Abstract
The amyloid cascade hypothesis on the pathogenesis of Alzheimer’s disease (AD) states that amyloid β (Aβ) accumulation in the brain is a key factor that initiates the neurodegenerative process. Aβ is generated from amyloid precursor protein (APP) through sequential cleavages by BACE1 (the major β-secretase in the brain) and γ-secretase. The purpose of this study was to characterize APP metabolism in vivo in AD patients versus cognitively healthy subjects by examining alterations in cerebrospinal fluid (CSF) biomarkers. We measured BACE1 activity and concentrations of α- and β-cleaved soluble APP (sAPPα and sAPPβ, respectively) and Aβ40 in CSF, biomarkers that all reflect the metabolism of APP, in 75 AD patients and 65 cognitively healthy controls. These analytes were also applied in a multivariate model to determine whether they provided any added diagnostic value to the core CSF AD biomarkers Aβ42, T-tau, and P-tau. We found no significant differences in BACE1 activity or sAPPα, sAPPβ, and Aβ40 concentrations between AD patients and controls. A multivariate model created with all analytes did not improve the separation of AD patients from controls compared with using the core AD biomarkers alone, highlighting the strong diagnostic performance of Aβ42, T-tau, and P-tau for AD. However, AD patients in advanced clinical stage, as determined by low MMSE score (≤20), had lower BACE1 activity and sAPPα, sAPPβ, and Aβ40 concentrations than patients with higher MMSE score, suggesting that these markers may be related to the severity of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most common dementing illness (Blennow et al. 2006). It is characterized by certain histopathological changes in the brain including extracellular deposits of amyloid β (Aβ) and intracellular tangles of hyperphosphorylated tau (P-tau) protein. These processes may be monitored by cerebrospinal fluid (CSF) biomarkers. Established CSF biomarkers for AD include the total concentration of tau protein (T-tau), correlated with cortical axonal degeneration; the concentration of P-tau, correlated with tangle pathology; and the concentration of the 42-amino acid—long isoform of Aβ (Aβ42), inversely correlated with plaque pathology (Blennow et al. 2010). Several studies show that a biomarker profile with elevated CSF concentrations of T-tau and P-tau accompanied by a reduced concentration of Aβ42 identifies dementia or mild cognitive impairment (MCI) due to AD with 85–95% sensitivity and specificity (Blennow et al. 2010).
Abnormal metabolism of Aβ is considered a key factor in the development of AD. Aβ is generated from amyloid precursor protein (APP) after sequential cleavages by β-secretase, which liberates the N-terminal soluble ectodomain APPβ (sAPPβ), and γ-secretase, which cuts at the C-terminal part of the Aβ peptide. On a molecular level, it is not clear exactly how Aβ contributes to the pathogenesis of AD, but oligomeric forms of Aβ42 have neurotoxic properties and inhibit long-term potentiation in experimental models (Shankar and Walsh 2009). The main Aβ isoform generated by β- and γ-secretase cleavages is Aβ40, which is less prone to aggregation and fibril formation than Aβ42. Most APP molecules are cleaved by α-secretase, which prohibits Aβ formation and releases sAPPα, which may have neuroprotective functions (Mattson et al. 1997).
The major β-secretase in the brain is the β-site APP-cleaving enzyme 1 (BACE1). Due to its pivotal role in Aβ production, BACE1 is now tested as an AD drug target in clinical trials (May et al. 2011). Increased BACE1 expression and enzymatic activity have been detected in postmortem AD brain samples (Fukumoto et al. 2002; Holsinger et al. 2002; Yang et al. 2003; Johnston et al. 2005). BACE1 may also be cut, releasing an enzymatically active BACE1 fragment into the extracellular space. Elevated CSF BACE1 activity and protein concentrations have been found in some studies of patients with dementia or MCI due to AD (Holsinger et al. 2004, 2006; Verheijen et al. 2006; Zetterberg et al. 2008). One large study found elevated BACE1 activity among MCI but not AD patients (Zhong et al. 2007). Some studies have found elevated CSF concentrations of sAPPα and sAPPβ in AD patients (Lewczuk et al. 2010; Perneczky et al. 2011), but other studies have failed to replicate this (Zetterberg et al. 2008; Johansson et al. 2011). More research on these biomarkers is needed to clarify the discrepancies.
The purpose of this study was to characterize alterations of APP metabolism in AD in vivo in humans by measuring CSF BACE1 activity and concentrations of sAPPα, sAPPβ, and Aβ40 in AD patients and cognitively healthy controls. In particular, we wanted to test whether these biomarkers may provide any added value to the established CSF biomarkers T-tau, P-tau, and Aβ42 in the diagnosis of AD.
Methods
Study Population
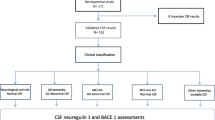
The study population consisted of 75 subjects with probable AD and 65 cognitively healthy control subjects, recruited from 3 specialized and coordinated memory clinics in Sweden within the Swedish Brain Power network. Demographics and biochemical characteristics are given in Table 1.
All subjects were examined clinically, including neuropsychological evaluations with mini-mental state examination (MMSE) (Folstein et al. 1975). They also underwent imaging of the brain with computed tomography and CSF collection. Controls had no history of dementia, did not show any signs of other psychiatric illnesses, and were followed up clinically for 3 years to exclude development of any neurodegenerative disease. For AD diagnosis, we used the criteria for dementia according to the Diagnostic and Statistical Manual of Mental Disorders (Third Edition Revised) (DSM-IIIR) (American Psychiatric Association 1987) and the criteria for probable AD according to the National Institute of Neurological and Communicative Disorders and Stroke-Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) (McKhann et al. 1984).
Disease severity was evaluated using MMSE scores. A score <10 indicated severe dementia, 10–20 indicated moderate dementia and >20 indicated mild dementia, according to earlier proposed cutoffs (Mungas 1991).
CSF collection was conducted following standardized operating procedures (Blennow et al. 2010). Lumbar puncture was performed in the L3-L4 or L4-L5 interspace. The first 12 mL of CSF was collected in a polypropylene tube and was centrifuged at 2000×g at 4°C for 10 min. The supernatant was pipetted off, gently mixed to avoid possible gradient effects, and aliquoted in polypropylene tubes that were stored at −80°C pending biochemical analyses, without being thawed and refrozen.
Laboratory Methods
CSF BACE1 activity was measured using a previously described solution-based assay (Zetterberg et al. 2008). In brief, 15 μL of CSF was first diluted to 60 μL with running buffer (50 mM sodium acetate, 15 mM EDTA, 0.2% 3-[(3-cholamidopropyl) dimethylammonio]-1-propanesulfonic acid (CHAPS), 1 mM deferoxamine mesylate, 10 μM pepstatin A, and 0.01% bovine serum albumin at pH 4.5), followed by incubation on a shaker for 30 min. A double volume (120 μL) of the biotinylated 15 mer optimized BACE1 substrate (biotin-KTEEISEVNFEVEFR) in running buffer was added to a final concentration of 133 nM, and the proteolytic reaction was allowed to proceed for 3 h at 37°C. The reaction was stopped by addition of 60 μL of 1 M Tris (pH 8.0), and 200 μL of the mixture was transferred to a streptavidin-coated 96-well plate (Pierce, Rockford, Illinois), where it was incubated for 17 h at 4°C. Unbound material was removed by successive washes using a combined solution of phosphate-buffered saline with 0.1% polysorbate 20 (Tween 20; Sigma Chemical Co, St Louis, Missouri, USA) (PBST). The BACE1 cleavage product was detected by using a rabbit polyclonal NF neoepitope-specific antibody (Shi et al. 2005) in combination with alkaline phosphate-conjugated goat antirabbit IgG. Each antibody was incubated for 1 h, with intermediate and final PBST washing steps. After addition of 100 μL of chemiluminescence substrate (CDP-star; PerkinElmer, Upplands Väsby, Sweden), the plate was immediately inserted into a device (SpectraMax Gemini XPS; Molecular Devices, Sunnyvale, California) for integrated luminescence for 30 min. The extent of BACE1 activity was quantified using recombinant BACE1 standards. CSF BACE1 activity was completely inhibited by statin-val- and BACE1-specific inhibitors, verifying the specificity of the assay (Zetterberg et al. 2008).
CSF concentrations of sAPPα and sAPPβ were determined using the MSD sAPPα/sAPPβ Multiplex Assay according to the instructions by the manufacturer (Meso Scale Discovery, Gaithersburg, Maryland, USA). This assay employs the 6E10 antibody to capture sAPPα and a neoepitope-specific antibody to capture sAPPβ. Both isoforms are detected by the SULFO-TAG-labeled anti-APP antibody p2-1. CSF concentration of AβX-40 (called Aβ40 in this paper) was determined using the MSD MULTI-ARRAY Human Aβ40 Ultra-Sensitive kit that uses 6E10 as capture antibody and an end-specific SULFO-TAG-labeled anti-Aβ40 antibody for detection.
We also analyzed the established CSF AD biomarkers Aβ1-42 (called Aβ42 in this paper), T-tau, and P-tau (“core” biomarkers). Aβ42 was measured using a sandwich enzyme-linked immunosorbent assay (ELISA) (INNOTEST β-amyloid[1-42], Innogenetics, Ghent, Belgium), specifically constructed to measure Aβ containing both the 1st and 42nd amino acids, as previously described (Andreasen et al. 1999). T-tau was measured using a sandwich ELISA (INNOTEST hTAU-Ag, Innogenetics) specifically constructed to measure all tau isoforms irrespective of phosphorylation status, as previously described (Blennow et al. 1995). Tau phosphorylated at threonine 181 (P-tau) was measured using a sandwich ELISA (INNOTEST Phospho-Tau[181P], Innogenetics), as previously described (Vanmechelen et al. 2000). Note that the absolute concentrations of CSF biomarkers differ across assays and analytical techniques, and the INNOTEST ELISAs generally report higher concentrations for Aβ42, T-tau, and P-tau than, for example, the xMAP Luminex assay INNO-BIA AlzBio3 (Innogenetics) (Olsson et al. 2005), although the diagnostic accuracy for AD is stable across these platforms (Hoistad et al. 2005; Fagan et al. 2011).
All biochemical analyses were performed by experienced and board-certified laboratory technicians who were blinded to the clinical diagnoses and other clinical information. Intra-assay coefficients of variation were below 10% for all analytes.
Statistical Analysis
The distribution of quantitative data was significantly skewed for several of the studied parameters according to the D’Agostino and Pearson omnibus normality test. Therefore, these data were analyzed with the Kruskal–Wallis test using Dunn’s post hoc test for multiple comparisons and Mann–Whitney U test for univariate pairwise comparisons of groups. For normally distributed data, the one-way ANOVA using Bonferroni’s post hoc test was applied for multiple comparisons and the t test for pairwise group comparisons. The Spearman rank and Pearson correlation coefficient tests were used for testing correlations. Statistical significance was determined at P < 0.05. Multivariate discriminant analysis (DA) using the orthogonal projection to latent structures (OPLS) algorithm (Bylesjö et al. 2006) was applied to examine whether the pattern of biomarkers could differentiate AD patients from controls and patients with mild AD from patients with moderate-to-severe AD. Score vectors representing combinations of biomarkers were constructed, and their diagnostic accuracies were compared using receiver-operating characteristics (ROC) statistics.
Results
Univariate Analyses
There were no significant differences in BACE1 activities or concentrations of sAPPα, sAPPβ, and Aβ40 between the AD and control groups (Fig. 1). However, a tendency to higher levels of BACE1 activity was noted in AD patients. As expected, AD patients had significantly higher concentrations of P-tau and T-tau and lower concentrations of Aβ42 than controls (Table 1). Regarding disease severity, three AD patients had MMSE score 30 and one had MMSE score 0. Exclusion of these outlying individuals did not change any results significantly (data not shown).
Multivariate Model
The pattern of analytes differed between the AD and control groups (Fig. 2), but the additional biomarkers sAPPα, sAPPβ, Aβ40, and BACE1 had a very small contribution to the discrimination compared with the core CSF AD biomarkers. The ROC statistics showed that the combination of the core biomarkers Aβ42, T-tau, and P-tau was superior to anyone of these three biomarkers alone in terms of area under the curve (AUC). Adding sAPPα, sAPPβ, Aβ40, and BACE1 to the model did not increase the AUC (Fig. 3).
Multivariate analysis scatter plot (a) and variable importance in projection (VIP) plot (b) for the Alzheimer’s disease (AD) and control groups. Aβ42, T-tau, and P-tau contributed most to the separation of AD patients and controls. Red lines in panel A represent the median. Aβ40 amyloid β 1-40, Aβ42 amyloid β 1-42, BACE1 β-site APP-cleaving enzyme 1 activity, P-tau hyperphosphorylated tau, sAPP soluble amyloid precursor protein, and T-tau total tau (Color figure online)
Receiver-operating characteristic (ROC) curves for Aβ42, T-tau, and P-tau. The black line shows the ROC curve for the combined use of the three core biomarkers. The area under the curve (AUC) for the combination of these three biomarkers did not differ significantly from when all the biomarkers measured in this study were included (AUC = 0.95). Aβ42 amyloid β 1-42, P-tau hyperphosphorylated tau, and T-tau total tau (Color figure online)
Correlations Between Biomarkers
There were strong correlations between sAPPα and sAPPβ in both diagnostic groups, and BACE1 correlated slightly with sAPPα, sAPPβ, and Aβ40 (Table 2). There were positive correlations between T-tau and all other biomarkers in controls and between T-tau and Aβ40, BACE1, and P-tau in the AD group. Aβ42 correlated with all biomarkers except sAPPβ in controls and with no biomarkers in the AD group. P-tau correlated (omitting the already mentioned correlations) with Aβ40 and BACE1 in controls and with sAPPα, sAPPβ, and Aβ40 in the AD group.
The AD patients were significantly older than the controls (Table 1, P < 0.001). To study the influence of age on biomarkers, we tested correlations between biomarkers and age within the diagnostic groups. No such correlations were seen, except for T-tau versus age in controls (Table 2).
Biomarkers and MMSE Scores
CSF BACE1 activity and concentrations of P-tau, sAPPα, sAPPβ, and Aβ40 all correlated with MMSE scores in AD patients (Table 2). In line with this, stratification of patients in mild AD and moderate-to-severe AD based on an MMSE cut-point score of 20 revealed significant differences in biomarker concentrations depending on the disease severity. Patients with moderate-to-severe AD had lower sAPPα, sAPPβ, and Aβ40 concentrations and BACE1 activity than mild AD patients and controls (Fig. 4). Patients with mild AD had higher P-tau concentrations than moderate-to-severe patients (Fig. 5). T-tau and Aβ42 concentrations were similar in the two AD groups.
Scatter plots of amyloid β-related biomarkers concentrations in mild (MMSE > 20) and moderate-to-severe (MMSE ≤ 20) Alzheimer’s disease (AD) patients and controls. Patients with moderate-to-severe AD had significantly lower CSF concentrations of sAPPα, sAPPβ, Aβ40, and BACE1 than patients with mild AD and controls. Aβ40 amyloid β 1-40, BACE1 β-site APP-cleaving enzyme 1 activity, MMSE mini-ental state examination, and sAPP soluble amyloid precursor protein
Scatter plots of core biomarker concentrations in mild (MMSE > 20) and moderate-to-severe (MMSE ≤ 20) Alzheimer’s disease (AD) patients and controls. All patients with AD had higher concentrations of T-tau and P-tau and lower concentrations of Aβ42 than controls. Patients with mild AD had significantly higher concentrations of P-tau than patients with moderate-to-severe AD. Aβ42 amyloid β 1-42, MMSE mini-mental state examination, P-tau hyperphosphorylated tau, and T-tau total tau
A multivariate model containing all biomarkers successfully separated patients with mild AD from patients with moderate-to-severe AD, although with some overlap (Fig. 6A). sAPPα, sAPPβ, Aβ40, and BACE1 had the most impact on the group discrimination, with P-tau having a slightly smaller, but still significant, contribution (Fig. 6B).
Multivariate analysis scatter plot (A) and variable importance in projection (VIP) plot (B) for mild (MMSE > 20) and moderate-to-severe (MMSE ≤ 20) Alzheimer’s disease (AD) patients. sAPPα, sAPPβ, Aβ40, and BACE1 contributed most to the separation of patients with mild and moderate-to-severe AD. Red lines in panel A represent the median. Aβ40 amyloid β 1-40, Aβ42 amyloid β 1-42, BACE1 β-site APP-cleaving enzyme 1 activity, MMSE mini-mental state examination, P-tau hyperphosphorylated tau, sAPP soluble amyloid precursor protein, and T-tau total tau (Color figure online)
Discussion
Here, we show that CSF biomarkers may distinguish different disease stages of AD. It is well known that CSF T-tau, P-tau, and Aβ42 can be useful in making an early AD diagnosis (Blennow et al. 2010), but data on the temporal dynamics of biomarkers are still limited (Jack et al. 2010). The amyloid cascade hypothesis states that Aβ accumulation in the brain is a key factor in the AD pathogenesis. The biomarkers in this study all reflect APP and Aβ metabolism. We did not detect any significant differences between AD patients and controls in CSF BACE1 activity or concentrations of sAPPα, sAPPβ, and Aβ40, and no added diagnostic value of these biomarkers compared with the core AD biomarkers Aβ42, T-tau, and P-tau in a multivariate analysis, arguing against them for plain AD diagnosis. However, there were significant differences in levels of BACE1 activity and concentrations of sAPPα, sAPPβ, Aβ40, and P-tau when comparing patients with mild and moderate-to-severe AD, with the latter group displaying the lowest levels. These data comport with recent findings from our laboratory, where concentrations of Aβ40 decreased over time in AD patients followed with serial CSF samplings over 4 years (Mattsson et al., manuscript in preparation). Note that such changes are unlikely to be detected with shorter follow-up (Blennow et al. 2007). Similarly, we have previously reported that patients in severe clinical stages of the neurodegenerative disease Niemann-Pick type C have lower concentrations of Aβ42, Aβ40, Aβ38, and sAPPβ than patients with less severe disease burden (Mattsson et al. 2011). Since neuronal Aβ release appears to depend on synaptic activity (Cirrito et al. 2008) such reductions might be related to loss of functional synapses or neurons with disease progression. We propose the hypothesis that CSF concentrations of distinct amyloid-related biomarkers, including sAPPα, sAPPβ, and Aβ40 might function as general markers of disease progression in patients with neurodegenerative diseases. These biomarkers could offer a way to monitor long-term effects of disease-modifying drugs in clinical trials, where a longitudinal stability in biomarker concentrations following drug administration might indicate successful inhibition of disease progression.
Comparing our data with earlier studies, it should be noted that previously described elevations of CSF BACE1 in AD patients have been reported in small study populations (Holsinger et al. 2004, 2006; Verheijen et al. 2006) or have been minor with large overlaps between the diagnostic groups (Zetterberg et al. 2008). One of the largest previous studies failed to report differences in CSF BACE1 activity between AD patients and controls but found significantly higher BACE1 activity in MCI patients compared with controls (Zhong et al. 2007). This is in line with our results and suggests that BACE1 activity may be elevated in early-stage AD. It should be noted though that comparisons between studies might be complicated by the use of different BACE1 assays in different studies.
The lack of difference between AD patients and controls in concentrations of sAPPα, sAPPβ, and Aβ40 is in line with previous results from our laboratory (Zetterberg et al. 2008; Johansson et al. 2011), but other studies have shown elevated sAPPβ (Perneczky et al. 2011) and/or sAPPα (Lewczuk et al. 2010; Perneczky et al. 2011) concentrations in patients with AD or MCI who later progressed to AD. However, these studies did not include cognitively healthy controls. CSF sAPP concentrations are reduced in cerebrovascular disease (Selnes et al. 2010), inflammatory conditions (Gisslen et al. 2009; Mattsson et al. 2009, 2010), and amyotrophic lateral sclerosis (Steinacker et al. 2011). It is possible that at least part of the associations described in earlier studies (Lewczuk et al. 2010; Perneczky et al. 2011) may have been driven by reductions in sAPP concentrations in the non-AD disease groups. In the present study, the heterogeneity in the disease severity among the AD patients averaged out disease stage-dependent differences in biomarker concentrations, showing that disease severity may be a confounding factor, which may contribute to differences among studies.
A limitation of our study is that MMSE is a rather crude measure of disease severity. Additional tests, such as ADAS-cog (Alzheimer’s Disease Assessment Scale—cognitive subscale) or CDR (Clinical Dementia Rating) were not performed in all included subjects, hindering us from analyzing them in relation to biomarkers.
We confirmed previously described correlations between sAPPα and sAPPβ (Zetterberg et al. 2008; Gisslen et al. 2009; Lewczuk et al. 2010; Selnes et al. 2010) and between CSF BACE1 activity and sAPPα, sAPPβ, and Aβ40 (Zetterberg et al. 2008; Mattsson et al. 2009). These expected correlations underscore the validity of the biomarker results and the biological relevance of CSF BACE1 activity in relation to APP processing within the central nervous system. There were differences in the correlations of Aβ42 with sAPPα, Aβ40, and BACE1 when comparing AD patients with controls, which can be explained by a lower CSF Aβ42 concentration in the AD group. The AD patients in this study expressed a characteristic pattern of established AD biomarkers, with low Aβ42 and high P-tau and T-tau concentrations, which strengthens the conclusions drawn from the other analyses.
In summary, we found no significant differences in CSF BACE1 activity or sAPPα, sAPPβ, and Aβ40 concentrations between AD patients and controls, and no added diagnostic value from these biomarkers compared with the core biomarkers Aβ42, T-tau, and P-tau. However, we found that the biomarker concentrations differed among AD patients with mild and moderate-to-severe dementia, suggesting that they may be valuable as markers of disease progression.
References
American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders: DSM-III-R (3rd ed.). Washington, DC: American Psychiatric Association.
Andreasen, N., Hesse, C., Davidsson, P., Minthon, L., Wallin, A., Winblad, B., et al. (1999). Cerebrospinal fluid beta-amyloid(1–42) in Alzheimer disease: Differences between early- and late-onset Alzheimer disease and stability during the course of disease. Archives of Neurology, 56, 673–680.
Blennow, K., de Leon, M. J., & Zetterberg, H. (2006). Alzheimer’s disease. Lancet, 368, 387–403. doi:10.1016/S0140-6736(06)69113-7.
Blennow, K., Hampel, H., Weiner, M., & Zetterberg, H. (2010). Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nature Reviews Neurology, 6, 131–144.
Blennow, K., Wallin, A., Agren, H., Spenger, C., Siegfried, J., & Vanmechelen, E. (1995). Tau protein in cerebrospinal fluid: A biochemical marker for axonal degeneration in Alzheimer disease? Molecular and Chemical Neuropathology, 26, 231–245.
Blennow, K., Zetterberg, H., Minthon, L., Lannfelt, L., Strid, S., Annas, P., et al. (2007). Longitudinal stability of CSF biomarkers in Alzheimer’s disease. Neuroscience Letters, 419, 18–22.
Bylesjö, M., Rantalainen, M., Cloarec, O., Nicholson, J. K., Holmes, E. A., & Trygg, J. (2006). OPLS discriminant analysis: Combining the strengths of PLS-DA and SIMCA classification. Journal of Chemometrics, 20, 341–351.
Cirrito, J. R., Kang, J. E., Lee, J., Stewart, F. R., Verges, D. K., Silverio, L. M., et al. (2008). Endocytosis is required for synaptic activity-dependent release of amyloid-beta in vivo. Neuron, 58, 42–51.
Fagan, A. M., Shaw, L. M., Xiong, C., Vanderstichele, H., Mintun, M. A., Trojanowski, J. Q., et al. (2011). Comparison of analytical platforms for cerebrospinal fluid measures of beta-amyloid 1–42, total tau, and p-tau181 for identifying Alzheimer disease amyloid plaque pathology. Archives of Neurology, 68, 1137–1144.
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198.
Fukumoto, H., Cheung, B. S., Hyman, B. T., & Irizarry, M. C. (2002). Beta-secretase protein and activity are increased in the neocortex in Alzheimer disease. Archives of Neurology, 59, 1381–1389.
Gisslén, M., Krut, J., Andreasson, U., Blennow, K., Cinque, P., Brew, B. J., et al. (2009). Amyloid and tau cerebrospinal fluid biomarkers in HIV infection. BMC Neurology, 9, 63. doi:10.1186/1471-2377-9-63.
Höistad, M., Samskog, J., Jacobsen, K. X., Olsson, A., Hansson, H. A., Brodin, E., et al. (2005). Detection of beta-endorphin in the cerebrospinal fluid after intrastriatal microinjection into the rat brain. Brain Research, 1041, 167–180.
Holsinger, R. M., Lee, J. S., Boyd, A., Masters, C. L., & Collins, S. J. (2006). CSF BACE1 activity is increased in CJD and Alzheimer disease versus [corrected] other dementias. Neurology, 67, 710–712.
Holsinger, R. M., McLean, C. A., Beyreuther, K., Masters, C. L., & Evin, G. (2002). Increased expression of the amyloid precursor beta-secretase in Alzheimer’s disease. Annals of Neurology, 51, 783–786.
Holsinger, R. M., McLean, C. A., Collins, S. J., Masters, C. L., & Evin, G. (2004). Increased beta-secretase activity in cerebrospinal fluid of Alzheimer’s disease subjects. Annals of Neurology, 55, 898–899.
Jack, C. R., Jr, Knopman, D. S., Jagust, W. J., Shaw, L. M., Aisen, P. S., Weiner, M. W., et al. (2010). Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurology, 9, 119–128.
Johansson, P., Mattsson, N., Hansson, O., Wallin, A., Johansson, J. O., Andreasson, U., et al. (2011). Cerebrospinal fluid biomarkers for Alzheimer’s disease: Diagnostic performance in a homogeneous mono-center population. Journal of Alzheimers Disease, 24, 537–546.
Johnston, J. A., Liu, W. W., Todd, S. A., Coulson, D. T., Murphy, S., Irvine, G. B., et al. (2005). Expression and activity of beta-site amyloid precursor protein cleaving enzyme in Alzheimer’s disease. Biochemical Society Transactions, 33, 1096–1100.
Lewczuk, P., Kamrowski-Kruck, H., Peters, O., Heuser, I., Jessen, F., Popp, J., et al. (2010). Soluble amyloid precursor proteins in the cerebrospinal fluid as novel potential biomarkers of Alzheimer’s disease: A multicenter study. Molecular Psychiatry, 15, 138–145.
Mattson, M. P., Barger, S. W., Furukawa, K., Bruce, A. J., Wyss-Coray, T., Mark, R. J., et al. (1997). Cellular signaling roles of TGF beta, TNF alpha and beta APP in brain injury responses and Alzheimer’s disease. Brain Research Reviews, 23, 47–61.
Mattsson, N., Axelsson, M., Haghighi, S., Malmeström, C., Wu, G., Anckarsäter, R., et al. (2009). Reduced cerebrospinal fluid BACE1 activity in multiple sclerosis. Multiple Sclerosis, 15, 448–454.
Mattsson, N., Bremell, D., Anckarsäter, R., Blennow, K., Anckarsäter, H., Zetterberg, H., et al. (2010). Neuroinflammation in Lyme neuroborreliosis affects amyloid metabolism. BMC Neurology, 10, 51. doi:10.1186/1471-2377-10-51.
Mattsson, N., Zetterberg, H., Bianconi, S., Yanjanin, N. M., Fu, R., Månsson, J. E., et al. (2011). Gamma-secretase-dependent amyloid-beta is increased in Niemann-Pick type C: A cross-sectional study. Neurology, 76, 366–372.
May, P. C., Dean, R. A., Lowe, S. L., Martenyi, F., Sheehan, S. M., Boggs, L. N., et al. (2011). Robust central reduction of amyloid-beta in humans with an orally available, non-peptidic beta-secretase inhibitor. Journal of Neuroscience, 31, 16507–16516.
McKhann, G., Drachman, D., Folstein, M., Katzman, R., Price, D., & Stadlan, E. M. (1984). Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology, 34, 939–944.
Mungas, D. (1991). In-office mental status testing: A practical guide. Geriatrics, 46, 54–58.
Olsson, A., Vanderstichele, H., Andreasen, N., De Meyer, G., Wallin, A., Holmberg, B., et al. (2005). Simultaneous measurement of beta-amyloid(1–42), total tau, and phosphorylated tau (Thr181) in cerebrospinal fluid by the xMAP technology. Clinical Chemistry, 51, 336–345.
Perneczky, R., Tsolakidou, A., Arnold, A., Diehl-Schmid, J., Grimmer, T., Förstl, H., et al. (2011). CSF soluble amyloid precursor proteins in the diagnosis of incipient Alzheimer disease. Neurology, 77, 35–38.
Selnes, P., Blennow, K., Zetterberg, H., Grambaite, R., Rosengren, L., Johnsen, L., et al. (2010). Effects of cerebrovascular disease on amyloid precursor protein metabolites in cerebrospinal fluid. Cerebrospinal Fluid Research, 7, 10. doi:10.1186/1743-8454-7-10.
Shankar, G. M., & Walsh, D. M. (2009). Alzheimer’s disease: Synaptic dysfunction and Abeta. Molecular Neurodegeneration, 4, 48. doi:10.1186/1750-1326-4-48.
Shi, X. P., Tugusheva, K., Bruce, J. E., Lucka, A., Chen-Dodson, E., Hu, B., et al. (2005). Novel mutations introduced at the beta-site of amyloid beta protein precursor enhance the production of amyloid beta peptide by BACE1 in vitro and in cells. Journal of Alzheimers Disease, 7, 139–148.
Steinacker, P., Fang, L., Kuhle, J., Petzold, A., Tumani, H., Ludolph, A. C., et al. (2011). Soluble beta-amyloid precursor protein is related to disease progression in amyotrophic lateral sclerosis. PLoS One, 6, e23600. doi:10.1371/journal.pone.0023600.
Vanmechelen, E., Vanderstichele, H., Davidsson, P., Van Kerschaver, E., Van Der Perre, B., Sjögren, M., et al. (2000). Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: a sandwich ELISA with a synthetic phosphopeptide for standardization. Neuroscience Letters, 285, 49–52.
Verheijen, J. H., Huisman, L. G., van Lent, N., Neumann, U., Paganetti, P., Hack, C. E., et al. (2006). Detection of a soluble form of BACE-1 in human cerebrospinal fluid by a sensitive activity assay. Clinical Chemistry, 52, 1168–1174.
Yang, L. B., Lindholm, K., Yan, R., Citron, M., Xia, W., Yang, X. L., et al. (2003). Elevated beta-secretase expression and enzymatic activity detected in sporadic Alzheimer disease. Nature Medicine, 9, 3–4.
Zetterberg, H., Andreasson, U., Hansson, O., Wu, G., Sankaranarayanan, S., Andersson, M. E., et al. (2008). Elevated cerebrospinal fluid BACE1 activity in incipient Alzheimer disease. Archives of Neurology, 65, 1102–1107.
Zhong, Z., Ewers, M., Teipel, S., Bürger, K., Wallin, A., Blennow, K., et al. (2007). Levels of beta-secretase (BACE1) in cerebrospinal fluid as a predictor of risk in mild cognitive impairment. Archives of General Psychiatry, 64, 718–726.
Acknowledgments
We thank Åsa Källén, Monica Christiansson, Sara Hullberg, and Dzemila Secic for excellent technical assistance. This study was supported by grants from the Swedish Research Council, the Söderberg Foundation, Alzheimer’s Association, Swedish Brain Power, Swedish State Support for Clinical Research, the Lundbeck Foundation, Stiftelsen Psykiatriska Forskningsfonden, Stiftelsen Gamla Tjänarinnor, Uppsala Universitets Medicinska Fakultets stiftelse för psykiatrisk och neurologisk forskning, Alzheimerfonden, Hjärnfonden, the Göteborg Medical Society, Thuréus stiftelse, Pfannenstills stiftelse, and Demensfonden.
Conflict of interest
None reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosén, C., Andreasson, U., Mattsson, N. et al. Cerebrospinal Fluid Profiles of Amyloid β-Related Biomarkers in Alzheimer’s Disease. Neuromol Med 14, 65–73 (2012). https://doi.org/10.1007/s12017-012-8171-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12017-012-8171-4