Abstract
Brain plasticity provides a mechanism to compensate for lesions produced as a result of stroke. The present study aims to identify new transcription factors (TFs) following focal cerebral ischaemia in rat as potential therapeutic targets. A transient focal cerebral ischaemia model was used for TF-binding activity and TF–TF interaction profile analysis. A permanent focal cerebral ischaemia model was used for the transcript gene analysis and for the protein study. The identification of TF variants, mRNA analysis, and protein study was performed using conventional polymerase chain reaction (PCR), qPCR, and Western blot and immunofluorescence, respectively. Rat cortical neurons were transfected with small interfering RNA against the TF in order to study its role. The TF-binding analysis revealed a differential binding activity of the octamer family in ischaemic brain in comparison with the control brain samples both in acute and late phases. In this study, we focused on Oct-2 TF. Five of the six putative Oct-2 transcript variants are expressed in both control and ischaemic rat brain, showing a significant increase in the late phase of ischaemia. Oct-2 protein showed neuronal localisation both in control and ischaemic rat brain cortical slices. Functional studies revealed that Oct-2 interacts with TFs involved in important brain processes (neuronal and vascular development) and basic cellular functions and that Oct-2 knockdown promotes neuronal injury. The present study shows that Oct-2 expression and binding activity increase in the late phase of cerebral ischaemia and finds Oct-2 to be involved in reducing ischaemic-mediated neuronal injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischaemic stroke occurs when the blood supply to the brain is obstructed. Currently, tissue plasminogen activator (t-PA) is the only approved treatment for ischaemic stroke. Unfortunately, t-PA has a limited time window for therapeutic use, and only 3–5 % of stroke patients arriving at the hospital qualify for the treatment (Fisher et al. 2009). Thus, there is a strong need to identify new targets and understand the molecular mechanisms associated with ischaemic stroke so that other treatment approaches can be pursued.
It has previously been demonstrated that distinct patterns of gene expression are seen in tissues from rat and non-human primate ischaemic (MCAO) stroke models (Xu et al. 2005; Ford et al. 2006; Rodriguez-Mercado et al. 2012). Microarray analyses from previous studies have shown that many classes of genes are activated following ischaemia, but inflammation and cell death are primary gene categories that appear to be associated with ischaemic stroke model (Pulliam et al. 2013). Moreover, cerebral ischaemia also promotes the up-regulation of genes that aim to remodel cerebral connections and cause structural and functional changes in all affected structures, including genes involved in brain plasticity processes (Nadareishvili and Hallenbeck 2003; Chopp et al. 2007, 2008). In turn, all these genes can be regulated by transcription factors (TFs) that bind to regulatory elements in their promoters to induce or suppress gene expression (Pulliam et al. 2013). Some examples of these TFs are NF-κB, Hes, HIF-1, STAT3, AP-1, CREB, Sox2, Pax6, Tcf/Lef, Gli, Olig2, Dlx2, TLX, and Bmi-1, which have all been reported to induce neurogenesis following cerebral ischaemia (Zhang et al. 2011). In the case of HIF-1, this TF has also been found to trigger cell survival mechanisms (Singh et al. 2012) and CREB has been found to play a critical role in synaptic plasticity and neuronal survival after ischaemia (Kitagawa et al. 2012). Previous authors have highlighted the importance of studying TFs due to the role they play in preventing damage in cerebral ischaemia (Baranova et al. 2007; Li et al. 2013). These molecules do not act as unique and direct regulators of gene expression, but most TFs will dimerise or contribute to large multimetric structures involved in RNA transcription (Raivich 2011). Although these factors are involved in plasticity processes, they do not share a common temporal expression profile after cerebral ischaemia. However, it is interesting to note the particular biphasic expression profile of HIF-1 TF, which functions as a pro-apoptotic and as a tissue repair and pro-survival factor, in the acute phase (from 1 to 12 h) and late phase (from 2 to 8 days) of ischaemia, respectively (Baranova et al. 2007; Singh et al. 2012).
The analysis of transcriptional regulators can be useful to understand how large sets of genes can be controlled by a small set of upstream signalling molecules. Moreover, the knowledge of genes and their transcriptional regulators that participate in giving the brain the potential to compensate for ischaemic lesions (plasticity mechanisms) may provide novel substrates for brain repair and are essential in the development of optimal stroke therapeutic strategies (Zhang et al. 2012).
In the present study, with the aim of better understanding brain plasticity mechanisms and of identifying new activated TFs involved in cerebral ischaemic response, a multiplex assay was performed. This assay revealed important differences in the binding activity of the Octamer TF family.
Octamer-binding proteins (Oct) are a family of five cloned and characterised TFs (Oct-1, Oct-2, Oct-3/4, Oct-6, and Oct-11) that recognise the octamer motif (5′-ATGCAAAT-3′). All members belong to the Pit–Oct–Unc (POU) family of TFs, characterised to contain a POU domain (with a bipartite structure: specific and homeo-subdomain) that mediates the DNA binding of these factors, allowing them to modulate the activity of specific genes with a critical role in normal development (Kristie and Sharp 1990). In this family, we focused on Oct-2 TF, given the structural and functional complexity of the different transcript variants described (Wirth et al. 1991; Lillycrop and Latchman 1992; Annweiler et al. 1994). Oct-2 was initially identified in B lymphocytes (Singh et al. 1986; Staudt et al. 1988) but has been found to be widely expressed throughout the central nervous system during rat embryonic development. Its expression was restricted to the brain in adult rats (He et al. 1989). Specifically, the Oct-2 TF has been reported to be expressed in neuronal cells in the mammalian developing nervous system (He et al. 1989) and in rat and mouse neuronal cell lines (Kemp et al. 1990; Dent et al. 1991; Lillycrop and Latchman 1992; Lillycrop et al. 1994; Deans et al. 1995; Liu et al. 1995) in control conditions. Neuronal Oct-2 differs from Oct-2 in B cells with respect to both sequence specificity and gene activation ability (Dent et al. 1991). Oct-2 is comprised of an N-terminal transactivation domain, the characteristic bipartite DNA-binding domain (Latchman 1996a, b), and a C-terminal transactivation domain (CTD), indispensable for in vivo Oct-2 function (Corcoran et al. 2004).
The present study aimed to characterise the Oct-2 TF following focal cerebral ischaemia in rat by (1) searching for the predicted transcript variants of the selected TF and checking their expression in control and ischaemic rat brain, (2) quantifying their temporal pattern expression at mRNA and protein levels, (3) determining the TF cellular localisation in neurons in rat cortex, (4) investigating in which signalling pathways the TF is involved, and, finally, (5) testing whether or not the selected TF is involved in neuronal damage and toxicity.
Results
Ischaemia Modified the Octamer-Binding Activity
We performed an initial screening to identify newly activated TFs involved in cerebral ischaemic response with an overall beneficial role, as potential therapeutic targets. The specific TF-binding activity comparisons between each transient ischaemic brain sample (ipsilesional core, ipsilesional peri-infarct, and ipsilesional non-damaged tissue) and their respective contralesional tissue at the different times analysed are represented as MFI values in scatter plot graphs (Fig. 1). Each plot represents the binding activity of a single TF or a specific TF family. Of particular note in this study was the peculiar TF-binding activity profile of the octamer family. The multiplex analysis from contralesional and ipsilesional cortex tissue revealed an inhibition of over 70 % of octamer-binding activity after transient brain ischaemia in comparison with contralesional tissue brain samples in the acute phase (from 6 to 72 h of reperfusion) (Fig. 2a), with the least binding activity being recorded at 24 h of reperfusion (a fold induction of 0.23 in the ipsilesional non-damaged tissue in comparison with the contralesional tissue, Dev F = 9.81). At 7 and 14 days, the binding activity was greater (Fig. 2b), especially at 14 days when ipsilesional core and peri-infarct tissue samples showed much greater binding activity than in the contralateral tissue (a fold induction of 1.78 in the ipsilesional core versus the contralesional tissue, Dev F = 7.56). The specific fold induction values of the different ischaemic areas versus the corresponding contralesional tissue when octamer TF-binding activity differences were significant (changes >25 % and Dev F ≥2.0) are shown in Supplementary material (Table S1). These results showed a differential binding activity of the octamer TF family in the acute and late phases of ischaemia.
Multiplex analysis of 50 different TFs from contralesional and ipsilesional rat cortex tissue. Comparison of transcription factor binding activity in cortical ipsilesional core, peri-infarct, and non-damaged tissue samples at 6, 24, and 72 h, and 7 and 14 days of reperfusion versus contralesional tissue (CL). Binding activity is measured as medium fluorescence intensity (MFI). Octamer transcription factor binding activity is ringed in red (Color figure online)
Octamer transcription factor binding activity study in nuclear extracts from rat brain exposed to tMCAO performed with the Luminex assay. Analysis of the octamer-binding activity (measured in MFI, median fluorescent intensity) in different infarct areas in the acute (a) and chronic phase of cerebral ischaemia (b) compared with the corresponding contralateral tissue. CL Contralesional control, C core, P peri-infart, ND non-damaged. * indicates the reperfusion time when the binding activity differences are significant (changes >25 % and the Dev F ≥2.0), and the fold induction is ≤0.75; ** indicates the reperfusion time when the binding activity differences are significant, and the fold induction is ≥1.25. The specific MFI values are shown in supporting information (S1)
Octamer-2 Transcription Factor Transcripts are Expressed in Both Control and Ischaemic Rat Brain
In the octamer family, we focused on Octamer-2 (Oct-2) TF given the structural and functional complexity of the different transcript variants described (Wirth et al. 1991; Lillycrop and Latchman 1992; Annweiler et al. 1994). In addition, Oct-2 was the only protein among the different members of this family that was specifically expressed in the brain with an expression profile that varied post-ischaemia (data not shown). In order to characterise Oct-2 in brain ischaemia, we searched for the predicted transcript variants with the Ensembl programme and checked its real expression in control and ischaemic (pMCAO) brain using PCR and specific designed primers. Ensembl prediction revealed six candidate Oct-2 transcripts for Rattus norvegicus. Conventional PCRs performed with the specific primers showed that the Oct-2 transcripts described as ENSRNOT00000048002 (Pou2f2-201) (269 bp), ENSRNOT00000027649 (Pou2f2-202) (252 bp), ENSRNOT00000041651 (156 bp), ENSRNOT00000046678 (Pou2f2-203) (509 bp), and ENSRNOT00000068776 (107 bp) are all expressed in both permanent ischaemic and control rat brain (Fig. 3a). The transcript described as ENSRNOT00000027655 (337 bp) was not present in the control or ischaemic brain, as the only fragment obtained in this PCR was a band of 470 bp corresponding to the amplification of the rest of the Oct-2 variants.
Octamer-2 transcript analysis, gene expression, and protein study. Conventional PCR (a), quantitative real-time PCR (b), and Western blot (c: Oct-2 002 isoform, 60 kDa; d: Oct-2 678 isoform, 44 kDa) were used in control and permanent ischaemic brain samples at different times post-ischaemia. Ywhaz and Sdha were used as reference genes in quantitative real-time PCR. Results from Western blot were normalised with β-actin. Oct-2 transcript names are abbreviated with the last three numbers of the Ensembl code. Cntr Sham control, min minutes, h hours, d days, and pMCAO middle cerebral artery permanent occlusion. (* p < 0.05; ** p < 0.01; # p < 0.001)
Oct-2 mRNA Expression Increases in the Late Phase of Ischaemia
The different transcript variants identified by conventional PCR in control and ischaemic conditions were further analysed by qPCR in order to study their mRNA expression profile at different times post-ischaemia (Fig. 3b). We designed specific probes (TaqMan® assay) for the five Oct-2 transcripts identified in rat brain to detect each transcript by qPCR except for the ENSRNOT00000068776 variant, which could not be done due to its short sequence. The present study showed that ischaemia induces changes in Oct-2 mRNA expression profile. Oct-2 transcript analysis revealed that ENSRNOT00000048002 (Pou2f2-201) expression in pMCAO cortex is maintained at basal levels from 6 to 72 h post-pMCAO. Expression was more than twice that of the control at 7 days (p < 0.001) and diminished at 14 days while still maintaining a higher expression than the control. This transcript is the most predominant one in the analysed samples, showing the lowest CT values (27–28) in the qPCR experiments. ENSRNOT00000027649 (Pou2f2-202) expression remained lower than in the control during the acute phase of ischaemia (from 6 to 72 h post-pMCAO). At 7 days, the expression was significantly higher than in the control (p < 0.01), and it diminished slightly at 14 days while maintaining a higher level of expression than in the control. ENSRNOT00000041651 expression progressively diminished from 6 to 24 h post-ischaemia, increasing progressively at 72 h post-pMCAO and reaching the maximum expression at 7 days, when it was 60 % higher than the control (p < 0.05). Finally, the ENSRNOT00000046678 (Pou2f2-203) transcript profile was characterised by progressive increasing between 6 h and 7 days, when it showed its highest expression at almost 15-fold greater than the control. Statistical analysis indicated that this increased expression was significant at 72 h (p < 0.001), 7 days (p < 0.001), and 14 days (p < 0.001) post-ischaemia (Fig. 3b). This analysis demonstrated that all Oct-2 transcript variants identified showed a common mRNA up-regulation 7 days after pMCAO.
Oct-2 Protein Expression Progressively Increases After Cerebral Ischaemia
In order to analyse the protein expression profile of Oct-2 after cerebral ischaemia, we used two different commercially available antibodies. One of these antibodies was able to detect all the transcripts (Fig. 3c) (although only one band, representing the main transcript 002, was observed in the membranes), whereas the other is specific for the 678 transcript variant (Fig. 3d). Octamer-2 protein (60 kDa) quantified by Western blot showed a progressive increase, especially from 72 h to 14 days after permanent ischaemia in comparison with the control, and was significant at 14 days post-pMCAO (p < 0.01). The ENSRNOT00000048002 (Pou2f2-201) isoform (abbreviated as 002), with a theoretical molecular weight of 59 kDa, was the only Oct-2 transcript detected in the Western blot shown in Fig. 3c.
The ENSRNOT00000046678 (Pou2f2-203) isoform (44 kDa), abbreviated as 678 isoform, showed a progressive increase from 24 h to 14 days post-pMCAO, which was significant at 14 days post-ischaemia (p < 0.05) (Fig. 3d) when the protein expression was more than tenfold greater than in the control. The other transcript variants could not be analysed separately by Western blot as there were no specific antibodies. We therefore concluded that ischaemia induced an up-regulation of Oct-2, which reached its maximum expression 14 days after pMCAO.
Oct-2 Protein is Expressed in Neuronal Cells in Rat Cortical Brain
To further characterise the Oct-2 TF in control and ischaemic rat brain, we determined the neuronal localisation of Oct-2 TF in rat cortex. The immunofluorescence results in rat cortex slices showed Oct-2 protein expression to be localised in NeuN-positive cells both in control and MCAO conditions (Fig. 4) and that it was slightly increased in ischaemic conditions. Oct-2 was found to be expressed both in the nucleus (co-localising with DAPI and the neuron-specific nuclear protein (Neun) staining) and the cytoplasm in control and ischaemic conditions, which was slightly greater in the nucleus of neurons from the infarct border zone (left of the pMCAO image) in ischaemic conditions.
The Oct-2 transcription factor protein is expressed in neuronal cells in control and ischaemic rat cortical brain. The presence and localisation of Oct-2 protein in brain cortex slices were analysed by immunofluorescence using antibodies against: Oct-2 (green), the cell marker NeuN (red), and DAPI (blue), in control and pMCAO (24 h) conditions. The images were obtained with a ×20 objective and merged on BD Pathway 855 Bioimager System using BD Attovision software (original magnification, ×200) (Color figure online)
Octamer-2 Protein Interacts with Transcription Factors involved in Neuronal and Vascular Development and Basic Cellular Functions
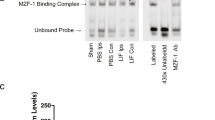
In order to elucidate in which signalling pathways Oct-2 is involved, we analysed the interaction profile of the Oct-2 TF in rat cortical brain slices. The TF–TF array showed that the Oct-2 protein in control conditions interacts with a variety of TFs, including ERE, MEF, ETS, MYC-MAX, OCT-1, NFκB, RXR(DR1), SIE, Smad SBE, and VDR(DR3). Other TFs including NF-E1, NF-E2, STAT4, USF-1, HSE, and RAR(DR5) were found with lesser intensity, meaning that they are weak interactions (Fig. 5b). Nevertheless, the previously mentioned TF interactions with Oct-2 changed in transient ischaemic conditions in comparison with the control tissue sample. On the one hand, ERE, OCT-1, NFKB, MYC-MAX, and VDR(DR3) interactions were maintained. On the other hand, ETS, MEF, NF-E2, NF-E1, RAR(DR5), RXR(DR1), SIE, Smad SBE, STAT4, USF-1, and HSE interactions disappeared. In contrast, new TF interactions with NF-1 and SRE were observed, although they were detected as weak interactions (Fig. 5c). All the different Oct-2 TF interactions showed in control and ischaemic condition panels of the array are summarised in Fig. 5d. The Oct-2 TF interactions found are involved in important brain processes, including neuronal and vascular development, neuronal survival, and basic cellular functions (growth, apoptosis, differentiation, and homeostasis). The present analysis demonstrated that ischaemia induced changes in the Oct-2 signalling pathways, promoting different TF interactions in comparison with the Oct-2 profile in control conditions.
Oct-2 TF–TF interaction profile analysis. Comparison of the Oct-2 interaction profile performed with the TranSignal™ TF–TF Array Kit version I between negative control (a), control tissue (b), and ischaemic (c) rat brain nuclear extract samples (7 days of reperfusion after tMCAO, ipsilesional core). The main Oct-2 interactions with other TFs in control and tMCAO conditions, found in the array, are listed in d. A negative control (normal goat IgG antibody) was used to elucidate false-positive interactions. Strong interactions of Oct-2 are shown in black, weak interactions are indicated in grey (a–c), and new interactions are showed underlined (d)
In Vitro Oct-2 Knockdown Promotes Neuronal Cytotoxicity
Finally, in order to further elucidate the Oct-2 function in brain, we performed a knockdown study in rat neuronal culture and analysed the potential role of Oct-2 in neuronal injury. The treatment of rat cortical neurons in culture with Oct-2 siRNA, which recognises all Oct-2 transcript variants, showed a diminution of Oct-2 protein expression at 4 and 5 days post-transfection (a reduction of 30 and 20 %, respectively) which was significant (p < 0.01) at the fourth day (Fig. 6a). Moreover, the Oct-2 siRNA-treated RN group presented a slight increase in LDH release compared to the non-target siRNA-treated RN group, from 4 to 6 days post-transfection, being significant at 6 days (p < 0.05) (Fig. 6b). These experiments showed that RN cultures with a decreased Oct-2 expression of 30 % or less correlated with an increase in neuronal toxicity and cell injury compared with neurons with unaltered Oct-2 expression, in control conditions.
The Oct-2 TF protein knockdown by siRNA treatment in rat cortical neurons (at 4 and 5 days after transfection) (a) promotes an increase in LDH release of the culture from 4 to 6 days post-transfection (b). Results from Western blot were normalised with β-actin. Cytotoxicity was expressed as a percentage of the mean maximal LDH value (0.1 % Triton X-100 treated cells) and represented in comparison with the negative control group (* p < 0.05; ** p < 0.01; # p < 0.001)
Discussion
In the present study, we found a differential binding activity of the Oct TFs family after cerebral ischaemia which led to the performance of an extensive characterisation of the Oct-2 TF in control and ischaemic rat brain cortex in order to investigate its putative role in stroke. A neuronal localisation of the TF was found in control and ischaemic rat brain and a progressive increase in mRNA and protein expression in the late phase of ischaemia. We found that Oct-2 interacts with other TFs involved in important brain processes including neuronal and vascular development, neuronal survival, and basic cellular functions and describe Oct-2 as being involved in preventing cytotoxicity and neuronal injury in vitro.
Two in vivo models of focal ischaemia have been used in the present study. tMCAO was selected for the TF-binding activity and TF–TF interaction array, in which the aim was to identify differences among the different affected brain zones along the time of post-ischaemia. This model shows a slow extension of the infarct core into the penumbra, thus allowing a more prolonged and consistent peri-infarct area (Hossmann and Traystman 2009). In contrast, for the study of transcript gene expression and sub-cellular localisation, a pMCAO was chosen, since in this model, the core expands into the penumbra much faster (Hossmann and Traystman 2009) and the infarct volume shows greater reproducibility.
In order to identify new TFs and elucidate novel regulatory mechanisms implicated in cerebral ischaemia, a multiplex TF-binding activity analysis was performed. For this analysis, we used the Marligen Multiplex Transcription Factor Profiling Assay, which is compatible with Luminex xMAP® technology, to simultaneously analyse the binding activity of different TFs in a quantitative and reproducible format. This technique is faster and easier than EMSAs, fivefold to tenfold more sensitive than colorimetric ELISAs, and the multiple binding site analysis mimics in vivo conditions.
Among the 50 TFs analysed, the octamer family showed a dramatic change in its binding activity profile during the acute and late phases after MCAO. Among octamer family, we focused on Oct-2 TF given that it is the only member of this family that was specifically expressed in the brain with an expression profile that varied post-ischaemia and due to the structural and functional complexity of the different transcript variants described (Wirth et al. 1991; Lillycrop and Latchman 1992; Annweiler et al. 1994).
Although Oct-2 expression has also been described in astrocytes (Schreiber et al. 1990) and in microvascular endothelial cells (Boutet et al. 2001), we focused the present study on determining the localisation of the Oct-2 protein in neuronal cells in control and ischaemic rat brain given that this has been reported by numerous laboratories as being expressed in the neuronal cells of different mammal species in control conditions (He et al. 1989; Scholer et al. 1989; Kemp et al. 1990; Hatzopoulos et al. 1990; Lillycrop et al. 1991; Stoykova et al. 1992). Immunofluorescence in rat cortical slices revealed a nuclear and cytoplasm localisation of Oct-2 in neuronal cells, which was slightly greater in the nucleus in ischaemic conditions (24 h post-pMCAO). The nuclear increase in Oct-2 was observed as limited to the infarct border. In contrast, Oct-2 protein up-regulation in the Western blot analysis was observed in the late phase after ischaemia. These differences between the two experiments may be due to the fact that the small differences observed in specific regions of the cortical slices by immunofluroescence overlapped in the Western blot analysis, where brain tissue homogenates were used.
In mouse, it has been described that the primary RNA transcript of the Oct-2 gene is subject to alternative splicing to yield different transcripts of the mRNA with distinct effects on gene expression in B lymphocytes (Oct-2.1 and Oct-2.3 isoforms) compared to neuronal cells (Oct-2.4 and Oct-2.5 isoforms). The inclusion (in Oct-2.1) or exclusion (in Oct-2.4 and Oct-2.5) of the full length CTD and the presence of a negative regulatory domain (NRD) (in Oct-2.3) in the Oct-2 protein determine the transcriptional function and its transactivation potential (Latchman 1996a). Thus, the identification and individual analysis of the different Oct-2 transcript variants in rat brain were essential in order to avoid misinterpretations whether due to analysis of all the transcripts together or the study of a specific reference variant. This study showed that five of the six predicted rat variants are expressed in control as well as in ischaemic rat cortex. According to Ensembl sequences and the nomenclature previously used for Oct-2 mouse transcripts (Wirth et al. 1991), rat transcripts should correspond to Oct-2.5 (ENSRNOT00000048002 or Pou2f2-201), Oct-2.3 (ENSRNOT00000027649 or Pou2f2-202), and Oct-2.6 (ENSRNOT00000046678 or Pou2f2-203). The ENSRNOT00000041651 and the ENSRNOT00000068776 did not match any of the transcripts previously described in mice, although ENSRNOT00000041651 showed a certain structural similarity with the Oct-2.3 (the NRD motif) and the Oct-2.5 transcript (a truncated C-terminus domain). All the transcripts analysed contained the DNA-binding motif necessary for the TF function with the exception of ENSRNOT00000068776. This transcript variant was found to consist only of the minimum structure (the specific POU and homeo-subdomains) for it to bind to its target sequence, without the presence of any transactivation domain. According to previous studies in mouse (Annweiler et al. 1994; Corcoran et al. 2004), the ENSRNOT00000046678 (Oct-2.6) and ENSRNOT00000027649 (Oct-2.3) transcripts identified in rat brain samples could have an activating transcriptional activity, as they present the full C-terminus activation domain. In this domain, the nine amino acids shown to be critical for the CTD function can be identified (Fig. S5). On the other hand, the ENSRNOT00000048002 (Oct-2.5) and ENSRNOT00000041651 transcripts that lack the full CTD domain containing the nine critical amino acids might perform an inhibitory transcriptional activity.
The results of the different experiments performed were found to agree with each other: (a) the mRNA expression profiles of the analysed Oct-2 transcripts tended to be similar, increasing progressively in the late phase of ischaemia (around 7 days); (b) the Oct-2 protein was shown to increase at 14 days post-pMCAO; and (c) the Oct-2 TF-binding activity induction (versus the control) was observed at 14 days after ischaemia. In addition, the mRNA and protein expression patterns followed a concordant profile, showing an mRNA increase 7 days after pMCAO which could lead to a peak in protein expression observed at 14 days after ischaemia. The ENSRNOT00000046678 (Pou2f2-203) transcript particularly stands out as it shows a huge increase in its expression at 7 days post-pMCAO. However, the ENSRNOT00000048002 (Pou2f2-201) transcript variant is found to be the predominant variant in the samples studied here.
With regards to the function of Oct-2, it has been suggested that it may play a critical role in the normal development of the central nervous system of mammals (Latchman 1996a) and, particularly, for post-natal survival (Phillips and Luisi 2000; Corcoran et al. 2004). In order to better understand this function, a TF–TF interaction array was performed. This analysis showed that Oct-2 interacts with several TFs which principally modulate neuronal and vascular development processes and basic cellular functions (surveillance, apoptosis, growth, differentiation, and homeostasis). Specifically, the present study showed that Oct-2 could participate in the regulation of the angiogenesis and vascular development (through ETS interaction) (Lelievre et al. 2001; Sato et al. 2001); the survival of newly differentiated neurons and the cardiovascular development (through MEF) (Ikeshima et al. 1995; Naya et al. 1999; Agarwal et al. 2011); neuronal cell death and inflammation (through NFκB) (Qin et al. 1998; Crack and Taylor 2005); cellular proliferation, differentiation, and apoptosis (through Myc-Max) (Chen et al. 1995; Tencheva and Panov 2008); and growth, differentiation, development, and homeostasis processes [through ERE (Lee and Mouradian 1999) and RXR(DR1) (Collino et al. 2008; Giaginis et al. 2011; Mathisen et al. 2011)]. These results agree with earlier studies in humans (Andersen and Rosenfeld 2001) in which some of the previous Oct-2 interactions with other DNA-binding proteins, such as MEF, NF1, and nuclear hormone receptors (RXR and VDR), are described. In addition, as previously reported (Andersen and Rosenfeld 2001), we can conclude that Oct-2 can heterodimerise with other factors as the interaction with the Oct-1 TF observed in the present study demonstrates. Moreover, the present study has shown that ischaemia induced changes in the Oct-2 interaction profile, promoting new as well as the disappearance of some interactions. However, this does not imply a decrease in Oct-2 transcription activity. The cooperative assembly among different TFs may act as a repressor (not allowing the TF to bind to its target sequences) or as a promoter (acting as a co-activator), which is necessary for target promoter binding (Martinez 2002). Therefore, depending on the function of these interactions in the Oct-2 interaction profile, disruption may lead to inhibition or activation of the different target promoter sequences. Further investigations will be required to elucidate the role of these specific multi-protein interactions.
Finally, in order to investigate the Oct-2 potential function in the brain, we performed knockdown experiments with rat cortical neurons in culture to test its possible involvement in neuronal survival and damage, as it seems to point the results from the TF–TF interaction array. The culture was treated with Oct-2 siRNA, and the neuronal cytotoxicity was analysed by LDH release measurement over time post-siRNA transfection. These experiments showed a correlation between Oct-2 knockdown and an increase in the LDH leakage from rat cortical neuron culture. Previous studies have shown that the efflux of LDH occurring from either necrotic or apoptotic neurons is proportional to the number of damaged or destroyed cells (Koh and Choi 1987; Gwag et al. 1995), being a parameter of cellular injury (Arce et al. 2012; Thoresen et al. 2012). Our results show that a reduction in Oct-2 expression in neuronal cells leads to a slight increase in neuronal injury in vitro, suggesting that Oct-2 seems to be involved in preventing neuronal cytotoxicity. We have observed a trend of increasing neuronal damage in Oct-2 siRNA-treated neurons from 4 to 6 days after transfection, showing non-markedly differences compared with the control neurons. Surely, this slight increase, we observed, is proportional to the percentage of Oct-2 protein knockdown obtained, which was of 20–30 % compared to the control. Some previous studies have already showed the Oct-2 TF role in promoting neuronal surveillance. It has been described that Oct-2 is being up-regulated 3–4 times by NGF (neuronal growth factor) in sensory rat neurons, thus suggesting that Oct-2 plays a role in mediating the transcriptional effects (promotion of neuronal survival and preventing neuronal death) induced by this growth factor (Wood et al. 1992; Kim et al. 2004). Moreover, it has also been reported that Oct-2 TF is involved in the regulation of genes encoding different synaptic proteins (SNAP-25 and synapsin I) in neuronal cells (Deans et al. 1997). In the present study, we have found that the inhibitory Pou2f2-201 isoform is the predominant one in the rat ischaemic brain, so we hypothesise that this variant could prevent neuronal injury directly inhibiting cellular death signalling pathways as described for Oct-4 and miR-125b/BAK1 pathway (Wang et al. 2013). On the other hand, we have also demonstrated that the transcripts variants Pou2f2-202 and Pou2f2-203 that are characterised for an activating transcriptional activity are up-regulated by ischaemia. These transcript variants could reduce neuronal injury by promoting pro-survival signalling pathways (by directly regulating bcl-2 expression) (Heckman et al. 2006). Thus, the present study is the first one to demonstrate the Oct-2 potential to prevent neuronal toxicity. Further experiments are necessary to fully understand how the TF perform this role: directly (inhibiting neuronal cell death or activating the neuronal pro-survival signalling pathways) or through the interaction with other TFs (found in the TF–TF array) involved in the activation of homeostasis processes which promote the restoration of neuronal functions.
Therefore, the results from the present functional studies (TF–TF interaction array and knockdown studies) suggest that Oct-2 is involved in counteracting the mechanisms that cause neuronal injury, which could lessen the infarct progression in the late phase when the maximum expression is observed. Hence, it seems likely that the up-regulation of Oct-2 TF could play a role in functional pathophysiological recuperation after ischaemia. In the acute phase, the induction of Oct-2 TF expression may be effective in reducing the ischaemic-mediated neuronal death and so could be an effective brain protector therapy to be used in the first hours after stroke.
Conclusion
To the best of our knowledge, this is the first study in which the octamer family, specifically the Oct-2 TF, has been studied in cerebral ischaemia. Here, we show that differences in Oct-2 binding activity and gene expression are observed in the acute and late phase of ischaemia. We also describe Oct-2 neuronal localisation and its interactions with other TFs in control and ischaemic rat brain. Finally, our findings provide evidence for Oct-2-mediated responses having an overall beneficial role in neuronal physiological functions, suggesting that it could be involved in reducing neuronal injury in the context of cerebral ischaemia. Further studies are necessary to validate the role of Oct-2 in stroke and determine whether Oct-2 TF promotes these effects directly or indirectly, forming a multi-protein complex through interaction with other TFs.
Materials and Methods
All procedures were approved by the Committee of Animal Care of the Universidad Complutense of Madrid in accordance with European Union regulations (86/609/CEE) and Spanish legislation (RD223/88).
Bioinformatics
Octamer-2 rat transcript variant identification was performed using Ensembl gene predictions and related sequences of Entrez Gen at the NCBI (National Center for Biotechnology Information). Ensembl release 69—October 2012, and Ensembl release 70—January 2013, were used (Hubbard et al. 2009, b). While the present manuscript was being prepared, the Ensembl database was updated with the result that Ensemble release 69 became Ensembl release 70 and that the original six transcript variants became only three (Pou2f2-201, Pou2f2-202, and Pou2f2-203) for the rat Oct-2 gene. Therefore, in the present study, all of the original six transcript variants were considered in characterising Oct-2 in ischaemic rat brain. Homology between transcript sequences was determined using Clustalw2. Sequence data were also aligned using this software (Chenna et al. 2003). The theoretical molecular weights of the different Oct-2 isoforms were obtained using the Compute pI/Mw tool of the Expert Protein Analysis System (ExPASy) on the Swiss Institute of Bioinformatics website (2006). Primer3 software was used for PCR primer design (2009c), and 7,000 System software v1.2.3 (Applied Biosystems) was used to perform qPCR and to further analyse the data obtained.
In Vivo Cerebral Ischaemia Models
Experiments were performed on adult male Fischer rats (250–300 g body weight; Harlan). Animals were housed individually under standard conditions of temperature and humidity and with a 12-h light/dark cycle (lights on at 08:00) with free access to food and water. Rats were anaesthetised with isoflurane 1.5–2 % with a mixture of 70 % nitrogen and 30 % oxygen. Body temperature was maintained at physiological levels with a heating pad during the surgical procedure and anaesthesia recovery.
Transient Middle Cerebral Artery Occlusion in Rats
The transitory cerebral ischaemia model was performed according to a previously reported 3-vessel occlusion model (Chen et al. 1986; Liu et al. 1989; Sobrado et al. 2003). After 90 min of distal occlusion of the left MCA and both common carotid arteries (CCA), the three arteries were opened and complete reperfusion was observed under an operating microscope. Transient MCAO rats were killed at 6, 24, and 72 h and 7 and 14 days after reperfusion (n = 3 rats in each group). Brains were removed, and cortical ipsilesional core, ipsilesional peri-infarct, and ipsilesional non-damaged tissue, as well as contralesional cortex tissue [as shown in Fig. 7, adapted from (Sobrado et al. 2011)], were collected at each period of time. The ischaemic core was defined as the cortical tissue surrounding the occluded MCA, which differed from adjacent tissue consistency and according to Sobrado et al. (2011). The peri-infarct tissue was identified as the cortical tissue immediately adjacent to the core and based on the average images (apparent diffusion coefficient, ADC; and cerebral blood flow, CBF) according to Sobrado et al. (2011).
Scheme of the sample collection after rat tMCAO. The brain was sliced in coronal sections corresponding to the territory of the MCA. The cortical ipsilesional tissue was identified by the different consistency of the tissue, and for the rest of the regions, we proceeded as shown in the picture [adapted from (Sobrado et al. 2011)]
Samples were immediately frozen at −80 °C until nuclear extract isolation. Contralesional tissue was used as a control to conduct the TF-binding activity assay.
Permanent Middle Cerebral Artery Occlusion in Rats
The permanent cerebral ischaemia model was induced following a previously described method (Hurtado et al. 2005; Mallolas et al. 2006). Briefly, permanent focal cerebral ischaemia was induced by ligature of the left common carotid artery and occlusion of the ipsilateral distal MCA. Brains were removed, and cortical infarcted and peri-infarcted tissue were collected from the pMCAO animals at 6, 24, and 72 h and 7 and 14 days after occlusion (n = 6 rats in each group). Samples were divided into two and frozen at −80 °C until RNA, and protein isolation were undertaken.
Likewise, control samples from healthy animals were also collected following the same protocol in order to perform the gene expression analysis, the protein study, and the TF–TF interaction array.
Transcription Factor Binding Activity Assay
A Luminex bead-based system was used to simultaneously assess the binding activity of 50 different TFs (Table S2) in nuclear extracts from rat brain after tMCAO. The nuclear extracts were obtained from control and transient ischaemic rat brain samples using a Nuclear Extraction kit (Marligen Biosciences) in accordance with the manufacturer’s instructions. TFs were analysed with a Luminex® 200™ instrument using Marligen Multiplex Transcription Factor Profiling Assay (Marligen Biosciences) and StarStation™ software for data acquisition. This assay is based on the specific binding of TFs to cognate DNA sequences on labelled beads (polystyrene microspheres internally dyed with fluorophores) (xMAP® technology). The sequences are mined from protein binding sequences in the TRANSFAC database (http://www.gene-regulation.com/pub/databases.html). Within the analyser, lasers excite the internal dyes that identify each microsphere particle and also capture any reporter dye during the assay. In this way, the technology allows multiplexing of up to 100 unique assays within a single sample. The assay is more sensitive than enzyme-linked immunosorbent assay (ELISA) or gel shift assay (Shurin et al. 2005; Hansmann et al. 2008). The ipsilesional core, the ipsilesional peri-infarct, and the ipsilesional non-damaged tissue, as well as the contralesional cortex tissue from each rat brain, were analysed separately following the manufacturer’s recommendations. About 10 μg of nuclear extracts was used to perform the activation profile analysis of the 50 TFs. Positive and negative (background) controls and HL-60 cells treated and untreated with PMA/lonomycin for 24 h were used as the assay control and nuclear extract control, respectively.
The binding activity was measured in mean fluorescence intensity (MFI) in accordance with the manufacturer’s instructions. In order to quantitatively measure the magnitude of the changes, an algorithm based on least median squares (LMS to estimate the slope and intercept of the line that best fits the collinear points) was used. The significance of change was represented by Dev F, which is the ratio of the difference between the MFI of the treated sample and the expected value to the sum of the standard deviations of the treated and untreated sample. A Dev F value of two or greater is considered significant. MFI values in control and ischaemic samples are compared in a scatter plot graph (Fig. 1). Each point in Fig. 1 represents a single TF. Data points on the scatter plot that are co-linear or nearly co-linear represent TFs with unchanged binding activity. Data points that are significantly distant from the co-linear points represent TFs that have changed their binding activity due to the treatment, which in this case is the induced ischaemia (tMCAO).
Oct-2 Expression Study in Rat Brain
RNA Extraction, Quantification, and Retrotranscription
RNA extraction was undertaken from rat brain tissue submitted to pMCAO. Qiazol lysis reagent (Qiagen) was immediately transferred to frozen samples of cerebral cortex and then homogenised using an Ultra-Turrax T25 homogeniser. The protocol for the use of the RNeasy® Lipid Tissue Mini Kit (Qiagen) for RNA quantification and purity estimation (GeneQuant, Biochrom) and reverse transcription (High Capacity cDNA Reverse Transcription Kit, Applied Biosystems) was followed as previously described (Gubern et al. 2009). Two independent retrotranscription reactions were performed for all samples.
Identification of Oct-2 Transcript Variants
Rat Oct-2 transcript variants were predicted using Ensembl software (Hubbard et al. 2009; 2009b). The identification of the Oct-2 transcripts in control and ischaemic cortex was performed by conventional polymerase chain reaction (PCR) using retrotranscribed cDNA and a pair of primers specifically designed, except in the case of ENSRNOT00000027655, to amplify each transcript variant separately (Table S3). In the case of ENSRNOT00000027655, amplification was undertaken by designing a pair of oligonucleotides that amplify both this specific transcript and the rest of the transcript variants.
Analysis of Oct-2 Transcripts Expression in Rat Cortex
Gene expression analysis of Oct-2 transcripts in each sample (control and permanent ischaemic samples) was conducted using quantitative real-time PCR (qPCR) (with the 2-ΔΔCT method). Specific TaqMan® Gene Expression Assays were designed to study the individual transcripts. To correctly perform ENSRNOT00000046678 (Pou2f2-203) transcript variant quantification, it was necessary to preamplify all samples for this transcript and the reference genes using TaqMan® PreAmp Master Mix following the manufacturer’s instructions. The assay design was performed with the Custom TaqMan® Assay Design Tool on the Applied Biosystems website (2009a). The gene expression conditions have been previously described (Gubern et al. 2009). Reactions were run in an ABI PRISM 7000 Instrument (Applied Biosystems), and TaqMan® Universal PCR Master Mix was used. Ywhaz and Sdha were used as reference genes for expression data normalisation as has been previously described (Gubern et al. 2009).
Protein Extraction and Quantification
Frozen cerebral cortex samples from permanent ischaemia were homogenised by sonication during 10–12 s and using a homogenisation buffer containing a protease inhibitor cocktail (serine, cysteine, and metalloproteases) and 0.1 % Nonidet P40 (Roche). Rat cortical neuronal culture (RN) samples (transfected Oct-2 and non-target siRNA) were homogenised using a lysis buffer (Cell Signalling) with PMSF (1 %), mixed with vortex every 5 min for 30 min while maintained in ice. Cortex and RN homogenised samples were then centrifuged, and the supernatant (protein) was collected. Protein quantification was performed using a Protein Assay Kit (Bio-Rad) based on the Bradford method in accordance with the manufacturer’s instructions.
Western Blot
Brain tissue homogenates from control and permanent ischaemic (pMCAO) rats containing 60 μg of protein and lysates from siRNA transfected RN containing 10 μg of protein were loaded, and the proteins were size-separated in 10 % SDS-PAGE (90 mA) (Romera et al. 2004; Mallolas et al. 2006). The proteins were blotted onto a PVDF membrane (GE Healthcare) and incubated with the specific primary antibody against Oct-2 (sc-25400; 1:200; Santa Cruz Biotechnology), which binds to 360-479 amino acids of Oct-2 so as to recognise all the different transcript variants. Another primary antibody against Oct-2 was used (sc-233; 1:200; Santa Cruz Biotechnology), which only recognises one of the transcript variants (ENSRNOT00000046678). Proteins recognised by the antibodies were revealed with SuperSignal West Pico Chemiluminescent Substrate (Thermo Scientific) used in accordance with the manufacturer’s instructions. β-actin was used as the loading control. Specific signals were quantified with densitometry analysis software (Kodak MI 5.0 SE version).
Immunofluorescence
Twenty-four hours after MCAO, rats (n = 2 for each group) were anaesthetised, fixed, and cryopreserved as previously reported (Sobrado et al. 2009). Brains were frozen and serials of 40-μm-thick coronal sections were cut with a sliding microtome (Leica SM200R) and mounted on glass slides. Adjacent sections were then processed to perform immunohistochemistry. Primary antibodies rabbit polyclonal anti-Oct-2 (1:50; Sta Cruz Biotechnology, sc-25400) and the respective cell marker mouse monoclonal anti-NeuN (1:100; Chemicon, MAB377) were used. Secondary antibody staining using Alexa Fluor 488/594 goat anti-rabbit/mouse IgGs (Invitrogen) and counterstaining using DAPI (Invitrogen) were performed following BD Biosciences protocols. Images were captured by different channels for Alexa Fluor 488 (pseudo-coloured green), Alexa Fluor 594 (pseudo-coloured red), and DAPI (pseudo-coloured blue) on a BD Pathway™ 855 Bioimager System (Becton–Dickinson Biosciences) with ×20 objective (NA 075 Olympus). The z-stack application was used to obtain the images using BD Attovision™ software. Both acquisition and merging of images were carried out according to the recommended assay procedure using BDAttovision™ software.
Oct-2 Interaction Analysis in Rat Brain
In order to assess the interactions of Oct-2 and determine the cellular processes it is involved in, a TranSignal™ TF–TF Array Kit version I (Panomics) was used in accordance with the manufacturer’s instructions. This kit consists of a ChIP-Array method based on a combination of the chromatin immunoprecipitation (ChIP) and a high-throughput technique (array). These two coupled techniques allow the active transcription factor binding sites (TFBS) of a specific TF to be mapped efficiently. Moreover, combining array profiling and ChIP data permits a more effective TFBS analysis for the study of the function of a TF (Qin et al. 2011).
About 30 μg of nuclear extracts was incubated with a cocktail of biotin-labelled double-strand DNA oligonucleotide probes (known TF-binding consensus sequences). About 2 μg of Oct-2 antibody (Santa Cruz Biotechnology) was used to immunoprecipitate Oct-2-associated TFs and their corresponding cis-elements. A control antibody (normal IgG; Santa Cruz Biothecnology) was used as a negative control. Different washing steps were then performed to eliminate free cis-elements and non-specific binding proteins. Finally, the bounded cis-elements were eluted and hybridised to the TranSignal™ Protein/DNA Array membranes, spotted with 54 different consensus DNA sequences, which are complementary to the known TF target sequences, TFBS. The symbols and complete names of the TFs which were studied are shown in Table S4 (supplementary information). The membranes were revealed with the detection compounds from the kit, which was used in accordance with the manufacturer’s instructions. This array is a qualitative assay in which the spots indicate the presence or absence of the TF interaction. Therefore, the signal intensity of the array spots is not proportional to the amount of interaction, but rather is proportional to the quality of these interactions (strong or weak).
Treatment of Cortical Neurons with Oct-2 siRNA
In order to study and elucidate the role of Oct-2 in cerebral ischaemia, pure rat cortical neuronal cultures (RN) were prepared as previously described (Romera et al. 2004) for use in gene knockdown experiments. Cells were seeded (1.5 × 106 per well) in six-well plates (Cultek) previously coated with poly-lysine (Sigma), and the Oct-2 siRNA transfection was performed at 10–12 days in vitro (DIV). The RN cells were transfected with a mixture containing basal medium, 16.7 μl/well HiperFect Transfection Reagent (Qiagen), and 50 nM/well of ON-TARGETplus SMARTpool Oct-2 siRNA (a mixture of four Oct-2 siRNAs) (Dharmacon) or 50 nM/well of non-targeting siRNA (Dharmacon) as the negative control of siRNA transfection. Twenty hours after siRNA transfection, the medium was replaced by complete RN growth medium. For this study, we used non-target siRNA-treated RN culture as control group, as in the optimisation study, the different control groups tested (non-treated cells, transfection reactive only treated cells (mock), and non-target siRNA-treated cells) showed no significant differences (p > 0.05) in viability and cytotoxicity. From 4 to 6 days after transfection, culture cytotoxicity was assessed by lactate dehydrogenase (LDH) assay (Fig. 6b). As a marker of cell injury (necrotic damage), LDH release from damaged cells was determined using the CytoTox 96® Non-Radioactive Cytotoxicity Assay (Promega) and measured spectrophotometrically at 490 nm using a microplate reader (Tecan). LDH was measured in at least three different wells per experiment. The results were normalised to the mean maximal LDH value, corresponding to cells exposed to 0, 1 % Triton X-100, which causes near complete neuronal cell death (100 %). The results are expressed as a percentage of the maximal LDH level and represented in comparison with the negative control group (Lobner 2000; Pan et al. 2012; Xie et al. 2012). At 4 and 5 days post-transfection, the cells were collected and frozen at −80 °C until protein isolation was undertaken (Fig. 6a).
Statistical Analysis
Results are expressed as mean ± standard error of the mean (SEM). A one-way analysis of variance (ANOVA) test (or the Kruskal–Wallis test when data were not normally distributed) was conducted, followed by Dunnett’s post hoc analysis (or the Mann–Whitney test when data were not normally distributed) to compare each of the time points analysed post-pMCAO with the control group mean. Comparison between groups of the siRNA transfection experiment was made by the Student’s unpaired t test. A p value <0.05 was considered statistically significant (* p < 0.05, ** p < 0.01, # p < 0.001). Statistical analysis was performed using the 11.5.0 version of SPSS software (SPSS Inc).
References
Agarwal, P., Verzi, M. P., Nguyen, T., Hu, J., Ehlers, M. L., McCulley, D. J., et al. (2011). The MADS box transcription factor MEF2C regulates melanocyte development and is a direct transcriptional target and partner of SOX10. Development, 138, 2555–2565.
Andersen, B., & Rosenfeld, M. G. (2001). POU domain factors in the neuroendocrine system: Lessons from developmental biology provide insights into human disease. Endocrine Reviews, 22, 2–35.
Annweiler, A., Zwilling, S., & Wirth, T. (1994). Functional differences between the Oct2 transactivation domains determine the transactivation potential of individual Oct2 isoforms. Nucleic Acids Research, 22, 4250–4258.
Arce, C., Diaz-Castroverde, S., Canales, M. J., Marco-Contelles, J., Samadi, A., Oset-Gasque, M. J., et al. (2012). Drugs for stroke: action of nitrone (Z)-N-(2-bromo-5-hydroxy-4-methoxybenzylidene)-2-methylpropan-2-amine oxide on rat cortical neurons in culture subjected to oxygen-glucose-deprivation. European Journal of Medicinal Chemistry, 55, 475–479.
Baranova, O., Miranda, L. F., Pichiule, P., Dragatsis, I., Johnson, R. S., & Chavez, J. C. (2007). Neuron-specific inactivation of the hypoxia inducible factor 1 alpha increases brain injury in a mouse model of transient focal cerebral ischemia. Journal of Neuroscience, 27, 6320–6332.
Boutet, S. C., Quertermous, T., & Fadel, B. M. (2001). Identification of an octamer element required for in vivo expression of the TIE1 gene in endothelial cells. Biochemistry Journal, 360, 23–29.
Chen, S. T., Hsu, C. Y., Hogan, E. L., Maricq, H., & Balentine, J. D. (1986). A model of focal ischemic stroke in the rat: Reproducible extensive cortical infarction. Stroke, 17, 738–743.
Chen, J., Willingham, T., Margraf, L. R., Schreiber-Agus, N., DePinho, R. A., & Nisen, P. D. (1995). Effects of the MYC oncogene antagonist, MAD, on proliferation, cell cycling and the malignant phenotype of human brain tumour cells. Nature Medicine, 1, 638–643.
Chenna, R., Sugawara, H., Koike, T., Lopez, R., Gibson, T. J., Higgins, D. G., et al. (2003). Multiple sequence alignment with the Clustal series of programs. Nucleic Acids Research, 31, 3497–3500.
Chopp, M., Zhang, Z. G., & Jiang, Q. (2007). Neurogenesis, angiogenesis, and MRI indices of functional recovery from stroke. Stroke, 38, 827–831.
Chopp, M., Li, Y., & Zhang, J. (2008). Plasticity and remodeling of brain. Journal of the Neurological Sciences, 265, 97–101.
ClustalW2. http://www.ebi.ac.uk/Tools/clustalw2/index.html. 2010.
Collino, M., Patel, N. S., & Thiemermann, C. (2008). PPARs as new therapeutic targets for the treatment of cerebral ischemia/reperfusion injury. Therapeutic Advances in Cardiovascular Disease, 2, 179–197.
Corcoran, L. M., Koentgen, F., Dietrich, W., Veale, M., & Humbert, P. O. (2004). All known in vivo functions of the Oct-2 transcription factor require the C-terminal protein domain. The Journal of Immunology, 172, 2962–2969.
Crack, P. J., & Taylor, J. M. (2005). Reactive oxygen species and the modulation of stroke. Free Radical Biology & Medicine, 38, 1433–1444.
Custom TaqMan® Assay Design Tool. https://www5.appliedbiosystems.com/tools/cadt/. 13-10-2009a.
Deans, Z., Dawson, S. J., Buttery, L., Polak, J. M., Wallace, D., & Latchman, D. S. (1995). Direct evidence that the POU family transcription factor Oct-2 represses the cellular tyrosine hydroxylase gene in neuronal cells. Journal of Molecular Neuroscience, 6, 159–167.
Deans, Z. C., Dawson, S. J., Kilimann, M. W., Wallace, D., Wilson, M. C., & Latchman, D. S. (1997). Differential regulation of genes encoding synaptic proteins by the Oct-2 transcription factor. Molecular Brain Research, 51, 1–7.
Dent, C. L., Lillycrop, K. A., Estridge, J. K., Thomas, N. S., & Latchman, D. S. (1991). The B-cell and neuronal forms of the octamer-binding protein Oct-2 differ in DNA-binding specificity and functional activity. Molecular and Cellular Biology, 11, 3925–3930.
Expert Protein Analysis System, Swiss Institute of Bioinformatics. http://www.expasy.ch/tools/pi_tool.html. 9-1-2006.
Ensembl. http://www.ensembl.org/index.html. 2009b.
Fisher, M., Feuerstein, G., Howells, D. W., Hurn, P. D., Kent, T. A., Savitz, S. I., et al. (2009). Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke, 40, 2244–2250.
Ford, G., Xu, Z., Gates, A., Jiang, J., & Ford, B. D. (2006). Expression Analysis Systematic Explorer (EASE) analysis reveals differential gene expression in permanent and transient focal stroke rat models. Brain Research, 1071, 226–236.
Giaginis, C., Klonaris, C., Katsargyris, A., Kouraklis, G., Spiliopoulou, C., & Theocharis, S. (2011). Correlation of peroxisome proliferator-Activated Receptor-gamma (PPAR-gamma) and Retinoid X Receptor-alpha (RXR-alpha) expression with clinical risk factors in patients with advanced carotid atherosclerosis. Medical Science Monitor, 17, CR381–CR391.
Gubern, C., Hurtado, O., Rodriguez, R., Morales, J. R., Romera, V. G., Moro, M. A., et al. (2009). Validation of housekeeping genes for quantitative real-time PCR in in vivo and in vitro models of cerebral ischaemia. BMC Molecular Biology, 10, 57.
Gwag, B. J., Lobner, D., Koh, J. Y., Wie, M. B., & Choi, D. W. (1995). Blockade of glutamate receptors unmasks neuronal apoptosis after oxygen-glucose deprivation in vitro. Neuroscience, 68, 615–619.
Hansmann, G., de, J. P., V, Alastalo, T. P., Alvira, C. M., Guignabert, C., Bekker, J. M., Schellong, S., Urashima, T., Wang, L., Morrell, N. W., Rabinovitch, M. (2008). An antiproliferative BMP-2/PPARgamma/apoE axis in human and murine SMCs and its role in pulmonary hypertension. The Journal of Clinical Investigation, 118, 1846–1857.
Hatzopoulos, A. K., Stoykova, A. S., Erselius, J. R., Goulding, M., Neuman, T., & Gruss, P. (1990). Structure and expression of the mouse Oct2a and Oct2b, two differentially spliced products of the same gene. Development, 109, 349–362.
He, X., Treacy, M. N., Simmons, D. M., Ingraham, H. A., Swanson, L. W., & Rosenfeld, M. G. (1989). Expression of a large family of POU-domain regulatory genes in mammalian brain development. Nature, 340, 35–41.
Heckman, C. A., Duan, H., Garcia, P. B., & Boxer, L. M. (2006). Oct transcription factors mediate t(14;18) lymphoma cell survival by directly regulating bcl-2 expression. Oncogene, 25, 888–898.
Hossmann, K. A. & Traystman, R. J. (2009). Cerebral blood flow and the ischemic penumbra. In M. Fisher (Ed.), Stroke, Part I (pp. 67–92).
Hubbard, T. J., Aken, B. L., Ayling, S., Ballester, B., Beal, K., Bragin, E., et al. (2009). Ensembl 2009. Nucleic Acids Research, 37, D690–D697.
Hurtado, O., Moro, M. A., Cardenas, A., Sanchez, V., Fernandez-Tome, P., Leza, J. C., et al. (2005). Neuroprotection afforded by prior citicoline administration in experimental brain ischemia: effects on glutamate transport. Neurobiology of Diseases, 18, 336–345.
Ikeshima, H., Imai, S., Shimoda, K., Hata, J., & Takano, T. (1995). Expression of a MADS box gene, MEF2D, in neurons of the mouse central nervous system: implication of its binary function in myogenic and neurogenic cell lineages. Neuroscience Letters, 200, 117–120.
Kemp, L. M., Dent, C. L., & Latchman, D. S. (1990). Octamer motif mediates transcriptional repression of HSV immediate-early genes and octamer-containing cellular promoters in neuronal cells. Neuron, 4, 215–222.
Kim, D. H., Zhao, X., Tu, C. H., Casaccia-Bonnefil, P., & Chao, M. V. (2004). Prevention of apoptotic but not necrotic cell death following neuronal injury by neurotrophins signaling through the tyrosine kinase receptor. Journal of Neurosurgery, 100, 79–87.
Kitagawa, K., Sasaki, T., Terasaki, Y., Yagita, Y., & Mochizuki, H. (2012). CREB activation is a key player for ischemic tolerance in the brain. Rinsho Shinkeigaku, 52, 904–907.
Koh, J. Y., & Choi, D. W. (1987). Quantitative determination of glutamate mediated cortical neuronal injury in cell culture by lactate dehydrogenase efflux assay 1. Journal of Neuroscience Methods, 20, 83–90.
Kristie, T. M., & Sharp, P. A. (1990). Interactions of the Oct-1 POU subdomains with specific DNA sequences and with the HSV alpha-trans-activator protein. Genes & Development, 4, 2383–2396.
Latchman, D. S. (1996a). Activation and repression of gene expression by POU family transcription factors. Philosophical Transactions of the Royal Society of London. Series B, Biological sciences, 351, 511–515.
Latchman, D. S. (1996b). The Oct-2 transcription factor. International Journal of Biochemistry & Cell Biology, 28, 1081–1083.
Lee, S. H., & Mouradian, M. M. (1999). Up-regulation of D1A dopamine receptor gene transcription by estrogen. Molecular and Cellular Endocrinology, 156, 151–157.
Lelievre, E., Lionneton, F., Soncin, F., & Vandenbunder, B. (2001). The Ets family contains transcriptional activators and repressors involved in angiogenesis. International Journal of Biochemistry & Cell Biology, 33, 391–407.
Li, L., Zhang, X., Cui, L., Wang, L., Liu, H., Ji, H., et al. (2013). Ursolic acid promotes the neuroprotection by activating Nrf2 pathway after cerebral ischemia in mice. Brain Research, 1497, 32–39.
Lillycrop, K. A., & Latchman, D. S. (1992). Alternative splicing of the Oct-2 transcription factor RNA is differentially regulated in neuronal cells and B cells and results in protein isoforms with opposite effects on the activity of octamer/TAATGARAT-containing promoters. Journal of Biological Chemistry, 267, 24960–24965.
Lillycrop, K. A., Dent, C. L., Wheatley, S. C., Beech, M. N., Ninkina, N. N., Wood, J. N., et al. (1991). The octamer-binding protein Oct-2 represses HSV immediate-early genes in cell lines derived from latently infectable sensory neurons. Neuron, 7, 381–390.
Lillycrop, K. A., Estridge, J. K., & Latchman, D. S. (1994). Functional interaction between different isoforms of the Oct-2 transcription factor expressed in neuronal cells. Biochemistry Journal, 298(Pt 1), 245–248.
Liu, T. H., Beckman, J. S., Freeman, B. A., Hogan, E. L., & Hsu, C. Y. (1989). Polyethylene glycol-conjugated superoxide dismutase and catalase reduce ischemic brain injury. American Journal of Physiology, 256, H589–H593.
Liu, Y. Z., Lillycrop, K. A., & Latchman, D. S. (1995). Regulated splicing of the Oct-2 transcription factor RNA in neuronal cells. Neuroscience Letters, 183, 8–12.
Lobner, D. (2000). Comparison of the LDH and MTT assays for quantifying cell death: validity for neuronal apoptosis? Journal of Neuroscience Methods, 96, 147–152.
Mallolas, J., Hurtado, O., Castellanos, M., Blanco, M., Sobrino, T., Serena, J., et al. (2006). A polymorphism in the EAAT2 promoter is associated with higher glutamate concentrations and higher frequency of progressing stroke. Journal of Experimental Medicine, 203, 711–717.
Martinez, E. (2002). Multi-protein complexes in eukaryotic gene transcription. Plant Molecular Biology, 50, 925–947.
Mathisen, G. H., Fallgren, A. B., Strom, B. O., Boldingh Debernard, K. A., Mohebi, B. U., & Paulsen, R. E. (2011). Delayed translocation of NGFI-B/RXR in glutamate stimulated neurons allows late protection by 9-cis retinoic acid. Biochemical and Biophysical Research Communications, 414, 90–95.
Nadareishvili, Z., & Hallenbeck, J. (2003). Neuronal regeneration after stroke. The New England Journal of Medicine, 348, 2355–2356.
Naya, F. J., Wu, C., Richardson, J. A., Overbeek, P., & Olson, E. N. (1999). Transcriptional activity of MEF2 during mouse embryogenesis monitored with a MEF2-dependent transgene. Development, 126, 2045–2052.
Pan, L. N., Zhu, W., Li, C., Xu, X. L., Guo, L. J., & Lu, Q. (2012). Toll-like receptor 3 agonist Poly I: C protects against simulated cerebral ischemia in vitro and in vivo. Acta Pharmacologica Sinica, 33, 1246–1253.
Phillips, K., & Luisi, B. (2000). The virtuoso of versatility: POU proteins that flex to fit. Journal of Molecular Biology, 302, 1023–1039.
Pulliam, J. V., Xu, Z., Ford, G. D., Liu, C., Li, Y., Stovall, K. C., et al. (2013). Computational identification of conserved transcription factor binding sites upstream of genes induced in rat brain by transient focal ischemic stroke. Brain Research, 1495, 76–85.
Primer3. http://frodo.wi.mit.edu/primer3/. 22-7-2009c.
Qin, Z. H., Wang, Y., Nakai, M., & Chase, T. N. (1998). Nuclear factor-kappa B contributes to excitotoxin-induced apoptosis in rat striatum. Molecular Pharmacology, 53, 33–42.
Qin, J., Li, M. J., Wang, P., Zhang, M. Q., & Wang, J. (2011). ChIP-Array: combinatory analysis of ChIP-seq/chip and microarray gene expression data to discover direct/indirect targets of a transcription factor. Nucleic Acids Research, 39, W430–W436.
Raivich, G. (2011). Transcribing the path to neurological recovery-From early signals through transcription factors to downstream effectors of successful regeneration. Annals of Anatomy-Anatomischer Anzeiger, 193, 248–258.
Rodriguez-Mercado, R., Ford, G. D., Xu, Z., Kraiselburd, E. N., Martinez, M. I., Eterovic, V. A., et al. (2012). Acute neuronal injury and blood genomic profiles in a nonhuman primate model for ischemic stroke. Comparative Medicine, 62, 427–438.
Romera, C., Hurtado, O., Botella, S. H., Lizasoain, I., Cardenas, A., Fernandez-Tome, P., et al. (2004). In vitro ischemic tolerance involves upregulation of glutamate transport partly mediated by the TACE/ADAM17-tumor necrosis factor-alpha pathway. Journal of Neuroscience, 24, 1350–1357.
Sato, Y., Teruyama, K., Nakano, T., Oda, N., Abe, M., Tanaka, K., et al. (2001). Role of transcription factors in angiogenesis: Ets-1 promotes angiogenesis as well as endothelial apoptosis. Annals of the New York Academy of Sciences, 947, 117–123.
Scholer, H. R., Hatzopoulos, A. K., Balling, R., Suzuki, N., & Gruss, P. (1989). A family of octamer-specific proteins present during mouse embryogenesis: evidence for germline-specific expression of an Oct factor. EMBO Journal, 8, 2543–2550.
Schreiber, E., Harshman, K., Kemler, I., Malipiero, U., Schaffner, W., & Fontana, A. (1990). Astrocytes and glioblastoma cells express novel octamer-DNA binding proteins distinct from the ubiquitous Oct-1 and B cell type Oct-2 proteins. Nucleic Acids Research, 18, 5495–5503.
Shurin, G. V., Ferris, R. L., Tourkova, I. L., Perez, L., Lokshin, A., Balkir, L., et al. (2005). Loss of new chemokine CXCL14 in tumor tissue is associated with low infiltration by dendritic cells (DC), while restoration of human CXCL14 expression in tumor cells causes attraction of DC both in vitro and in vivo. The Journal of Immunology, 174, 5490–5498.
Singh, H., Sen, R., Baltimore, D., & Sharp, P. A. (1986). A nuclear factor that binds to a conserved sequence motif in transcriptional control elements of immunoglobulin genes. Nature, 319, 154–158.
Singh, N., Sharma, G., & Mishra, V. (2012). Hypoxia inducible factor-1: Its potential role in cerebral ischemia. Cellular and Molecular Neurobiology, 32, 491–507.
Sobrado, M., Lopez, M. G., Carceller, F., Garcia, A. G., & Roda, J. M. (2003). Combined nimodipine and citicoline reduce infarct size, attenuate apoptosis and increase bcl-2 expression after focal cerebral ischemia. Neuroscience, 118, 107–113.
Sobrado, M., Pereira, M. P., Ballesteros, I., Hurtado, O., Fernandez-Lopez, D., Pradillo, J. M., et al. (2009). Synthesis of lipoxin A4 by 5-lipoxygenase mediates PPARgamma-dependent, neuroprotective effects of rosiglitazone in experimental stroke. Journal of Neuroscience, 29, 3875–3884.
Sobrado, M., Delgado, M., Fernandez-Valle, E., Garcia–Garcia, L., Torres, M., Sanchez-Prieto, J., et al. (2011). Longitudinal studies of ischemic penumbra by using 18F-FDG PET and MRI techniques in permanent and transient focal cerebral ischemia in rats. Neuroimage, 57, 45–54.
Staudt, L. M., Clerc, R. G., Singh, H., LeBowitz, J. H., Sharp, P. A., & Baltimore, D. (1988). Cloning of a lymphoid-specific cDNA encoding a protein binding the regulatory octamer DNA motif. Science, 241, 577–580.
Stoykova, A. S., Sterrer, S., Erselius, J. R., Hatzopoulos, A. K., & Gruss, P. (1992). Mini-Oct and Oct-2c: two novel, functionally diverse murine Oct-2 gene products are differentially expressed in the CNS. Neuron, 8, 541–558.
Tencheva, T., & Panov, I. R. (2008). Intracerebral development of transplanted glioblastoma C6 cells in rats after preliminary exposure to neuropeptides and an MAPK inhibitor. Neuroscience and Behavioral Physiology, 38, 913–916.
Thoresen, M., Liu, X., Jary, S., Brown, E., Sabir, H., Stone, J., et al. (2012). Lactate dehydrogenase in hypothermia-treated newborn infants with hypoxic-ischaemic encephalopathy. Acta Paediatrica, 101, 1038–1044.
Wang, Y. D., Cai, N., Wu, X. L., Cao, H. Z., Xie, L. L., & Zheng, P. S. (2013). OCT4 promotes tumorigenesis and inhibits apoptosis of cervical cancer cells by miR-125b/BAK1 pathway. Cell Death & Disease, 4, e760.
Wirth, T., Priess, A., Annweiler, A., Zwilling, S., & Oeler, B. (1991). Multiple Oct2 isoforms are generated by alternative splicing. Nucleic Acids Research, 19, 43–51.
Wood, J. N., Lillycrop, K. A., Dent, C. L., Ninkina, N. N., Beech, M. M., Willoughby, J. J., et al. (1992). Regulation of expression of the neuronal POU protein Oct-2 by nerve growth factor. Journal of Biological Chemistry, 267, 17787–17791.
Xie, R., Li, X., Ling, Y., Shen, C., Wu, X., Xu, W., et al. (2012). Alpha-lipoic acid pre- and post-treatments provide protection against in vitro ischemia-reperfusion injury in cerebral endothelial cells via Akt/mTOR signaling. Brain Research, 1482, 81–90.
Xu, Z., Ford, G. D., Croslan, D. R., Jiang, J., Gates, A., Allen, R., et al. (2005). Neuroprotection by neuregulin-1 following focal stroke is associated with the attenuation of ischemia-induced pro-inflammatory and stress gene expression. Neurobiology of Diseases, 19, 461–470.
Zhang, C., Wu, H., Zhu, X., Wang, Y., & Guo, J. (2011). Role of transcription factors in neurogenesis after cerebral ischemia. Reviews in the Neurosciences, 22, 457–465.
Zhang, Y., Huang, S., Wang, B., Sun, B., Li, W., Lu, X., et al. (2012). Atorvastatin and whisker stimulation synergistically enhance angiogenesis in the barrel cortex of rats following focal ischemia. Neuroscience Letters, 525, 135–139.
Acknowledgments
This work was partially supported by the Centre d’Innovació i Desenvolupament Empresarial (CIDEM) of the Generalitat de Catalunya (Grant No. RDITSCON07-1-0006), Grupo Ferrer Internacional SA, Spanish Ministry of Science and Innovation and the European Regional Development Fund (ERDF) (PROFIT Grant No. CIT 090000-20008-11), Institut de Salud Carlos III (ISCIII) Grant Nos. FIS-PI070322, and ISCIII retics-RENEVAS-RD06/0026/0005 and RD07/0026/2002. Finally, thanks to Andrew Hughes for the linguistic revision of the manuscript.
Conflict of interest
The authors (Susanna Camós, Carme Gubern, Mónica Sobrado, Rocío Rodríguez, Víctor G Romera, María Ángeles Moro, Ignacio Lizasoain, Joaquín Serena, Judith Mallolas, and Mar Castellanos) declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Senior authors: Judith Mallolas and Mar Castellanos. Corresponding author: Judith Mallolas.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Camós, S., Gubern, C., Sobrado, M. et al. Oct-2 Transcription Factor Binding Activity and Expression Up-Regulation in Rat Cerebral Ischaemia is Associated with a Diminution of Neuronal Damage In Vitro. Neuromol Med 16, 332–349 (2014). https://doi.org/10.1007/s12017-013-8279-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-013-8279-1