Abstract
Human γδ T cells, which play innate and adaptive, protective as well as destructive, roles in the immune response, were discovered in 1986, but the clinical significance of alterations of the levels of these cells in the peripheral blood in human diseases has not been comprehensively reviewed. Here, we review patterns of easily measurable changes of this subset of T cells in peripheral blood from relevant publications in PubMed and their correlations with specific disease categories, specific diagnoses within disease categories, and prognostic outcomes. These collective data suggest that enumeration of γδ T cells and their subsets in the peripheral blood of patients could be a useful tool to evaluate diagnosis and prognosis in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intensive research in the 1980s led to the discovery of the rearranging α and β genes encoding the αβ T cell receptor (TCR), which is expressed on CD4+ and CD8+ T cells [1–4]. However, at that time, the role of a third, rearranging gene, γ, initially detected in a clone of cytotoxic T cells expressing the αβ TCR, remained a mystery [5]. The enigma of the γ gene was resolved when lymphocytes bearing γδ TCR, were unveiled in 1986 [6, 7]. In those studies, clones of CD4− and CD8− cytotoxic and cytokine producing thymocytes and peripheral blood (PB) T cells expressing a CD3-associated heterodimeric TCR encoded by the γ gene, along with a novel polypeptide encoded by an additional rearranging gene, δ were derived from human thymus and the PB of patients with immunodeficiencies [6, 7]. Although subsequent studies revealed major functional overlap between T cells expressing either γδ or αβ TCR (γδ or αβ T cells, respectively), modes of antigen recognition and activation of each subset are distinct. The most striking difference between the two subsets is the lack of requirement of antigen processing and presentation by major histocompatibility (MHC) molecules for γδ T cells, allowing more rapid response to their respective antigens [8]. Moreover, the antigenic repertoire of γδ T cells appears to be quite unique. Most striking, and as opposed to αβ T cells whose TCR are designed to recognize peptides presented by autologous MHC, an entire human γδ T cell subset, expressing a TCR heterodimer encoded by V (variable) γ9Vδ2 genetic combinations, is primed during infancy and early adulthood to respond to phosphorylated metabolic intermediates of bacteria and protozoa [9]. These cells also recognize (with lower affinity) corresponding intermediates of the mevalonate pathway (e.g., isopentenyl pyrophosphate, IPP) in eukaryotic cells that increase during cellular stress induced by infection, cancer, and inflammation [10]. Although the mechanism of recognition of the phosporylated moieties by the Vγ9Vδ2 TCR remains a mystery, recent data suggest involvement of butyrophillin CD277 as a molecule involved in sensing perturbations of IPP in target cells, which mediates Vγ9Vδ2 activation [11].
Importantly, exposure of Vγ9Vδ2 T cells to cells (e.g., monocytes, fibroblasts, tumor cells) expressing high levels of these non-peptidic antigens, initiates a cascade of clinically relevant immune responses including cytokine release, activation of other T cells, dendritic cells and B cells as well as potent cytotoxicity [9]. The second major human subset of γδ T cells expresses the Vδ1 gene, is located for the most part at mucosal surfaces, in particular within the lining epithelium as a significant proportion of the “intraepithelial T cell compartment” and appears to have specialized to recognize lipids presented by cluster of differentiation (CD) 1d [12]. Vδ1+ T cells, which for the most part are also CD4− and CD8− may also express CD8αα, are potent producers of cytokines and also mediate cytotoxicity against malignantly transformed cells. Table 1 summarizes major features of human γδ T cells in comparison with αβ T cells.
Excellent reviews of the basic biology of γδ T cells have been published highlighting their unique role in the murine and human immune systems [13–15]. Although many insights have been gleaned from studies of murine γδ T cells, including the mode of antigen recognition by the TCR, processes of differentiation in the thymus, and the emergence of subsets during intrathymic differentiation, striking differences between murine and human γδ T cells are evident. For example, an entire subset of murine γδ T cells known as dendritic T cells (DETC), all expressing a single TCR, densely populates the murine epidermis, but an equivalent population is not present in human skin. Another intriguing difference is that in murine systems, recent data have clearly differentiated a population of γδ T cells that are primed during differentiation to produce interleukin (IL) -17, a cytokine that plays a crucial role in inflammatory responses, and these cells continue to secrete this cytokine in the periphery [16]. Although human γδ T cells also can produce IL-17 after stimulation, this function has not as yet been linked to a clearly defined subset, but may be context dependent in the periphery. Thus, for example, activation of Vγ9Vδ2+ cells with IPP in the presence of IL-1β, IL-23, IL-6, and TGFβ and aromatic hydrocarbons, will result in the induction of secretion of IL-17 in cells with a CD45RA+CCR6+CD161+TRAIL+FasL+ phenotype [17]. Conversely, there is no equivalent of the human phosphoantigen-reactive Vγ9Vδ2 T cells in mice. Thus, the role of γδ T cells in murine models of immune regulation and disease may not appropriately simulate the corresponding human situation. On the other hand, primates, whose immune system is similar to humans and includes a phosphoantigen-reactive subset, are much less amenable to extensive experimentation [18]. These considerations imply that in order to understand more fully the role of the unique γδ T cell subset in humans, direct evaluation of these cells in human health and disease are crucial.
Indeed, the unique roles and significance of γδ T cells during human clinical disease are gradually being uncovered. In particular, perturbations of numbers and phenotype of γδ T cells in PB and in tissues have been observed in cancer, infections, allergy, and autoimmunity, and individual studies suggest that these alterations can be related to specific diseases and carry prognostic implications. However, enumeration of γδ T cells in PB has not as yet entered routine clinical practice, which hampers further progress in understanding how these crucial immune cells participate in human health.
To evaluate whether numerically measurable perturbations of PB γδ T cells and their subsets could indeed serve as a useful clinical tool, we reviewed studies available in the PubMed database reporting numerical evaluations and alterations of these cells in human diseases, with the exclusion of primary immunodeficiency syndromes and malignant conditions of the γδ T cells themselves.
In the following sections, we detail alterations in levels of PB γδ T cells in physiological conditions and within specific diseases. The combined results of this review suggest that enumeration of PB γδ T cells could be an important tool in routine clinical practice in a variety of conditions. Importantly, because many of the studies report analysis of both total numbers and percentages of these cells, as well as subsets within the total population of γδ T cells, we herein provide a brief review of how human γδ T cells are divided into further subsets, and the significance of each.
Human γδ T Cell Subsets
The primary division within the human γδ T cell subsets is based on the expression of the V region genes of the γ and δ TCR chains. Cells expressing Vγ9 and Vδ2 (Vγ9Vδ2 T cells) are present mainly in PB and lymphoid organs. In contrast, those expressing Vδ1 with a gene other than Vγ9 within the TCRγ polypeptide are more prevalent in tissues. Major characteristics of each of these subsets, in comparison to the major subsets of αβ T cells are summarized in Table 1. A second fundamental classification pertains to the status of the cells with respect to previous antigen stimulation and acquisition of a memory or effector functional status. Most commonly this classification is applied to the Vγ9Vδ2 subset, for which antigens (IPP and (E)-4-hydroxy-3-methyl-but-2-enyl pyrophosphate, HMBPP) have been identified, and is based on the expression of surface membrane markers CD45RO, CD45RA, and CD27. Thus, CD27+CD45RA+CD45RO− are thought to represent naïve cells, a CD27+CD45RO+CD45RA− phenotype is a hallmark of a “central memory” cell (TCM), whereas CD27−CD45RA− cells are effector memory γδ T cells (TEM). A further subset is CD27−CD45RA+ and known as TEMRA, i.e., effector memory terminally differentiated cells that express potent cytotoxic functions. Other markers associated with subsets of γδ T cells are chemokine and cytokine receptors, and cytokines secreted by specific subsets. The functions of each subset are designated in Table 2, which is based on data presented in reviews by Pang et al. and Kabeliz [17, 19].
Association of γδ T Cell Alterations in Peripheral Blood with Physiological Conditions in Humans
Age
Age is associated with numerical alterations of γδ T cells and their subsets. Vδ1 cells predominate during fetal and early life in the PB of humans. In most studies, these represent the minority in the PB of adults, whereas Vδ2 cells, which exhibit features of cells previously activated by antigens (“memory” T cells) constitute the majority of adult.
PB γδ T Cells [20]. O’Leary first noted that elderly (>69 years old) patients among clinic subjects with chronic disease (e.g., osteoarthritis or congestive heart failure) had a consistent decrease in the percent of CD3+ lymphocytes due to a 5−10 % reduction of CD3+, TCRαβ-negative (i.e., γδ T cell receptor bearing) T cells in the peripheral blood mononuclear cell (PBMC) population compared to young adults [21]. This absolute number of circulating γδ T cells was shown to be reduced significantly in old people and centenarians in comparison with young subjects as a result of an age-dependent reduction of Vδ2 T cells, whereas the absolute number of Vδ1 T cells was unaffected by age. The decreased absolute number of the Vγ9Vδ2 T cells was due to the reduction of naive (antigen inexperienced) and “central” memory (antigen experienced) cells capable of circulating in the lymphatic system) Vγ9Vδ2 T cells bearing the CD27 and CCR7 cell surface molecules [22]. A comprehensive study confirmed that Vγ9Vδ2 T cell numbers change characteristically with age, rising from birth to puberty and gradually decreasing again beyond 30 years of age. In adults, female blood donors have significantly higher levels than males, implying that circulating Vγ9δ2 T cells in women remain elevated for a longer period in life. In this study, the loss (in men) was associated with depletion of effector memory CD27− CD45RA− and CD27− CD45RA+ T cells and a parallel increase in CD27+ CD45RA− central memory T cells, while in women, the distribution of Vγ9Vδ2 T cell subsets remained virtually unchanged [23]. Similar finding were reported in 120 healthy Japanese individuals in whom the average numbers of T lymphocytes in a cubic millimeter blood were 1,084 ± 369 (SD) αβ T cells, 68 ± 44 γδ T cells, 16 ± 12 Vδ1 T cells, and 43 ± 36 Vδ2 T cells and the absolute numbers of γδ T cells decreased with aging (R = −0.378, P < 0.001) as a result of reduction of Vδ2, but not of Vδ1, T cells. However, in this study, numbers of Vδ2 T cells were significantly higher in male than in female donors [24]. Interestingly, the decrease of total γδ T cells with age (4 % in young vs 2 % in the old) is also influenced by cytomegalovirus infection status, being limited to uninfected individuals, whereas the decrease of Vδ2 T cells specifically, occurs in both cytomegalovirus (CMV)+ and in CMV− individuals (from 4 to 0.8), along with an increase in Vδ2− γδ T cells (0.9 to 2) only in CMV+ individuals (Fig. 1) [25]. γδ T cells from old people and centenarians show enhanced levels of the early cell surface membrane activation marker CD69 both after culture in medium alone and in lipopolysaccharide (LPS), a basal increased production of TNFα and an impaired response to IPP [26]. In another study, a higher percentage of γδ T cells producing TNFα, but not IFNγ, was found in old donors and centenarians [27].
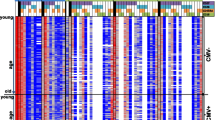
Variation of peripheral blood (PB) γδ T cells with age (a) and race (b). a Mean of percent of indicated γδ T cell subsets of among CD3+ T cells (bars) or absolute numbers of cells per cubic millimeter of PB (lines) are shown in relation to age groups indicated on abscisse. Data is based on ref. [22–24]. b Mean of percent among CD3+ T cells of indicated γδ T cell subsets. Bars below and to the right of indicated references (ref) represent values quoted from the referenced studies
Race and Origin
The frequency of PB γδ T cells in healthy West Africans was reported to be about twice that of Caucasians, but mainly due to a fivefold increase in Vδ1+ cells, which is consequently the dominant subset in West Africans (Fig. 1b) [28]. Indeed, in adult European donors the major γδ T cell population in PB is Vγ9+ (approximately 70 % of all γδ cells), whereas in the majority of adult Africans Vγ9− Vδ1+ T cells predominated (approximately 70 % of total γδ cells) [29]. Likewise, substantial differences in the Vγ9 repertoire for cord blood collected in Jos (Nigeria, a malaria endemic endemic) or Rome were noted, which were consistent with a negative selection mechanism operating on the fetal Vγ9 chain repertoire in neonates from Jos, perhaps due to exposure to malaria, as discussed below [30]. In the USA, Caucasian donors had 3.71 ± 4.37 % Vδ2 cells (as a percentage of total lymphocytes in PB) compared with 1.18 ± 2.14 % Vδ2 cells for African American donors (P < 0.0001). In addition, age as well as race had the greatest impact on Vδ2 cell levels, and the effect of age was similar for both racial groups [31] (Fig. 1b). Finally, in Sweden, the percentage of γδ T cells was higher in Bangladeshi than Swedish subjects [32]. Thus, genetic as well as environmental influences are clearly important in determining the composition and numbers of γδ T cells in human PB.
Pregnancy
In PB of healthy pregnant women the percentage of γδ TCR+ cells was significantly higher than in recurrent aborters or non-pregnant individuals. Interestingly, 97 % of γδ TCR+ pregnancy lymphocytes expressed progesterone receptor [33].
Alterations of γδ T cells in Diseases:
Infectious Disease
Human Acquired Immunodeficiency Syndrome (HIV)
Expansion of Vδ1 T cells occurs in both HIV-1 and HIV-2 infections but is accompanied by a significant contraction of the Vδ2 T cell population only in the former [34] (Fig. 2). Nevertheless, Vδ2 T cell activation was increased in both HIV-1− and HIV-2 and did not revert after treatment with highly active antiretroviral therapy (HAART) [34, 35]. Likewise, the high prevalence of memory (CD45RO+) and HLA-DR expressing Vδ1+ T cells in HIV-1-infected patients, but not in healthy donors, indicates antigenic activation of these cells in HIV-1 [36]. Furthermore, compared with healthy HIV-negative subjects, HIV+ patients had a total decreased number of IFNγ+ γδ T cells due to a decrease of the number of Vγ9Vδ2 cells, whereas the number of IFN-γ+Vδ1+ cells was actually increased [37]. Indeed, at variance with healthy donors, in HIV-1-infected patients, ex vivo-isolated Vδ1 T cells co-express cytoplasmic proinflammatory cytokines IFNγ and IL-17, as well as CD27, the surface marker of the central memory T cell subset [38]. In another study, HIV-1 infection was associated with significant expansion of Vδ1 and contraction of Vδ2 cell populations in mucosa in addition to PB during both acute and chronic HIV-1 [35]. Furthermore, the γδ–intraepithelial lymphocyte (IEL) ratio (median 14.5 %, range 1.5–56.3 %) was significantly increased compared with clinically healthy HIV (−) control subjects (n = 11, median 2.8 %; range 0.3–38 %) [39]. Thus HIV is associated with activation of γδ T cells, with enhancement and activation of the Vδ1 and depletion of the Vδ2 subsets. Interestingly however, in HIV patients naive to antiretroviral therapy, combined treatment with intravenous zoledronate (zol) and sub-cutaneous IL-2, induced in vivo expansion and maturation of their Vδ2 T cells. Paralleling Vδ2 T cell activation, increased dendritic cell maturation and HIV-specific CD8 T cell responses were found [40].
Peripheral blood (PB) γδ T cell subsets in human immunodeficiency virus-1 (HIV-1) and tuberculosis (TB). Mean percent of indicated γδ T cell subsets among CD3+ T cells, based on references indicated above and to the left of each set of values, are shown. Clinical status of studied groups is described along x-axis. ref, reference
Tuberculosis (TB)
Among health care workers who were tuberculin skin test positive and had constant contact with patients with active TB (“healthy contacts”) the percent of γδ T cells in fresh PB was significantly higher than in healthy noncontacts (Fig. 2). By contrast, patients with active pulmonary tuberculosis had low levels of γδ T cells [41]. The general decrease of γδ T cells, however, is accompanied by expansion of central memory Vγ9Vδ2 T cells and reduction of the pool of effector memory (CD45RO+) and terminally differentiated cells (CD45RA+), which reversed after anti-mycobacterial therapy [42]. Further analysis in active pulmonary tuberculosis showed, moreover, that the size of the mycobacteria-reactive Vγ9+Vδ2+γδ T cell subset in both the blood and lung was dramatically reduced compared with both normal healthy subjects and patients with unrelated pulmonary granulomatous diseases—sarcoidosis and berylliosis. In addition, the Vγ9+Vδ2+cells left intact in patients with tuberculosis were refractory to in vitro stimulation by mycobacteria tuberculosis antigens which are potent stimuli for these cells in normal subjects [43] [44] [45] (Fig. 2). In another study of 27 patients with active pulmonary tuberculosis and 16 healthy donors (HD), the proportion of total IL-17-producing cells among lymphocyte was similar between TB patients and HD, but the proportions of γδ T cells in IL-17-producing cells and of IL-17-producing cells in γδ T cells in PB were markedly increased in TB patients (43.9 and 7.7 %, respectively) contrasting with lower levels of IFNγ-producing γδ T cells [46]. γδ T cells were also studied in tuberculosis-infected 24 HIV patients—11 with and 13 without immune reconstitution syndrome (IRS) that sometimes occurs after institution of highly active anti-retroviral therapy (HAART). At baseline, lower proportions of γδ T cells and Vδ2+ T cells and of those displaying the inhibitory receptors CD94/NKG2 and CD158ah,b (Killer inhibitory receptors, KIR) were found in the patients who developed IRS. During IRS, Vδ2+ T cells, mostly KIR−, significantly peaked as opposed to non-IRS patients suggesting that KIR(−)Vδ2+ γδ T cells play an immunoregulatory role in HIV patients developing IRS [47].
Parasitic Infections
Malaria
In Ethiopia, γδ+ T cells were significantly elevated in patients infected with malaria falciparum (f) and in those doubly infected with f. malaria and vivax malaria but not in vivax malaria alone, compared to healthy controls, and the increase was mostly due to Vδ1+ cells (Fig. 3)[48]. Likewise, in Ghanaian children, both frequency and absolute number of γδ T cells, again mostly highly activated and polyclonal Vδ1 cells, were transiently increased to 30 to 50 % of all T cells shortly after initiation of antimalarial chemotherapy for plasmodium falciparum malaria [49] (Fig. 3). Furthermore, among nine non-immune patients who contracted malaria during travel to endemic areas (five with Plasmodium falciparum and four with Plasmodium vivax infections) γδ T lymphocytes expanded to comprise 17.92 ± 11 % of the PBMC (vs 3.08 ± 2.4 % γδ cells in normal control subjects). In these patients, Vδ2+ cells predominated, although cells expressing Vδ1 also expanded significantly in some patients. The mean level of γδ cells peaked during the second month after the acute clinical syndrome, when patients were free of symptoms [50] (Fig. 3). In another study of non-immune patients, a highly significant increase in both the proportion and the absolute numbers of γδ T cells up to 30 % of PBMC, was observed in Plasmodium vivax-infected patients during clinical paroxysms compared to nonmalarial controls. Curiously, in an age-matched group of semi-immune patients resident in a malaria-endemic region, in whom the clinical disease was comparatively mild, there was no increase in γδ T cells during infection during paroxysms or convalescence [51] (Fig. 3). The potential strong effect of malaria exposure on γδ T cell subsets is highlighted by the finding of a substantial difference in the Vγ9 repertoire for cord blood collected in Nigeria, a malaria endemic country and a non-endemic region (Rome, Italy) consistent with a negative selection mechanism (perhaps exposure to malaria) operating on the fetal Vγ9 chain repertoire in Nigerian neonates [30].
Variation of γδ T cells in malaria. Mean percent of indicated γδ T cell subsets among peripheral blood CD3+ T cells, based on references (ref) indicated above and to the left of each set of values, are shown. Clinical status of studied groups is described along the x-axis. f, falciparum; v, vivax; double, vivax plus falciparum; d, day after infection
Other Parasites
Among 20 patients with local cutaneous leishmaniasis, significantly more γδ T cells were observed in untreated patients (15.9 ± 5.9 %), when compared with glucantime-treated patients (4.6 ± 1.4 %) and controls (5.3 ± 2.3 %)[52]. In addition, pregnant women with primary toxoplasmosis displayed a significant decrease of the CD4/CD8 T cell ratio concurrent with a significant increase of circulating γδ T cells compared to uninfected counterparts [53].
Viral Diseases Other than HIV
Cytomegalovirus (CMV), Epstein Barr Virus (EBV), and Human Herpes Virus (HHV)-8 Infections
During the first 24 months after stem cell transplantation, significant long-term expansions of Vδ2 negative (−) but not Vδ2+ γδ T cells was noted in patients with CMV reactivation early after transplantation. Similarly, significantly higher numbers of Vδ2− γδ T cells were detected in CMV-seropositive healthy persons compared with seronegative donors. In contrast Vδ2− γδ T cell expansion was absent in CMV-negative/Epstein–Barr virus-positive patients [54] (Fig. 4). Effector memory γδ T cells likewise showed a concomitant increase and persistence in most kidney transplant recipients with CMV infection [55] (Fig. 4). Furthermore, a dramatic expansion of activated γδ T cells in the PB of renal allograft recipients developing CMV infection lasted more than 1 year, and involved only Vδ1 or Vδ3+ T cells [56]. A comprehensive study of circulating γδ T cells in renal allograft recipients, using multivariate analysis confirmed that CMV infection was the only independent parameter associated with >6 % γδ T cells [57] (Fig. 4). Importantly, patients who developed a delayed γδ T cell expansion after CMV infection (≥45 days) had significantly longer and higher pp65 antigenemia and more-symptomatic CMV disease than did patients with early expansion. Furthermore, γδ T cell expansion was concomitant with the resolution of CMV infection [58] (Fig. 4). Fetal Vγ9-γδ T cells also specifically expand and become differentiated upon CMV infection in utero [59]. At a functional level, Vδ2− γδ T cell PB numbers, repertoire restriction, and cytotoxicity against CMV-infected fibroblasts were markedly increased in CMV seropositive, compared with CMV seronegative, healthy persons and exhibited a cytotoxic effector/memory phenotype only in the CMV+ patients [60]. Together, these data strongly support an important role of Vδ2− in response to and resolution of CMV. In other studies, protractedly (up to 5 months) elevated γδ T cell component occurs in Epstein Barr Virus (EBV) related but not EBV negative, infectious mononucleosis. HHV-8 infection has also been associated with significant expansion of effector γδ Vδ1+ T cells, suggesting an important role of γδ T cells in herpes virus infection in general [61, 62] [63].
γδ T cells in cytomegalovirus (CMV) infections after kidney transplants. Absolute number or percentage among peripheral blood CD3+ T cells (secondary y-axis, bars indicated asterisk) of γδ T cell subsets based on references (ref) shown in the legend, along with subset measured, are shown. Plus sign and minus sign indicate patients with or without a CMV infection. H, healthy controls. m (number) = months after transplant of kidney
Other Viral Infections
γδ T cells from respiratory syncytial virus-infected infants included a lower proportion of IFNγ− (median, 4.00 %; range, 0.58–6.60 %) and a slightly higher proportion of IL-4-producing cells (median, 0.40 %; range, 0.13–2.76 %) than rotavirus-infected infants (median, 32.10 %; range, 14.43–61.21 %; P < 0.01, median [64]. In children with dengue hemorrhagic fever absolute γδ T cell counts were decreased compared with those with dengue fever early in the course of illness [65].
Bacterial Infections Other than Tuberculosis
Salmonella
Proportions of γδ T cells in Salmonella infections were significantly increased (17.9 ± 13.2 %) compared with normal controls (5.0 ± 2.6 %) and patients with other bacterial infections (4.0 ± 1.4 %). Furthermore, the most prominent expansions occurred in the systemic (28.9 ± 10.8 %) rather than in the gastroenteritic form (10.5 ± 7.9 %) of salmonellosis. Furthermore, γδ T cell activation was significantly greater than αβ T cell activation during early illness (Fig. 5) [66]. In addition, the proportion of γδ T cells expressing NKRP1A as well as IFNγ+NKRP1A+γδ T cells were significantly higher in Salmonella patients than in other intestinal infections or in healthy individuals [67]. Indeed, patients with Shigella dysenteriae and Shigella flexnerii revealed an expansion of γδ T cells in the rectal mucosa, but a decrease in blood compared to healthy age-matched controls [68].
In four patients with acute Coxiella burnetii infection Vγ9δ2 γδ T cells increased to a mean of 16 % (range, 13–30 %) as compared with five healthy (mean, 4 %) and pneumonia controls (2 %; range, 1–3 %; P < 0.0014) [69] (Fig. 5). In acute leptospirosis, a four- to fivefold increase in the number of PB γδ T cells was observed [70] (Fig. 5). Likewise, serial analyses of PBMC obtained from eight patients infected with Listeria monocytogenes showed a higher percentage of γδ T cells (median, 11.7; range, 3.7 to 35.3) than age-matched uninfected controls (median,1.7; range 0.4 to 13) and patient’s cells expressed significantly more HLA-DR [71] (Fig. 5). In 13 patients with tularemia, Vγ9δ2+ cells represented an average of 30.5 % of the CD3+ cells, (nearly 100 % of the PB γδ+ T cells), on days 7 to 18 after the onset of disease whereas after vaccination with the live vaccine strain of Francisella tularensis, only a minor increase was noted [72] (Fig. 5). Likewise, in ulcero glandular tularaemia, % Vγ9Vδ2 T cells within the first week of onset of disease did not differ from that of control subjects (5.3 ± 0. 8) but did increase rapidly on days 8–40 (mean > 20 %, P < 0.001). Of 45 individuals sampled within 3 months of onset, 42 had >10 % of Vγ9Vδ2 T cells. Moreover, significantly increased levels were still recorded at 18 but not at 24 months (10.2 ± 2.1 %; P > 0.10) [73]. Similarly, among 14 subjects undergoing a Pontiac fever-like disease caused by Legionella micdadei, a pronounced increase of γδ T cells occurred only 2 to 7 weeks after onset, with values slowly declining over 6 months, although without reaching the normal range [74]. In ehrlichiosis, in contrast, a course of antibiotic treatment (48–72 h) corrects the lymphocytopenia and is rapidly followed by a lymphocytosis of CD3+4-8− Vγ9Vδ2+ γδ T cells [75]. Patients with whooping-cough by contrast had significantly lower relative and absolute numbers of PB γδ T cells than normal controls [76] (Fig. 5). In two cases of psittacosis the number of γδ T cell in the bronchoalveolar lavage fluid was markedly increased, declining to normal range along with recovery of their radiographical findings [77]. Finally, in pediatric bacterial meningitis, γδ T cells producing IL-17 increased both in PB and cerebrospinal fluid, declining during therapy [78]. High levels of γδ T cells, mainly Vδ2+, have also been seen in pediatric and adults patients suffering from acute brucellosis (13.23 ± 4.7 and 5.25 ± 1.4, respectively (P = 0.0001) decreasing after treatment [79, 80] (Fig. 5). Taken together these data show strong and dynamic participation of γδ T cells in infections, with measurable and pathogen-related patterns of responses.
Cancer
Because of the anti-tumoral effects of γδ T cells, their potential therapeutic utility alterations of their subsets and correlation with cancer and its progression have been studied quite extensively. For example, the numbers of Vγ9+ γδ T cells and in particular, CD27− CD45RA− effector memory Vγ9+ subsets in PB were found to be significantly lower in 25 unselected advanced solid tumor cancer patients than in healthy subjects [81] (Fig. 6). Likewise γδ T cell counts and mitogen-stimulated proliferative response of γδ T cells were markedly decreased prior to glioblastoma multiforme (GBM) resection and throughout therapy (Fig. 6) [82]. However, others have not found a decrease of γδ T cells or Vγ9Vδ2 T cells in advanced cancer when analyzing small numbers of patients (Fig. 6) [83]. This discrepancy could be related to the nature of the alterations in the γδ T cell subset in specific forms of cancer, and stage of the disease. For example late effector memory (CD27−CD45RA+) Vγ9Vδ2 T cells (TEM RA) were significantly increased in nasopharyngeal carcinoma (NPC) with a corresponding decrease in central memory (CD27+CD45RO+) Vγ9Vδ2 T cells (TCM), compared to healthy controls. Moreover, TEM RA and TCM Vγ9Vδ2 cells from patients produced significantly less IFNγ and TNFα, suggesting impaired cytotoxic potential(Fig. 6) [84]. On the other hand, in squamous cell carcinoma of the head and neck, γδ T cells are significantly increased in PB (Fig. 6) [85]. Likewise, in gastric cancer, the frequency of Vδ1, but not Vδ2 or Vγ9 γδ T cells, in the malignant tissue is significantly lower than in normal gastric mucosa and they produce significantly less IFNγ, suggesting a defect of the Vδ1 subset specifically [86]. Conversely, the mean percentage of PB γδ T cells in 48 gastric cancer patients and 49 controls was 5.0 ± 3.4 and 2.3 ± 1.6 % respectively; moreover, 41.7 % of the patients had a high percentage (greater than 5 %) of PB γδ T cells compared to 8.2 % of the controls (Fig. 6) [87]. In American Joint Committee on Cancer (AJCC) stages I–III melanoma, the number of circulating γδ T cells was significantly increased compared with healthy individuals with γδ T cells producing TNFα or IFNγ increasing after melanoma removal (Fig. 6) [88] [89]. In another study including 41 patients who underwent surgery for renal cell carcinoma (RCC), 13 had stage III disease without metastasis. Those patients with peripheral γδ T cell greater than 8.7 % before surgery had better overall survival in a follow-up of 137 months. In contrast, five out of seven patients with a lower proportion of γδ T cells died [90].
γδ T cells in cancer patients. Mean absolute number per cubic millimeter of peripheral blood (PB) or percent of indicated γδ T cell subsets among PB CD3+ T cells (bars labeled asterisk, secondary y-axis), based on indicated references. GBM, glioblastoma multiforme; EM, effector memory; control>45 or control<45 indicate age of controls; NPC, nasopharyngeal carcinoma; SCC of H and N, squamous cell carcinoma of head and neck; LN, lymph node
Cancer Treatment
γδ T cells bearing the Vγ9Vδ2 TCR respond strongly to low molecular weight phosphorylated antigens in the mevalonate pathway, such as IPP, which are increased in cells by aminobisphosphonate inhibition of farnesyl pyrophosphorylase synthase (FPPS) [10]. Treatment of peripheral blood leukocytes with bisphosphonate reagents such as zoledronate (zol) or pamidronate thus leads to robust activation and proliferation of Vγ9Vδ2 T cells. Synthetic reagents mimicking the physiological activators IPP have also been developed and they can activate and expand γδ T cells. Due to the anti-cancer cell potential of Vγ9Vδ2 T cells, a number of clinical trials in which either Vγ9Vδ2 T cell-stimulating agents or ex-vivo expanded Vγ9Vδ2 T cells were used to treat solid tumor cancer have been designed.
Studies addressing γδ T cells in cancer patients who were treated with synthetic reagents mimicking the physiological activators (i.e., IPP) that activate and expand γδ T cells in vitro, e.g., reagent IPH1101 in combination with sub cutaneous (SC) low-dose IL-2 revealed a potent γδ T lymphocyte expansion in 28 solid tumor patients [91]. However, in 12 patients with metastatic RCC, only a modest increase in Vγ9Vδ2 T cell frequency could be detected by day 8 of therapy, in four of the nine patients who received at least one cycle of the bisphosphonate zoledronic acid together with low-dose IL-2 therapy. Furthermore, repeated administration actually diminished the in vivo percentage of Vγ9Vδ2 T cells. In this study, although no objective clinical responses were observed by response evaluation criteria in solid tumor (RECIST) criteria, two patients experienced prolonged stable disease [92]. In ten therapeutically terminal metastatic breast cancer patients administered zol plus low-dose IL-2, treatment was well tolerated and promoted effector maturation of Vγ9Vδ2 T cells. Seven patients who failed to sustain Vγ9Vδ2 T cells showed progressive clinical deterioration, while three patients who sustained robust peripheral Vγ9Vδ2 cell populations showed declining CA15-3 levels with one instance of partial remission and two of stable disease [93]. In another study, moreover, of 23 breast cancer patients, a single-dose (4 mg) of zol, with no follow-up of IL-2, induced a gradual and significant decrease of the different γδ T cell subsets, demonstrating a deleting effect of administration of zol in breast cancer patients [94]. In a phase I clinical trial in metastatic hormone-refractory prostate cancer, only two of nine patients treated with zol displayed a significant long-term shift of peripheral γδ cells toward an activated effector-memory-like state (TEM) associated with production of IFNγ and perforin, compared to induction of this phenotype in most of the patients who were treated with zol and IL-2. Numbers of TEM γδ T cells significantly correlated with declining prostate-specific antigen levels and objective clinical outcomes (three partial remissions and five stable disease). However, most patients treated with zol alone failed to sustain γδ cell numbers and deteriorated clinically [95].
In another set of phase I/II studies, cancer patients received intravenous infusions of ex vivo expanded autologous γδ cells. In seven advanced renal cell carcinoma (RCC) patients receiving these infusions, prolongation of tumor doubling time was observed in three of five in whom an increase in the number of PB γδ T cells was achieved [96]. In another phase I study, of metastatic RCC, infusion of Vγ9δ2 γδ T lymphocytes combined with a low dose of SC IL-2 resulted in initial clearance of Vγ9δ2 T from the blood, followed by their reappearance at the end of IL-2 administration [97]. An increase of γδ T cells was confirmed in non-small cell lung cancer ( NSCLC) patients, whose PBMC were stimulated and expanded with zol (5 μM) and IL-2 (1000 IU/mL) for 14 days ex vivo, followed by intravenous (IV) administration of harvested cells every 2 weeks. With increasing numbers of infusions, the number of PB γδ T cells gradually increased. Median survival was 589 days, median progression-free survival 126 days and no objective responses were observed. Six patients had stable disease, whereas 6 evaluable patients experienced progressive disease 4 weeks after the sixth transfer [98]. Finally, in a study of 25 patients with various solid tumors the numbers of CD3+ T cells, Vγ9+ γδ T cells and CD27− CD45RA− (memory) Vγ9+ subsets in PB were significantly lower in patients than in healthy subjects. Encouragingly, numbers and frequency of CD3+ Vγ9+ γδ T cells subsets significantly increased in patients treated with infusions of ex vivo zol-activated and expanded Vγ9+ γδ T cells [81]. Together these studies show that pharmacological activation of CD3+ Vγ9+ γδ T cells is feasible in cancer patients, and may have clinical implications, but requires further investigation and refining.
Development of cancer in post transplant patients has also yielded important insights into the roles of γδ T cells in cancer. A longitudinal case–control study involved 18 solid organ recipients who developed cancer between 2 and 6 years after transplantation and 45 recipients who did not. The median percentage of γδ T cells among total lymphocytes in patients with malignancies was significantly lower compared with control patients at evaluations 6, 12, and 18 months before the diagnosis of cancer. In contrast, patients with a γδ T cell percentage of more than 4 % were protected. An increase of the Vδ2− γδ T cell subset significantly associated with lower incidence of cancer only in recipients who experienced pre- or postgraft CMV infection. Interestingly, moreover, a retrospective follow-up of 131 recipients for 8 years revealed that CMV-naive recipients had an approximately fivefold higher risk of cancer compared with CMV-exposed patients [99].
Hematologic Malignancies
γδ Tcells (Vγ9Vδ2+) were reduced in PB of Burkitt Lymphoma patients whereas in follicular lymphoma, γδ T lymphocytes were normally expressed in PB but less abundant in lymph nodes (LN) compared to inflammatory-reactive LNs [100] [101]. In newly diagnosed acute myeloid leukemia (AML) absolute cell numbers of Vγ9δ2 T cells were normal in both PB and bone marrow, but with a preponderance of the effector memory population [102]. In acute leukemia patients, increased cytotoxic Vδ1+ T cells were seen in 10 of 43 patients receiving anti-αβ TCR monoclonal antibody (mAb) T10B9 T cell depleted (TCD) bone marrow transplants compared to only 7 of 100 of those receiving pan T cells mAb OKT3 TCD transplants (P = 0.010). Furthemore, the γδ T cells remained higher in the PB for a longer period of time. Patients with increased γδ T cells, whose grafts had been depleted with T10B9, showed a significant decrease in relapse, and estimated 3-year disease-free survival was significantly improved (0.79 vs 0.31, P = 0.009) [103]. γδ T cell levels were also collected prospectively in 77 acute lymphoblastic leukemia (ALL) and 76 acute myelogenous leukemia (AML) patients undergoing partially mismatched-related donor allogeneic stem cell transplants (ASCT). Patients received a partially T cell-depleted graft using T10B9 (n = 46) or OKT3 (n = 107). Five-years leukemia free survival (LFS) and overall survival (OS) of patients with increased γδ compared to those with normal/decreased numbers were 54.4 vs 19.1 %; P < 0.0003, and 70.8 vs 19.6 % P < 0.0001, respectively, with no difference in graft versus host disease (GvHD) (P = 0.96). Thus, γδ T cells may facilitate a graft-versus-leukemia effect, without causing GvHD [104]
Immune-Mediated Diseases (Autoimmune, Auto-Inflammatory, and Allergic)
Due to their ability to secrete inflammatory cytokines, regulate dendritic cell and B cell functions and contribute to tissue destruction and repair, γδ T cells appear to play an important role in auto immune allergic and auto inflammatory diseases. Moreover, as reviewed below, different subsets may play unique roles in discrete diseases.
Behcet’s Disease (BD)
γδ T cells accounted for 7.01 ± 4.42 % of the PBMCs in BD compared with 3.56 ± 3.45 % in Familial Mediterranean Fever (FMF, P < 0.005) and 3.7 ± 3.15 % in healthy individuals (P < 0.009) and their numbers were significantly higher during active disease than in remission (9.45 ± 5.08 vs 2.27 ± 3.3 %; P < 0.009) (Fig. 7) [105]. Likewise, the increased γδ T cells (and CD8+ γδ T cells) in BD patients exhibited increased expression of CD69, IFNγ and TNFα, compared with healthy controls [106] [107]. Also, CD45RA+Vγ9Vδ2+ γδ T cells, which constitute a minor population of γδ T cells in healthy individuals, were increased in number in BD irrespective of disease activity and, during active disease, co-expressed IL-2 receptors and HLA-DR (Fig. 7) [108]. Indeed, a significantly greater proportion of both Vδ1 and Vδ2 γδ T cell subsets were more highly activated in active BD compared to inactive BD or healthy controls [109]. Surprisingly, in one open prospective study of ten patients given 200 mg/day thalidomide for 12 weeks γδ T cells further increased at day 90 (11 vs 21 %) after treatment (Fig. 7) [110]. In contrast, CD56+ γδ T cells which were found to be significantly higher in active Behcet’s uveitis, normalized after treatment (Fig. 7) [111]. Importantly, γδ T cells were only observed in the ulcerated oral mucosa but not in the non-ulcerated mucosa from BD patients or healthy controls with no preferential expression of specific Vγ or Vδ chains [112]. Together, these reports indicate an important role of γδ T cells in the pathogenesis and immune regulation of BD.
γδ T cells in auto-immune diseases. Mean percent of indicated γδ T cell subsets among CD3+ T cells (solid bars) or absolute number per cubic millimeter of PB or (refs. [123] and [132], secondary y-axis), based on references (ref) indicated just before respective data bars, in the diseases on x-axis are shown. IGAN, IgA nephropathy; SLE, systemic lupus erythematosus, numbers indicate value for subset represented by adjacent bar inset; RA, rheumatoid arthritis; FMF, familial mediterranean fever. Inactive or active refers to listed disease. MS, multiple sclerosis; MRI magnetic resonance imaging
Auto Immune Arthritis; Rheumatoid Arthritis (RA), and Spondylarthritis
In one study, γδ T cells were significantly increased among the peripheral lymphocytes (5.5 ± 4 %) in RA and patients with primary Sjogren’s syndrome (SS) (4.75 ± 3.85 %) as compared with healthy subjects (2.09 ± 1.01 (P < 0.001 for RA; P < 0.004 for SS) (Fig. 7) [113]. A significant increase in the number of γδ-lymphocytes in the PB of patients with RA, especially in those with extra-articular manifestation of the disease, compared with normal controls, was likewise reported in a separate study [114]. On the other hand, significantly lower levels of γδ T cells were found by Smith et al. in RA [115]. Another group likewise reported that γδ T cells, expressed as a percentage of CD3+ lymphocytes, were reduced in RA PB compared with a control group (3.9 ± 0.5 vs 5.7 ± 0.7 %; P less than 0.0001) most notably with a reduction in the Vγ9δ2+ subset (from 5.6 ± 1.2 to 1.7 ± 0.4 %; Fig. 7) [116]. Data favoring a decrease in RA patients was further supported in a study of 17 psoriatic arthritis (PsA) and 16 RA patients who had, with respect to 27 healthy controls, lower values (both as percentages and in absolute numbers) of PB T cells expressing γδ TCR [117]. Liu et al. also found that RA patients had significantly lower levels of γδ T cells in PB than control subjects (1.38 ± 1.08 vs 3.23 ± 2.12 %, P < 0.05; Fig. 7) [118]. However, in yet another study, the percentages (mean ± SEM = 6.3 ± 0.8 %, n = 22) and absolute numbers (70 ± 11/μl, n = 22) of γδ T cells in PB from RA patients were no different from 22 age-matched healthy controls (7.5 ± 0.9 %, 81 ± 17/μl, respectively). The γδ T cells in PB from 50 RA patients were, however, significantly decreased in negative correlation with the value of C-reactive protein (CRP) although they had no correlation with the titer of rheumatoid factor (Fig. 7) [119]. On the other hand, in PB lymphocytes of 12 patients with adult Still’s disease, an unusual inflammatory systemic disease sometimes preceding RA, both the percentage and absolute number of γδ T cells in active disease (n = 6) were significantly higher than during inactive disease (n = 6), inactive RA patients (n = 8), or healthy controls (n = 20) [120]. Curiously, in contrast, during systemic juvenile idiopathic arthritis (JIA) disease flare, γδ T cells were reduced (Fig. 7) [121]. These conflicting results suggest involvement of γδ T cells in RA, which may be related to disease activity and stage. Interestingly, the single study addressing γδ T cells in ankylosing spondylitis (AS), revealed that the proportion of IL-23 receptor -expressing T cells in the periphery was twofold higher in AS patients than in healthy controls, specifically driven by a threefold increase of IL-23 receptor-positive γδ T cells [122].
Systemic Lupus Erythematosus (SLE)
Absolute numbers of cells expressing γδ TCR in most of 32 SLE blood specimens were significantly lower than in the control group (n = 16) (P < 0.006) whereas mean values of the percentage of γδ T cells among pan T lymphocytes were almost the same (7.1 vs 6.3 %, respectively). Furthermore, no differences between the numbers of γδ T lymphocytes were observed between patients with active and inactive disease. However, Vδ3+ T cells were higher in SLE patients (20 × 10 cells/μl) than in healthy controls (2 × 2 cells/μl) (P = 0.001) (Fig. 7) [123]. Another study, however, reported a significantly decreased number of γδ T cells in SLE patients (26.4 ± 16.9/μl) compared with a control group (55.3 ± 20.6/μl (P < 0.001) due to a decrease of Vδ2 TCR+and Vγ9 TCR+subpopulations; however, no correlation between disease activity and the number of γδ T cells was demonstrated [124]. Reduced γδ T cells in SLE were found to express activation markers, CD69 and reduced CD94 [125]. Another group reported that a Vδ1 γδ regulatory population, specifically decreased in the PB of SLE patients (Fig. 7) [126].
Takayasu Arteritis (TA)
γδ T cells in 20 patients with TA were increased (8.1 ± 5.1 %) compared to healthy controls, (n = 20, 3.7 ± 2.1 %, P = 0.014), RA (n = 10, 4.8 ± 0.6 %, P = 0.032), and Wegeners Granulomatosis patients (n = 5, 4.2 ± 0.8 %, P = 0.030). The increase was more prominent in active TA and associated with Vδ1+ cells, normalizing after 180 days of follow-up (Fig. 7) [127]. Immunopathologic analyses of vessel walls in TA revealed that the infiltrating cells consisted mainly of γδ T cells, αβ T cells and natural killer (NK) cells, which directly injured the vascular cells by releasing perforin [128].
Scleroderma
One study showed that percentage of Vδ1+ γδ T cells significantly increased among the PB T cells in scleroderma patients who did not have radiographic evidence of interstitial lung disease (ILD) (n = 7) compared to healthy controls and patients with ILD. Vγ9+ T cells were equally and persistently represented irrespective of pulmonary disease or cyclophosphamide treatment, at levels similar to healthy controls (Fig. 7) [129]. γδ T cells in scleroderma were also reported to express CD69 to a greater extent than controls, indicating their activation in vivo [130]. Others, on the other hand have reported decreases of γδ T cells in scleroderma (Fig. 7) [131]
Auto-Immune Neurological Diseases
Multiple Sclerosis
Among 20 multiple sclerosis (MS) patients presenting a first inflammatory event in the central nervous system, six showed intense magnetic resonance imaging (MRI) activity and had elevated CCR5+ γδT cells and total γδ T cells in the PB, which were not found in six patients without or with low MRI activity (Fig. 7) [132]. In addition, the percentage of CD16+ γδ T cells was elevated in MS patients compared with healthy controls especially in patients with a progressive course of the disease and the extent of elevation positively correlated with time of disease progression and severity [133]. A recent study confirmed elevated γδ T cells among PB CD3+ T cells in relapse of MS and clinically isolated syndrome (CIS) patients (7.4 ± 5.2 vs 3.6 ± 2.8 % in non-inflammatory disease controls), further showing specific elevation of the subset expressing CD161 and CCR6, markers associated with IL-17 production [134].
Opsoclonus Myoclonus (OMS)
In two studies by Pranzatelli et al., the absolute but not relative size of the γδ T cell subset was reduced (−44 %, P = 0.02) in paraneoplastic OMS [135]. In comparing cerebrospinal fluid (CSF) and blood of 36 children with OMS and 18 control subjects, most children with OMS had normal CSF cell counts but an expansion of γδ T cells (up to 26 %) subsets and a lower percentage of CD4+ T cells and CD4/CD8 ratio, which persisted even years after disease onset and conventional treatments. The percentage of activated CSF T cells was also higher. Abnormalities correlated with neurologic severity and disease duration [136].
Guillaine Barre Syndrome (GBS)
Serial flow cytometry studies revealed no significant difference in median γδ T cell percentages between GBS patients and controls at onset and at convalescence. However, five patients had marked Vδ1+ CD8+ elevations. Elevated Vδ1 or Vδ1+ CD8+ cells occurred in three of six patients with C jejuni or GM1 titer elevations [137].
Miscellaneous Autoimmune Diseases
A significant decrease of γδ TCR+cells in comparison to subjects after methimazole treatment as well as healthy controls has been observed in newly diagnosed Graves’ disease patients. A significant increase of γδ TCR+CD8+ cells in the PB of subjects with insulin-dependent diabetes, treated with insulin for 3–6 months, has also been noted [138]. Finally, the proportion of γδ T cells in PBMC was higher in IgAN patients than in controls and correlated with the proportion of surface IgA-positive B cells, which are precursors of IgA-secreting plasma cells (Fig. 7) [139].
Atopic Diseases
Asthma
The percentages of γδ T cells declined from 4.1 % in healthy to 3.2 % in allergic subjects and to a significantly lower 2.4 % in allergic asthmatics. The absolute numbers of circulating γδ T cells also were diminished in a similar fashion. In contrast, αβ T cells were comparable in healthy, allergic, and allergic asthmatic populations (Fig. 8) [140, 141]. Furthermore, in the PB of 26 adult patients with difficult-to-control asthma (DCA) and 22 patients with minimally symptomatic asthma (MSA) statistically significantly decreased relative and absolute numbers of γδ T cells (3.02 ± 2.16 % and 0.06 ± 0.04 × 10(9)/l), in comparison with controls (5.65 ± 2.90 % and 0.13 ± 0.08 × 10(9)/l), were found in the DCA patient group. Moreover, the relative and absolute numbers of γδ T cells were found to be diminished in both the allergy and nonallergy groups in comparison with healthy controls (Fig. 8) [142]. Interestingly, moreover, while smokers had elevated levels of PB γδ T cells, those developing COPD did not, suggesting that bronchial inflammation is associated with a relative decrease in γδ T cells in general [143]. Further support for a role of γδ T cells in asthma was demonstrated among 153 individuals, 95 with controlled asthma and 58 healthy controls, aged over 65 years. The γδ T cells were significantly decreased in the asthmatic patients compared to the controls (Fig. 8) [144]. Another study involving a group of patients with atopic disease including 11 children with atopic dermatitis, 20 with atopic asthma, and 18 adults with atopic dermatitis compared to 38 healthy age-matched controls aged 4–51 years, revealed, in the patients with atopic diseases, a significantly (P < 0.01) lower proportion of γδ T cells in PB compared with healthy controls (median 4.8 vs 7.1 %), as well as significantly lower proportions of CD8+ γδ T cells (Fig. 8) [145].
Asthma–Bronchoalveolar Lavage (BAL) and Induced Sputum γδ T Cells
In induced sputum collected from ten patients with acute exacerbation of asthma and from healthy controls, a significantly decreased proportion of αβ T cells and an increased proportion of γδ T cells, CD56+ cells and CD8+ γδ T cells were found in the asthma patients [146]. However, in asthmatics, no difference in the percentage of CD4+, CD8+, or γδ T cells in the BAL fluid before and after allergen challenge was observed. The major difference between the groups was manifested by an increased percentage of cells staining for the T helper-(Th)2-cytokines IL-5 and IL-13 in the γδ T cell subset [147]. In another study, BAL fluid of untreated atopic patients (six children and six adults) with mildly symptomatic chronic asthma was compared with BAL of ten healthy non-smoking volunteers and age-matched children with cystic fibrosis (n = 5) or anatomic malformation of the airways (n = 4). The proportion of γδ T lymphocytes, primarily CD4+ or CD4− CD8− cells, was higher in asthmatic patients than in controls. Most lung γδ CD4+ lymphocytes expressed the γδ T cell receptor Vδ1 chain, proliferated in response to allergen stimulation, underwent steroid-induced apoptosis in vitro, and disappeared after systemic steroid treatment [148]. Thus, in asthma whether allergic or non-allergic, γδ T cells are decreased peripherally and increased in the lungs, suggest in their important role in this group of diseases in humans.
Gastrointestinal and Liver Diseases
Liver Disease
γδ T cells have been studied in Hepatitis B virus (HBV) liver disease, autoimmune hepatitis (AIH) and in cirrhosis. A decreased proportion γδ T cells was observed in acute or chronic, compared to normal and chronic HBV disease, and was inversely proportional to liver enzyme elevations (Fig. 9) [149]. In addition, the proportion of circulating Vδ2 T cells among all γδ T cells was significantly decreased in patients with chronic HBV infection compared to healthy individuals (Fig. 9) [150]. On the other hand, γδT cells, in AIH patients were more numerous versus healthy controls, with an inverted Vδ1/Vδ2 ratio (Fig. 9) [151]. γδ T cells also play a role in infectious complications in liver diseases. γδ T cells were increased in bacterially infected ascites fluid of cirrhotic patients relative to non-infected ascites [152], whereas in patients with end-stage liver disease (ESLD) prior to orthotopic liver transplantation (OLT), the median total lymphocyte count and both γδ T cells in general and the Vδ2+ subset in particular, at baseline, were significantly lower in patients with compared with those without infection [153]. Furthermore, after liver, as well as kidney, transplantation, an increase of Vδ1 T cells occurred in PB of patients, in particular those with a stable transplant not requiring immunosuppression (Fig. 9) [154]
γδ T cells in liver diseases. Mean percent among peripheral blood (PB) CD3+ T cells or all PB mononuclear cells (asterisk) (solid bars) or number of cells per cubic millimeter of blood (hatched, secondary y-axis), in liver diseases indicated on the x-axis, of the indicated γδ T cell subsets based on references indicated above or to left of data bars. HBV, hepatitis B virus; AIH *, autoimmune hepatitis
Crohns Disease (CrD)
Conflicting results have been reported in CrD. In one study, γδ T subsets were lower in CrD patients (mean 0.0259 × 10(9)/l) versus healthy controls (mean 0.0769 × 10(9)/l, P < 0.001), in particular the CD8+ γδ T cell subset [155]. This decrease was associated moreover with an increase in the levels of IgE produced against Encephalitozoon cuniculi, a microsporidium whose presence in the gut was associated with CrD [156].
In contrast, others have reported that PB γδ T cells increased in patients with CrD compared with controls, with an elevated proportion expressing Vδ1 and Vγ8—genes typically used by intraepithelial lymphocytes [157]. Lastly, a more extensive analysis of 46 patients found that most had γδ− T cells level comparable to healthy individuals (mean 2.2 %), whereas 24 % exhibited an increased level of γδ T cells (5–15 %) expressing Vδ2. In four male patients with a high baseline value, the γδ− T cell population increased dramatically following infliximab therapy and was oligoclonal [158]. Together, these studies suggest marked perturbations within the γδ− T cell repertoire in CrD that may be influenced by immunosuppressive therapy.
Coeliac Disease (CoD)
Total circulating Vδ1+ lymphocytes among PB T cells were lower in 22 patients with untreated CoD compared with 16 healthy family members, whereas percentages of circulating CD45RO+ TCR γδ cells and CD45RO+ Vδ1+ cells were higher [159]. A series of studies addressed intraepithelial γδ T cells in CoD; patients had significantly higher levels of TCRγδ intraepithelial lymphocytes than patients with other enteropathies, Helicobacter pylori-associated gastritis, and 37 normal control patients [160]. Likewise, in both children and adult patients, duodenal intraepithelial TCR γδ lymphocytosis significantly differs from healthy individuals (although more markedly in children. However, increased CD3+ γδ T cells were diet and Marsh grade independent [161]. Indeed, increased γδ IELs exhibit a sensitivity of 93 % and specificity of 88 % for CoD [162]. Even reticulin autoantibody-positive children with normal jejunal mucosal morphology had significantly higher densities of intraepithelial γδ+ T cells than antibody-negative ones [163].
Gastritis
γδ T cell count in the mucosa was significantly higher in grade III gastritis with strong immunoglobulin (Ig)A and IgG responses to H. pylori urease than in grade II, I and normal mucosa. γδ T cell count significantly correlated with IL-1β and IL-7 levels in the gastric mucosa. An association was also seen between γδ T cell accumulation and H. pylori urease-specific Ig levels [164].
Dermatological Disease
Psoriasis
In psoriatic patients, a striking reduction of circulating Vγ9Vδ2 T cells compared with healthy controls and atopic dermatitis patients has been noted, that normalized after successful psoriasis-targeted therapy. Furthemore, a distinct subset of pro-inflammatory cutaneous lymphocyte Ag, CCR6-positive Vγ9Vδ2 T cells is rapidly recruited into the diseased skin, and Vγ9Vδ2 T cells produced IL-17A and activated keratinocytes in a TNFα- and IFNγ-dependent manner [165]. Other studies confirmed that the expression of TCR γδ was higher in guttate and plaque psoriasis than in normal skin [166] and that in psoriasis patients, γδ T cells were greatly increased in affected skin and produced large amounts of IL-17 [167].
Atopic Dermatitis (AD)
In one study, the percentage of circulating Vγ9Vδ2+ T lymphocytes was significantly increased in AD patients with respect to the age-matched controls, and a positive correlation with clinical score severity was found. Memory CD45RO+ CD62L+ Vδ2+ lymphocytes were significantly lower in AD patients. Furthermore, naive circulating Vδ2+ T lymphocytes were significantly lower in AD children than in age-matched controls. No correlation was observed between circulating Vγ9Vδ2 T cell expansion and IgE serum levels [168]. In another study, however, the frequencies of circulating NK cells and γδ T cells were both profoundly reduced in AD patients [169].
Miscellaneous Skin Diseases
In a granulomatous syndrome, due to a recessive genetic mutation in the TAP2 gene which is linked to the human leucocyte antigen (HLA) locus, both autoreactive NK cells and γδ T lymphocytes increased in the PB cells of two patients [170]. In Bullous pemphigoid, γδ T cells were reduced but rarely detected in lesional skin. In most patients, clinical remission and reduction of autoantibody titers after immunosuppressive therapy was not accompanied by an increase of circulating γδ T cells [171].
Miscellaneous Medical Conditions
Stress
Granulocytes, macrophages, NK cells, extrathymic T cells, γδ T cells, and CD8+ subset were all found to increase in the daytime (i.e., daytime rhythm) whereas, conversely total T cells, B cells, αβ T cells, and the CD4+ subset increased at night [172]. Both the Vδ1 and Vδ2 subsets were mobilized during stress, and for both subsets, TEMRA cells were mobilized to a much greater extent than the other memory phenotypes [173]. Acute psychological stress also significantly increased γδ T cells (5 to 5.55 % of CD3+ cells)[174].
During the severe systemic inflammatory response (SIRS) caused by trauma in 14 patients and by sepsis in 23 patients, the count of γδ T lymphocytes in the PB (30.1 ± 6.0/μl) was significantly lower than that of the healthy volunteers (104.3 ± 10.9/μl). The expression of CD69, an index of early activation of T lymphocytes, was significantly greater on γδ T lymphocytes from SIRS patients (patients 23.9 ± 3.4 %, healthy controls 4.8 ± 0.6 %, P < 0.05). In the trauma patients, the expression of CD69 on γδ T lymphocytes increased rapidly within 48 h after injuries [175]. However, trauma patients undergoing splenectomy had a sustained increase in the percentage and/or absolute numbers of lymphocytes, CD8 T cells, activated CD8 T cells, NK T cells, NK cells, and γδ T cells, and a reduction in naive CD4 T cells [176]. In an adult intensive care unit in a university hospital, a study of patients with septic shock (n = 21) and healthy individuals (n = 21) likewise revealed a decreased percentage of γδ T lymphocytes in PB (1 % [0.7–3.1], median [interquartile range]) in comparison with the healthy individuals (3.5 % [2.1–4.8])[177]. Furthermore, lower numbers of γδ T cells, in particular of CD56+ γδ T cells, in septic patients was the only marker (among all T cell subsets) significantly associated with death due to sepsis [178].
Immunodeficiency
In recombinase-activating gene deficiency (RAGD) with residual V(D)J activity (>1 % recombination activity of wild type), several clinical and immunological subtypes have been described: RAGD with skin inflammation and αβ T cell expansion (classical Omenn syndrome), RAGD with skin inflammation and without T cell expansion (incomplete Omenn syndrome), RAGD with γδ T cell expansion and RAGD with granulomas [179].
Transplantation
Phenotype, repertoire, and functional properties of γδ T cell subsets in a large population of allograft recipients were studied. Most immunosuppressed liver and kidney recipients displayed an enlarged PB γδ T cell pool mainly resulting from an expansion of Vδ1 T cells exhibiting an oligoclonal repertoire and different phenotypic and cytokine production traits than Vδ2 T cells [154]. In another study, the percentage of CD4 and CD8 T cells in transplanted patients was lower than in the control group (P < 0.001) with the exception of CD8 γδ T cells from patients with stable evolution (P > 0.05) [180].
Surgery
Blood samples from 24 children who underwent cardiac surgery with cardiopulmonary bypass (CPB) were collected serially to analyze TCR subsets by flow cytometry. The αβ T cells reached a nadir on postoperative day (POD) 1, but recovered to pre-CPB levels on POD 3. On the other hand, the γδ T cells decreased after CPB and did not recover to pre-CPB levels even after POD 7 [181]. In contrast, another study reported that the proportion of T cells bearing the γδ TCR as well as NK cells increased during CPB [182].
Effect of Bisphosphonates
In volunteers receiving 5 mg ZA by intravenous infusion, a transient fall in circulating Vγ9Vδ2 T cell levels at 48 h accompanied by increased serum levels of TNFα, IFNγ, IL-6, and CRP were found in ≥70 % of the study volunteers [183]. Likewise, a notable loss of Vγ9Vδ2 T cells occurred over time in osteoporotic patients on n-BP therapy, particularly those on IV therapy (n = 68) with no difference in total T cells, monocytes or granulocytes. The observed negative effect on Vγ9Vδ2 T cells coincided with the reported route of administration and timing of osteonecrosis of the jaw (ONJ). Six patients who had experienced ONJ were all significantly deficient in Vγ9Vδ2 T cells (median = 0.07 %) in comparison to age- and sex-matched treatment-naive controls (N = 11; median = 2.40 %), and this was the only consistent difference in the leukocytes assessed. All ONJ cases had an underlying condition that further contributed to impaired immunity [184].
Hemodialysis
Peripheral γδ T cells were decreased in hemodialysis patients suggesting that circulating γδ T cells are susceptible to activation-induced cell death in comparison with αβ T cells in uremic environments [185].
General Disease
Among 62 consecutive patients with >5 % γδ T cells of all PB T cells, more infectious, inflammatory, and autoimmune diseases were found than in controls [186].
Summary and Discussion
This review of the published literature reveals 91 conditions and diseases (C&D) in which a significant alteration of PB γδ T cells and their subsets, compared to healthy individuals or other diseases, were reported as detailed in Fig. 10. Increases of γδ T cells were reported in 41 and decreases in 39 C&D (Fig. 11a). As shown in Fig. 11b, 43.90 % (n = 18), 21.95 % (n = 9), 12.20 % (n = 5), 9.76 % (n = 4), and 7.32 % (n = 3) of reported increase of the cells were accounted for by infectious, autoimmune, malignant, GI and miscellaneous diseases respectively, and 4.8 % by medications. On the other hand, 27 % (n = 11), 22 % (n = 9), 17 % (n = 7), 17 % (n = 7), and 12 % (n = 5) of the C&D with decreased γδ T cells were auto-immune, infectious, malignant, miscellaneous, or gastrointestinal, respectively, in nature and 5% of decreases were pharmacologically induced.
a, b Summary of reported alterations in γδ T cells in disease. Increases (pointing left) or decreases (pointing right of upright axis) in γδ T cell and indicated subsets thereof, in physiological and disease conditions grouped according to categories indicated on the right of each diagram are shown. The specific diseases or conditions are indicated on the right of the y-axis with appropriate references in parenthesis
Distribution of γδ T cell alterations among disease categories. a Number of diseases from Fig. 10 (n = 82), in categories designated on the upright axis, in which increased or decreased γδ T cells or their subsets in peripheral blood (PB) have been described. b proportionate distribution of disease categories with increased (n = 41) or decreased (n = 41) γδ T cells in PB
Disease-related increases or decreases of each of the γδ T cells subsets in PB presumably reflect a perturbation of the homeostatic mechanisms that normally govern the levels of >these cells in PB in health. Mechanisms involved could include activating effects of disease-related antigens of cytokines or of chemokines leading to cell proliferation or apoptosis as well as disease-related effects on migration to and from lymphatic or peripheral tissues. For example, the preponderance of infectious diseases associated with increased γδ T cells in the PB probably reflects, for the most part, the strong activating effects of phosphorylated antigens in the alternative mevalonate pathway of pathogenic bacteria on the Vγ9 Vδ2 T cell subset [10]. In cancer and autoimmunity, antigenic influences are less well defined and are only recently being gradually uncovered. In these diseases, general dysregulation of the immune system via inflammatory and anti-inflammatory cytokines and chemokines produced in inflamed and malignant tissues presumably play an important role in the PB disease associated alterations of γδ T cells.
The possible pathogenic or protective significance of alteration of peripheral blood γδ T cells and their subsets should thus be viewed in the context of specific disease. For example, the strong activation of the Vγ9δ2 T cells by pathogenic organisms might augment, on the one hand, clearance of the offending organism by γδ T cell mediated mechanisms, while inducing severe tissue damage mediated by cytokines released by activated γδ T cells. In cancer, the reduction of anti-cancer cytotoxic γδ T cells observed in many instances might be supportive of cancer cell growth, whereas increased IL-17-producing γδ T cells might actually enhance tumor spread. Likewise, in autoimmunity γδ T cells could enhance inflammation, as well as induce apoptosis of proinflammatory and destructive cells.
Nevertheless, irrespective of the complex mechanism underlying the involvement of γδ T cells in each disease, analysis of the data collected here suggests that simple enumeration of these cells in PB of patients, albeit in the context of comparison to healthy age, sex, and race controls, may contribute, in the appropriate clinical setting, to diagnostic and prognostic evaluation of individual patients. For example, in the clinically common setting of a patient with undifferentiated peripheral arthritis, finding of elevated levels of γδ T cells would support a diagnosis of Behcet’s disease, rather than of SLE. Likewise, elevated γδ T cells might favor a diagnosis of psittacosis over pneumococcal pneumonia in the appropriate clinical setting. Elevated γδ T cells in a patient with undiagnosed glomerulonephritis might support IgA nephropathy rather than lupus glomerulonephritis. Finding elevated Vδ2− T cells in a transplant patient may indicate the development of a CMV infection, whereas a decreased Vγ9Vδ2 population may help differentiate psoriasis from atopic dermatitis. Elevated γδ T cells in bone marrow transplanted leukemic patients appear to suggest a better prognosis, and the same applies to development of cancer in solid transplant patients. On the other hand, finding a low level of γδ T cells in a cancer patient might enter clinical consideration of whether to administer zoledronate intravenously, since low levels of these cells are associated with increased chances of developing a devastating condition—osteonecrosis of the jaw. A summary of conditions in which differential diagnostic and prognostic value of enumerating peripheral blood γδ T cells may be potentially clinically relevant is presented in Table 3.
In summary, this paper represents an attempt to bring together, for the first time, data in the medical and scientific literature pertaining to the relationship of perturbations of γδ T cells in the peripheral blood of patients to medical conditions. Although most of the studies reported have as yet to be extended and substantiated, the current data suggests a strong potential for the clinical utility of a simple laboratory procedure—i.e., that of enumerating γδ T cells and their subsets in the peripheral blood—as a diagnostic and prognostic tool. Needless to say, much future study is required to substantiate this proposal.
References
Davis MM et al (1984) A murine T cell receptor gene complex: isolation, structure and rearrangement. Immunol Rev 81:235–258
Saito H et al (1984) Complete primary structure of a heterodimeric T-cell receptor deduced from cDNA sequences. Nature 309(5971):757–762
Royer HD et al (1984) Genes encoding the Ti beta subunit of the antigen/MHC receptor undergo rearrangement during intrathymic ontogeny prior to surface T3-Ti expression. Cell 39(2 Pt 1):261–266
Fabbi M et al (1984) Homology of Ti alpha-subunit of a T-cell antigen-MHC receptor with immunoglobulin. Nature 312(5991):269–271
Saito H et al (1984) A third rearranged and expressed gene in a clone of cytotoxic T lymphocytes. Nature 312(5989):36–40
Bank I et al (1986) A functional T3 molecule associated with a novel heterodimer on the surface of immature human thymocytes. Nature 322(6075):179–181
Brenner MB et al (1986) Identification of a putative second T-cell receptor. Nature 322(6075):145–149
Chien YH, Konigshofer Y (2007) Antigen recognition by gammadelta T cells. Immunol Rev 215:46–58
Nedellec S et al (2010) Human Vgamma9Vdelta2 T cells: from signals to functions. Semin Immunol 22(4):199–206
Kabelitz D et al (2000) Antigen recognition by human gammadelta T lymphocytes. Int Arch Allergy Immunol 122(1):1–7
Palakodeti A et al (2013) The molecular basis for modulation of human Vgamma9Vdelta2 T cell responses by CD277/butyrophilin-3 (BTN3A)-specific antibodies. J Biol Chem 287(39):32780–32790
Bai L et al (2012) The majority of CD1d-sulfatide-specific T cells in human blood use a semiinvariant Vdelta1 TCR. Eur J Immunol 42(9):2505–2510
Bonneville M et al (2010) Gammadelta T cell effector functions: a blend of innate programming and acquired plasticity. Nat Rev Immunol 10(7):467–478
Born WK et al (2011) Peptide antigens for gamma/delta T cells. Cell Mol Life Sci 68(14):2335–2343
Hayday AC (2000) [gamma][delta] cells: a right time and a right place for a conserved third way of protection. Annu Rev Immunol 18:975–1026
Roark CL et al (2008) gammadelta T cells: an important source of IL-17. Curr Opin Immunol 20(3):353–357
Pang DJ et al (2012) Understanding the complexity of gammadelta T-cell subsets in mouse and human. Immunology 136(3):283–290
Chen ZW (2013) Multifunctional immune responses of HMBPP-specific Vgamma2Vdelta2 T cells in M. tuberculosis and other infections. Cell Mol Immunol 10(1):58–64
Kabelitz D, He W (2012) The multifunctionality of human Vgamma9Vdelta2 gammadelta T cells: clonal plasticity or distinct subsets? Scand J Immunol 76(3):213–222
De Rosa SC et al (2004) Ontogeny of gamma delta T cells in humans. J Immunol 172(3):1637–1645
O’Leary JJ et al (1988) Expression of the human T cell antigen receptor complex in advanced age. Mech Ageing Dev 45(3):239–252
Re F et al (2005) Skewed representation of functionally distinct populations of Vgamma9Vdelta2 T lymphocytes in aging. Exp Gerontol 40(1–2):59–66
Caccamo N et al (2006) Sex-specific phenotypical and functional differences in peripheral human Vgamma9/Vdelta2 T cells. J Leukoc Biol 79(4):663–666
Michishita Y et al (2013) Age-associated alteration of gammadelta T-cell repertoire and different profiles of activation-induced death of Vdelta1 and Vdelta2 T cells. Int J Hematol 94(3):230–240
Roux A et al (2013) Differential impact of age and cytomegalovirus infection on the gammadelta T cell compartment. J Immunol 191(3):1300–1306
Colonna-Romano G et al (2002) Gamma/delta T lymphocytes are affected in the elderly. Exp Gerontol 37(2–3):205–211
Argentati K et al (2002) Numerical and functional alterations of circulating gammadelta T lymphocytes in aged people and centenarians. J Leukoc Biol 72(1):65–71
Hviid L et al (2000) High frequency of circulating gamma delta T cells with dominance of the v(delta)1 subset in a healthy population. Int Immunol 12(6):797–805
Goodier M et al (1993) Gamma delta T cells in the peripheral blood of individuals from an area of holoendemic Plasmodium falciparum transmission. Trans R Soc Trop Med Hyg 87(6):692–696
Cairo C et al (2008) Altered cord blood gammadelta T cell repertoire in Nigeria: possible impacts of environmental factors on neonatal immunity. Mol Immunol 45(11):3190–3197
Cairo C et al (2010) Impact of age, gender, and race on circulating gammadelta T cells. Hum Immunol 71(10):968–975
Worku S et al (1997) Higher proportion of CD8+ T cells in the blood in healthy adults from Ethiopia and Bangladesh compared with Sweden. Trans R Soc Trop Med Hyg 91(5):618–622
Polgar B et al (1999) The role of gamma/delta T cell receptor positive cells in pregnancy. Am J Reprod Immunol 41(4):239–244
Zheng NN et al (2011) Association between peripheral gammadelta T-cell profile and disease progression in individuals infected with HIV-1 or HIV-2 in West Africa. J Acquir Immune Defic Syndr 57(2):92–100
Poles MA et al (2003) Human immunodeficiency virus type 1 induces persistent changes in mucosal and blood gammadelta T cells despite suppressive therapy. J Virol 77(19):10456–10467
Rossol R et al (1998) Increase in Vdelta1+ gammadelta T cells in the peripheral blood and bone marrow as a selective feature of HIV-1 but not other virus infections. Br J Haematol 100(4):728–734
Dobmeyer TS et al (2002) Reciprocal alterations of Th1/Th2 function in gammadelta T-cell subsets of human immunodeficiency virus-1-infected patients. Br J Haematol 118(1):282–288
Fenoglio D et al (2009) Vdelta1 T lymphocytes producing IFN-gamma and IL-17 are expanded in HIV-1-infected patients and respond to Candida albicans. Blood 113(26):6611–6618
Nilssen DE, Brandtzaeg P (2012) Intraepithelial gammadelta T cells remain increased in the duodenum of AIDS patients despite antiretroviral treatment. PLoS One 7(1):e29066
Poccia F et al (2009) Zoledronic acid and interleukin-2 treatment improves immunocompetence in HIV-infected persons by activating Vgamma9Vdelta2 T cells. AIDS 23(5):555–565
Ueta C et al (1994) Increase of gamma/delta T cells in hospital workers who are in close contact with tuberculosis patients. Infect Immun 62(12):5434–5441
Meraviglia S et al (2010) Partial and ineffective activation of V gamma 9V delta 2 T cells by Mycobacterium tuberculosis-infected dendritic cells. J Immunol 185(3):1770–1776
Li B et al (1996) Disease-specific changes in gammadelta T cell repertoire and function in patients with pulmonary tuberculosis. J Immunol 157(9):4222–4229
Gioia C et al (2003) Different cytokine production and effector/memory dynamics of alpha beta+ or gamma delta+ T-cell subsets in the peripheral blood of patients with active pulmonaryA tuberculosis. Int J Immunopathol Pharmacol 16(3):247–252
Szereday L et al (2003) Gamma/delta T cell subsets in patients with active Mycobacterium tuberculosis infection and tuberculin anergy. Clin Exp Immunol 131(2):287–291
Peng MY et al (2008) Interleukin 17-producing gamma delta T cells increased in patients with active pulmonary tuberculosis. Cell Mol Immunol 5(3):203–208
Bourgarit A et al (2009) Tuberculosis-associated immune restoration syndrome in HIV-1-infected patients involves tuberculin-specific CD4 Th1 cells and KIR-negative gammadelta T cells. J Immunol 183(6):3915–3923
Worku S et al (1997) Lymphocyte activation and subset redistribution in the peripheral blood in acute malaria illness: distinct gammadelta+ T cell patterns in Plasmodium falciparum and P. vivax infections. Clin Exp Immunol 108(1):34–41
Hviid L et al (2001) Perturbation and proinflammatory type activation of V delta 1(+) gamma delta T cells in African children with Plasmodium falciparum malaria. Infect Immun 69(5):3190–3196
Schwartz E et al (1996) Delayed expansion of V delta 2+ and V delta 1+ gamma delta T cells after acute Plasmodium falciparum and Plasmodium vivax malaria. J Allergy Clin Immunol 97(6):1387–1392
Perera MK et al (1994) Transient increase in circulating gamma/delta T cells during Plasmodium vivax malarial paroxysms. J Exp Med 179(1):311–315
Darabi H et al (2002) Expansion of gammadelta T Cells in patients infected with cutaneous leishmaniasis with and without glucantime therapy. Braz J Infect Dis 6(5):258–262
Prigione I et al (2006) T cell mediated immune responses to Toxoplasma gondii in pregnant women with primary toxoplasmosis. Microbes Infect 8(2):552–560
Knight A et al (2010) The role of Vdelta2-negative gammadelta T cells during cytomegalovirus reactivation in recipients of allogeneic stem cell transplantation. Blood 116(12):2164–2172
Couzi L et al (2009) Common features of gammadelta T cells and CD8(+) alphabeta T cells responding to human cytomegalovirus infection in kidney transplant recipients. J Infect Dis 200(9):1415–1424
Dechanet J et al (1999) Implication of gammadelta T cells in the human immune response to cytomegalovirus. J Clin Invest 103(10):1437–1449
Dechanet J et al (1999) Major expansion of gammadelta T lymphocytes following cytomegalovirus infection in kidney allograft recipients. J Infect Dis 179(1):1–8
Lafarge X et al (2001) Cytomegalovirus infection in transplant recipients resolves when circulating gammadelta T lymphocytes expand, suggesting a protective antiviral role. J Infect Dis 184(5):533–541
Vermijlen D et al (2010) Human cytomegalovirus elicits fetal gammadelta T cell responses in utero. J Exp Med 207(4):807–821
Pitard V et al (2008) Long-term expansion of effector/memory Vdelta2-gammadelta T cells is a specific blood signature of CMV infection. Blood 112(4):1317–1324
Macsween KF et al (2010) Infectious mononucleosis in university students in the United kingdom: evaluation of the clinical features and consequences of the disease. Clin Infect Dis 50(5):699–706
Hudnall SD et al (2003) Comparative immunophenotypic features of EBV-positive and EBV-negative atypical lymphocytosis. Cytometry B Clin Cytom 55(1):22–28
Barcy S et al (2008) Gamma delta+ T cells involvement in viral immune control of chronic human herpesvirus 8 infection. J Immunol 180(5):3417–3425
Aoyagi M et al (2003) Respiratory syncytial virus infection suppresses IFN-gamma production of gammadelta T cells. Clin Exp Immunol 131(2):312–317
Green S et al (1999) Early CD69 expression on peripheral blood lymphocytes from children with dengue hemorrhagic fever. J Infect Dis 180(5):1429–1435
Hara T et al (1992) Predominant activation and expansion of V gamma 9-bearing gamma delta T cells in vivo as well as in vitro in Salmonella infection. J Clin Invest 90(1):204–210
Hoshina T et al (2012) NKRP1A+ gammadelta and alphabeta T cells are preferentially induced in patients with Salmonella infection. Hum Immunol 73(6):623–628
Islam D, Christensson B (2000) Disease-dependent changes in T-cell populations in patients with shigellosis. APMIS 108(4):251–260
Schneider T et al (1997) The number and proportion of Vgamma9 Vdelta2 T cells rise significantly in the peripheral blood of patients after the onset of acute Coxiella burnetii infection. Clin Infect Dis 24(2):261–264
Klimpel GR et al (2003) Leptospira interrogans activation of human peripheral blood mononuclear cells: preferential expansion of TCR gamma delta+ T cells vs TCR alpha beta+ T cells. J Immunol 171(3):1447–1455
Jouen-Beades F et al (1997) In vivo and in vitro activation and expansion of gammadelta T cells during Listeria monocytogenes infection in humans. Infect Immun 65(10):4267–4272
Poquet Y et al (1998) Expansion of Vgamma9 Vdelta2 T cells is triggered by Francisella tularensis-derived phosphoantigens in tularemia but not after tularemia vaccination. Infect Immun 66(5):2107–2114
Kroca M et al (2000) The proportion of circulating gammadelta T cells increases after the first week of onset of tularaemia and remains elevated for more than a year. Clin Exp Immunol 120(2):280–284
Kroca M et al (2001) V gamma 9V delta 2 T cells in human legionellosis. Clin Diagn Lab Immunol 8(5):949–954
Caldwell CW et al (1995) Lymphocytosis of gamma/delta T cells in human ehrlichiosis. Am J Clin Pathol 103(6):761–766
Bertotto A et al (1997) Gamma delta T cells are decreased in the blood of children with Bordetella pertussis infection. Acta Paediatr 86(1):114–115
Watanabe H et al (2000) Psittacosis with increased gammadelta T cells in bronchoalveolar lavage fluid. Respirology 5(2):161–164
Caccamo N et al (2011) Differentiation, phenotype, and function of interleukin-17-producing human Vgamma9Vdelta2 T cells. Blood 118(1):129–138
Bertotto A et al (1993) Lymphocytes bearing the gamma delta T cell receptor in acute Brucella melitensis infection. Eur J Immunol 23(5):1177–1180
Kilic SS et al (2009) Gamma/delta T cells in patients with acute brucellosis. Clin Exp Med 9(2):101–104
Noguchi A et al (2011) Zoledronate-activated Vgamma9gammadelta T cell-based immunotherapy is feasible and restores the impairment of gammadelta T cells in patients with solid tumors. Cytotherapy 13(1):92–97
Bryant NL et al (2009) Characterization and immunotherapeutic potential of gammadelta T-cells in patients with glioblastoma. Neuro Oncol 11(4):357–367
Bilgi O et al (2008) Peripheral blood gamma-delta T cells in advanced-stage cancer patients. Adv Ther 25(3):218–224
Puan KJ et al (2009) Phenotypic and functional alterations of Vgamma2Vdelta2 T cell subsets in patients with active nasopharyngeal carcinoma. Cancer Immunol Immunother 58(7):1095–1107
Bas M et al (2006) Gamma-delta T-cells in patients with squamous cell carcinoma of the head and neck. Oral Oncol 42(7):691–697
Kuroda H et al (2012) Decreased number and reduced NKG2D expression of Vdelta1 gammadelta T cells are involved in the impaired function of Vdelta1 gammadelta T cells in the tissue of gastric cancer. Gastric Cancer 15(4):433–439
Lee AJ et al (2012) Gammadelta T cells are increased in the peripheral blood of patients with gastric cancer. Clin Chim Acta 413(19–20):1495–1499
Campillo JA et al (2007) Increased number of cytotoxic CD3+ CD28- gammadelta T cells in peripheral blood of patients with cutaneous malignant melanoma. Dermatology 214(4):283–288
Provinciali M et al (2010) Persistent ex vivo low number and functional in vitro recovery of circulating gammadelta T cells after removal of a cutaneous primary melanoma. Scand J Immunol 72(2):142–149
Kobayashi H et al (2011) A new indicator of favorable prognosis in locally advanced renal cell carcinomas: gamma delta T-cells in peripheral blood. Anticancer Res 31(3):1027–1031
Bennouna J et al (2010) Phase I study of bromohydrin pyrophosphate (BrHPP, IPH 1101), a Vgamma9Vdelta2 T lymphocyte agonist in patients with solid tumors. Cancer Immunol Immunother 59(10):1521–1530
Lang JM et al (2011) Pilot trial of interleukin-2 and zoledronic acid to augment gammadelta T cells as treatment for patients with refractory renal cell carcinoma. Cancer Immunol Immunother 60(10):1447–1460
Meraviglia S et al (2010) In vivo manipulation of Vgamma9Vdelta2 T cells with zoledronate and low-dose interleukin-2 for immunotherapy of advanced breast cancer patients. Clin Exp Immunol 161(2):290–297
Santini D et al (2009) In vivo effects of zoledronic acid on peripheral gammadelta T lymphocytes in early breast cancer patients. Cancer Immunol Immunother 58(1):31–38
Dieli F et al (2007) Targeting human gamma}delta T cells with zoledronate and interleukin-2 for immunotherapy of hormone-refractory prostate cancer. Cancer Res 67(15):7450–7457
Kobayashi H et al (2007) Safety profile and anti-tumor effects of adoptive immunotherapy using gamma-delta T cells against advanced renal cell carcinoma: a pilot study. Cancer Immunol Immunother 56(4):469–476
Bennouna J et al (2008) Phase-I study of Innacell gammadelta, an autologous cell-therapy product highly enriched in gamma9delta2 T lymphocytes, in combination with IL-2, in patients with metastatic renal cell carcinoma. Cancer Immunol Immunother 57(11):1599–1609
Sakamoto M et al (2011) Adoptive immunotherapy for advanced non-small cell lung cancer using zoledronate-expanded gammadeltaTcells: a phase I clinical study. J Immunother 34(2):202–211
Couzi L et al (2010) Cytomegalovirus-induced gammadelta T cells associate with reduced cancer risk after kidney transplantation. J Am Soc Nephrol 21(1):181–188
Futagbi G et al (2007) Selective activation of TCR-gammadelta+ cells in endemic Burkitt’s lymphoma. Malar J 6:69
Braza MS et al (2010) Gammadelta T lymphocytes count is normal and expandable in peripheral blood of patients with follicular lymphoma, whereas it is decreased in tumor lymph nodes compared with inflammatory lymph nodes. J Immunol 184(1):134–140
Gertner-Dardenne J et al (2012) Human Vgamma9Vdelta2 T cells specifically recognize and kill acute myeloid leukemic blasts. J Immunol 188(9):4701–4708
Lamb LS Jr et al (1999) Influence of T cell depletion method on circulating gammadelta T cell reconstitution and potential role in the graft-versus-leukemia effect. Cytotherapy 1(1):7–19
Godder KT et al (2007) Long term disease-free survival in acute leukemia patients recovering with increased gammadelta T cells after partially mismatched related donor bone marrow transplantation. Bone Marrow Transplant 39(12):751–757
Bank I et al (2003) Expansion of gammadelta T-cells in Behcet’s disease: role of disease activity and microbial flora in oral ulcers. J Lab Clin Med 141(1):33–40
Freysdottir J et al (1999) Gammadelta T cells in Behcet’s disease (BD) and recurrent aphthous stomatitis (RAS). Clin Exp Immunol 118(3):451–457
Clemente A et al (2010) Phenotype markers and cytokine intracellular production by CD8+ gammadelta T lymphocytes do not support a regulatory T profile in Behcet’s disease patients and healthy controls. Immunol Lett 129(2):57–63
Yamashita N et al (1997) Role of gammadelta T lymphocytes in the development of Behcet’s disease. Clin Exp Immunol 107(2):241–247
Yasuoka H et al (2008) Preferential activation of circulating CD8+ and gammadelta T cells in patients with active Behcet’s disease and HLA-B51. Clin Exp Rheumatol 26(4 Suppl 50):S59–S63
Direskeneli H et al (2008) Thalidomide has both anti-inflammatory and regulatory effects in Behcet’s disease. Clin Rheumatol 27(3):373–375
Ahn JK et al (2005) Down-regulation of IFN-gamma-producing CD56+ T cells after combined low-dose cyclosporine/prednisone treatment in patients with Behcet’s uveitis. Invest Ophthalmol Vis Sci 46(7):2458–2464
Freysdottir J et al (2006) Diversity of gammadelta T cells in patients with Behcet’s disease is indicative of polyclonal activation. Oral Dis 12(3):271–277
Brennan F et al (1989) Coordinate expansion of ‘fetal type’ lymphocytes (TCR gamma delta+ T and CD5+ B) in rheumatoid arthritis and primary Sjogren’s syndrome. Clin Exp Immunol 77(2):175–178
Kowal-Bielecka O et al (2001) Gamma delta-Lymphocytes in the peripheral blood of patients with rheumatoid arthritis–correlation with clinical and laboratory parameters of the disease and with the treatment used. Rocz Akad Med Bialymst 46:170–181
Smith MD et al (1990) T gamma delta cells and their subsets in blood and synovial tissue from rheumatoid arthritis patients. Scand J Immunol 32(6):585–593
Lunardi C et al (1992) T gamma delta cells and their subsets in blood and synovial fluid from patients with rheumatoid arthritis. Br J Rheumatol 31(8):527–530
Spadaro A et al (2004) Natural killer cells and gamma/delta T cells in synovial fluid and in peripheral blood of patients with psoriatic arthritis. Clin Exp Rheumatol 22(4):389–394
Liu MF et al (1999) Distribution of double-negative (CD4− CD8−, DN) T subsets in blood and synovial fluid from patients with rheumatoid arthritis. Clin Rheumatol 18(3):227–231
Mitogawa T et al (1992) Frequency of gamma delta T cells in peripheral blood, synovial fluid, synovial membrane and lungs from patients with rheumatoid arthritis. Acta Med Okayama 46(5):371–379
Hoshino T et al (1996) TCR gamma delta+ T cells in peripheral blood of patients with adult Still’s disease. J Rheumatol 23(1):124–129
Macaubas C et al (2010) Distribution of circulating cells in systemic juvenile idiopathic arthritis across disease activity states. Clin Immunol 134(2):206–216
Kenna TJ et al (2012) Enrichment of circulating interleukin-17-secreting interleukin-23 receptor-positive gamma/delta T cells in patients with active ankylosing spondylitis. Arthritis Rheum 64(5):1420–1429
Robak E et al (1999) Circulating TCR gammadelta cells in the patients with systemic lupus erythematosus. Mediators Inflamm 8(6):305–312
Robak E et al (2001) Lymphocyctes Tgammadelta in clinically normal skin and peripheral blood of patients with systemic lupus erythematosus and their correlation with disease activity. Mediators Inflamm 10(4):179–189
Wang L et al (2012) Downregulation of CD94/NKG2A inhibitory receptor on decreased gammadelta T cells in patients with systemic lupus erythematosus. Scand J Immunol 76(1):62–69
Li X et al (2011) Generation of human regulatory gammadelta T cells by TCRgammadelta stimulation in the presence of TGF-beta and their involvement in the pathogenesis of systemic lupus erythematosus. J Immunol 186(12):6693–6700
Chauhan SK et al (2006) T-cell receptor repertoire of circulating gamma delta T-cells in Takayasu’s arteritis. Clin Immunol 118(2–3):243–249
Seko Y (2000) Takayasu arteritis: insights into immunopathology. Jpn Heart J 41(1):15–26
Bendersky A et al (2010) Vgamma9+ gammadelta T cells in systemic sclerosis patients are numerically and functionally preserved and induce fibroblast apoptosis. Immunobiology 215(5):380–394
Ueda-Hayakawa I, et al. Circulating gamma/delta T cells in systemic sclerosis exhibit activated phenotype and enhance gene expression of proalpha2(I) collagen of fibroblasts. J Dermatol Sci 69(1):54–60
Riccieri V et al (2005) Reduced circulating natural killer T cells and gamma/delta T cells in patients with systemic sclerosis. J Rheumatol 32(2):283–286
Rinaldi L et al (2006) Longitudinal analysis of immune cell phenotypes in early stage multiple sclerosis: distinctive patterns characterize MRI-active patients. Brain 129(Pt 8):1993–2007
Chen Z, Freedman MS (2008) Correlation of specialized CD16(+) gammadelta T cells with disease course and severity in multiple sclerosis. J Neuroimmunol 194(1–2):147–152
Schirmer L et al (2013) Enriched CD161high CCR6+ gammadelta T cells in the cerebrospinal fluid of patients with multiple sclerosis. JAMA Neurol 70(3):345–351
Pranzatelli MR et al (2004) Immunophenotype of blood lymphocytes in neuroblastoma-associated opsoclonus-myoclonus. J Pediatr Hematol Oncol 26(11):718–723
Pranzatelli MR et al (2004) B- and T-cell markers in opsoclonus-myoclonus syndrome: immunophenotyping of CSF lymphocytes. Neurology 62(9):1526–1532
Scelsa SN et al (2004) Blood gammadelta T cells, Campylobacter jejuni, and GM1 titers in Guillain–Barre syndrome. Muscle Nerve 30(4):423–432
Kretowski A et al (2000) Abnormal distribution of gammadelta T lymphocytes in Graves’ disease and insulin-dependent diabetes type 1. Arch Immunol Ther Exp (Warsz) 48(1):39–42
Toyabe S et al (2001) Oligoclonally expanding gammadelta T lymphocytes induce IgA switching in IgA nephropathy. Clin Exp Immunol 124(1):110–117
Chen KS et al (1996) Diminution of T cells with gamma delta receptor in the peripheral blood of allergic asthmatic individuals. Clin Exp Allergy 26(3):295–302
Zhao Y et al (2011) Altered expressions of helper T cell (Th)1, Th2, and Th17 cytokines in CD8(+) and gammadelta T cells in patients with allergic asthma. J Asthma 48(5):429–436
Krejsek J et al (1998) Decreased peripheral blood gamma delta T cells in patients with bronchial asthma. Allergy 53(1):73–77
Pons J et al (2005) Blunted gamma delta T-lymphocyte response in chronic obstructive pulmonary disease. Eur Respir J 25(3):441–446
Mota-Pinto A et al (2011) Regulatory T cells in elderly patients with asthma. J Investig Allergol Clin Immunol 21(3):199–206
Schauer U et al (1991) T cell receptor gamma delta bearing cells are decreased in the peripheral blood of patients with atopic diseases. Clin Exp Immunol 86(3):440–443
Hamzaoui A et al (2002) T cells expressing the gammadelta receptor are essential for Th2-mediated inflammation in patients with acute exacerbation of asthma. Mediators Inflamm 11(2):113–119
Krug N et al (2001) Cytokine profile of bronchoalveolar lavage-derived CD4(+), CD8(+), and gammadelta T cells in people with asthma after segmental allergen challenge. Am J Respir Cell Mol Biol 25(1):125–131
Spinozzi F et al (1996) Increased allergen-specific, steroid-sensitive gamma delta T cells in bronchoalveolar lavage fluid from patients with asthma. Ann Intern Med 124(2):223–227
Chen M et al (2012) Enhanced peripheral gammadeltaT cells cytotoxicity potential in patients with HBV-associated acute-on-chronic liver failure might contribute to the disease progression. J Clin Immunol 32(4):877–885
Chen M et al (2008) Characteristics of circulating T cell receptor gamma-delta T cells from individuals chronically infected with hepatitis B virus (HBV): an association between V(delta)2 subtype and chronic HBV infection. J Infect Dis 198(11):1643–1650
Ferri S et al (2010) A multifaceted imbalance of T cells with regulatory function characterizes type 1 autoimmune hepatitis. Hepatology 52(3):999–1007
Kiyici M et al (2006) Lymphocyte subsets and cytokines in ascitic fluid of decompensated cirrhotic patients with and without spontaneous ascites infection. J Gastroenterol Hepatol 21(6):963–969
Fernandez-Ruiz M et al (2009) Pretransplant lymphocyte count predicts the incidence of infection during the first two years after liver transplantation. Liver Transpl 15(10):1209–1216
Puig-Pey I et al (2010) Characterization of gammadelta T cell subsets in organ transplantation. Transpl Int 23(10):1045–1055
Andreu-Ballester JC et al (2011) Deficit of gammadelta T lymphocytes in the peripheral blood of patients with Crohn’s disease. Dig Dis Sci 56(9):2613–2622
Andreu-Ballester JC et al (2013) Microsporidia and its relation to Crohn’s disease. A retrospective study. PLoS One 8(4):e62107
Soderstrom K et al (1996) Increased frequency of abnormal gamma delta T cells in blood of patients with inflammatory bowel diseases. J Immunol 156(6):2331–2339
Kelsen J et al (2011) Infliximab induces clonal expansion of gammadelta-T cells in Crohn’s disease: a predictor of lymphoma risk? PLoS One 6(3):e17890
Kerttula TO et al (1998) Circulating T lymphocyte subsets in coeliac disease (CoD) patients and healthy family members. Clin Exp Immunol 111(3):536–540
Camarero C et al (2000) Intraepithelial lymphocytes and coeliac disease: permanent changes in CD3−/CD7+ and T cell receptor gammadelta subsets studied by flow cytometry. Acta Paediatr 89(3):285–290
Calleja S et al (2011) Dynamics of non-conventional intraepithelial lymphocytes-NK, NKT, and gammadelta T-in celiac disease: relationship with age, diet, and histopathology. Dig Dis Sci 56(7):2042–2049
Jarvinen TT et al (2003) Intraepithelial lymphocytes in celiac disease. Am J Gastroenterol 98(6):1332–1337
Iltanen S et al (1999) Increased density of jejunal gammadelta+ T cells in patients having normal mucosa–marker of operative autoimmune mechanisms? Autoimmunity 29(3):179–187
Torrente F et al (2004) Focal-enhanced gastritis in regressive autism with features distinct from Crohn’s and Helicobacter pylori gastritis. Am J Gastroenterol 99(4):598–605
Laggner U et al (2011) Identification of a novel proinflammatory human skin-homing Vgamma9Vdelta2 T cell subset with a potential role in psoriasis. J Immunol 187(5):2783–2793
Seung NR et al (2007) Comparison of expression of heat-shock protein 60, Toll-like receptors 2 and 4, and T-cell receptor gammadelta in plaque and guttate psoriasis. J Cutan Pathol 34(12):903–911
Cai Y et al (2011) Pivotal role of dermal IL-17-producing gammadelta T cells in skin inflammation. Immunity 35(4):596–610
Cairo C et al (2005) Analysis of circulating gammadelta T cells in children affected by IgE-associated and non-IgE-associated allergic atopic eczema/dermatitis syndrome. Clin Exp Immunol 141(1):116–121
Katsuta M et al (2006) NK cells and gamma delta+ T cells are phenotypically and functionally defective due to preferential apoptosis in patients with atopic dermatitis. J Immunol 176(12):7736–7744
Moins-Teisserenc HT et al (1999) Association of a syndrome resembling Wegener’s granulomatosis with low surface expression of HLA class-I molecules. Lancet 354(9190):1598–1603
Oswald E et al (2009) Reduced numbers of circulating gammadelta T cells in patients with bullous pemphigoid. Exp Dermatol 18(11):991–993
Suzuki S et al (1997) Circadian rhythm of leucocytes and lymphocytes subsets and its possible correlation with the function of the autonomic nervous system. Clin Exp Immunol 110(3):500–508
Anane LH et al (2010) Phenotypic characterization of gammadelta T cells mobilized in response to acute psychological stress. Brain Behav Immun 24(4):608–614
Atanackovic D et al (2013) Acute psychological stress increases peripheral blood CD3(+)CD56(+) natural killer T cells in healthy men: possible implications for the development and treatment of allergic and autoimmune disorders. Stress 16(4):421–428
Matsushima A et al (2004) Early activation of gammadelta T lymphocytes in patients with severe systemic inflammatory response syndrome. Shock 22(1):11–15
Theodorou GL et al (2007) Effect of non-operative management (NOM) of splenic rupture versus splenectomy on the distribution of peripheral blood lymphocyte populations and cytokine production by T cells. Clin Exp Immunol 150(3):429–436
Venet F et al (2005) Both percentage of gammadelta T lymphocytes and CD3 expression are reduced during septic shock. Crit Care Med 33(12):2836–2840
Andreu-Ballester JC et al (2013) Association of gammadelta T cells with disease severity and mortality in septic patients. Clin Vaccine Immunol 20(5):738–746
Niehues T et al (2010) More than just SCID—the phenotypic range of combined immunodeficiencies associated with mutations in the recombinase activating genes (RAG) 1 and 2. Clin Immunol 135(2):183–192
Malan Borel I et al (2003) Gammadelta T cells and interleukin-6 levels could provide information regarding the progression of human renal allograft. Scand J Immunol 58(1):99–105
Yamaguchi T et al (2000) Changes in T-cell receptor subsets after cardiac surgery in children. Surg Today 30(10):875–878
Habermehl P et al (2003) Changes in lymphocyte subsets after cardiac surgery in children. Eur J Pediatr 162(1):15–21
Thompson K et al (2011) Fluvastatin does not prevent the acute-phase response to intravenous zoledronic acid in post-menopausal women. Bone 49(1):140–145
Kalyan S et al (2013) Can peripheral blood gammadelta T cells predict osteonecrosis of the jaw? An immunological perspective on the adverse drug-effects of aminobisphosphonate therapy. J Bone Miner Res 28(4):728–735
Matsumoto Y et al (1998) Peripheral deletion of gammadelta T cells in haemodialysis patients. Nephrol Dial Transplant 13(11):2861–2866
Roden AC et al (2008) Immunophenotypic attributes of benign peripheral blood gammadelta T cells and conditions associated with their increase. Arch Pathol Lab Med 132(11):1774–1780
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bank, I., Marcu-Malina, V. Quantitative Peripheral Blood Perturbations of γδ T Cells in Human Disease and Their Clinical Implications. Clinic Rev Allerg Immunol 47, 311–333 (2014). https://doi.org/10.1007/s12016-013-8391-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-013-8391-x