Abstract
Reduced bone mineral density is frequently found especially in adult celiac disease (CD) and dietary guidelines favor vitamin D supplementation in adults and children with CD. Vitamin D serum levels were investigated in CD populations in order to challenge its routine supplementation. Israeli (61), Spanish (59), CD children (groups 1 and 5, respectively) were compared to children with nonspecific abdominal pain (56), their parents (84) and Spanish adult CD patients (22) (group 2, 3, 4, respectively). 25(OH)-vitamin D was checked by LIAISON chemiluminescent immunoassays. Groups 5 and 1 had the highest levels compared to groups 4 and 3 with the lowest levels. The levels in groups 1 and 2 were comparable. Concerning 25(OH)-vitamin D sera levels, only the difference between group 5 and 4 was statistically significant (30.3 ± 12.3 and 20.2 ± 10.5 ng/ml, respectively p = 0.003). When vitamin D was splitted above and below 20 ng/ml level, 54.5% of Spanish adult CD had vitamin D deficiency compared to 16.9% of the local CD children (p = 0.001). 29.6% of group 2 had deficient levels compared to their parents with 50% (p = 0.019). In conclusion, Vitamin D sera levels negatively correlate with age. Thus, mainly adult CD population should be assessed for vitamin D levels and supplemented accordingly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Celiac disease (CD) is a life-long autoimmune condition [1] mainly of the gastrointestinal tract, affecting the small intestine of genetically susceptible individuals. Gluten, which is the storage protein of wheat and its alcohol soluble gliadins are the offending inducers of the disease together with structurally related molecules found in barley and rye. Nevertheless, additional environmental factors like infections might play a role in CD induction [2]. Tissue transglutaminase (tTG) is the autoantigen against which the abnormal immune response is directed to [3] and two main auto antibodies, anti-endomysium and anti-tTG, are the most useful serological markers to screen for the disease [4]. Recently, two additional autoantibodies, namely anti-deaminated gliadin peptide and anti-neoepitope tTG, were found to be reliable for CD screening [5]. HLA-DQ2 and HLA-DQ8 molecules are the most important, so far known, predisposing genetic factors. A lot is known on the pathogenesis of the disease. The sequential chain of events operating in the disease was recently unraveled and gives the hope for future therapeutic strategies [6]. Furthermore, its epidemiology, prevalence, and clinical presentation are changing constantly, and with time, new clinical presentations are depicted and widen the plethora of clinical variability of CD [7].
It has been shown that the classical intestinal clinical picture is disappearing, and the extra-intestinal presentation is emerging. Skin, endocrine, hepatic, skeletal, hematological, gynecological, infertility, dental, and behavioral abnormalities are often described [8–10]. With the growing awareness of family practitioners, hematologists and gastroenterologists, and now gynecologists and neurologists, the diagnosis of CD is increasingly being made during the whole life-span. In fact, about 20% of newly diagnosed cases occur in patients who are older than 60 years of age.One of the growing domains is the extra-intestinal presentations of CD affecting the bone, presenting as osteopenia or osteoporosis, fractures, and falls [11–18].
It is becoming increasingly clear that vitamin D has a wide range of biological activity in addition to the classic endocrine pathway affecting bone state, thus making this hormone important to many aspects of general health. Ecological and epidemiological studies suggest that vitamin D insufficiency plays a role in the development of colorectal, breast, prostatic, ovarian cancers and lymphoma, autoimmune diseases like multiple sclerosis, type 1 diabetes, systemic lupus erythematosus, rheumatic arthritis, hypertension, infectious diseases, diabetes, cardiovascular disease, musculoskeletal disorders, asthma, as well as several psychiatric conditions such as schizophrenia, depression, and dementia [19–21].
Vitamin D is closely linked to autoimmunity. Many autoimmune conditions are more frequent in geographical areas far from the equator and/or less sunny ones. Low serum vitamin D levels are found in patients with autoimmune diseases, and higher levels are inversely correlated with the incidence of some of them. Anti-vitamin D antibodies were found in a subset of patients with autoimmune diseases. Many animal models of autoimmune diseases identified vitamin D as an immunomodulator of the autoimmune process. Vitamin D suppresses several autoimmune pathways including the Th1, B cells, Th-17, dendritic cell, and co-stimulatory molecule systems. Furthermore, polymorphic classical genes, important in vitamin D functions like VDR and CP27B, are associated with susceptibility to several autoimmune diseases. Those epidemiological, immunological, and genetic data are summarized in Table 1 [22–64]. More so, beneficial effects of vitamin D supplementation or vitamin D agonists' therapy further strengthen this causal relation (Table 1). In a recent study on different clinical subgroups of multiple sclerosis patients, 1,25(OH)(2)D(3)was found to play an important role in T cell homeostasis during the course of the disease, suggesting that correction of vitamin D deficiency may be a useful therapeutical strategy, affecting the clinical course of multiple sclerosis [63].
Unfortunately, it is estimated that as many as one billion people worldwide suffer from vitamin D deficiency or insufficiency (commonly defined as levels below 20 and 20–30 ng/ml, respectively), and this was shown to be prevalent across all age groups, genders, and geographic regions [65–74].
The intestine plays a critical role in bone homeostasis in the normal population as well as in various gastrointestinal disorders [75–77]. An increased prevalence of CD in the osteoporotic population was reported, and serological screening was recommended [78]. Others casted doubt on the association and opposed routine CD screening [79]. On the other hand, numerous studies depicted reduced bone mineral density in untreated CD possibly due to calcium and vitamin D malabsorption, release of proinflammatory cytokines, and misbalanced bone remodeling [13, 80–82]. Only few assessed serum vitamin D metabolites and none compared them along the life span in an interfamilial design and compared two sunny countries with a different genetic background.
The present study was undertaken to fill this gap. The main aims were to investigate vitamin D status in children and adults, in two Mediterranean sunny countries like Spain and Israel, in an inter- and intra-family structures in celiac populations. The secondary aims were to challenge the call to investigate all the celiacs for osteopathy, vitamin D levels determination, and their routine vitamin D supplementation, and additionally, to try to understand the differential role played by the genetic background compared to age in the pathogenesis of celiac bone pathology.
Material and Methods
Study Populations
Serum vitamin D levels were determined in 272 individuals, divided to five groups. Group 1 comprised of 51 Israeli children with definitive CD (age, 6 ± 4 years, M/F ratio 29:32) and group 5 included 59 Spanish CD affected children (age, 4 ± 4 years, M/F ratio 37:22). Group 2 comprised of 56 Israeli children diagnosed with nonspecific abdominal pain (age, 8 ± 5 years, M/F ratio 27:29). The pediatric populations were compared to two adults ones: group 3 include 84 adults, parents of group 2 (age, 39 ± 8 years, M/F ratio 49:35), and groups 4–22 Spanish adults with CD (age, 44 ± 13 years, M/F ratio 16:6).
The following information was collected on the Israeli population: Diet: gluten-containing or free diet. Symptoms: abdominal pain, short stature, vomiting, diarrhea, anemia, failure to thrive, and IgA deficiency. Familial diseases: CD, Diabetes mellitus type1/2, FMF, IBD, thyroid disease. Ethnicity: Ashkenazi (European and North American origin)/Sephardic (African and Asian origin)/mixed (Ashkenazi and Sephardic) Jews, Christians, Moslems and Druze, Laboratory parameters: complete blood count, biochemical profile, IgA levels, CD serology: antiendomysial, anti-tissue transglutaminase antibodies. Degree of small intestinal injury: 0 = normal, 1 = slight inflammation, 2 = moderate inflammation and moderate villous atrophy, 3 = mild inflammation and sub-total villous atrophy, 4 = heavy inflammation and total villous atrophy. Presence of Helicobacter pylori in the antral biopsy.
Celiac disease was diagnosed according to the revised criteria of the European Society for Pediatric Gastroenterology and Nutrition based on specific serology (anti-endomysial and/or anti-tissue transglutaminase antibodies by immunofluorescence and ELIZA, respectively) and duodenal biopsies [83]. All the participants were on a gluten-containing diet and had physical examination, laboratory workup, and celiac serology. Endoscopy with at least four duodenal and one antral biopsies was performed in all the groups, except group 3. On the day of endoscopy, 5 ml of peripheral blood was withdrawn, centrifuge 5,000 c/s for 10 min, and the serum was frozen in −80°C until assayed for vitamin D metabolites. None of the participants received vitamin D supplementation.
The study was approved by the local Helsinki Committee in Spain and Israel and informed consent was obtained from all subject or caregivers.
Vitamin D Measurement
A commercial kit, LIAISON® 25(OH)D Assay (DiaSorin, Italy) was used in order to measure serum concentration of 25(OH)D in sera of subjects. The method for quantitative determination of 25(OH) D is a direct, competitive chemiluminescence immunoassay. Specific antibody to vitamin D is used for coating magnetic particles (solid phase), and vitamin D is linked to an isoluminol derivative. During the incubation, 25(OH) D is dissociated from its binding protein and competes with labeled vitamin D for binding sites on the antibody. After the incubation, the unbound material is removed with a wash cycle. Subsequently, the starter reagents are added and a flash chemiluminescent reaction is initiated. The light signal is measured by a photomultiplier as relative light units and is inversely proportional to the concentration of 25(OH) D present in calibrators, controls, or samples.
As different investigators have defined the normal lower limit in the serum as 25(OH)D levels below 12 ng/ml (30 nmol/l) or below 20 ng/ml (50 nmol/l) [84, 85], in the present study, we defined vitamin D deficiency as levels of 25(OH)D below 20 ng/ml, according to the new definition [85]. Vitamin D insufficiency was considered to be at levels between 20 and 30 ng/ml (50–75 nmol/l).
Statistical Analysis
Data analysis was performed using the SPSS statistical package version15.
Comparison of prevalence rates (i.e., vitamin D deficiency and insufficiency percentages) between groups was preformed by chi-square test or Fisher exact test as was appropriate. Continuous variables are expressed as mean ± standard deviation throughout the manuscript.
ANOVA was performed for comparison of vitamin D levels between groups. The Bonferroni correction was applied in case of multiple comparisons. Pearson correlation coefficients were calculated. All p values are two-sided, with a significance level of p < 0.05.
Results
The Israeli and Spanish CD children (groups 1 and 5, respectively) had the highest levels of serum vitamin D metabolites (30.3 ± 12.3 and 25.6 ± 9.7 ng/ml, respectively), compared to the two adult groups (groups 3 and 4) who had the lowest ones (20.7 ± 10.7 and 20.2 ± 10.5 ng/ml, respectively). Vitamin D levels in the two pediatric Israeli groups (groups 1 and 2, 25.6 ± 9.7 and 24.9 ± 11.4 ng/ml, respectively) were comparable. Concerning 25(OH) D sera levels in the five groups, only the difference between groups 5 and 4 was significant (30.3 ± 12.3 and 20.2 ± 10.5 ng/ml, respectively p < 0.003) (Table 2).
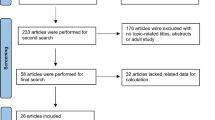
When vitamin D was splited above and below (deficiency) 20 ng/ml level, 54.5% of Spanish adult CD had vitamin D deficiency, compared to 16.9% of the local CD children (p < 0.001). In group 2, 29.6% had deficient levels compared to their parents with 50% (p < 0.019). Comparing the two CD pediatric population, groups 1 and 5, vitamin D deficiency was more prevalent in the Israeli CD children (33.3% compared to 16.9%, respectively (p < 0.046; Fig. 1).
Percentage of individuals with vitamin D deficiency (<20 ng/ml) in five groups: (1) CD children from Israel. (2) Recurrent abdominal pain (RAP), Israeli children. (3) Parents of RAP children. (4) CD Spanish adults. (5) CD Spanish children. *p < 0.046 comparing CD group 1 to 5. **p < 0.019 comparing intra-familial groups 2 to 3. ***p < 0.001 comparing Spanish groups 4 to 5
Concerning origin and ethnicity in the Israeli populations, a significant correlation was found between serum vitamin D levels in Ashkenazi + mixed compared to Sephardic Jews (27.8 ± 10.3, 22.7 ± 10.0 ng/ml, respectively, p = 0.02), Ashkenazi + mixed to Moslem + Druze subjects (27.8 ± 10.3, 16.5 ± 9.4 ng/ml, respectively, p = 0.0001), Sephardic Jews to Moslem + Druze (22.7 ± 10.0,16.5 ± 9.4 ng/ml, respectively, p < 0.012), Christian to Moslem + Druze groups (31.6 ± 10.9,16.5 ± 9.4, respectively, p = 0.01). Grading mean serum vitamin D levels, from the highest to the lowest levels: Christian, Ashkenazi and mixed Jews, Sephardic Jews, Moslem and Druze (31.6, 27.8, 22.7, 16.5 ng/ml, respectively, p = 0.0001). It can be concluded that there is a west to east gradient in vitamin D status.
No correlation was depicted between serum vitamin D metabolites levels and gender, celiac serology magnitude, degree of intestinal injury, and anemia. However, the following parameters correlated to vitamin D levels: age-negative correlation (−0.332, p < 0.0001), IgA levels-negative correlation (−453, p < 0.006), FTT-positive correlation (vitamin D levels in FTT/no FTT, 29.3/22.1 ng/ml, respectively, p < 0.001). There are more percentage of vitamin D deficiency among the non-FTT children, compared to the FTT ones (43.5%, 19.4% respectively, p < 0.01), H. pylori presence-negative correlation (vitamin D levels in Hp+/Hp−, 21.2/26.5 ng/ml, respectively, <0.03). There are more percentage of vitamin D deficiency among the antral Hp+ patients compared to the Hp− ones (50%, 25%, respectively, p < 0.02).
Discussion
Regardless of the definition of vitamin D insufficiency or deficiency, it is clear that suboptimal levels are a worldwide phenomenon with hardly any region spared. Moreover, the Middle East and populations, despite the abundant sun and favorable attitude of the regions, is the most deficient ones [73, 74]. Recent studies emphasize the high frequency of vitamin D insufficiency, even in sunny countries like Florida, Turkey, Lebanon, Tunisia, Jordan, and Saudi Arabia [73]. In the present study, 95 out of 272 (34.9%) subjects are vitamin D deficient with a serum level <20 ng/ml, and 182 (66.9%) are insufficient, having serum levels <30 ng/ml, thus complying with the world pandemic of hypovitaminosis D.
The present study design allows us to study the effect of age, intestinal inflammation, and familial factors on vitamin D status. Choosing two sunny countries along the same geographical area of the Mediterranean, with comparable latitude and subject with the same intestinal disease, eliminates many confounding factors that may bias the conclusions. It is known that geography, older age, higher latitude, winter season, darker skin pigmentation, less sunlight exposure, dietary habits, and absence of vitamin D fortification or non-adherence to vitamin D recommendations among infants are the main conditions that might attribute to hypovitaminosis D.
In order to minimize the age effect, a pathological control group of age-matched children with RAP (group 2) was chosen and compared to an age-matched CD children, coming from two different countries: Israel (group 1) and Spain (group 5). To challenge the age effects, the non-CD pediatric group (group 2) was compared to their parents, thus equilibrating genetic factors and dietary habits. Additionally, the two Spanish group, suffering from the same disease, living in the same climate, latitude, social and dietary habits, but not intra-family relating, permitted to study the age effect on vitamin D levels. The significant negative correlation between the age and vitamin D levels and the significantly lower vitamin D levels in the adult CD Spanish group compared to their pediatric counterparts, strengthen the age effects. Furthermore, the significantly higher percentage of vitamin D deficiency in the two adults group, compared to the three pediatric groups, not related to CD diagnosis, goes along the same conclusion. It is concluded that the age is the major factor affecting serum vitamin D levels. This conclusion is supported by several recent and old dated studies from US, England, and Israel [65, 73, 86, 87].
Several explanations are suggested for the negative effect of the age on vitamin D levels in the celiac patients: (1) Adults are less compliant to gluten-free diet. Gluten elimination improves bone osteopathy and nutritional deficiencies. (2) Children are more exposed to sunlight, being unaware of its deleterious effects. (3) Preventive vitamin D supplementation is a routine in the first year of life, thus delaying the deficiency. (4) Children consume more milk and milk-based products, sometimes fortified with vitamin D. (5) Unrelated to CD, vitamin D deficiency, osteopenia/porosis are age related. It is worthwhile noting that difference in bone mass between children and adults might be explained by the following factors:
a. Children tend to be more motorically active, thus prevent osteopathy b. Smoking and sedentary life is more prevalent in adults. Both are involved in reduced bone mass. c. Gluten elimination in children is much more effective normalization of bone mineral density, compared to adults [81]. d. In general, gluten-free diet is inadequate in calcium and vitamin D [88].
On the same background, it appears that the intestinal inflammation in CD is not a major contributor to the decreased vitamin D. The comparable vitamin D levels in the three pediatric, CD and non-CD, groups are against intestinal inflammation and/or inflammatory factors affecting serum vitamin D. Moreover, one can conclude that malabsorption and dietary deficiencies, sited as contributing to vitamin D deficiency/osteopenia/osteoporosis in CD [11, 13–15, 75–77, 81] are a minor, if at all contributors.
As the genetic and familial influences are concerned, the comparison of the percentage of vitamin D deficiency between the RAP group with their parents further minimizes their influences on vitamin D and maximizes the age effect.
Vitamin D receptors are found in the crypts of CD intestine and alkaline phosphatase, a vitamin D regulated enzyme, exists on their surface enterocytes [89]. Furthermore, no correlation was found, in the present study, between serum vitamin levels and celiac serology levels and the degree of the intestinal injury. Since the amount of those autoantibodies is positively correlated to the degree of intestinal atrophy and the magnitude of the inflammatory infiltrate [90], the minor role played by vitamin D malabsorption in CD is supported.
The west to east gradient in vitamin D status found in the present study is supported by a recent observation in Israel were Ashkenazi Jews had higher vitamin D levels then the Sephardic ones who had a higher levels than the Arabs[74].
The ethnicity influence can be explained by several raisons: (1) Sephardic Jews, Arabs, and Druze have darker skin pigmentation compared to the Christian and the Ashkenazi populations, resulting in reduced skin synthesis of the vitamin [19, 65, 71, 73, 91]. (2) Arab and Druze communities' lives in villages in Israel are more conservative and wear long-sleeved clothes, thus contributing to reduced light skin exposure. The darker skin complexion and the customary clothing most probably join cultural-related habits and other genetic factors distinguishing those ethnic groups. In view of the multiple roles of vitamin D against cancer, autoimmune diseases, infections, diabetes, hypertension, and cardiovascular events, the question arises if the described ethnical hypovitaminosis D affects morbidity/mortality of those communities. Such a phenomenon was described in the USA [19, 65] and recently in Israel [74].
The positive correlation between FTT and vitamin D serum levels is surprising. Is it because those children are supplemented with multivitamins, more often then their non-FTT counterparts?
Hp gastric presence is negatively correlated to serum vitamin D levels. It is plausible that due to the gastric mucosal atrophy and decreased stomach acidity, associated with Hp antritis, vitamin D absorption is affected. Vitamin D deficiency is potentiated after bariatric surgery and after highly selective vagotomy [92, 93]. Alternatively, Hp induces a plethora of proinflammatory cytokines: IL-8, IL-12, gamma-interferon, TNF-alfa [94, 95]. Lastly, since Hp gastritis is accompanied by abdominal pains, nausea and refusal to eat vitamin D consumption may be decreased. Independently of the specific cause, those events could affect vitamin intestinal absorption.
Several studies on CD and the related osteopathy and its consequences recommend routine serum vitamin D evaluation and bone mineral density determination [14, 15, 85, 96–98] while others challenged this approach [16]. Furthermore, some recommend preventing approach by routine vitamin D fortification of the CD population [85, 99, 100]. The present data are going against the routine preventive treatment or fortification of vitamin D in the celiac patients. It is suggested that the approach should be selective. In the pediatric CD age, vitamin D and bone assessment should be applied to malabsorption or chronic diarrhea children. Since a significant negative correlation exists between age and adult CD, it is recommended to investigate this group of age for vitamin D levels and osteopathy and treat accordingly. An alternative approach might be installed by vitamin D routine fortification.
In summary, vitamin D insufficiency and deficiency are prevalent among the CD affected patients. The phenomenon is age and not intestinal injury/inflammation depended, ethnicity and not gender related, and occurs even in sunny countries like Spain and Israel. It is recommended to routinely check the adult CD patients for vitamin D levels and to act selectively in the pediatric CD population.
References
Lerner A, Blank M, Shoenfeld Y (1996) Celiac disease and autoimmunity. Isr J Med Sci 32:33–36
Reif S, Lerner A (2004) Celiac disease and infection. In: infections and Autoimmunity. Shoenfeld, Y. and Rose, N. (Eds) Elsevier B.V. pp.689–692.
Reif S, Lerner A (2004) Tissue transglutaminase—the key player in celiac disease: a review. Autoimm Rev 3:40–45
Shamir R, Eliakim R, Lahat N, Sobel E, Lerner A (2002) ELISA assay of anti endomysial antibodies in the diagnosis of celiac disease: comparison with immunofluorescence assay of anti endomysial antibodies and tissue transglutaminase antibodies. Isr Med Assoc J 4:594–596
Rozenberg O, Lerner A, Pacht A, Grinberg M, Reginashvili D, Henig C, Barak M (2010) A novel algorithm for childhood celiac disease serological diagnosis based upon intestinal biopsies. Crit Rev Allerg Immunol (in press)
Lerner A (2010) New therapeutic strategies for celiac disease. Autoimmun Rev 9:144–147
Lerner A (1994) Factors affecting the clinical presentation and time diagnosis of celiac disease: the Jerusalem and the West Bank-Gaza experience (editorial). Isr J Med Sci 30:294–295
Branski D, Ashkenazy A, Frier S, Lerner A et al (1992) Extra intestinal manifestation and associated disorders of celiac disease. In: Branski D, Rozen P, Kaganoff MF (eds) Gluten-sensitive enteropathy from gastrointest res. Karger, Basel, pp 164–175
Zelnik N, Pacht A, Obeid R, Lerner A (2004) Range of neurological disorders in patients with celiac disease. Pediatrics 113:1672–1676
Lerner A, Makhoul B, Eliakim (2010) Neurological manifestations of celiac disease in children and adults. Eur Neurolog J (in press)
Capriles VD, Martini LA, Arêas JA (2009) Metabolic osteopathy in celiac disease: importance of a gluten-free diet. Nutr Rev 67:599–606
Zanchi C, Di Leo G, Ronfani L, Martelossi S, Not T, Ventura A (2008) Bone metabolism in celiac disease. J Pediatr 153:262–265
Bianchi ML, Bardella MT (2008) Bone in celiac disease. Osteoporos Int 19:1705–1716
Scott EM, Gaywood I, Scott BB (2000) Guidelines for osteoporosis in coeliac disease and inflammatory bowel disease. British Society of Gastroenterology. Gut 46(Suppl 1):1–8
Turner J, Pellerin G, Mager D (2009) Prevalence of metabolic bone disease in children with celiac disease is independent of symptoms at diagnosis. J Pediatr Gastroenterol Nutr 49:589–593
Lewis NR, Scott BB (2005) Should patients with coeliac disease have their bone mineral density measured? Eur J Gastroenterol Hepatol 17:1065–1070
Mora S (2008) Celiac disease in children: impact on bone health. Rev Endocr Metab Disord 9:123–130
Olmos M, Antelo M, Vazquez H, Smecuol E, Mauriño E, Bai JC (2008) Systematic review and meta-analysis of observational studies on the prevalence of fractures in coeliac disease. Dig Liver Dis 40:46–53
Shoenfeld N, Amital H, Shoenfeld Y (2009) The effect of melanism and vitamin D synthesis on the incidence of autoimmune disease. Nat Clin Pract Rheumatol 5:99–105
Albert PJ, Proal AD, Marshall TG (2009) Vitamin D: the alternative hypothesis. Autoimmun Rev 8:639–644
Toubi E, Shoenfeld S (2010) The role of vitamin D in regulating immune responses. IMAJ 12:174–175
Pappa H, Gordon C, Saslowsky T et al (2006) Vitamin D status in children and young adults with inflammatory bowel disease. Pediatrics 118:1950–1961
Nieves J, Cosman F, Herbert J, Shen V, Lindsay R (1994) High prevalence of vitamin-D deficiency and reduced bone mass in multiple sclerosis. Neurology 44:1687–1692
Aguado P, del Campo M, Garces M et al (2000) Low vitamin-D levels in outpatient postmenopausal women from a rheumatology clinic in Madrid, Spain: their relationship with bone mineral density. Osteoporos Int 11:739–744
Kamen D, Cooper G, Bouali H et al (2006) Vitamin-D deficiency in systemic lupus erythematosus. Autoimmun Rev 5:114–117
Di Cesar D, Ploutz-Snyder R, Weinstock R, Moses A (2006) Vitamin D deficiency is more common in type 2 than in type 1 diabetes. Diab Care 29:174
Arnson Y, Amital H, Shoenfeld Y (2007) Vitamin-D and autoimmunity: new aetiological and therapeutic considerations. Ann Rheum Dis 66:1137–1142
Orbach H, Zandman-Goddard G, Amital H, Barak V et al (2007) Novel biomarkers in autoimmune diseases: prolactin, ferritin, vitamin-D, and TPA levels in autoimmune diseases. Ann NY Acad Sci 1109:385–400
Munger K, Levin L, Hollis B, Howard N, Ascherio A (2006) Serum 25-hydroxyvitamin-D levels and risk of multiple sclerosis. JAMA 296:2832–2838
Hewison M (2010) Vitamin D and the immune system: new perspectives on an old theme. Endocrinol Metab Clin N Am 39:365–379
Pelajo CF, Lopez-Benitez JM, Miller LC (2010) Vitamin D and autoimmune rheumatologic disorders. Autoimmune Rev 9:507–510
Shapira Y, Agmon-levin N, Shoenfeld Y (2010) Mycobacterium tuberculosis, autoimmunity, and vitamin D. Clin Rev Allerg Immunol 38:169–177
Holick MF (2010) Vitamin D: extraskeletal health. Endocrinol Metab Clin N Am 39:381–400
Chen S, Sims GP, Chen X et al (2007) Modulatory effects of 1, 25-dihydroxyvitamin-D3 on human B cell differentiation. J Immunol 179:1634–1647
van Etten E, Mathieu C (2005) Immunoregulation by 1, 25-dihydroxyvitamin-D3: basic concepts. J Steroid Biochem Mol Biol 97:93–101
Overbergh L, Decallonne B, Waer M et al (2000) 1alpha, 25-dihydroxyvitamin-D3 induces an autoantigen-specific T-helper 1/T-helper 2 immune shift in NOD mice immunized with GAD65 (p 524–543). Diabetes 49:1301–1307
Bhalla A, Amento E, Serog B, Glimcher L (1984) 1, 25-Dihydroxyvitamin-D3 inhibits antigen-induced T cell activation. J Immunol 133:1748–1754
Lemire J (1992) Immunomodulatory role of 1, 25-dihydroxyvitamin-D3. J Cell Biochem 49:26–31
Lemire JM, Archer D, Beck L, Spiegelberg H (1995) Immunosuppressive actions of 1, 25-dihydroxyvitamin-D3: preferential inhibition of Th1 functions. J Nutr 125:1704S–1708S
Cutolo M, Otsa K, Uprus M, Paolino S, Seriolo B (2007) Vitamin D in rheumatoid arthritis. Autoimmun Rev 7:59–64
Penna G, Amuchastegui S, Cossetti C et al (2006) Treatment of experimental autoimmune prostatitis in nonobese diabetic mice by the vitamin-D receptor agonist elocalcitol. J Immunol 177:8504–8511
Penna G, Adorini L (2000) 1α, 25-dihydroxyvitamin D3 inhibits differentiation, maturation, activation, and survival of dendritic cells leading to impaired alloreactive T cell activation. J Immunol 164:2405–2411
Adorini L, Giarratana N, Penna G (2004) Pharmacological induction of tolerogenic dendritic cells and regulatory T cells. Semin Immunol 16:127–134
Luciano A, Giuseppe P (2008) Control of autoimmune diseases by the vitamin D endocrine system. Nat Clin Pract Rheumatol 4:404–412
Daniel C, Schlauch T, Zugel U, Steinmeyer A et al (2005) 22-ene-25-oxa-vitamin D: a new vitamin D analogue with profound immunosuppressive capacities. Eur J Clin Invest 35:343–349
Carvalho JF, Blank M, Kiss E, Tarr T, Amital H, Shoenfeld Y (2007) Anti-vitamin-D, vitamin-D in SLE: preliminary results. Ann NY Acad Sci 1109:550–557
Ramos-Lopez E, Jansen T, Ivaskevicius V et al (2006) Protection from type 1 diabetes by vitamin-D receptor haplotypes. Ann NY Acad Sci 1079:327–334
Rudko AA, Kondrateva EI, Iankina GN, Loshkova EV, Puzyrev VP (2008) Influence of polymorphism of immune defense modifier genes on celiac disease development and various clinical features of disease in Tomsk population. Mol Biol Mosk 42:42–49
San-Pedro JI, Bilbao JR, Perez de nanclares G, Vitoria JC, Martul P, Castano L (2005) Heterogeneity of vitamin D receptor gene association with celiac disease and type 1 diabetes mellitus. Autoimmunity 38:439–444
Bailey R, Cooper J, Zeitels L et al (2007) Association of the vitamin-D metabolism gene CYP27B1 with type 1 diabetes. Diabetes 56:2616–2621
Huang C, Wu M, Wu J, Tsai F (2002) Association of vitamin-D receptor gene BsmI polymorphisms in Chinese patients with systemic lupus erythematosus. Lupus 11:31–34
Shimada A, Kanazawa Y, Motohashi Y et al (2008) Evidence for association between vitamin D receptor BsmI polymorphism and type 1 diabetes in Japanese. J Autoimmun 30:207–211
Abe J, Nakamura K, Takita Y, Nakano T, Irie H, Nishii Y (1990) Prevention of immunological disorders in MRL/l mice by a new synthetic analogue of vitamin D3: 22-oxa-1 alpha, 25-dihydroxyvitamin-D3. J Nutr Sci Vitaminol 36:21–31
Daniel C, Radeke H, Sartory N et al (2006) The new low calcemic vitamin-D analog 22-ene-25-oxa-vitamin-D prominently ameliorates Th1-mediated colitis in mice. J Pharmacol Exp Ther 319:622–631
Cantorna M, Hayes C, DeLuca H (1996) 1, 25-Dihydroxyvitamin-D3 reversibly blocks the progression of relapsing encephalomyelitis, a model of multiple sclerosis. Proc Natl Acad Sci USA 93:7861–8764
Cantorna M, Humpal-Winter J, DeLuca H (1999) Dietary calcium is a major factor in 1, 25-dihydroxycholecalciferol suppression of experimental autoimmune encephalomyelitis in mice. J Nutr 129:1966–1971
Mathieu C, Waer M, Laureys J, Rutgeerts O, Bouillon R (1994) Prevention of autoimmune diabetes in NOD mice by 1, 25 dihydroxyvitamin-D3. Diabetologia 37:552–558
Munger K, Zhang S, O'Reilly E et al (2004) Vitamin-D intake and incidence of multiple sclerosis. Neurology 62:60–65
Goldberg P, Fleming M, Picard E (1986) Multiple sclerosis: decreased relapse rate through dietary supplementation with calcium, magnesium and vitamin-D. Med Hypotheses 21:193–200
Merlino L, Curtis J, Mikuls T et al (2004) Vitamin-D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women's Health Study. Arthritis Rheum 50:72–77
Birlea S, Costin G, Norris D (2008) Cellular and molecular mechanisms involved in the action of vitamin-D analogs targeting vitiligo depigmentation. Curr Drug Targets 9:345–359
Holick M (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Correale J, Ysrraelit MC, Gaitan MI (2009) Immunomodulatory effects of vitamin D in multiple sclerosis. Brain 132:1146–1160
Adorini L, Penna G (2009) Induction of tolerogenic dendritic cells by vitamin D receptor agonists. Handb Exp Pharmacol 188:251–273
Ginde AA, Liu MC, Camargo CA Jr (2009) Demographic differences and trends of vitamin D insufficiency in the US population, 1988–2004. Arch Intern Med 169:626–632
Pignotti GAP, Genaro PS, Pinheiro MM, Szejnfeld VL, Martini LA (2009) Is a lower dose of vitamin D supplementation enough to increase 25(OH)D status in a sunny country? Eur J Nutr 49:277–283
Mansbach JM, Ginde AA, Camargo CA Jr (2009) Serum 25-hydroxyvitamin D levels among US children aged 1 to 11 years: do children need more vitamin D? Pediatrics 124:1404–1410
Gannage-Yared MH, Chemali R, Yaacoub N, Halaby G (2000) Hypovitaminosis D in a sunny country: relation to lifestyle and bone markers. J Bone Miner Res 15:1856–1862
Mishal AA (2001) Effects of different dress styles on vitamin D levels in healthy young Jordanian women. Osteoporos Int 12:931–935
Kimlin M, Harrison S, Nowak M, Moore M, Brodie A, Lang C (2007) Does a high UV environment ensure adequate vitamin D status? J Photochem Photobiol B 89:139–147
Holick MF (2008) Deficiency of sunlight and vitamin D. BMJ 336:1318–1319
Bischoff-Ferrari H (2009) Vitamin D: what is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol 23:789–795
Mithal A, Wahl DA, Bonjour JP, Burckhardt P et al (2009) Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 20:1807–1820
Oren Y, Shapira Y, Agmon-Levin N, Kivity S, Zafrir Y, Altman A, Lerner A, Shoenfeld Y (2010) Vitamin D insufficiency in a sunny environment: a demographic and seasonal analysis. IMAJ 12:2–7
Walters JR (2003) The role of the intestine in bone homeostasis. Eur J Gastroenterol Hepatol 15:845–849
Bernstein CN, Leslie WD (2003) The pathophysiology of bone disease in gastrointestinal disease. Eur J Gastroenterol Hepatol 15:857–864
Vestergaard P (2003) Bone loss associated with gastrointestinal disease; prevalence and pathogenesis. Eur J Gastroenterol Hepatol 15:851–856
Stenson WF, Newberry R, Lorenz R, Baldus C, Civitelli R (2005) Increased prevalence of celiac disease and need for routine screening among patients with osteoporosis. Arch Intern Med 28:393–399
Legroux-gerot I, Leloire O, Blanckaert F, Tonnel F et al (2009) Screening for celiac disease in patients with osteoporosis. Joint Bone Spine 76:162–165
Stazi AV, Trecca A, Trinti B (2008) Osteoporosis in celiac disease and in endocrine and reproductive disorders. World J Gastroenterol 28:498–505
Capriles VD, Martini LA, Areas JA (2009) Metabolic osteopathy in celiac disease: importance of gluten-free diet. Nutr Rev 67:599–606
Hartman C, Hino B, Lerner A et al (2004) Bone quantitative ultrasound and bone mineral density in children with celiac disease. J Pediatr Gastrointerol Nutr 39:504–510
Walker-Smith JA, Guandalini S, Schmitz J et al (1990) Revised criteria for the diagnosis of celiac disease. Report of the working group of European Society of Pediatric Gastroenterology and Nutrition. Arch Dis Child 65:909–911
Levis S, Gomez A, Jimenez C et al (2005) Vitamin D deficiency and seasonal variation in an adult South Florida population. J Clin Endocrinol Metab 90:1557–1562
Saintonge S, Bang H, Gerber LM (2009) Implication of a new definition of vitamin D deficiency in a multiracial US adolescent population: the national health and nutrition examination survey III. Pediatrics 123:797–803
Hirani V, Tull K, Ali A, Mindell J (2010) Urgent action needed to improve vitamin D status among older people in England! Age Ageing 39:62–68
Lagunova Z, Porojnicu AC, Lindberg F et al (2009) The dependency of vitamin D status on body mass index, gender, age, and season. Anticancer Res 29:3713–3720
Kinsey L, Burden ST, Bannerman E (2008) A dietary survey to determine if patients with celiac disease are meeting current healthy eating guidelines and how their diet compared to that of the British general population. Eur J Clin Nutr 62:1333–1342
Colston KW, Mackay AG, Finlayson C et al (1994) Localization of vitamin D receptor in normal human duodenum and in patients with coeliac disease. Gut 35:1219–1225
Rossi TM, Kumar V, Lerner A, Heitlinger LA, Tucker N, Fisher J (1988) Relationship of endomysial antibodies to jejunal mucosa pathology: specificity towards both symptomatic and asymptomatic celiacs. J Pediatr Gastroenterol Nutr 7:858–863
Yanbin D, Polloc N, Stallmann-Jorgensen IS et al (2010) Low 25-hydroxyvitamin D levels in adolescents: race, season, adiposity, physical activity, and fitness. Pediatrics 125:1104–1111
Toh SY, Zarshenas N, Jorgensen J (2009) Prevalence of nutrient deficiencies in bariatric patients. Nutrition 25:1150–1156
Nilas L, Christiansen C (1987) Vitamin D deficiency after selective vagotomy. Acta Med Scand 221:303–306
D’Elios MM, Amedel A, Benagiano M et al (2005) Helicobacter pylori, T cells, and cytokines: the “dangerous liaisons”. FEMS Immunol Med Microbiol 44:113–119
Hosseini ME, Oghalaie A, Habibi G et al (2010) Molecular detection of host cytokine expression in Helicobacter pylori infected patients via semi-quantitative RT-PCR. Indian J Med Microbiol 28:40–44
Souberbielle JC, Body JJ, Lappe JM, Plebani M, Shoenfeld Y et al (2010) Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: recommendations for clinical practice. Autoimmun Rev 9:709–715
Mimouni FB (2010) Vitamin D status in growing children: Should we routinely screen for vitamin D adequacy. J Pediatr Gastroenterol Nutr 51:S121–S122
Hill ID, Dirks MH, Liptak GS et al (2005) Guidelines for the diagnosis and treatment of celiac disease in children: recommendation of the North American society for pediatric gastroenterology, hepatology and nutrition. J Pediatr Gastroenterol Nutr 40:1–19
Kupper C (2005) Dietary guidelines and implementation for celiac disease. Gastroenterology 128:s121–s127
Blazina S, Bratanic N, Campa AS, Blagus R, Orel R (2010) Bone mineral density and importance of strict gluten-free diet in children and adolescents with celiac disease. Bone 47:598–603
Acknowledgment
To Mrs. Lavi Idit, Department of Epidemiology, Statistic Section, Carmel Medical Center, for her excellent statistic workup and constructive advices.
Author information
Authors and Affiliations
Corresponding author
Additional information
Aaron Lerner and Yinon Shapira contributed equally to this article.
Rights and permissions
About this article
Cite this article
Lerner, A., Shapira, Y., Agmon-Levin, N. et al. The Clinical Significance of 25OH-Vitamin D Status in Celiac Disease. Clinic Rev Allerg Immunol 42, 322–330 (2012). https://doi.org/10.1007/s12016-010-8237-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-010-8237-8