, 319–326 (1994)
J.H. Duncan Bassett, G.R. Williams, Trends Endocrinol. Metab. 14, 356–364 (2003)
C. Bozzini, M.I. Olivera, M. Meta, R. Capozza, C.E. Bozzini, J.L. Ferretti, R.M. Alippi, J. Dent. Res. A 76, 926 (1997)
J.H. Duncan Bassett, K. Nordström, A. Boyde, P.G.T. Howell, S. Kelly, B. Vennström, G.R. Williams, Mol. Endocrinol. 21, 1893–1904 (2007)
G.R. Williams, H. Robson, S.M. Shalet, J. Endocrinol. 157, 391–403 (1998)
E. Murphy, G.R. Williams, Clin. Endocrinol. 61, 265–298 (2004)
R.M. Alippi, M.I. Olivera, C. Bozzini, P.A. Huygens, C.E. Bozzini, Comp. Clin. Pathol. 14, 76–80 (2005)
C. Bozzini, A.C. Barcelo, R.M. Alippi, T.L. Leal, C.E. Bozzini, J. Dent. Res. 68, 840–842 (1989)
C.H. Turner, D.B. Burr, Bone 14, 595–608 (1993)
H.A. Hogan, J.A. Groves, H.W. Sampson, Alcohol. Clin. Exp. Res. 23, 1825–1833 (1999)
G.M. Kiebzak, R. Smith, C.C. Gundberg, J.C. Howe, B. Sacktor, J. Bone Miner. Res. 3, 37–45 (1988)
J.L. Ferretti, R.D. Tessaro, E.O. Audicio, Calcif. Tissue Int. 37, 608–612 (1985)
E.L. Barengolts, H.F. Gajardo, T.I. Rosol, J.J. D’Anza, M. Pena, J. Botsis, S.C. Kukreja, J. Bone Miner. Res. 11, 1143–1147 (1990)
P.J. Burstein, B. Draznin, C.J. Johnson, D.S. Schalch, Endocrinology 104, 1107–1111 (1974)
S.A. Rivkees, H.H. Bode, J.D. Crawford, N. Engl. J. Med. 318, 599–602 (1988)
D. Lewinson, G.M. Bialik, Z. Hochberg, Endocrinology 135, 1504–1510 (1994)
D. Lewinson, Z. Harel, P. Shenzed, M. Silbermann, Z. Hochberg, Endocrinology 124, p37–p945 (1989)
D.A. Stevens, R.P. Hasserjian, H. Robson, T. Siebler, S.M. Shalet, G.R. Williams, J. Bone Miner. Res. 15, 2431–2442 (2000)
A.L. Boskey, E.R. Myers, BoneKEy Osteovision 1, 4–7 (2004)
D.A. Martinez, A.C. Vailas, R.E. Grindeland, Am. J. Physiol. 260, E690–E694 (1991)
R. Amprino, Acta Anat. (Basel) 34, 161–186 (1958)
R.J. Minns, A. Atkinson, F.S. Steven, J. Bone Joint Surg. (Br) 64, 382 (1982)
L. Mosekilde, F. Melsen, Acta Pathol. Microbiol. Scand. 86, 56–62 (1978)
E.F. Eriksen, L. Mosekilde, F. Melsen, Bone 7, 101–108 (1986)
C.J. Hernandez, Bone 42, 1014–1020 (2008)
Acknowledgements
This investigation was supported by Research Grants from both University of Buenos Aires (UBACYT O-002, UBACYT O-005) and CONICET (PIP 5501).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Conti, M.I., Martínez, M.P., Olivera, M.I. et al. Biomechanical performance of diaphyseal shafts and bone tissue of femurs from hypothyroid rats. Endocr 36, 291–298 (2009). https://doi.org/10.1007/s12020-009-9212-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-009-9212-0