Abstract
Posttranslational modifications (PTMs) are defined as covalent modifications occurring in a specific protein amino acid in a time- and signal-dependent manner. Under physiological conditions, proteins are posttranslationally modified to carry out a large number of cellular events from cell signaling to DNA replication. However, an absence, deficiency, or excess in PTMs of a given protein can evolve into a target to trigger autoimmunity, since PTMs arise in the periphery and may not occur in the thymus; hence, proteins with PTMs never tolerize developing thymocytes. Consequently, when PTMs arise during cellular responses, such as inflammation, these modified self-antigens can be taken up and processed by the antigen-presenting cells (APCs). Autoreactive T cells, which recognize peptides presented by APCs, can then infiltrate into host tissue where the modified antigen serves to amplify the autoimmune response, eventually leading to autoimmune pathology. Furthermore, a PTM occurring in an amino acid residue can induce changes in the net charge of the protein, leading to conformational modifications in the tertiary and quaternary structure of the protein, especially interaction with human leukocyte antigen (HLA) molecules. Molecular mimicry (MM) was until now the prevailing hypothesis explaining generation of autoimmunity; nevertheless, experimental animal models need inflammation via infection or other immunogens to ensure autoimmunity; MM alone is not sufficient to develop autoimmunity. PTMs could arise as an additive factor to MM, which is required to start an autoimmune response. PTMs have been found to be present in different pathologic conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), antiphospholipid syndrome, and primary biliary cirrhosis. The aim of the present review is to expose protein posttranslational modifications and the evidence suggesting their role in the generation of autoimmunity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posttranslational Modifications
In nature, only 20 amino acids (aa) make up most of the proteins, but when considering posttranslational modifications (PTMs), more than 140 amino acids can constitute a protein [1].
PTMs are defined as covalent modifications occurring in a specific aa in a protein. A variety of chemical modifications can be present in a protein, and these modifications occur in a time- and signal-dependent manner; PTMs can arise either by enzymatic modification or spontaneously [2]. PTMs’ presence can determine the tertiary and quaternary structure of a protein and can influence the regulation of its activities, like protein–protein interaction, localization, degradation, and many other functions [3].
Recent advances in proteomic methodology, including the use of mass spectrometry, have made it possible to identify very rapidly proteins in complexes [4]; in general, PTM analyses can be performed by 2-D gel electrophoresis and mass spectrometry. Nevertheless, there are some disadvantages when studying PTMs; firstly, protein modifications in vivo occur only in a small fraction of total proteins (less than 1 %), and secondly, when we consider a sample, it contains a heterogeneous mixture of variously modified and unmodified proteins, and current proteomic technology is useful for detecting only simple modifications in a large amount of modified samples. Another challenge is the study of endogenous protein modifications since sample preparation may disrupt the natural environment of the protein and may affect the peptide in its modified state [2].
Under physiological conditions, proteins are posttranslationally modified to carry out a large number of cellular events, going from cell signaling to DNA replication. However, an absence, deficiency, or excess of these PTMs in proteins can evolve into a target to trigger autoimmunity. The aim of the present review is to expose protein posttranslational modifications and the evidence suggesting their role in the generation of autoimmunity.
Posttranslational Modifications and Their Biologic Functions
PTMs are not encoded in the DNA. They occur after the protein is synthesized and regulate its functions; for example, PTMs are crucial in all aspects of signaling cascades [2].
In general, the cell uses PTMs to control protein functions by regulating its activity, subcellular localization, stability, as well as its interaction with other proteins. PTMs can be reversible, enabling regulation and orchestrating protein functions in response to changes in a cell’s state or environment, without altering its synthesis or turnover rates [5].
Phosphorylation and dephosphorylation of amino acids S, T, Y, and H are the best known and most common PTMs in biological processes, involved in reversible activation and inactivation of enzyme activity and modulation of molecular interactions in the signaling pathway [6].
Acetylation and deacetylation in N-terminal and K-residue are PTMs that modify a variety of proteins, including transcription factors, nuclear import factors, and alpha-tubulin. Acetylases regulate diverse cell functions including DNA recognition, protein–protein interaction, and protein stability [7].
Ubiquitination and deubiquitination and sumoylation and desumoylation alter the biological functions of many proteins. Ubiquitin has a well-documented role in targeting proteins for degradation by the proteasome [8]. Sumoylation has been reported to have crucial roles in regulatory pathways in nucleated cells, like control of nucleocytoplasmic signaling and transport, replication, and regulation of gene expression [9].
Certain cellular processes such as aging, cellular stresses, inflammation, apoptosis, and trauma are known to increase the frequency of posttranslational modifications [10, 11].
Posttranslational Modifications and the Generation of Autoimmunity
How are self-proteins recognized as non-self?
Specific immune responses are initiated by the interaction between processed antigen, presented in association with major histocompatibility complex (MHC) molecules by antigen-presenting cells (APCs), and the T cell receptor (TCR) complex on the surface of CD4+ T helper (Th) cells. Upon activation, the latter cells produce cytokines, which help in the development of antigen-specific B cells and of CD8+ cytotoxic T cells (CTL) from precursor cells. Upon a normal state, the immune system does not react to self-proteins, a phenomenon called self–non-self discrimination. This is attributed, in part, to the elimination of autoreactive T cells by negative selection in the thymus. However, some autoreactive T cells may escape this process and succeed into the periphery. If autoreactive T cells get activated in the periphery, an autoimmune disease may develop. A second hypothesis considers PTMs occurring in the periphery as the cause of autoimmunity, since PTMs arise in the periphery and may not occur in an identical manner in the thymus; thus, these proteins never tolerize developing thymocytes. Consequently, when PTMs arise during cellular responses, such as inflammation, these modified self-antigens can be taken up and processed by APC, which, then, present the modified antigens to autoreactive T and B cells. These cells, in turn, can infiltrate the host tissue where the modified antigen then serves to amplify the autoimmune responses, eventually, leading to autoimmune pathology [12]. Furthermore, the PTM of an amino acid residue, which is critical for recognition and cleavage by certain proteinases, has the potential to influence the generation of new antigenic peptides or can induce a change in the net charge of the protein that can be translated into conformational changes in the tertiary structure of the protein; it could affect also the association with other proteins, since modified self-proteins and peptides derived therein may change how a peptide interacts with MHC molecules [12].
Posttranslational Modifications and Molecular Mimicry
The hypothesis of molecular mimicry (MM) as the cause of immune diseases initiated about 30 years ago stated that either virus or bacteria could exacerbate an autoimmune response through sequence and structural similarities between pathogen peptides and self-antigens. In 1983, Fujinami and his colleagues demonstrated the presence of mouse antibodies to measles virus and herpes simplex virus 1 (HSV-1) that were reactive to both intermediate filaments of normal cells and the proteins of measles virus and HSV-1, thereby demonstrating relatedness between host and viral antigens [13]. After this, a copious amount of information has been published to prove such hypothesis, but the identification of a particular virus or bacterium that is solely responsible for the development of an autoimmune response is rare [14]. However, there are a variety of examples of bacterial infections that can participate in autoimmune disease progression (Table 1). The first observations came from the discovery in similarity between Streptococcus pyogenes M protein and human cardiac myosin as a factor that can contribute to the pathogenesis of rheumatic fever, the specific amino acid sequence present in both proteins was described, and antibodies directed against this peptide could react with both M protein and myosin [32]. Further evidence was published when researchers found an increase in titer prevalence of antibodies against different bacteria (Proteus mirabilis, Escherichia coli) [15, 24] and viruses (Epstein-Barr virus (EBV)) [25] in rheumatoid arthritis (RA) patients when compared to healthy subjects, and the same applied for different autoimmune diseases including infection with Klebsiella pneumoniae and Campylobacter jejuni in ankylosing spondylitis and Guillain-Barré syndrome, respectively [33, 34]. The next question was if a specific sequence derived from a pathogen could be the cause of antibodies that, then due to similarity, could cross-react against sequences within host cells. In this scenario, a given autoimmune disease could be caused by mechanisms in response to molecular mimicry. Furthermore, the presence of elevated serum concentrations of a specific antibody against infectious agents must be considered in the context of specificity of the assay and of control populations of infected and noninfected individuals in order to be meaningful [35].
Several common autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, multiple sclerosis, and ankylosing spondylitis, are genetically linked to distinct human leukocyte antigen complex (HLA) class II molecules and other immune modulators; additionally, autoimmunity often clusters families indicating genetic predisposition to immunological tolerance defects. However, the exact mechanisms that lead proteins, derived from these genes, to produce autoimmune responses remain largely unknown [36].
A plethora of animal models in which molecular mimicry can trigger an autoimmune disease have been developed (for a review, see Cusick [14]). These models consist mainly of an animal induced to express a peptide derived from a specific pathogen in a particular tissue; then, the infection with the microorganism containing the original peptide is performed, and autoimmunity towards the organ expressing the peptide is ensued [37]. It is noteworthy that animals are not generally susceptible to develop spontaneous autoimmune diseases; in the absence of microbes, inflammation and autoimmunity never result [38]. An exception, to a certain degree, are two animal models for primary biliary cirrhosis (PBC), where antimitochondrial antibodies directed against the E2 subunit of pyruvate dehydrogenase complex (PDC-E2) are the hallmark [39]. The first animal model came after the discovery of a PBC-like disease in a child with inborn deficiency of interleukin-2 receptor α (CD25), so an IL-2R alpha/CD25-deficient (IL-2R alpha(-/-)) mice was developed and followed longitudinally for the appearance of liver immunopathology and antimitochondrial antibodies (AMAs) along with wild-type littermate controls. Only IL-2Rα (-/-) mice developed portal inflammation and biliary duct damage similar to that in human patients with PBC and produced AMAs with specificity for PDGE2, which recognizes the inner lipoyl domain of the autoantigen [39, 40]. The second involved a guinea pig model for PBC and demonstrated that environmental factors can act as PBC inducers, including bacteria (Novosphingobium aromaticivorans) and chemical xenobiotics like the cosmetic and food additive, 2-octoynoic acid [2-OA]. Pigs were treated with 2-OA-BSA, and the tolerance deficit of the first model was replicated by the effects of complete Freund’s adjuvant (CFA), resulting in manifested autoimmune cholangitis, antimitochondrial antibodies, and infiltration of the liver with activated CD8 T cells [41]. Nevertheless, the use of adjuvants in animal research studies requires special consideration, since CFA is a water-in-oil emulsion, containing heat-killed mycobacteria or mycobacterial cell wall components, that effectively potentiates cellular and humoral responses to the injected immunogens, producing a relatively nonspecific inflammatory response that results in an influx of cells from the immune system to the site of antigen deposition and interaction with the antigen [42]. Such inflammatory response can increase the number of PTMs at the inflammation site and serve as danger signals to elicit an autoimmune response, as we hypothesized before.
Furthermore, in a transgenic model of insulin-dependent diabetes mellitus, it was established that even when the transgenic antigen is expressed in the animal thymus to induce tolerance and the negative selection process efficiently eliminates high-affinity T cells, infection eventually results in autoimmunity [43]. Indicating that T cells with low affinity, which survive negative selection, can be activated in the periphery and produce autoimmunity [44].
For a long time, molecular mimicry has been considered the prevailing hypothesis as to how viral or bacterial antigens initiate and maintain autoimmune responses that can lead to specific tissue damage. Nevertheless, the ability to induce autoimmunity based only on molecular mimicry mechanisms has not been established, accessory mechanisms are missing, since we are still not able to prove that autoimmunity initiated by molecular mimicry can generate enough auto-aggressive lymphocytes with sufficient avidity to cross the threshold for clinical autoimmune diseases. Local inflammation produced by other means plays a key role in the generation of autoimmune diseases. This last asseveration supports our theory that molecular mimicry exists, but other components are required to finally break tolerance and ensure autoimmunity. These other components may act as “danger signals,” and our suggestion is to focus on PTMs as danger signals that ultimately will lead to the production of autoimmunity (Fig. 1).
Autoimmunity generation through molecular mimicry (MM) and posttranslational modifications (PTMs). Molecular mimicry exists, but it has not been possible until now to explain autoimmunity solely through MM mechanisms; the generation of PTMs after inflammation upon infection or any other mechanism might be enough to act as danger signals and initiate an autoimmune disease to a previously recognized antigen
Posttranslational Modifications and Disease
RA
The systemic autoimmune disease, RA, is characterized by synovial tissue inflammation leading to bone and cartilage degradation with ultimate articular destruction. It affects about 1 % of the population; although, its etiology is unknown, genetic predisposition, environmental factors, and an aberrant activation of the innate and adaptive immune system play a role in disease pathogenesis [45]. A number of characteristics such as the occurrence of erosions at presentation shortly after onset of symptoms, the presence of synovial infiltrates in clinically unaffected joints, and the appearance of autoantibodies long before onset of the disease suggest that there are pathological mechanisms before clinical symptoms become apparent [46] (see Tables 2 and 3).
Autoantibodies in Rheumatoid Arthritis
RA patients produce autoantibodies. The first one identified was the rheumatoid factor (RF) directed against the Fc fraction of immunoglobulin G (IgG), which is not very specific for RA, since it can be found in other conditions where inflammation is present. Autoantibodies that are now well recognized as being very specific for RA are anti-citrullinated peptide antibodies (ACPA) [47] and anti-citrullinated mutated vimentin antibodies (anti-CMV) [48]. Both and other autoantibodies, previously described to be specific for RA, share a peptide with a specific PTM: citrullination [49]. The importance of ACPA is that they are not only very specific but they also have a positive predictive value, mainly if taking into account results from two studies, where their presence in asymptomatic individuals (blood donors) was a predictor for RA disease generation [50], and in patients with undifferentiated arthritis, they predicted the development towards RA [51].
PTMs in Rheumatoid Arthritis
Citrullination
The enzyme peptidylarginine deiminase (PAD) is responsible for the posttranslational conversion of arginine residues to citrulline [52]. Until now, five isotypes of these enzymes have been described in mammals, and they are unable to alter free l-arginine, only arginines bound into proteins [53]. These enzyme isotypes are differentiated by their localization [54], and only PAD4 and PAD2 can be found in synovia. The protein PAD4 consists of 663 amino acid residues and is the only isotype, out of five enzymes described, to be expressed in the cellular nucleus [55] and has a 74-kDa molecular weight [56]. PAD enzymes have diverse physiologic functions: aggregation of keratin during terminal differentiation in the epidermis [57], involvement in brain development [58], and gene expression regulation by chromatin modeling [55, 59].
PAD4 enzyme is then responsible for the production of the antigenic determinant recognized by ACPA and anti-CMV antibodies. It is important to outline the fact that not only the expression of this enzyme in synovial tissue is sufficient for citrullinated antigens to appear, since this enzyme needs an increase in cytosolic Ca+2 concentration (2 μM) [56]. Calcium ions induce conformational changes that create the active site in the α/β catalytic domain. Intracellular calcium concentrations range from ∼200 nM (resting cells) to ∼1 μM (activated cells) [60], but concentrations in the cytosol can be increased during apoptosis or necrosis, leading to PAD activation [61].
During cellular death, membrane integrity is lost, and enzymes then can get activated and induce protein citrullination [62]. Nevertheless, the presence of citrullinated proteins in synovia is not associated only with RA, since protein citrullination can be observed in subjects with inflammation secondary to a number of causes different from RA. The interesting fact is that only RA patients develop ACPA production [63]. When murine models of collagen-induced RA were examined, it was proved that citrullinated proteins are expressed by day 21 after the induction of RA, and their presence correlates with disease progression [64]. Recent genome-wide association studies suggest that ACPA-positive RA and ACPA-negative RA differ significantly in the frequency of risk alleles, mainly the HLA locus (30–50 %) [65]. Finally, RA patient’s serum has demonstrated variability in the reactivity pattern towards different peptides, but all of them must have citrulline, indicating that this aa is important for antigenicity and that ACPA antibodies are being produced in a polyclonal form [66]. Altogether, these data support the fact that protein citrullination is a phenomenon that is being produced early during the course of the disease and that it might be involved in disease generation [51, 67]. Proteins described to contain citrullinated residues in synovium include fibrin [68], fibrinogen [69], vimentin [70], collagen [71], and α-enolase [72].
Consequences of protein citrullination include protein charge neutralization, change in isoelectric point, ionic interaction breakage, partial unfolding of protein, decreased photolytic degradation, increased antigenicity, and increased affinity with the HLA.
Immune reactions against citrullinated peptides, generated in the joints during arthritis, have demonstrated local antibody production [73], and recent studies on the specificity and structure of monoclonal IgG ACPAs, generated from synovial fluid B cells, demonstrated that between 16 and 33 % of all CD19+ IgG + B cells were able to produce antibodies specific for different citrullinated antigens [74].
Citrullination is a PTM involved in many physiological processes in the body from skin keratinization, through gene regulation, to immune functions, and it is also implicated in pathological processes such as autoimmunity and tumor genesis.
Protein Carbamylation
Carbamylation (carbamoylation) of lysine residues and N-terminal domains in different proteins is a nonenzymatic PTM that has been related to protein aging [75].
Different models to trigger experimental arthritis in animals by the use of anti-citrulline antibodies have been developed, but they have yielded only modest results; for this reason, the existence of other triggering factors has been proposed [76, 77].
Carbamylation also known as homocitrullination involves a reaction of urea-derived cyanate with free NH2- groups on lysine (Lys) residues to yield homocitrulline (Hcit), which is an amino acid that highly resembles citrulline. Cyanate can be formed in low concentrations from urea under physiologic conditions and can also originate from the environment (e.g., car fumes). Under inflammatory conditions, cyanate can be formed from thiocyanate catalyzed by myeloperoxidase (MPO) release (activated neutrophils) [78], and this enzyme has been recognized recently as a potential trigger factor for inflammation [79]. Since ACPAs from RA patients can induce the production of neutrophil extracellular traps (NETs) [80], this could represent a connection between ACPA production and carbamylation, making both important participants in the generation of RA.
Furthermore, collagen is easily carbamylated in vivo, and this modification may be directly linked to granulocyte activation and protease release [81, 82]. Additionally, immunization of mice with carbamylated peptides (Hcit immunization) induced T CD4+ and B cell activation and proliferation followed by high levels of cytokines (IL-10, IL-17, and IFN-γ) and autoantibody production, which contribute to ongoing inflammation; interestingly, such mice became susceptible to arthritis induced by the intra-articular injection of Cit peptides [83]. Hence, carbamylation may be a mechanism involved in the generation of arthritis secondary to PTMs’ presence.
Recently, antibodies against carbamylated proteins (anti-CarP) have been associated with the development of RA in a cohort of patients with arthralgia, who were followed for 3 years independent of ACPA antibodies [78]. Antibodies to citrullinated and carbamylated antigens have shown cross-reactivity [84], and this fact should be taken into account for diagnostic purposes.
Epigenetic Modifications in RA
In the last years, resident synovial fibroblasts (SF) emerged as key players in RA development, since it was demonstrated that they actively contribute to joint destruction by implanting SF from RA patients (RASF) together with healthy human cartilage into severe combined immunodeficient mice and registering that activated RASF migrate in vivo and spread the disease to sites of implanted cartilage, whereas control mice with implanted SF from osteoarthritis (OA) patients and dermal fibroblasts did not. This evidence suggested that RASF, even in the absence of cellular and humoral immune response, are capable of human cartilage destruction [85]. RASF differ from healthy SF in their morphology and aberrant gene expression pattern and are further characterized by the expression of anti-apoptotic molecules, proto-oncogenes, and lack of expression of tumor suppressor genes; they can attract inflammatory cells and produce enzymes such as matrix metalloproteinases (MMPs) that promote invasion and cartilage destruction [86]. There are PTMs occurring in RASF that involve histone tails, transcription factors, and tumor suppressor proteins, grouped as epigenetic modifications since they can determine the stability of the chromatin structure, genome integrity, and modulation of gene expression; such modifications include acetylation, phosphorylation, methylation, ubiquitination, and sumoylation [45]. The best studied modifications are acetylation of specific lysine residues of histones H3 and H4; these modifications play a role in replication and transcriptional regulation; the acetylation state is controlled by two antagonizing enzyme families, namely histone acetylasetransferases (HATs) and histone deacetylases (HDACs) [87]. Acetylation is generally associated with transcriptional activation and, on the contrary, deacetylation is linked to gene silencing [45]. Results on the prevailing state of histones are contradictory, but overall it has been suggested that changes in RASF acetylation or deacetylation of histones may be influenced by the local inflammatory status [88]. The predominant histones modified by methylation are H3 and H4; lysine residues can be monomethylated, dimethylated, or trimethylated, depending on the degree of histone methylation, and regions of more active or inactive chromatin can be seen [89]. In RASF, an overexpression of the histone methyltransferase enhancer of zeste homolog 2 (EZH2) was reported in comparison with OASF. EZH2 overexpression has been implicated in the pathogenesis of inflammatory arthropathies [90].
Sumoylation of Proteins in RA
Another PTM described in RA is sumoylation. The small ubiquitin-like modifier (SUMO)-1 is an important posttranslational regulator of different signaling pathways and is involved in the formation of promyelocytic leukemia (PML) protein nuclear bodies (NBs). SUMO is a family of proteins that are not only structurally but also mechanistically related to ubiquitin in that they are posttranslationally attached to other proteins. SUMO is covalently linked to its substrates via amide (isopeptide) bonds formed between its C-terminal glycine residue and the epsilon-amino group of internal lysine residues. Its substrates include a variety of biomedically important proteins such as tumor suppressor p53, c-jun, PML, and huntingtin [5]. The study of SUMO-1 is of interest because it can accommodate with the Fas-associated death domain (FADD) [91], and overexpression of SUMO-1 was shown to protect BJAB cells from Fas-induced death [92]. This is relevant since RASF have shown that modification of PML protein by SUMO-1 regulates Fas-induced cell apoptosis, inducing resistance to death, described by Minecke and colleagues [93].
RA and Molecular Mimicry
The molecular mimicry hypothesis in RA mainly came after two important discoveries:
-
1)
The presence of high titers of antibodies against P. mirabilis in RA patients from different countries [15–20] providing support to the suggestion of RA being a reactive arthritis [94] and following the “Popper sequences,” Ebringer and colleagues [95] concluded that upper urinary tract Proteus infections are the most probable cause of RA.
-
2)
The discovery of the HLA-DR-susceptible alleles for rheumatoid arthritis, HLA DRB1 0101 0401 0404 and 0405, gave insights into the genetic basis participating in disease generation and could be used to evaluate candidate autoantigens. These alleles together with the HLA DRB4 are present in over 90 % of RA patients compared to 35 % in the general population. Such alleles have in common a conserved sequence of amino acids QKRAA, QRRAA, or RRRAA from position 70 to 74 on the DR1 chain. A common denominator between these sequences and some from the HLA DRB4 is the sequence EQRRAA, named the shared epitope (SE) [96], where E or glutamic acid is negatively charged and R or arginine is positively charged at physiological pH. These sequences are located within the binding groove of the HLA class II molecule, where peptides are located to be presented to T cells by antigen-presenting cells, and sequences containing arginine are susceptible to citrullination via PAD enzymes. Two explanations can come from the latter findings: either HLA-DR1/4 molecules present citrullinated antigens to immune cells or the EQRRAA sequence shows molecular mimicry and is being citrullinated at the same time in the R residues inducing RA.
In accordance to the first explanation, collagen was the first candidate autoantigen described for RA, and specifically two peptides from this protein were identified to bind effectively with the HLA SE [97]. In support of the molecular mimicry theory, two sequences identified in P. mirabilis, E. coli, rubella, and herpes viruses were structurally related to the two previously identified collagen peptides and, by analyzing their sequences, they were predicted to effectively bind to the SE [98, 99]. A role for mimicry has also been established in Lyme disease, where an association with HLA-DRB1*0401 was described; the homology was found between lymphocyte function-associated antigen-1 and the outer surface protein (OspA) in Borrelia burdogferi. However, further elucidation of the mechanisms linking the presence of peptide mimicry and generation of chronic arthritis is missing [35].
Traditionally, comparisons were made between linear amino acid sequences from proteins of suspect pathogens and host antigens. The advent of molecular techniques and computerized protein databanks has greatly enhanced the ability to predict the probability of a microbial peptide to bind the SE. It has been suggested that primary structural mimicry is far more common than previously thought with a calculation of up to ten perfect matches for any single five amino acid sequence [100]. However, the missing link between molecular mimicry and the induction of an autoimmune disease might not be related to peptide sequence but to its conformation, which can be dependent on a specific PTM allowing a change in peptide structure. Another possibility is that the peptide can only be recognized by the immune system if a specific PTM is present, acting as a danger signal, as is the case of citrullinated peptides in RA [66, 101].
Systemic Lupus Erythematosus (SLE)
SLE is an autoimmune disease characterized by a variety of multiple organ damage through inflammation and autoantibody production [102]. Patients with SLE have been studied over the years; important research in this autoimmune model has focused on the origin of tolerance loss to self-tissues; however, to this day, information is missing about its etiology. It has been proposed that possible causes for SLE include immune dysregulation and genetic and environmental factors [26].
Posttranslational Modifications in SLE
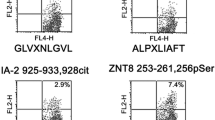
Specifically, it has been proposed that immune dysregulation involves the participation of PTMs through the generation of amino acid sequence change in self-proteins leading to the production of neo-peptides that can be recognized as “foreign,” initiating a progressive immune response through autoantibody production [12, 29, 103]. PTMs frequently found in SLE are phosphorylation, methylation, acetylation, and isoaspartylation. A protein susceptible to phosphorylation in SLE is U1-70k (also known as 68k). The U1-70k protein is a small nuclear ribonucleoprotein (snRNP), located in the nucleus, with an established role in processing pre-mRNAs. This protein has been identified as an autoantigen selectively phosphorylated on serine and arginine domains (RS) during apoptosis associated to cellular stress. More than 20 isoforms of U1-70k with different molecular weights and isoelectric points have been described in SLE patients. One altered isoform called 2-1 showed lower levels of phosphorylation in patients with SLE compared to a group of rheumatoid arthritis patients. These findings may relate to the pathogenesis of SLE; however, the results are not conclusive as only one of four patients tested positive for anti-RNP antibodies, so it is necessary to analyze whether the PTM phosphorylation in U1-70k is a mechanism of disease induction or a consequence [104]. Recently, the phosphoproteome was characterized in the PBMC of SLE patients by a highly sensitive liquid chromatography-mass spectrometry system (LC-MS/MS); this study reported that there are 1,035 phosphorylation sites corresponding to 618 genes identified in SLE patients. Besides these modified genes, the authors found that the cellular components with higher concentration of phosphoproteins are the nucleus and cell membrane, and the processes with higher presence of phosphoproteins are those related to nucleobase, nucleoside, nucleotide, and nucleic acid metabolism. Considering these results in terms of structure and function, they demonstrated that 50 metabolic pathways are modified in the pathogenesis of SLE, specifically the MAPK signaling pathway, leading to an abnormal intracellular signaling [104]. Moreover, other proteins that can be modified by PTMs are Ro/SSA and La/SSB, which are complex ribonucleoproteins found in the nucleus and cytoplasm; such proteins can be recognized by antibodies to Ro/La, and both autoantibodies are present in SLE and Sjögren's syndrome (SS) patients. The analysis of a phosphorylated epitope consisting of 349 to 368 aa in La/SSB protein has shown that this peptide is recognized and bound with high avidity by anti-La/SSB antibodies when compared with the same epitope but not phosphorylated [104, 105]. Another PTM associated with the pathogenesis of SLE is methylation of the Sec1/Munc18 (Sm) protein, which is part of the structure of snRNP proteins U1, U2, U4, and U5. There are seven Sm proteins, B/B′, D1, D2, D3, E, F, and G, which may be targets of anti-Sm immune response; in SLE, autoantibodies to Sm have been shown to be more specific. Sequencing and mass spectrometry evidenced that proteins SmD1 and D3 showed a symmetrically methylated arginine carboxyl terminal region (sDMA, symmetrical dimethylarginines). When D1 sDMA modification was tested with sera of SLE patients positive to Sm autoantibodies, 10 of the 11 positive patient sera to Sm reacted to the D1 sDMA protein; however, not the same results were observed with homologous peptides with an asymmetric methylation (aDMA, asymmetrical dimethylarginines), so recognition by anti-SmD1 autoantibodies depends on symmetrical dimethylation of the arginines located at the carboxyl terminal regions [106–109]. In addition to these autoantigens, nucleosomes are immunogens that can be recognized by pathogenic Th cells in SLE. It has been proposed that the origins of these autoantigens are released particles from apoptotic cells. Nucleosomes consist of an octamer of histones, 2H2A, 2H2B, 2H3, and 2H4; particularly H2B and H4 have been shown to undergo apoptosis-induced acetylation in lupus mice and SLE patients [110, 111]. Besides the acetylation of histone H2B, a second modification is made by isoaspartylation, another PTM involved in the conversion of aspartic acid (Asp) to isoaspartic acid (isoAsp). This modification occurs spontaneously under physiological conditions. The isoAsp at position 25 of histone H2B is an autoantigen recognized by autoantibodies in both mouse models and humans [112].
In addition to the strong data on the dysregulation of the immune system induced by PTMs, about 30 years ago, it was reported that the intake of l-canavanine amino acid, an l-arginine analog, found in beans, clover, onions, seeds, and sprouts of alfalfa may induce or exacerbate SLE [113]. Besides being associated with autoimmunity, it has been observed that l-canavanine has an important role in plant chemical defense toward a wide range of pests, competitors, and predators of canavanine-storing plants [114]. Although no data exist on the possible loss of immune tolerance induced by l-canavanine, it has been hypothesized that this amino acid can be incorporated into cellular proteins by arginyl tRNA synthetase, leading to the formation of aberrant proteins. This assertion has been linked with a possible mechanism in antitumor activity [115]. The involvement of l-canavanine in lupus pathology was supported by the presence of abnormal blood cell counts in humans and nonhuman primates after the intake of alfalfa sprouts [116, 117]. There is scarce clinical information in humans about l-canavanine and its participation as a risk factor for autoimmunity development; nevertheless, in a case–control study, in southern Sweden, the proportion of women who reported consumption of alfalfa sprouts was similar among case and controls, 12 and 15 %, respectively [118]. It is necessary to investigate how the addition of l-canavanine into the protein structure can participate in the breakage of immune tolerance and the generation of autoimmunity, specifically SLE.
SLE and Molecular Mimicry
Additional molecular mechanisms to SLE pathogenesis involve molecular mimicry, specifically focused on EBV, which is a potential source of antibodies that can cross-react with self-antigens, including autoantibodies against dsDNA, Sm, and Ro antigens in SLE patients [119]. Animal models have been used to clarify this information, but, until now, the creation of a small animal model for EBV infection has failed, since experimental mouse models do not reproduce the spectrum of viruses that infect humans; for this reason, research has focused on clinical data obtained from patients. A high percentage of patients with SLE have shown an increased frequency of antibodies against various proteins of the EBV in particular to the major latent protein Epstein-Barr nuclear antigen 1 (EBNA-1) [120]. More specifically, a study designed to investigate fragments of the EBNA-1 particle and its reactivity found titers of antibodies against the aa35–58 EBNA-1 fragment elevated in both SLE and multiple sclerosis (MS) patients. But EBNA-1 antibodies against aa398–404 were elevated significantly only in the SLE patients. High anti-EBNA-1 IgG titers were independent of the susceptibility HLA-DRB1*15:01 allele [121].
Several studies in female BALB/c mice immunized with EBNA-1 of the EBNA-1 have demonstrated the production of antibodies that cross-react with dsDNA and Sm particles [122, 123]. Recently, nonhuman primate models have been developed to manipulate specific viral genes, which allow the study of humoral and cellular immune responses [124, 125]. Furthermore, bacterial infections have also been proposed as triggers for SLE. Burkholderia fungorum is an opportunistic pathogen that colonizes the lungs of cystic fibrosis patients with immune deficiency. Zhang and colleagues showed that anti-dsDNA antibodies purified from SLE patients can react specifically with B. fungorum compared with control sera [126]. However, before considering a pathogen to be a trigger of any autoimmune disease, it is necessary to clarify the pathway that initiates with the infection and ends in a loss of tolerance.
Antiphospholipid Syndrome (APS)
The APS is characterized by a prothrombotic state, leading to arterial and venous thrombosis, together with pregnancy complications and recurrent history of pregnancy loss together with the presence of antiphospholipid antibodies. Such manifestations can be presented in primary APS or associated with an autoimmune systemic disease like SLE (secondary APS). β2-glycoprotein I (β2GPI) has been described as the primary antigen detected by specific autoantibodies in this syndrome [127]. APS represents the most frequent cause of acquired thrombophilia (15–20 %) [128]. β2GPI is a highly abundant apolipoprotein and a member of the complement control protein family, and it consists of 326 aa arranged in 5 short consensus repeat domains; normally, β2GPI binds to cell surface receptors and negatively charged surfaces due to a highly positively charged fifth domain. The involvement of β2GPI in the coagulation cascade seems multifaceted, since the protein can exert both procoagulant and anticoagulant activities. Binding of β2GPI to anionic phospholipids on activated platelets and endothelial cells (ECs) possibly results in a competition between β2GPI and coagulation factors for phospholipid surfaces, but, on the other hand, plasmin and less efficiently FXa in vitro can cleave the fifth domain of β2GPI, abolishing its binding to anionic phospholipids, a phenomenon enhanced by heparin, inhibiting plasmin generation, which is a key event in the fibrinolytic system. Dysregulation of such pathways is achieved by autoantibody production that can bind and interact with β2GPI and generate a prothrombotic state in APS [129].
Historically, APS was detected as the presence of either a lupus anticoagulant (LA) or anticardiolipin antibodies (aCL). It was originally thought that the LA phenomenon was due to autoantibodies against anionic phospholipids interfering with the assembly of the tenase and prothrombinase complexes; afterwards, the aCL assay was developed as an alternative way of detecting these hypothetical antibodies. In 1990, it became clear that these tests were detecting antibodies to phospholipid binding proteins; in fact, the aCL enzyme-linked immunosorbent assay (ELISA) typically detects antibodies to β2GPI [130]. Antibodies against β2GPI (anti-β2GPI) that bind to the first domain of the protein correlate better with thrombotic complications, rather than with autoantibodies to other domains [131, 132]. Furthermore, autoantibodies react to β2GPI only when the protein is bound to an anionic surface and not when it is soluble or circulating. Two conformational different forms of β2GPI have been described: the soluble form (circular) and an active form (open). The circular conformation is generated after an interaction between domain I and domain V of the protein. The open conformation is required for its inhibitory function on the coagulation intrinsic pathway. In the open form of the protein, the domain I is exposed, so antibodies against β2GPI can then bind; part of the epitope recognized by autoantibodies consists of aa Arg39–Arg43 in the first domain [132].
Antibodies against β2GPI or cardiolipin are key factors to determine diagnosis, but evidence is still missing about how these autoantibodies participate in the generation of a thrombotic event, making it an area of intense research.
PTMs in APS
Biochemical differences between the physiological and pathogenic structure of β2GPI have been previously described; such differences can be produced by PTMs.
Most of the β2GPI that is circulating has two or more unpaired cysteines (free thiols). This form constitutes the reduced form of β2GPI. The free thiols exposed on β2GPI interact with platelets and endothelial cells. Posttranslational modification of cysteines includes the addition of oxygen, nitrogen oxide (NO), or glutathione. These modifications can also alter the function of extracellular proteins and can be increased under oxidative stress conditions. Oxidative stress is characterized by overproduction of reactive oxygen species (ROS) that react with cysteine residues, especially redox active cysteine, to form reversible or irreversible oxidized forms. β2GPI oxidation results in a change of its structure and, more importantly, it could confer an increase in immunogenicity [133].
In the antiphospholipid syndrome, as noted in a recent review paper [134], several findings account for the oxidative environment, such as the decrease in paraxonase activity, lacking or preventing oxidation of low-density lipoprotein cholesterol, and increase in lipid peroxidation markers mainly represented by the increased levels of β2GPI-oxidized LDL complexes [135–137].
Ioannou et al. conducted a study to determine levels of β2GPI in its reduced and oxidized form, and an increase in oxidized β2GPI was found in APS patients as compared to control subjects, suggesting that this PTM could play a role in APS pathogenesis. These authors also hypothesized that clinical states associated with an increased oxidative stress load, such as pregnancy and infection, may lead to further increases in the levels of oxidized β2GPI, elevating the risk of pathologic thrombosis in patients who are positive for anti- β2GPI antibodies [138].
Another posttranslational modification named sialylation has been described in patients with APS. This PTM occurs in the glycan structures of the β2GPI. The authors confirmed that sialylation of β2GPI can change the conformational stability of the protein and induce the exposition of an otherwise cryptic epitope, leading to an intermolecular interaction between amino acid residues Arg39–Arg43 in the first domain of the protein and autoantibodies [139].
A few mechanisms have been proposed to consider β2GPI as an autoantigen: (1) antigenicity of the protein can be generated if it is converted into an endogenous immunogenic adjuvant and (2) loss of tolerance to a β2GPI chemically modified through a posttranslational modification. Furthermore, depending on the redox state of the β2GPI, an innate immune response can be initiated and maintained, but only a few forms of the oxidized β2GPI are capable of activating dendritic cells in vitro [140].
Other considerations that need to be taken into account in APS to be able to elucidate the mechanisms involved in posttranslational modifications and thrombophilia are changes in β2GPI structure, net charge, sites of antibody production, isotype of the antibodies, antigen localization, effector cells that participate in the immune response, inflammation pathways with special emphasis towards complement molecules, and coagulation elements; after a proper integration of all these mechanisms, we might be able to elucidate the pathway for autoimmune thrombophilia [141].
Celiac Disease (CD)
A unique property of wheat flour is the formation of a viscous mass upon contact with water called gluten, which is characterized by a big and heterogeneous polymeric complex, formed by several polypeptide chains of glutenin united by disulfide bonds (SS) and a monomer of gliadin. The gliadin family comprises alpha gliadins, gamma-gliadins, and omega gliadins; all of them are soluble in 40/70 % ethanol. On the other hand, the glutenin family is divided in low molecular weight gluteins and high molecular weight gluteins, and they are both insoluble in alcohol and provide elasticity to gluten [142]. CD is the most common autoimmune process of genetic origin causing food intolerance; it affects 1:70–1:200 individuals worldwide. CD can manifest at any age since it depends on gluten protein exposure, mainly prolamins from wheat gliadin, secalin from rye, and hordein from barley [143, 144]. CD, like other autoimmune diseases, is chronic and multifactorial with 2:1 female/male proportion. Patients with CD show diverse grades of intestinal inflammation, ranging from moderate intraepithelial lymphocytosis to severe mononuclear subepithelial infiltration, which leads to atrophy of the villous mucosa from the small intestine and cryptic hyperplasia, being the reason for bad absorption in the digestive tract [144]. Basic treatment for these patients, previous to duodenum or jejunum biopsy, should be restriction of gluten intake; this would prevent symptoms to appear and intestinal villous mucosa should normalize [145].
The genetic component in this autoimmune disease was established after verification of higher prevalence of the disease among first-degree relatives (10 %) and a high concordance between monozygotic twins (70 %). Nevertheless, other theories have been postulated due to an increasing incidence in the later years and because other factors are being taken into account, like changes in diet consumption and/or viral infections [146]. In the past, CD had been associated to other autoimmune diseases, like SLE, Sjogren syndrome, selective IgA deficit, type 1 diabetes, Graves’s disease, and autoimmune hepatitis, probably by the pleiotropic effect of the involved genes [147–149].
Mechanisms for CD development are not well established, but it is recognized that four components are needed: gluten intolerance, tissue transglutaminase enzyme (TG), HLA-DQ, and T cells [144]. Once the gluten is ingested, it is degraded to peptides by gastrointestinal enzymes; some of these peptides can bind to HLA class II DR, DQ2, or DQ8, present in APC, and trigger T cell responses. Locally, it will cause tissue damage and increased levels of transglutaminase 2 (TG2).
Posttranslational Modifications in CD
The enzyme TG2 can be found in all tissues, and it is calcium (Ca+) dependent; so, under physiological conditions, it is inactive, and TG2 is rapidly inactivated in the extracellular environment by oxidation. TG2 belongs to a family of enzymes that are involved in crosslinking reactions; the enzyme targets specific glutamine residues of polypeptides. As a first step in the enzymatic reaction, the glutamine residue makes a thiol-ester bond to the active cysteine site of TG2. This enzyme–substrate intermediate then reacts with a primary amine group, such as a lysine residue, and an isopeptide bonded covalent crosslink is formed in a process termed transamidation. Alternatively, the enzyme substrate intermediate can react with water, and then, the glutamine residue is converted to glutamate in a process termed deamidation. A deamidated product can also be formed by TG2-mediated hydrolysis of the isopeptide bond in the cross link [150]. Consequences of glutamine deamidation include the formation of a more stable HLA-peptide complex and a stronger immunological synapse formation, since the change in peptide charge also appears to interact with the TCR. T cell responses include the production of inflammatory cytokines (IL-15) that induce local inflammation and epithelial damage [142, 150].
Until now, 15 different epitopes for T cell recognition have been described in gluten, and the majority of these T cell epitopes contain glutamine residues that are targeted by TG2 converted to glutamate residues by a deamidation reaction. In general, T cells of celiac disease patients recognize deamidated epitopes with greater efficiency than native ones. This PTM effect appears to be stronger for HLA-DQ2.5 than for HLA-DQ8, as many of the HLA-DQ2.5-restricted epitopes are not recognized in their native form, whereas some HLA-DQ8-restricted epitopes are equally well recognized as native peptides. The reason for this difference may be related to the ability of HLA-DQ8 to recruit T cells with a negative charge, which can stabilize native peptides bound to HLA-DQ8 [150, 151].
The disease is further characterized by the presence of autoantibodies to transglutaminase 2 that have extraordinary high disease specificity and sensitivity. The presence of autoantibodies in these patients can be explained as a consequence of three specific processes that determine epitope selection in T cells: (1) proteolytic stability (Since gluten peptides are rich in proline residues, hence they are resistant to intestinal proteolysis and, therefore, they could be stimulating the production of T CD4+ cells in the lamina propia, which are needed for isotype switch by B cells); (2) HLA complex selection of gluten epitopes binding motifs (Both HLA-DQ2.5 and HLA-DQ8 prefer negatively charged anchor residues and, notably, these are residues that have been introduced by a PTM); and (3) transglutaminase specificity.
CD and Molecular Mimicry
CD is characterized by systemic manifestations that contribute to a complex clinical presentation. Besides enteropathy, the most common extraintestinal symptoms associated with CD are neurological deficits that include axonal neuropathy and cerebellar ataxia [152]. Patients with CD exhibit elevated levels of different autoantibodies. The most specific are antibodies against tissue transglutaminase (anti-tTG) [153]. In addition, elevated levels of anti-gliadin antibodies have also been detected in patients with CD with less specificity but in association with idiopathic neuropathy and ataxia [154]; furthermore, patient serum and anti-gliadin antibodies have been shown to bind neural tissue, implying a cross-reactivity with autoantigens (synapsin I) and postulating a mechanism of molecular mimicry [155]. Additional information regarding the molecular mimicry theory came from the discovery that a subset of anti-tTG IgA antibodies recognizes the rotavirus viral protein VP7 [156]; changes in gene expression of T84 cells upon stimulation with such antibody demonstrated a tendency towards apoptosis and inflammation, but a model in which molecular mimicry is sufficient for an autoimmune phenomenon is still missing.
PBC
Similar to other immune complex mediated diseases, the combination of a susceptible genetic background and exposure to environmental triggers is needed to initiate and promote this disorder. PBC is an autoimmune liver disease characterized by the presence, in serum, of highly specific AMAs directed against the PDC-E2 and progressive destruction of intrahepatic bile ducts, resulting in chronic cholestasis, portal inflammation, and fibrosis that can lead to cirrhosis and, ultimately, liver failure [156].
Participation of environmental factors has been claimed to contribute to the onset of PBC; among factors proposed to play a role in triggering the disease onset are infections and chemicals through molecular mimicry and modification of autoantigens, respectively [156]. Several bacterial proteins have certain homology to the E2 epitope recognized by AMAs, but no support exists for the generation of autoimmunity through molecular mimicry alone. On the other hand, xenobiotics can either alter or form a complex with host proteins, generating neoantigens that can be recognized by the immune system.
Lipoic acid is attached to only a few proteins, yet it is a vital component of the E2 epitope, and it is covalently attached to the ε group of lysine via an amide bond and is displayed on the outer surface of the PDC-E2 [157] and is susceptible to reductive acylation [158]. Such PTM has two effects: it allows catalyzing of the acyl transfer and renders PDC-E2 susceptible to aberrant chemical modifications [159]. In fact, it was demonstrated that when the lipoyl domain of a PDC-E2 peptide was conjugated to synthetic small molecule lipoyl mimics, they displayed highly specific reactivity to AMA-positive PBC sera [160]. Furthermore, it has been demonstrated that oxidative states of lipoic acids affect immunogenicity, being more immunogenic if it is in a reduced form [161].
Hence, conformational changes of the PDC-E2 lipoyl domain during physiological acyl transfer could be the lynchpin to the etiology of PBC, and xenobiotics can be postulated as inducers of modifications in the lipoyl domain of PDC-E2, making them susceptible to PTMs that induce T cell activation with subsequent production of AMA by B cells in patients with PBC.
Concluding Remarks
Challenges for future study of posttranslational modifications include the development of new techniques that would allow the analysis of different proteins, contained in a single sample, as well as techniques that require a decreased amount of proteins for their analysis. The understanding of the relationship between PTMs and physiological balance will give us a comprehensive view of how complicated biological processes arise in signaling pathways and antigen expression. A special mention is to be given to the recently reinforced notion of molecular mimicry interplay with posttranslational modifications in both health and disease. It will also help us to understand biological processes in disease states, mainly autoimmunity, as the present evidence indicates that PTMs could be important triggers to an autoimmune state.
References
Uy R, Wold F (1977) Posttranslational covalent modification of proteins. Science 198:890–896
Seo J, Lee KJ (2004) Post-translational modifications and their biological functions: proteomic analysis and systematic approaches. J Biochem Mol Biol 37:35–44
Baenziger JU (2003) A major step on the road to understanding a unique posttranslational modification and its role in a genetic disease. Cell 113:421–422
Mann M, Jensen ON (2003) Proteomic analysis of post-translational modifications. Nat Biotechnol 21:255–261
Dohmen RJ (2004) SUMO protein modification. Biochim Biophys Acta 1695:113–131
Pawson T (2002) Regulation and targets of receptor tyrosine kinases. Eur J Cancer 38(Suppl 5):S3–S10
Kouzarides T (2000) Acetylation: a regulatory modification to rival phosphorylation? EMBO J 19:1176–1179
Schwartz JH (2003) Ubiquitination, protein turnover, and long-term synaptic plasticity. Sci STKE 2003:pe26
Seeler JS, Dejean A (2003) Nuclear and unclear functions of SUMO. Nat Rev Mol Cell Biol 4:690–699
Najbauer J, Orpiszewski J, Aswad DW (1996) Molecular aging of tubulin: accumulation of isoaspartyl sites in vitro and in vivo. Biochemistry 35:5183–5190
Utz PJ, Gensler TJ, Anderson P (2000) Death, autoantigen modifications, and tolerance. Arthritis Res 2:101–114
Doyle HA, Mamula MJ (2011) Autoantigenesis: the evolution of protein modifications in autoimmune disease. Curr Opin Immunol 24:112–118
Fujinami RS, Oldstone MB, Wroblewska Z, Frankel ME, Koprowski H (1983) Molecular mimicry in virus infection: crossreaction of measles virus phosphoprotein or of herpes simplex virus protein with human intermediate filaments. Proc Natl Acad Sci U S A 80:2346–2350
Cusick MF, Libbey JE, Fujinami RS (2012) Molecular mimicry as a mechanism of autoimmune disease. Clin Rev Allergy Immunol 42:102–111
Ebringer A, Ptaszynska T, Corbett M, Wilson C, Macafee Y, Avakian H, Baron P, James DC (1985) Antibodies to proteus in rheumatoid arthritis. Lancet 2:305–307
Fielder M, Tiwana H, Youinou P, Le Goff P, Deonarain R, Wilson C, Ebringer A (1995) The specificity of the anti-Proteus antibody response in tissue-typed rheumatoid arthritis (RA) patients from Brest. Rheumatol Int 15:79–82
Tani Y, Tiwana H, Hukuda S, Nishioka J, Fielder M, Wilson C, Bansal S, Ebringer A (1997) Antibodies to Klebsiella, Proteus, and HLA-B27 peptides in Japanese patients with ankylosing spondylitis and rheumatoid arthritis. J Rheumatol 24:109–114
Wanchu A, Deodhar SD, Sharma M, Gupta V, Bambery P, Sud A (1997) Elevated levels of anti-proteus antibodies in patients with active rheumatoid arthritis. Indian J Med Res 105:39–42
Rashid T, Darlington G, Kjeldsen-Kragh J, Forre O, Collado A, Ebringer A (1999) Proteus IgG antibodies and C-reactive protein in English, Norwegian and Spanish patients with rheumatoid arthritis. Clin Rheumatol 18:190–195
Newkirk MM, Goldbach-Mansky R, Senior BW, Klippel J, Schumacher HR Jr, El-Gabalawy HS (2005) Elevated levels of IgM and IgA antibodies to Proteus mirabilis and IgM antibodies to Escherichia coli are associated with early rheumatoid factor (RF)-positive rheumatoid arthritis. Rheumatology (Oxford) 44:1433–1441
Ebringer A, Cunningham P, Ahmadi K, Wrigglesworth J, Hosseini R, Wilson C (1992) Sequence similarity between HLA-DR1 and DR4 subtypes associated with rheumatoid arthritis and proteus/serratia membrane haemolysins. Ann Rheum Dis 51:1245–6
Wilson C, Ebringer A, Ahmadi K, Wrigglesworth J, Tiwana H, Fielder M, Binder A, Ettelaie C, Cunningham P, Joannou C, et al. (1995) Shared amino acid sequences between major histocompatibility complex class II glycoproteins, type XI collagen and Proteus mirabilis in rheumatoid arthritis. Ann Rheum Dis 54:216–20
Senior BW, Anderson GA, Morley KD, Kerr MA (1999) Evidence that patients with rheumatoid arthritis have asymptomatic 'non-significant' Proteus mirabilis bacteriuria more frequently than healthy controls. J Infect 38:99–106
Albani S, Tuckwell JE, Esparza L, Carson DA, Roudier J (1992) The susceptibility sequence to rheumatoid arthritis is a cross-reactive B cell epitope shared by the Escherichia coli heat shock protein dnaJ and the histocompatibility leukocyte antigen DRB10401 molecule. J Clin Invest 89:327–331
Alspaugh MA, Henle G, Lennette ET, Henle W (1981) Elevated levels of antibodies to Epstein-Barr virus antigens in sera and synovial fluids of patients with rheumatoid arthritis. J Clin Invest 67:1134–1140
Kyttaris VC (2013) Systemic lupus erythematosus: from genes to organ damage. Methods Mol Biol 662:265–283
Nagai K, Arito M, Takakuwa Y, Ooka S, Sato T, Kurokawa MS, Okamoto K, Uchida T, Suematsu N, Kato T (2012) Altered posttranslational modification on U1 small nuclear ribonucleoprotein 68k in systemic autoimmune diseases detected by 2D Western blot. Electrophoresis 33:2028–2035
Zhang X, Ma H, Huang J, Dai Y (2013) Characterization of the phosphoproteome in SLE patients. PLoS One 7:e53129
Dieker J, Muller S (2009) Post-translational modifications, subcellular relocation and release in apoptotic microparticles: apoptosis turns nuclear proteins into autoantigens. Folia Histochem Cytobiol 47:343–348
Saal JG, Steidle M, Einsele H, Muller CA, Fritz P, Zacher J (1992) Persistence of B19 parvovirus in synovial membranes of patients with rheumatoid arthritis. Rheumatol Int 12:147–51
Dolcino M, Zanoni G, Bason C, Tinazzi E, Boccola E, Valletta E, Contreas G, Lunardi C, Puccetti A (2013) A subset of anti-rotavirus antibodies directed against the viral protein VP7 predicts the onset of celiac disease and induces typical features of the disease in the intestinal epithelial cell line T84. Immunol Res 56:465–476
Cunningham MW, McCormack JM, Fenderson PG, Ho MK, Beachey EH, Dale JB (1989) Human and murine antibodies cross-reactive with streptococcal M protein and myosin recognize the sequence GLN-LYS-SER-LYS-GLN in M protein. J Immunol 143:2677–2683
Sfriso P, Ghirardello A, Botsios C, Tonon M, Zen M, Bassi N, Bassetto F, Doria A (2010) Infections and autoimmunity: the multifaceted relationship. J Leukoc Biol 87:385–395
Shahrizaila N, Yuki N. Guillain-Barre syndrome animal model: the first proof of molecular mimicry in human autoimmune disorder. J Biomed Biotechnol 2011: 829129
Albert LJ (2000) Infection and rheumatoid arthritis: guilt by association? J Rheumatol 27:564–566
Delogu LG, Deidda S, Delitala G, Manetti R (2011) Infectious diseases and autoimmunity. J Infect Dev Ctries 5:679–687
Munz C, Lunemann JD, Getts MT, Miller SD (2009) Antiviral immune responses: triggers of or triggered by autoimmunity? Nat Rev Immunol 9:246–258
Croker BA, Lawson BR, Rutschmann S, Berger M, Eidenschenk C, Blasius AL, Moresco EM, Sovath S, Cengia L, Shultz LD, Theofilopoulos AN, Pettersson S, Beutler BA (2008) Inflammation and autoimmunity caused by a SHP1 mutation depend on IL-1, MyD88, and a microbial trigger. Proc Natl Acad Sci U S A 105:15028–15033
Gershwin ME, Mackay IR (2008) The causes of primary biliary cirrhosis: convenient and inconvenient truths. Hepatology 47:737–745
Wakabayashi K, Lian ZX, Leung PS, Moritoki Y, Tsuneyama K, Kurth MJ, Lam KS, Yoshida K, Yang GX, Hibi T, Ansari AA, Ridgway WM, Coppel RL, Mackay IR, Gershwin ME (2008) Loss of tolerance in C57BL/6 mice to the autoantigen E2 subunit of pyruvate dehydrogenase by a xenobiotic with ensuing biliary ductular disease. Hepatology 48:531–540
Leung PS, Park O, Tsuneyama K, Kurth MJ, Lam KS, Ansari AA, Coppel RL, Gershwin ME (2007) Induction of primary biliary cirrhosis in guinea pigs following chemical xenobiotic immunization. J Immunol 179:2651–2657
Billiau A, Matthys P (2001) Modes of action of Freund's adjuvants in experimental models of autoimmune diseases. J Leukoc Biol 70:849–860
von Herrath MG, Dockter J, Oldstone MB (1994) How virus induces a rapid or slow onset insulin-dependent diabetes mellitus in a transgenic model. Immunity 1:231–242
Getts MT, Miller SD. 99th Dahlem conference on infection, inflammation and chronic inflammatory disorders: triggering of autoimmune diseases by infections. Clin Exp Immunol 160: 15-21
Klein K, Ospelt C, Gay S (2012) Epigenetic contributions in the development of rheumatoid arthritis. Arthritis Res Ther 14:227
Smolen J, Aletaha D (2008) The burden of rheumatoid arthritis and access to treatment: a medical overview. Eur J Health Econ 8(Suppl 2):S39–S47
Vander Cruyssen B, Peene I, Cantaert T, Hoffman IE, De Rycke L, Veys EM, De Keyser F (2005) Anti-citrullinated protein/peptide antibodies (ACPA) in rheumatoid arthritis: specificity and relation with rheumatoid factor. Autoimmun Rev 4:468–474
Wagner E, Skoumal M, Bayer PM, Klaushofer K (2009) Antibody against mutated citrullinated vimentin: a new sensitive marker in the diagnosis of rheumatoid arthritis. Rheumatol Int 29:1315–1321
Schellekens GA, de Jong BA, van den Hoogen FH, van de Putte LB, van Venrooij WJ (1998) Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest 101:273–281
Nielen MM, van Schaardenburg D, Reesink HW, van de Stadt RJ, van der Horst-Bruinsma IE, de Koning MH, Habibuw MR, Vandenbroucke JP, Dijkmans BA (2004) Specific autoantibodies precede the symptoms of rheumatoid arthritis: a study of serial measurements in blood donors. Arthritis Rheum 50:380–386
van Gaalen FA, Linn-Rasker SP, van Venrooij WJ, de Jong BA, Breedveld FC, Verweij CL, Toes RE, Huizinga TW (2004) Autoantibodies to cyclic citrullinated peptides predict progression to rheumatoid arthritis in patients with undifferentiated arthritis: a prospective cohort study. Arthritis Rheum 50:709–715
Yamada R, Suzuki A, Chang X, Yamamoto K (2003) Peptidylarginine deiminase type 4: identification of a rheumatoid arthritis-susceptible gene. Trends Mol Med 9:503–508
Takahara H, Sugawara K (1986) Peptidylarginine deiminase, protein-arginine deiminase and protein-L-arginine iminohydrolase. Tanpakushitsu Kakusan Koso 31:1654–1660
Vossenaar ER, Zendman AJ, van Venrooij WJ, Pruijn GJ (2003) PAD, a growing family of citrullinating enzymes: genes, features and involvement in disease. Bioessays 25:1106–1118
Nakashima K, Hagiwara T, Yamada M (2002) Nuclear localization of peptidylarginine deiminase V and histone deimination in granulocytes. J Biol Chem 277:49562–49568
Luo Y, Arita K, Bhatia M, Knuckley B, Lee YH, Stallcup MR, Sato M, Thompson PR (2006) Inhibitors and inactivators of protein arginine deiminase 4: functional and structural characterization. Biochemistry 45:11727–11736
Senshu T, Kan S, Ogawa H, Manabe M, Asaga H (1996) Preferential deimination of keratin K1 and filaggrin during the terminal differentiation of human epidermis. Biochem Biophys Res Commun 225:712–719
Pritzker LB, Nguyen TA, Moscarello MA (1999) The developmental expression and activity of peptidylarginine deiminase in the mouse. Neurosci Lett 266:161–164
Wang Y, Li M, Stadler S, Correll S, Li P, Wang D, Hayama R, Leonelli L, Han H, Grigoryev SA, Allis CD, Coonrod SA (2009) Histone hypercitrullination mediates chromatin decondensation and neutrophil extracellular trap formation. J Cell Biol 184:205–213
Lewis RS (2001) Calcium signaling mechanisms in T lymphocytes. Annu Rev Immunol 19:497–521
Stensland ME, Pollmann S, Molberg O, Sollid LM, Fleckenstein B (2009) Primary sequence, together with other factors, influence peptide deimination by peptidylarginine deiminase-4. Biol Chem 390:99–107
Vossenaar ER, Radstake TR, van der Heijden A, van Mansum MA, Dieteren C, de Rooij DJ, Barrera P, Zendman AJ, van Venrooij WJ (2004) Expression and activity of citrullinating peptidylarginine deiminase enzymes in monocytes and macrophages. Ann Rheum Dis 63:373–381
Vossenaar ER, Smeets TJ, Kraan MC, Raats JM, van Venrooij WJ, Tak PP (2004) The presence of citrullinated proteins is not specific for rheumatoid synovial tissue. Arthritis Rheum 50:3485–3494
Lundberg K, Nijenhuis S, Vossenaar ER, Palmblad K, van Venrooij WJ, Klareskog L, Zendman AJ, Harris HE (2005) Citrullinated proteins have increased immunogenicity and arthritogenicity and their presence in arthritic joints correlates with disease severity. Arthritis Res Ther 7:R458–R467
Padyukov L, Seielstad M, Ong RT, Ding B, Ronnelid J, Seddighzadeh M, Alfredsson L, Klareskog L (2013) A genome-wide association study suggests contrasting associations in ACPA-positive versus ACPA-negative rheumatoid arthritis. Ann Rheum Dis 70:259–265
Schellekens GA, Visser H, de Jong BA, van den Hoogen FH, Hazes JM, Breedveld FC, van Venrooij WJ (2000) The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum 43:155–163
Kastbom A, Strandberg G, Lindroos A, Skogh T (2004) Anti-CCP antibody test predicts the disease course during 3 years in early rheumatoid arthritis (the Swedish TIRA project). Ann Rheum Dis 63:1085–1089
Chapuy-Regaud S, Nogueira L, Clavel C, Sebbag M, Vincent C, Serre G (2005) IgG subclass distribution of the rheumatoid arthritis-specific autoantibodies to citrullinated fibrin. Clin Exp Immunol 139:542–550
Takizawa Y, Suzuki A, Sawada T, Ohsaka M, Inoue T, Yamada R, Yamamoto K (2006) Citrullinated fibrinogen detected as a soluble citrullinated autoantigen in rheumatoid arthritis synovial fluids. Ann Rheum Dis 65:1013–1020
Van Steendam K, Tilleman K, De Ceuleneer M, De Keyser F, Elewaut D, Deforce D. Citrullinated vimentin as an important antigen in immune complexes from synovial fluid of rheumatoid arthritis patients with antibodies against citrullinated proteins. Arthritis Res Ther 12: R132
Suzuki A, Yamada R, Ohtake-Yamanaka M, Okazaki Y, Sawada T, Yamamoto K (2005) Anti-citrullinated collagen type I antibody is a target of autoimmunity in rheumatoid arthritis. Biochem Biophys Res Commun 333:418–426
Kinloch A, Tatzer V, Wait R, Peston D, Lundberg K, Donatien P, Moyes D, Taylor PC, Venables PJ (2005) Identification of citrullinated alpha-enolase as a candidate autoantigen in rheumatoid arthritis. Arthritis Res Ther 7:R1421–R1429
Pitzalis C, Kelly S, Humby F (2013) New learnings on the pathophysiology of RA from synovial biopsies. Curr Opin Rheumatol 25:334–344
Amara K, Steen J, Murray F, Morbach H, Fernandez-Rodriguez BM, Joshua V, Engstrom M, Snir O, Israelsson L, Catrina AI, Wardemann H, Corti D, Meffre E, Klareskog L, Malmstrom V (2013) Monoclonal IgG antibodies generated from joint-derived B cells of RA patients have a strong bias toward citrullinated autoantigen recognition. J Exp Med 210:445–455
Kollipara L, Zahedi RP (2013) Protein carbamylation: in vivo modification or in vitro artefact. Proteomics 13:941–944
Cantaert T, De Rycke L, Bongartz T, Matteson EL, Tak PP, Nicholas AP, Baeten D (2006) Citrullinated proteins in rheumatoid arthritis: crucial…but not sufficient! Arthritis Rheum 54:3381–3389
Klareskog L, Catrina AI, Paget S (2009) Rheumatoid arthritis. Lancet 373:659–672
Shi J, van de Stadt LA, Levarht EW, Huizinga TW, Toes RE, Trouw LA, van Schaardenburg D (2013) Anti-carbamylated protein antibodies are present in arthralgia patients and predict the development of rheumatoid arthritis. Arthritis Rheum 65:911–915
Wang Z, Nicholls SJ, Rodriguez ER, Kummu O, Horkko S, Barnard J, Reynolds WF, Topol EJ, DiDonato JA, Hazen SL (2007) Protein carbamylation links inflammation, smoking, uremia and atherogenesis. Nat Med 13:1176–1184
Khandpur R, Carmona-Rivera C, Vivekanandan-Giri A, Gizinski A, Yalavarthi S, Knight JS, Friday S, Li S, Patel RM, Subramanian V, Thompson P, Chen P, Fox DA, Pennathur S, Kaplan MJ (2013) NETs are a source of citrullinated autoantigens and stimulate inflammatory responses in rheumatoid arthritis. Sci Transl Med 5:178
Garnotel R, Sabbah N, Jaisson S, Gillery P (2004) Enhanced activation of and increased production of matrix metalloproteinase-9 by human blood monocytes upon adhering to carbamylated collagen. FEBS Lett 563:13–16
Jaisson S, Delevallee-Forte C, Toure F, Rieu P, Garnotel R, Gillery P (2007) Carbamylated albumin is a potent inhibitor of polymorphonuclear neutrophil respiratory burst. FEBS Lett 581:1509–1513
Mydel P, Wang Z, Brisslert M, Hellvard A, Dahlberg LE, Hazen SL, Bokarewa M, Mydel P, Wang Z, Brisslert M, Hellvard A, Dahlberg LE, Hazen SL, Bokarewa M (2010) Carbamylation-dependent activation of T cells: a novel mechanism in the pathogenesis of autoimmune arthritis. J Immunol 184:6882–6890
Shi J, Willemze A, Janssen GM, van Veelen PA, Drijfhout JW, Cerami A, Huizinga TW, Trouw LA, Toes RE (2013) Recognition of citrullinated and carbamylated proteins by human antibodies: specificity, cross-reactivity and the 'AMC-Senshu' method. Ann Rheum Dis 72:148–150
Lefevre S, Knedla A, Tennie C, Kampmann A, Wunrau C, Dinser R, Korb A, Schnaker EM, Tarner IH, Robbins PD, Evans CH, Sturz H, Steinmeyer J, Gay S, Scholmerich J, Pap T, Muller-Ladner U, Neumann E (2009) Synovial fibroblasts spread rheumatoid arthritis to unaffected joints. Nat Med 15:1414–1420
Ospelt C, Gay S (2008) The role of resident synovial cells in destructive arthritis. Best Pract Res Clin Rheumatol 22:239–252
Wang Z, Zang C, Cui K, Schones DE, Barski A, Peng W, Zhao K (2009) Genome-wide mapping of HATs and HDACs reveals distinct functions in active and inactive genes. Cell 138:1019–1031
Grabiec AM, Reedquist KA (2010) Histone deacetylases in RA: epigenetics and epiphenomena. Arthritis Res Ther 12:142
Strahl BD, Allis CD (2000) The language of covalent histone modifications. Nature 403:41–45
Trenkmann M, Brock M, Gay RE, Kolling C, Speich R, Michel BA, Gay S, Huber LC (2011) Expression and function of EZH2 in synovial fibroblasts: epigenetic repression of the Wnt inhibitor SFRP1 in rheumatoid arthritis. Ann Rheum Dis 70:1482–1488
Jang MS, Ryu SW, Kim E (2002) Modification of Daxx by small ubiquitin-related modifier-1. Biochem Biophys Res Commun 295:495–500
Okura T, Gong L, Kamitani T, Wada T, Okura I, Wei CF, Chang HM, Yeh ET (1996) Protection against Fas/APO-1- and tumor necrosis factor-mediated cell death by a novel protein, sentrin. J Immunol 157:4277–4281
Meinecke I, Cinski A, Baier A, Peters MA, Dankbar B, Wille A, Drynda A, Mendoza H, Gay RE, Hay RT, Ink B, Gay S, Pap T (2007) Modification of nuclear PML protein by SUMO-1 regulates Fas-induced apoptosis in rheumatoid arthritis synovial fibroblasts. Proc Natl Acad Sci U S A 104:5073–5078
Ebringer A, Wilson C, Tiwana H (2000) Is rheumatoid arthritis a form of reactive arthritis? J Rheumatol 27:559–563
Ebringer A, Rashid T, Wilson C (2010) Rheumatoid arthritis, Proteus, anti-CCP antibodies and Karl Popper. Autoimmun Rev 9:216–223
Gregersen PK, Silver J, Winchester RJ (1987) The shared epitope hypothesis. An approach to understanding the molecular genetics of susceptibility to rheumatoid arthritis. Arthritis Rheum 30:1205–1213
Hammer J, Gallazzi F, Bono E, Karr RW, Guenot J, Valsasnini P, Nagy ZA, Sinigaglia F (1995) Peptide binding specificity of HLA-DR4 molecules: correlation with rheumatoid arthritis association. J Exp Med 181:1847–1855
Baum H, Wilson C, Tiwana H, Ahmadi K, Ebringer A (1995) HLA association with autoimmune disease: restricted binding or T-cell selection? Lancet 346:1042–1043
Wilson C, Tiwana H, Ebringer A, Cunningham P, Ettelaie C (1997) HLA-DR4 restriction, molecular mimicry and rheumatoid arthritis. Immunol Today 18:96–97
Roudier C, Auger I, Roudier J (1996) Molecular mimicry reflected through database screening: serendipity or survival strategy? Immunol Today 17:357–358
Hill JA, Southwood S, Sette A, Jevnikar AM, Bell DA, Cairns E (2003) Cutting edge: the conversion of arginine to citrulline allows for a high-affinity peptide interaction with the rheumatoid arthritis-associated HLA-DRB1*0401 MHC class II molecule. J Immunol 171:538–541
Choi J, Kim ST, Craft J (2012) The pathogenesis of systemic lupus erythematosus-an update. Curr Opin Immunol 24:651–657
Anderton SM (2004) Post-translational modifications of self antigens: implications for autoimmunity. Curr Opin Immunol 16:753–758
Routsias JG, Tzioufas AG (2010) B-cell epitopes of the intracellular autoantigens Ro/SSA and La/SSB: tools to study the regulation of the autoimmune response. J Autoimmun 35:256–264
Terzoglou AG, Routsias JG, Avrameas S, Moutsopoulos HM, Tzioufas AG (2006) Preferential recognition of the phosphorylated major linear B-cell epitope of La/SSB 349-368 aa by anti-La/SSB autoantibodies from patients with systemic autoimmune diseases. Clin Exp Immunol 144:432–439
Zieve GW, Khusial PR (2003) The anti-Sm immune response in autoimmunity and cell biology. Autoimmun Rev 2:235–240
Brahms H, Raymackers J, Union A, de Keyser F, Meheus L, Luhrmann R (2000) The C-terminal RG dipeptide repeats of the spliceosomal Sm proteins D1 and D3 contain symmetrical dimethylarginines, which form a major B-cell epitope for anti-Sm autoantibodies. J Biol Chem 275:17122–17129
Hoch SO, Eisenberg RA, Sharp GC (1999) Diverse antibody recognition patterns of the multiple Sm-D antigen polypeptides. Clin Immunol 92:203–208
Barakat S, Briand JP, Weber JC, van Regenmortel MH, Muller S (1990) Recognition of synthetic peptides of Sm-D autoantigen by lupus sera. Clin Exp Immunol 81:256–262
Dieker JW, Fransen JH, van Bavel CC, Briand JP, Jacobs CW, Muller S, Berden JH, van der Vlag J (2007) Apoptosis-induced acetylation of histones is pathogenic in systemic lupus erythematosus. Arthritis Rheum 56:1921–1933
van Bavel CC, Dieker J, Muller S, Briand JP, Monestier M, Berden JH, van der Vlag J (2009) Apoptosis-associated acetylation on histone H2B is an epitope for lupus autoantibodies. Mol Immunol 47:511–516
Doyle HA, Aswad DW, Mamula MJ (2013) Autoimmunity to isomerized histone H2B in systemic lupus erythematosus. Autoimmunity 46:6–13
Akaogi J, Barker T, Kuroda Y, Nacionales DC, Yamasaki Y, Stevens BR, Reeves WH, Satoh M (2006) Role of non-protein amino acid L-canavanine in autoimmunity. Autoimmun Rev 5:429–435
Rosenthal GA (1990) Metabolism of l-canavanine and l-canaline in leguminous plants. Plant Physiol 94:1–3
Jang MH, Jun DY, Rue SW, Han K, Park W, Kim YH (2002) Arginine antimetabolite L-canavanine induces apoptotic cell death in human Jurkat T cells via caspase-3 activation regulated by Bcl-2 or Bcl-xL. Biochem Biophys Res Commun 295:283–288
Malinow MR, Bardana EJ Jr, Pirofsky B, Craig S, McLaughlin P (1982) Systemic lupus erythematosus-like syndrome in monkeys fed alfalfa sprouts: role of a nonprotein amino acid. Science 216:415–417
Alcocer-Varela J, Iglesias A, Llorente L, Alarcon-Segovia D (1985) Effects of L-canavanine on T cells may explain the induction of systemic lupus erythematosus by alfalfa. Arthritis Rheum 28:52–57
Bengtsson AA, Rylander L, Hagmar L, Nived O, Sturfelt G (2002) Risk factors for developing systemic lupus erythematosus: a case-control study in southern Sweden. Rheumatology (Oxford) 41:563–571
McClain MT, Heinlen LD, Dennis GJ, Roebuck J, Harley JB, James JA (2005) Early events in lupus humoral autoimmunity suggest initiation through molecular mimicry. Nat Med 11:85–89
James JA, Robertson JM (2012) Lupus and Epstein-Barr. Curr Opin Rheumatol 24:383–388
Csuka D, Simon D, Hobor R, Uray K, Prohaszka Z, Banlaki Z, Jani PK, Szilagyi A, Hudecz F, Rajczy K, Beke G, Boros Major A, Tordai A, Illes Z, Berki T, Czirjak L, Fust G (2013) Serum concentration of immunoglobulin G-type antibodies against the whole Epstein-Barr nuclear antigen 1 and its aa35-58 or aa398-404 fragments in the sera of patients with systemic lupus erythematosus and multiple sclerosis. Clin Exp Immunol 171:255–262
Sundar K, Jacques S, Gottlieb P, Villars R, Benito ME, Taylor DK, Spatz LA (2004) Expression of the Epstein-Barr virus nuclear antigen-1 (EBNA-1) in the mouse can elicit the production of anti-dsDNA and anti-Sm antibodies. J Autoimmun 23:127–140
Yadav P, Tran H, Ebegbe R, Gottlieb P, Wei H, Lewis RH, Mumbey-Wafula A, Kaplan A, Kholdarova E, Spatz L (2011) Antibodies elicited in response to EBNA-1 may cross-react with dsDNA. PLoS One 6:e14488
Wang F (2013) Nonhuman primate models for Epstein-Barr virus infection. Curr Opin Virol 3:233–237
Poole BD, Templeton AK, Guthridge JM, Brown EJ, Harley JB, James JA (2009) Aberrant Epstein-Barr viral infection in systemic lupus erythematosus. Autoimmun Rev 8:337–342
Zhang W, Reichlin M (2008) A possible link between infection with Burkholderia bacteria and systemic lupus erythematosus based on epitope mimicry. Clin Dev Immunol 2008:683489
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, DEG PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA (2006) International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost 4:295–306
Pierangeli SS, Chen PP, Raschi E, Scurati S, Grossi C, Borghi MO, Palomo I, Harris EN, Meroni PL (2008) Antiphospholipid antibodies and the antiphospholipid syndrome: pathogenic mechanisms. Semin Thromb Hemost 34:236–250
Miyakis S, Giannakopoulos B, Krilis SA (2004) Beta 2 glycoprotein I—function in health and disease. Thromb Res 114:335–346
Galli M, Comfurius P, Maassen C, Hemker HC, de Baets MH, van Breda-Vriesman PJ, Barbui T, Zwaal RF, Bevers EM (1990) Anticardiolipin antibodies (ACA) directed not to cardiolipin but to a plasma protein cofactor. Lancet 335:1544–1547
de Groot PG, Derksen RH (2004) Pathophysiology of antiphospholipid antibodies. Neth J Med 62:267–272
Agar C, van Os GM, Morgelin M, Sprenger RR, Marquart JA, Urbanus RT, Derksen RH, Meijers JC, de Groot PG (2011) Beta2-glycoprotein I can exist in 2 conformations: implications for our understanding of the antiphospholipid syndrome. Blood 116:1336–1343
Passam FH, Giannakopoulos B, Mirarabshahi P, Krilis SA (2011) Molecular pathophysiology of the antiphospholipid syndrome: the role of oxidative post-translational modification of beta 2 glycoprotein I. J Thromb Haemost 9(Suppl 1):275–282
Giannakopoulos B, Krilis SA (2013) The pathogenesis of the antiphospholipid syndrome. N Engl J Med 368:1033–1044
Delgado Alves J, Ames PR, Donohue S, Stanyer L, Nourooz-Zadeh J, Ravirajan C, Isenberg DA (2002) Antibodies to high-density lipoprotein and beta2-glycoprotein I are inversely correlated with paraoxonase activity in systemic lupus erythematosus and primary antiphospholipid syndrome. Arthritis Rheum 46:2686–2694
Charakida M, Besler C, Batuca JR, Sangle S, Marques S, Sousa M, Wang G, Tousoulis D, Delgado Alves J, Loukogeorgakis SP, Mackworth-Young C, D'Cruz D, Luscher T, Landmesser U, Deanfield JE (2009) Vascular abnormalities, paraoxonase activity, and dysfunctional HDL in primary antiphospholipid syndrome. JAMA 302:1210–1217
Ames PR, Nourooz-Zadeh J, Tommasino C, Alves J, Brancaccio V, Anggard EE (1998) Oxidative stress in primary antiphospholipid syndrome. Thromb Haemost 79:447–449
Ioannou Y, Zhang JY, Qi M, Gao L, Qi JC, Yu DM, Lau H, Sturgess AD, Vlachoyiannopoulos PG, Moutsopoulos HM, Rahman A, Pericleous C, Atsumi T, Koike T, Heritier S, Giannakopoulos B, Krilis SA (2011) Novel assays of thrombogenic pathogenicity in the antiphospholipid syndrome based on the detection of molecular oxidative modification of the major autoantigen beta2-glycoprotein I. Arthritis Rheum 63:2774–2782
Kondo A, Miyamoto T, Yonekawa O, Giessing AM, Osterlund EC, Jensen ON (2009) Glycopeptide profiling of beta-2-glycoprotein I by mass spectrometry reveals attenuated sialylation in patients with antiphospholipid syndrome. J Proteomics 73:123–133
Giannakopoulos B, Mirarabshahi P, Krilis SA (2011) New insights into the biology and pathobiology of beta2-glycoprotein I. Curr Rheumatol Rep 13:90–95
Urbanus RT, Derksen RH, de Groot PG (2008) Current insight into diagnostics and pathophysiology of the antiphospholipid syndrome. Blood Rev 22:93–105
Koning F (2012) Celiac disease: quantity matters. Semin Immunopathol 34:541–549
Caputo I, Lepretti M, Martucciello S, Esposito C (2010) Enzymatic strategies to detoxify gluten: implications for celiac disease. Enzyme Res 2010:174354
Sollid LM (2000) Molecular basis of celiac disease. Annu Rev Immunol 18:53–81
Dewar DH, Donnelly SC, McLaughlin SD, Johnson MW, Ellis HJ, Ciclitira PJ (2012) Celiac disease: management of persistent symptoms in patients on a gluten-free diet. World J Gastroenterol 18:1348–1356
Blanco A (1995) Genética de la Enfermedad Celiaca. Bol Pediatr 36:39–50
Smyth DJ, Plagnol V, Walker NM, Cooper JD, Downes K, Yang JH, Howson JM, Stevens H, McManus R, Wijmenga C, Heap GA, Dubois PC, Clayton DG, Hunt KA, van Heel DA, Todd JA (2008) Shared and distinct genetic variants in type 1 diabetes and celiac disease. N Engl J Med 359:2767–2777
Caglar E, Ugurlu S, Ozenoglu A, Can G, Kadioglu P, Dobrucali A (2009) Autoantibody frequency in celiac disease. Clinics (Sao Paulo) 64:1195–1200
Kumar V, Wijmenga C, Withoff S (2012) From genome-wide association studies to disease mechanisms: celiac disease as a model for autoimmune diseases. Semin Immunopathol 34:567–580
Sollid LM, Jabri B (2011) Celiac disease and transglutaminase 2: a model for posttranslational modification of antigens and HLA association in the pathogenesis of autoimmune disorders. Curr Opin Immunol 23:732–738
Qiao SW, Raki M, Gunnarsen KS, Loset GA, Lundin KE, Sandlie I, Sollid LM (2011) Posttranslational modification of gluten shapes TCR usage in celiac disease. J Immunol 187:3064–3071
Bushara KO (2005) Neurologic presentation of celiac disease. Gastroenterology 128:S92–S97
Armstrong D, Don-Wauchope AC, Verdu EF (2011) Testing for gluten-related disorders in clinical practice: the role of serology in managing the spectrum of gluten sensitivity. Can J Gastroenterol 25:193–197
Bushara KO, Goebel SU, Shill H, Goldfarb LG, Hallett M (2001) Gluten sensitivity in sporadic and hereditary cerebellar ataxia. Ann Neurol 49:540–543
Alaedini A, Okamoto H, Briani C, Wollenberg K, Shill HA, Bushara KO, Sander HW, Green PH, Hallett M, Latov N (2007) Immune cross-reactivity in celiac disease: anti-gliadin antibodies bind to neuronal synapsin I. J Immunol 178:6590–6595
Selmi C, Bowlus CL, Gershwin ME, Coppel RL (2011) Primary biliary cirrhosis. Lancet 377:1600–1609
Howard MJ, Fuller C, Broadhurst RW, Perham RN, Tang JG, Quinn J, Diamond AG, Yeaman SJ (1998) Three-dimensional structure of the major autoantigen in primary biliary cirrhosis. Gastroenterology 115:139–146
Vijayakrishnan S, Kelly SM, Gilbert RJ, Callow P, Bhella D, Forsyth T, Lindsay JG, Byron O (2010) Solution structure and characterisation of the human pyruvate dehydrogenase complex core assembly. J Mol Biol 399:71–93
Leung PS, Wang J, Naiyanetr P, Kenny TP, Lam KS, Kurth MJ, Gershwin ME (2013) Environment and primary biliary cirrhosis: electrophilic drugs and the induction of AMA. J Autoimmun 41:79–86
Naiyanetr P, Butler JD, Meng L, Pfeiff J, Kenny TP, Guggenheim KG, Reiger R, Lam K, Kurth MJ, Ansari AA, Coppel RL, Lopez-Hoyos M, Gershwin ME, Leung PS (2011) Electrophile-modified lipoic derivatives of PDC-E2 elicits anti-mitochondrial antibody reactivity. J Autoimmun 37:209–216
Odin JA, Huebert RC, Casciola-Rosen L, LaRusso NF, Rosen A (2001) Bcl-2-dependent oxidation of pyruvate dehydrogenase-E2, a primary biliary cirrhosis autoantigen, during apoptosis. J Clin Invest 108:223–232
Acknowledgments
We would like to thank Martha Cristina Fernandez-Chairez for her contribution to image creation and editing.
Conflict of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zavala-Cerna, M.G., Martínez-García, E.A., Torres-Bugarín, O. et al. The Clinical Significance of Posttranslational Modification of Autoantigens. Clinic Rev Allerg Immunol 47, 73–90 (2014). https://doi.org/10.1007/s12016-014-8424-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-014-8424-0