Abstract
Organoid technique has achieved significant progress in recent years, owing to the rapid development of the three-dimensional (3D) culture techniques in adult stem cells (ASCs) and pluripotent stem cells (PSCs) that are capable of self-renewal and induced differentiation. However, our understanding of human female reproductive system organoids is in its infancy. Recently, scientists have established self-organizing 3D organoids for human endometrium, fallopian tubes, oocyte, and trophoblasts by culturing stem cells with a cocktail of cytokines in a 3D scaffold. These organoids express multicellular biomarkers and show functional characteristics similar to those of their origin organs, which provide potential avenues to explore reproductive system development, disease modelling, and patient-specific therapy. Nevertheless, advanced culture methods, such as co-culture system, 3D bioprinting and organoid-on-a-chip technology, remain to be explored, and more efforts should be made for further elucidation of cell–cell crosstalk. This review describes the development and applications of human female reproductive system organoids.

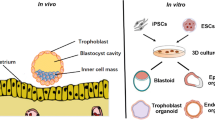
Figure: Applications in developmental biology, disease modelling, and drug discovery of human female reproductive system organoids. ASCs: adult stem cells; PSCs: pluripotent stem cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Organoids are extensions of two-dimensional (2D) biology that present as multicomponent aggregations with tissue-autonomous self-organization involved in homeostasis, regeneration, and development [1, 2]. In recent years, organoid technique has been widely applied in multi-disciplinary research fields, on the basis of more advanced stem cell and three-dimensional (3D) culture skills. This thriving 3D technology provides a novel cell culture method, exhibiting more intuitive spatial structure that makes the exploration of physiological and pathological mechanisms more convenient. Combination of 3D culture skills and stem cells, including adult stem cells (ASCs) and pluripotent stem cells (PSCs), allows self-organized and self-renewing “organoids” present disease processes temporally. Organoids not only exhibit characteristics of traditional 2D cell culture, such as biomarkers and biofunctions, but also show multiple morphological components as well as realize multicellular interactions [1,2,3,4,5]. Up to date, organoids derived from the gut, lungs, prostate, fallopian tube stem cells, and even more advanced structures such as brain, have been established. Organoids from different cell origin can be widely applied in modelling human diseases, understanding disease mechanisms, testing therapeutic or toxic compounds, cell transplantation [6,7,8,9,10], and patient-specific therapies.
The term “organoid” was initially used in oncology to describe teratomas, such as dermoid cysts, and was reported as early as 1946 [2]. Yoshiki Sasai [11] and Hans Clevers [12] pioneered breakthroughs in organoid field with the successful cultivation of optic cup organoids derived from PSCs and intestinal organoids derived from ASCs, respectively. Thereafter, widescale use of stem cells, including ASCs and PSCs, for the formation of 3D organoids began [1, 5, 11, 12]. As ASCs can be only induced into specific cell types similar to those in the origin organs, the cell diversity in an ASC-derived organoid is limited. This shortcoming was overcome by the use of PSCs, which consist of embryonic stem cells (ESCs) and induced PSCs (iPSCs) [2, 5], that can differentiate into almost all cell types. This expanded the cellular diversity and enabled the formation of multi-component cell culture systems. With the rapid progress in stem cell isolation and culture techniques, currently, organoids derived from ASCs and PSCs from several organs, including the brain, liver, retina, endometrium, fallopian tubes, and trophoblast, have been generated for elucidating the mechanisms underlying organogenesis and pathophysiological progression. Particularly, patient-specific iPSC-derived organoids have the potential for significant contribution to personalized medicine.
Unlike other organs, the female reproductive system is directly regulated by multiple hormones that play different roles in several physiological stages such as pregnancy and the menstrual cycle. The application of organoids to the field of female reproductive system research is still an emerging area, even though the first report in this field was made in 1988 by Rinehart et al. [13], which was prior to the emergence of the general organoid research in 1989 [1]. Rinehart et al. described an endometrial organoid derived from the human endometrium epithelium without specific selection of cell types, which contributed to the establishment of 3D stem cell structure from fallopian tube epithelial cells (FTECs), trophoblast cells, and follicles. Recently, researchers have reported several female reproductive organoids displaying a near-native and hormone-regulated microanatomy with organ-specific differentiated cell types and tissue compartmentalization; they exhibit functionalities similar to those of in vivo organs owing to their remarkable self-organizing properties [1, 2]. This finding may solve several research-related issues, such as low sample accessibility, ethical dilemmas, and homology issues in 2D experiments, and realize structural polarity and differentiated function in the study model. Above all, the 3D organoid technique can provide a promising strategy for further research on female reproduction in areas investigating etiology of endometrial disorders, carcinogenesis, drug screening, or implantation issues. Nevertheless, organoid research on the reproductive system is new and few, and culture techniques are empirical; furthermore, its applications are limited.
In order to review all the scientific reports on human female reproductive organoids, we used the terms ‘“endometrium” or “fallopian tubes” or “ovaries” or “trophoblast” or “female reproductive system”’ as well as ‘“organoids” or “organotypic” or “organogenesis” or “three-dimensional” or “polarization”’ as key words to search the PubMed database. To date, approximately 26 articles on 3D modelling of the endometrium [3, 13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37] (except for tumoroids) have been published; these investigate organogenesis, simulate biological functions, and even establish disease models to elucidate the etiology of endometrial disorders, including endometriosis and carcinoma, with five studies on fallopian tubes [38,39,40,41,42], three on trophoblasts of the placenta [4, 43, 44] (except for animal organoid models and embryogenesis), and only one on follicle organoids [45] (Table 1). The organoids described in this review are strictly defined as human ASC- and PSC-derived 3D self-organized architectures grown in vitro. We excluded patient tumor-derived organoids because their biological behavior is more similar to that of tumor cells. Additionally, as ovarian surface epithelial (OSE) cell 3D models [46, 47] lack stem cell origin and induced differentiation, they were also excluded from this review.
Organoids of the Female Reproductive System
Generally, the cultivation of organoids requires three main components: original cells, extracellular matrix (ECM), and endogenous and exogenous signals. The most common original cells for female reproductive system organoids are the organ-specific ASCs and iPSCs; only oocyte organoids are derived from ESCs. ECM provides 3D support and Matrigel, which is the most common 3D scaffold, plays a key role in organoid culture system. Additionally, other 3D scaffold materials, such as methacrylamide-functionalized gelatine (GelMA) hydrogel [36] or scaffolds with collagen [32] for endometrium, poly-2-hydroxyethyl methacrylate (polyHEMA) for fallopian tubes [40], and co-culture systems [20, 27, 32], that are suitable for various culture methods have also been applied in reproductive organoids. A specific culture medium containing a cocktail of growth factors to maintain self-renewal capability or induce differentiation provides a neutralizing environment.
Human Endometrial Organoids
The endometrium is distinct from other organs because of the complex periodic changes it undergoes throughout the menstrual cycle that correlate with hormonal changes. The functional layer, mainly consisting of glands, undergoes regeneration, differentiation, secretion, and atrophy, which are under the control of the hypothalamic–pituitary–ovarian axis and respond to sexual hormones. During pregnancy, the endometrium transforms into the decidua, which provides a microenvironment essential for placentation of the conceptus [3, 29, 33]. Endometrial problems, such as endometriosis, endometrial cancer, or implantation issues, can all be attributed to changes in endometrial physiological development under different hormone conditions [24, 27]. Thus, to study these, the 3D organoid technique, simulating endometrial development in terms of morphology and biological functions, including hormonal reactions and even pathological processes, is advantageous [1,2,3, 13, 14, 35].
There are three different types of endometrium organoids, as described below, for different stem cell origins according to the present reports: endometrial epithelium-derived, CD146+ mesenchymal stem cells-derived, and endometrial stromal cell-derived organoids, among which the epithelium-derived one is the most common.
Self-renewing ASCs derived from the endometrial epithelium, several types of 3D support, and empirical culture media are essential for endometrial epithelial organoid performance (Fig. 1). Because of the unknown identities and locations of stem cell groups in the human endometrium, original cells for endometrial organoids are often isolated from the unselected endometrial epithelium at specific physiological or pathological stages. The primary gland-like organoid was first established using endometrial epithelium in 1988 by Rinehart et al. [17]. Its structure indicated that a small population of clonogenic epithelial cells, with high proliferative potential that are within the human endometrium, can differentiate into large gland-like structures. Since this discovery, self-renewing cells for endometrium organoids have been obtained from the decidua, proliferative and secretory endometrium, and atrophic endometrium [3, 25, 26, 33]. Several 3D supporting structures have been applied to epithelial cells, such as Matrigel droplets, GelMA hydrogel [36], scaffolds with collagen or fibrin [32], or cocultured stromal cells [14, 20, 27]. Moreover, the use of specific organoid expansion medium containing epidermal growth factor (EGF), Noggin, and R-spondin-1 (ENR) provided strong evidence of enhanced clonogenic capability [3, 13, 14, 16, 33]. A total of 3–4 weeks were required for the formation and polarization of spheroid-like structures as well as the appearance of stromal cells that produce and secrete collagen in the center [20]. The established organoids could be expanded at passage ratios of 1:2 or 1:3 every 7–10 days for >6 months.
Organoids of the endometrial epithelium recapitulate several structural or functional characteristics of human endometrial gland-like epithelial tissue, including cell morphology, proliferation and differentiation, secretory properties, sexual hormone responsiveness as well as gene expression patterns similar to that of the origin tissue [3, 13, 16, 22, 25, 26, 33]. Under electron microscope, the organoid glands present endometrial epithelium-like polar columnar cells facing a central lumen along with junctional complexes/desmosomes and microvilli; cytoplasm containing abundant rough endoplasmic reticulum, Golgi bodies, and numerous secretory vesicles showed evidence of secretory activity identifying the endometrial characteristics [3, 13, 33, 48]. Turco et al. [3, 13,14,15] and Yang et al. [30] demonstrated the expression of original endometrial protein markers, such as epithelial markers and epithelial progenitor markers, in endometrial organoids; they described a more detailed profile of endometrium organoid from epithelial progenitors. Moreover, the gene expression profiles and gene ontology (GO) analysis revealed the glandular epithelium signatures of these organoids [3, 18, 33]. Response to sexual hormones such as estrogen (E2) and progesterone (P4) in endometrial organoids is considered to be characteristic of a successful organoid. Specifically, such excellent responses can be induced in endometrial organoids where multiple biomarkers, such as estrogen or progesterone receptors, and proliferative marker-antigen KI67 (Ki67) have been identified [3, 19, 24, 33]. Moreover, Turco et al. [3] reported that estrogen along with progesterone and cyclic adenosine monophosphate (cAMP) induced downregulation of SOX9, a marker of progenitor cells expressed in the base of endometrial glands, as well as growth factor-binding protein-1 (IGFBP1) and prolactin (PRL), which indicates the occurrence of decidual reaction when simulating pregnancy in the organoids [3, 19, 20, 24, 29, 32, 33]. In the presence of another kind of progesterone, medroxyprogesterone acetate, a significant decrease in cell proliferation was detected by Bläuer et al. [14]. According to Kamelle et al., such cells can be manipulated with retinoids and steroids to assume the histological features of the proliferative and secretory phases [24]. In summary, endometrial 3D organoids can recapitulate the original gland structures and biological functions.
The endometrial epithelium 3D organoids can provide a biological structure or disease model for identifying molecular signals, exploring disease etiology, and carcinogenesis [23]. Hennes et al. demonstrated and validated the functional expression of the mechanosensitive PIEZO1 channel in an endometrial organoid; PIEZO1 channel was identified as an important signal pathway that is a potential target for the development of novel treatments to further improve the success of implantation processes [31]. In terms of disease simulation, genetic profiles, transcriptional differentiation, marker identification, and pathogen interactions, organoids can be used to model the development of recurrent miscarriage, endometriosis, endometrial carcinoma, or other endometrial disorders [23, 28]. For instance, endometriotic organoids with a basalis-like phenotype in the ectopic functionalis layer suggested that abnormally located SSEA1+/SOX9+ endometrial epithelial cells may contribute to the pathogenesis of endometriosis as reported by Hapangama et al. [34]. Additionally, Valentijn et al. applied this spheroid formation technique for detecting human endometrial epithelial telomerase, which is important for epithelial proliferation and glandular formation and has potential implications for endometriosis [17]. To determine the hormone reaction within endometrial organoids, Wiwatpanit et al. [27] employed androgens to observe pathological endometrial development consistent with that resulting in polycystic ovarian syndrome (PCOS). Boretto et al. [28] successfully established organoids from precancerous pathologies, including endometrial hyperplasia and Lynch syndrome, to observe inherited gene mutations so as to further investigate carcinogenesis. Bishop et al. [21] proved the positive effect of insulin in promoting proliferation and carcinogenesis in endometrial cells within organoids. Further, Łaniewski et al. [22, 35] suggested the application of this 3D endometrial epithelial cell model to study host interactions with vaginal bacteria and Neisseria gonorrhoeae for improving treatment strategies. However, problems during implantation and the secretion of uterine histotrophs during early pregnancy remain to be investigated.
Further, the first successful construction of endometrial-like epithelium in a 3D culture system using CD146+ mesenchymal stem cells derived from human endometrium has been reported [25, 26]. This kind of organoid was embedded in a collagen–Matrigel scaffold on top of smooth muscle cells and was cultured with complete DMEM/F12 with 10% fetal bovine serum. Despite the unpopularity of CD146+ cell isolation compared to epithelial stem cells for generating endometrium organoids, this culture method provided a new direction to explore more complete endometrial organoid generation. It also demonstrated the potential application of such cultures in regenerative medicine, for example, construction of endometrium in patients with endometrial deficiencies such as Asherman syndrome and endometrial atrophy. Such culture systems may also play a role in human embryo implantation-related studies. In addition, the type of stem cell used in this system may serve as a bridge between undifferentiated endometrial epithelial cells and organoid genesis.
Moreover, 3D endometrial stromal cell models could also be established as another key part of endometrium organoids. Normally, either stromal fibroblasts (EMSFs) derived from iPSCs through staged induction or human endometrial stromal cells (HESCs) can be used origin cells. iPSC-derived EMSFs cultured with multi-hormones containing E2, progestin and 8-bromoadenosine 3′,5′- cAMP were found to simulate hormone responsiveness of the endometrial stroma. Markers for decidualization, such as Forkhead box O1 (FOXO1), HAND2, IGFBP, and PRL, were found to be up-regulated. Moreover, RNA sequencing (RNAseq) analysis of these EMSFs confirmed a transcriptional signature similar to that in human endometrial stroma [37]. Similarly, HESCs cultured in GelMA hydrogel and exposed to hormonal cues also exhibited decidual response similar to that of the human endometrial stroma, as indicated by the secretion of two decidual proteins, PRL and IGFBP1. In addition, an HESC plus human umbilical vein endothelial cell (HUVEC) coculture system mimicked the endometrial angiogenesis network, as indicated by CD31 staining [36]. Thus, these two methods provided a more convenient and sufficiently powerful means to study decidualization, human embryonic implantation, and vessel remodeling.
Human Fallopian Organoids
The fallopian tube epithelium (FTE), which is lined by simple columnar epithelium containing secretory and ciliated cells, is critical for human reproduction and has been implicated as a site of origin for high-grade serous ovarian cancer (sHGSC) [38, 39, 49, 50]. Therefore, organoids derived from the FTE may aid in exploring the etiology of infertility in infection models, induction of tumor growth by specific stimulators, and simulation of changes in the plasma concentrations of drugs.
Generally, self-renewing FTECs that are considered ASCs and a 3D support system with conditioned culture media is required for generation of the fallopian tube organoids (Fig. 2). FTECs isolated from patients and seeded to form 3D organoids was initially reported by Lawrenson et al. in 2013 [40]. Matrigel or PolyHEMA is normally used as a 3D support [38, 40] supplemented with a cocktail of growth factors to modulate the Wnt/Notch pathway, which contributes to stemness [38]. Co-culture with fallopian mesenchymal stem cells (FTMSCs) and HUVECs in Matrigel [42] was found to provide a more supportive 3D scaffold for a contracted organoid. The progeny cells were passaged at a 1:3 ratio every 2–3 weeks and could be expanded over a long period (>3 months); they consisted of both secretory and ciliated cells, demonstrating the bipotential of the progenitor unciliated cells, which did not appear to have cilia in the first 2 weeks of culture.
Fallopian organoids replicate the mucosal fold architecture and exhibit several biological functions similar to those of the origin tissue. Morphologically, FTE organoids exhibit highly polarized columnar cells and high-order epithelial tissue architecture analogous to that of the origin FTE. In particular, they exhibit precisely aligned nuclei, similar functional tight junctions, restricted localization of the main epithelial adhesion molecule E-cadherin (CDH1) to the lateral membrane, and the orientation of the apical pole to the luminal side [38, 40, 42]. Moreover, 3D-cultured FTE consistently clustered with luteal phase fallopian tube epithelium as observed by Lawrenson et al. [40]. Secretory epithelial markers, such as vimentin, FOXJ1, PAX8, and detyrosinated tubulin, as well as the hallmark carbohydrate antigen 125 (CA125) [42] were detected in the FTE organoids, which were similar to the origin cells with respect to their function. With respect to cell differentiation in the organoid, the loss of PAX8 expression [42] coincided with the ciliated phenotype. Moreover, the downregulation of Wnt/Notch pathway was observed in the gene profile of FTE organoid, which is essential for differentiation. Fallopian organoids showed a good response to sexual hormones in terms of upregulation of related genes such as those associated with the menstrual period or pregnancy, which was similar to the expression pattern observed in the human fallopian tube epithelium [38]. In addition, the performance of 3D organoids was reportedly more similar to that of human fallopian tube tissue, and presented different gene profiles compared with those in 2D cell lines, such as a higher gene expression during proliferation [40].
In addition to FTE-derived organoids, fallopian tube organoids can also be derived from iPSCs, which accurately simulate the organogenesis of the urogenital system [39] (Fig. 2). Three different iPSC lines (87iCTR-n3, 01iMEC-n4, and 14iCTR-n6) were used to induce mesoderm formation, but only 87iCTR-n3 cell line was verified to be effective. During the organoid construction, determining the expression and location of markers at each step was necessary for verifying the correct differentiation into fallopian tubes rather than nephric ducts and uretic buds; for example, activin A with CHIR99021 for inducing mesoderm development, stepwise addition of BMP4 for regulating the intermediate mesoderm fate, followed by Wnt4 and follistatin to replicate the Mullerian duct were carefully monitored. Matrigel served as a 3D scaffold with pro-Mullerian growth factors that promoted FTE precursor function. However, the preferred mediums were different depending on the sequential stages. E2, P4, and conditional media isolated from patient tissue stimulated the anatomic formation of tubes that were identified by the expression of ciliated FTE marker tubulin beta 4A (TUBB4A), secretory cell markers oviductal glycoprotein 1 (OVGP1) and PAX8, and epithelial cell marker CDH1, similar to that observed in the primary tissue. Interestingly, iPSC-derived FTE organoids closely mimicked the precise physiology and anatomy of the human FTE.
FTE organoids provided a disease model for chronic chlamydia infection by demonstrating the role of epithelial homeostasis in the defense against this pathogen as reported by Kessler et al. [41]. However, problems related to long-term culturing and functional maturity need to be resolved for future investigations regarding the origin of sHGSC.
Trophoblast Organoids
Trophoblasts from early pregnancy play essential roles in early placenta formation and implantation, especially in the invasion process involved in spiral artery remodeling. Impaired trophoblast function is the underlying reason for pregnancy complications such as preterm delivery, recurrent abortion, and preeclampsia [4, 43]. Cytotrophoblasts (CTBs), are bipotent ASCs that exist in the placenta in the first trimester and have been identified as progenitors of different cell subtypes such as syncytiotrophoblasts (STBs) and invasive extravillous trophoblasts (EVTs). Therefore, a 3D self-renewing model of CTB-derived trophoblast organoids may be valuable for imitating implantation and exploring the etiology of placental diseases.
Normally, CTBs are considered stem cell origin for trophoblast organoids, which are cultured in trophoblast organoid medium (TOM) with the analogous defined growth factors mentioned above, an essential and empirical culture medium [4, 43] (Fig. 3a). CTB organoids (CTB-ORGs) generally originated from proliferative cell clusters [4, 43] that were obtained by enzymatic digestion of 6–9-week-old placentas containing different trophoblast types. Neutralizing Matrigel with low levels of growth factors provided 3D scaffold for isolated trophoblasts cultured in TOM containing EGF, fibroblast growth factor 2 (FGF2), CHIR99021 (a Wnt activator), A83-01 [a tumor growth factor beta (TGFβ) and Sma-Mad (SMAD) inhibitor], and R-spondin 1. The cluster expanded quickly and could be passaged for approximately 1 week.
Trophoblast organoid modelling and applications. (a) Origin tissue from human villi; (b) Inducing trophectoderm from iPSCs in limited area; (c) Maternal–fetal interface model for trophoblast invasion and cross-talks. pM placental macrophages, pSC placental stromal cells, pEC placental endothelial cells, STB syncytiotrophoblast, EVT extra villous trophoblast, CTB cytotrophoblasts, dNK decidual natural killer cell
CTB-ORGs significantly simulated the multicomponent morphology, differentiation ability, and specific trophoblast gene expression patterns found in human placental villi [4, 43]. Morphologically, hematoxylin and eosin staining and immunofluorescence staining of CTB-ORGs revealed densely packed cell clusters of epithelial origin with fused regions in the centers, similar to that of villous CTBs (vCTBs) in first-trimester placenta. Moreover, representative electron transmission microscopy images of a CTB-ORG showed a stippled line indicating the boundary between CTBs and STBs, which indicated its differentiation potential as reported by Haider et al. [4]. In terms of biofunctions, CTB-ORGs showed vCTB characteristics such as stemness, proliferation, fusion, with staining of epithelial cell adhesion molecule, CDH1, Ki67, and tumor protein 63 (TP63). Fusion between hormone-secreting STBs was also observed in CTB-ORGs, along with staining of CD46 and CD71, a characteristic of vCTBs [4, 43].By adapting the EVT differentiation protocol with EVT medium lacking Wnt signaling [8] for verifying organoid differentiation function, it was found that human leucocyte antigen-G (HLA-G+) cells emerged as outgrowths of the organoids, digested the Matrigel to form tracks, and eventually adhered to the plastic base [43]. Expression of functional genes in CTB-ORGs have been detected through mRNA sequencing or more completely through RNAseq. To investigate the overlap of gene expression in CTB-ORGs and vCTBs, genetic profiling was performed, and more than 40% of upregulated genes were identified [4].
However, Li et al. [44] described an entirely different method to develop trophoblast cystic structures form human iPSCs (hiPSCs) using the ChiPSC22 cell line (Fig. 3b). I-Matrix-551 and empirical medium were used to support the cysts in a limited culture area. The cysts were observed to have characteristics in common with trophectoderm (TE), including a hemispherical shape, a clear interior cavity, and a thin enclosing wall. The expression of key pluripotency genes and trophoblast lineage-specific genes, such as TP67, was analyzed through mRNA detection. Immunostaining of TP63 and E-cadherin provided evidence for trophoblast cyst formation; the presence of human chorionic gonadotropin in the cytoplasm was confirmed, indicating that the multinucleated cells were STBs, which contributed to the cell diversity of TE-like organoid. Thus, the TE-like organoids showed potential as a new method for implantation exploration.
Although this organoid modelling strategy has been widely applied in spiral artery remodeling by trophoblast invasion in vitro, its practical application in placental diseases is lacking. (Fig. 3c). Researchers have reportedly embedded human primary EVTs in Matrigel to observe the effects of granulocyte-macrophage colony-stimulating factor (GM-CSF) on trophoblast invasion capability via microfluidics assays [51]. Additionally, maternal–fetal interactions attributed to tubulogenesis were identified through co-culturing of decidual natural killer (dNK) cells inducing CTBs and HUVECs [51, 52]. Nonetheless, it is essential to further optimize the culture conditions to improve trophoblast self-renewal, specificity, and differentiation in CTB-ORGs, and more efforts are required towards establishment of such disease models [4, 43].
Additionally, several cell lines, such as the Bewo, JEG3, HTR8, and Sw.71 cell lines, were previously utilized to form 3D structures within collagen gel types and corresponding culture media prior to the development of CTB-ORGs. The resulting models were applied to recapitulate placental STB development and microbial resistance [53], evaluate the efficacy of different types of ECM [54], assess the distinctions between 3D structures and 2D cells [55], and help establish invasion models together with HUVECs [51, 52, 56]. However, these 3D models were not considered “organoids” because of their improper cell origins.
Ovarian 3D Modelling and Oocyte Organoids
Human ovaries are covered with a monolayer of flat/cuboidal mesothelial-type cells referred to as the ovarian surface epithelium (OSE) [46], which represents the origin of approximately 90% of all malignant ovarian tumors including epithelial ovarian cancers [46, 47]. Therefore, 2D or 3D modelling [46, 47] of primary OSE has been a research focus for a long time. Although 3D culturing of normal OSE [46] could be applied to explore the etiology of endometriosis [47], the stemness of the OSE has not been assessed for constructing organoids. Hence, we have not described this in detail as a conventional organoid in the present review.
Human oocytes play a key role in fertility; however, few studies have provided evidence for constructing 2D or 3D structures of human oocyte-like cells in vivo. The first follicle-like cell (FLC) structure was established from human ESCs (hESCs), which can differentiate into germ cell lineages, in 2017 by Jung et al. [45]. The hESC lines H9 and HSF6 (female XX lines) were seeded in neutralizing Matrigel with three different types of differentiated media. Upregulation of DAZL and BOULE pathway promoted entry into meiosis, and growth differentiation factor 9 (GDF9) and bone morphogenetic protein (BMP15) were applied as stimulators for FLC formation. Immunofluorescent staining of PRDM9, gH2AX, SC, and SYCP3 identified the occurrence of meiosis similar to that observed in an oocyte. The FLC transcriptome indicated a primordial follicle identity, as evidenced by the presence of the oocyte-specific markers, such as spermatogenesis and oogenesis-specific basic helix-loop-helix 2 (SOHLH2), zona pellucida glycoprotein 2 (ZP2), homeobox protein (NOBOX), and H1FOO, as well as expression of genes encoding cytochrome P450/family 19/subfamily A (CYP19A) and R-spondin-1 (RSPO1) in granulosa cells. Moreover, FLCs transplanted into mouse kidney capsules showed more oocyte biofunctions with upregulated biological markers such as anti-Müllerian hormone (AMH), enhanced cuboidal morphology of the surrounding cells, and germinal vesicle-like staining in the oocyte-like cells. This system may assist in investigating genes or mechanisms involved in human germ cell development, including long noncoding RNAs (lncRNAs), which have a low degree of conservation among species.
Application of Female Reproductive System Organoids
As previously described, organoids have important applications in investigations regarding tissue homeostasis, regeneration, and development [1, 2]. ASC-derived organoids are capable of structural and functional regeneration of the organ, and thus play an important role in tissue repair in vivo and in vitro [9]. Organoids established from differentiated hESCs could potentially identify gene targets for new drugs [10]. Moreover, iPSCs derived from somatic cells by direct reprogramming provides an effective origin cell for establishing patient-specific 3D organoids [6,7,8]. Combining CRISPR/Cas9, the most popular gene editing technique, with patient-specific iPSC-derived organoids may mimic the disease process, phenotype, and micro-environment in vitro for studying gene disorders. Particularly, they may provide an opportunity to repair gene defects ex vivo. Furthermore, iPSC-derived organoids also offer a novel method to study sporadic diseases [7].
Rebuilding the functional layer of the endometrium or fallopian epithelium may contribute to tissue repair and prevent infertility and early-onset of menopause [3]. In addition, organoids would be useful for the exploration of carcinogenesis, drug efficiency, dysfunctions and etiology of endometriosis, metabolism pathways, pathogen interactions, and hormone reactions. By inducing the progeny of organoids to differentiate into various subtypes, such as CTB-ORG-derived STBs and EVTs [4, 43], physiological cell lines can be established to explore organogenesis, biological functions such as hormone secretion, spiral artery remodeling, maternal–fetal interactions, and the putative development of diseases, such as ischemic placental diseases and implantation disorders. Owing to the benefits of empirical coculture methods with proper combination of different cell types in the preferred ECM, it would also be possible to imitate a whole physiological system with multi-organoid coculturing for further investigation of pathological interactions. Moreover, 3D organoids raise fewer ethical concerns and may be considered a better replacement of animal models or even clinical trials, thereby making them more suitable for drug tests and factor induction due to their similarities with primary lesions [57, 58].
Limitations in the Development of Human Female Reproductive System Organoids
Compared to different kinds of gel scaffolds used in conventional organoids, bioprinting and organoid-on-a-chip technology provide more specific 3D biomimetic structures for stem cell-derived organoids. A few miniaturized organs have been established through these two methods, such as bioprinting bone marrow cells within bio ink [59], heart-on-a-chip with adult heart-like functions [60], and cancer metastasis models [61]. These leading engineering approaches allow precise customization of culture systems enabling them to be more similar to the human physiology for drug discovery as well as exploration in cancer bio behavior. Further, they may help realize multiorgan coculture to manufacture organ environment [62]. For instance, embedding JEG3 on a chip can precisely interact with HUVECs, which acts as a placenta unit in the maternal–fetal interface for placental disorder research [62]. Since no innovative progress has been reported in the human reproductive system till date, the potential to generate human female reproductive system organoids with 3D bioprinting and organoid-on-a-chip technology has great significance. In future, organ coculture systems may be constructed using these technologies to represent multi system disorders, such as preeclampsia and hormone related diseases, in a micro vision for female reproductive system.
Despite the progress in this area, all the methods associated with organoids are empirical. Most organoids cannot replicate the complete architecture of native organs in terms of stemness preservation and maturation, especially PSC-derived organoids. Crosstalk and immunological reactions between different compartments have not been widely realized. Moreover, there have been only a few successful cases of human ovary organoids with hormone secretion. We still lack the evidence necessary to construct models of diseases such as preeclampsia and HELLP syndrome, that indicate the insufficient invasion of trophoblasts during implantation and pregnancies. Furthermore, organoids with gene editing technique like CRISPR/Cas9, may cause complications such as insertional inactivation of tumor suppressor genes or activation of oncogenes [9].
Conclusions
Overall, organoids are capable of mimicking the cell type composition and functionality of native organs, and thus serve as better tumor models for drug screening. In case of the human female reproductive system, there is a wide range of potential for precise cancer treatment and etiological exploration. However, we still need to focus on improving culture conditions for the cost effectiveness, multi-organoid coculturing methods, and vessel modelling as well as further co-culture models including immune cells. Additionally, we need to expand not only-organ derived organoids but also include stem cell-derived organoids as a model system.
References
Giuliana, R., Andrea, M., & Lutolf, M. P. (2018). Progress and potential in organoid research. Nature Reviews Genetics, 19, 671–687.
Kai, K., & Hans, C. (2016). Organoids: Modeling development and the stem cell niche in a dish. Developmental Cell, 38, 590–600.
Turco, M. Y., Lucy, G., Jasmine, H., et al. (2017). Long-term, hormone-responsive organoid cultures of human endometrium in a chemically defined medium. Nature Cell Biology, 19, 568–577.
Sandra, H., Gudrun, M., Leila, S., et al. (2018). Self-renewing trophoblast organoids recapitulate the developmental program of the early human placenta. Stem Cell Reports, 11, 537–551.
Lancaster, M. A., & Knoblich, J. A. (2014). Organogenesis in a dish: Modeling development and disease using organoid technologies. Science, 345, 1247125.
Kazutoshi, T., Koji, T., Mari, O., et al. (2007). Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell, 131, 861–872.
In-Hyun, P., Natasha, A., Hongguang, H., et al. (2008). Disease-specific induced pluripotent stem cells. Cell, 134, 877–886.
Narasimman, G., Abdulrhman, A., Sheeja, R., et al. (2018). Adult stem cells for regenerative therapy. Progress in Molecular Biology and Translational Science, 160, 1–22.
Youssef, H., & Anis, F. (2020). Organoid models of human endometrial development and disease. Frontiers in Cell and Developmental Biology, 8, 84.
Thomson, J. A., Itskovitz-Eldor, J., Shapiro, S., et al. (1998). Embryonic stem cell lines derived from human blastocysts. Science, 282, 1145–1147.
Mototsugu, E., Nozomu, T., Hiroki, I., et al. (2011). Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature, 472, 51–56.
Toshiro, S., Vries, R. G., Snippert, H. J., et al. (2009). Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature, 459, 262–265.
Rinehart, C. A., Lyn-Cook, B. D., & Kaufman, D. G. (1988). Gland formation from human endometrial epithelial cells in vitro. In Vitro Cellular & Developmental Biology, 24, 1037–1041.
Bläuer, M., Heinonen, P. K., Martikainen, P. M., Tomás, E., & Ylikomi, T. (2005). A novel organotypic culture model for normal human endometrium: Regulation of epithelial cell proliferation by estradiol and medroxyprogesterone acetate. Human Reproduction, 20, 864–871.
Nguyen, H. P. T., Xiao, L., Deane, J. A., et al. (2017). N-cadherin identifies human endometrial epithelial progenitor cells by in vitro stem cell assays. Human Reproduction, 32, 2254–2268.
Fitzgerald, H. C., Dhakal, P., Behura, S. K., et al. (2019). Self-renewing endometrial epithelial organoids of the human uterus. Proceedings of the National Academy of Sciences of the United States of America, 116, 23132–23142.
Valentijn, A. J., Saretzki, G., Tempest, N., Critchley, H. O., & Hapangama, D. K. (2015). Human endometrial epithelial telomerase is important for epithelial proliferation and glandular formation with potential implications in endometriosis. Human Reproduction, 30, 2816–2828.
Syed, S. M., Kumar, M., Ghosh, A., et al. (2020). Endometrial axin2 cells drive epithelial homeostasis, regeneration, and cancer following oncogenic transformation. Cell Stem Cell, 26, 64–80.e13.
Sandra, H., Magdalena, G., Burkard, T. R., et al. (2019). Estrogen signaling drives ciliogenesis in human endometrial organoids. Endocrinology, 160, 2282–2297.
Murphy, A. R., Teerawat, W., Lu, Z., et al. (2019). Generation of multicellular human primary endometrial organoids. Journal of Visualized Experiments, 152. https://doi.org/10.3791/60384.
Bishop, E. A., Stan, L., Elangovan, T., et al. (2014). Insulin exerts direct effects on carcinogenic transformation of human endometrial organotypic cultures. Cancer Investigation, 32, 63–70.
Paweł, Ł., Gomez, A., Hire, G., et al. (2017). Human three-dimensional endometrial epithelial cell model to study host interactions with vaginal bacteria and Neisseria gonorrhoeae. Infection and Immunity, 85, e01049-16.
Benbrook, D. M., Stan, L., James, R.-M., et al. (2008). Gene expression analysis of biological systems driving an organotypic model of endometrial carcinogenesis and chemoprevention. Gene Regulation and Systems Biology, 2, 21–42.
Kamelle, S., Sienko, A., & Benbrook, D. M. (2002). Retinoids and steroids regulate menstrual phase histological features in human endometrial organotypic cultures. Fertility and Sterility, 78, 596–602.
Fayazi, M., Salehnia, M., & Ziaei, S. (2017). In-vitro construction of endometrial-like epithelium using CD146 mesenchymal cells derived from human endometrium. Reproductive Biomedicine Online, 35, 241–252.
Johnson, M. H. (2017). First evidence that endometrial-like organoids can develop from the endometrial mesenchymal stem/stromal cell population. Reproductive Biomedicine Online, 35, 239–240.
Wiwatpanit, T., Murphy, A. R., Lu, Z., et al. (2020). Scaffold-free endometrial organoids respond to excess androgens associated with polycystic ovarian syndrome. The Journal of Clinical Endocrinology and Metabolism, 105, 769–780.
Boretto, M., Maenhoudt, N., Luo, X., et al. (2019). Patient-derived organoids from endometrial disease capture clinical heterogeneity and are amenable to drug screening. Nature Cell Biology, 21, 1041–1051.
Classen-Linke, I., Kusche, M., Knauthe, R., & Beier, H. M. (1997). Establishment of a human endometrial cell culture system and characterization of its polarized hormone responsive epithelial cells. Cell and Tissue Research, 287, 171–185.
Yang, H., Sungwon, H., Haekwon, K., et al. (2002). Expression of integrins, cyclooxygenases and matrix metalloproteinases in three-dimensional human endometrial cell culture system. Experimental & Molecular Medicine, 34, 75–82.
Aurélie, H., Katharina, H., Matteo, B., et al. (2019). Functional expression of the mechanosensitive PIEZO1 channel in primary endometrial epithelial cells and endometrial organoids. Scientific Reports, 9, 1779.
Barros, F. S. V. (2017). Characterization of human endometrial glandular epithelium in vitro and in vivo (pp. 1–252). Warwick: Division of Biomedical Sciences Warwick Medical School University of Warwick.
Boretto, M., Cox, B., Noben, M., et al. (2017). Development of organoids from mouse and human endometrium showing endometrial epithelium physiology and long-term expandability. Development, 144, 1775–1786.
Hapangama, D. K., Drury, J., Da Silva, L., et al. (2019). Abnormally located SSEA1+/SOX9+ endometrial epithelial cells with a basalis-like phenotype in the eutopic functionalis layer may play a role in the pathogenesis of endometriosis. Human Reproduction, 34, 56–68.
Łaniewski, P., & Herbst-Kralovetz, M. M. (1997). Analysis of host responses to Neisseria gonorrhoeae using a human three-dimensional endometrial epithelial cell model. Methods in Molecular Biology, 2019, 347–361.
Zambuto, S. G., Clancy, K. B. H., & Harley, B. A. C. (2019). A gelatin hydrogel to study endometrial angiogenesis and trophoblast invasion. Interface Focus, 9, 20190016.
Miyazaki, K., Dyson, M. T., Coon, V., John, S., et al. (2018). Generation of progesterone-responsive endometrial stromal fibroblasts from human induced pluripotent stem cells: Role of the WNT/CTNNB1 pathway. Stem Cell Reports, 11, 1136–1155.
Kessler, M., Hoffmann, K., Brinkmann, V., et al. (2015). The Notch and Wnt pathways regulate stemness and differentiation in human fallopian tube organoids. Nature Communications, 6, 8989.
Yucer, N., Holzapfel, M., Vogel, T. J., et al. (2017). Directed differentiation of human induced pluripotent stem cells into fallopian tube epithelium. Scientific Reports, 7, 10741.
Lawrenson, K., Notaridou, M., Lee, N., et al. (2013). In vitro three-dimensional modeling of fallopian tube secretory epithelial cells. BMC Cell Biology, 14, 43.
Kessler, M., Hoffmann, K., Fritsche, K., et al. (2019). Chronic Chlamydia infection in human organoids increases stemness and promotes age-dependent CpG methylation. Nature Communications, 10, 1194.
Yu-Hsun, C., Tang-Yuan, C., & Dah-Ching, D. (2020). Human fallopian tube epithelial cells exhibit stemness features, self-renewal capacity, and Wnt-related organoid formation. Journal of Biomedical Science, 27, 32.
Turco, M. Y., Gardner, L., Kay, R. G., et al. (2018). Trophoblast organoids as a model for maternal-fetal interactions during human placentation. Nature, 564, 263–267.
Li, Z., Kurosawa, O., & Iwata, H. (2018). Development of trophoblast cystic structures from human induced pluripotent stem cells in limited-area cell culture. Biochemical and Biophysical Research Communications, 505, 671–676.
Dajung, J., Xiong, J., Min, Y., et al. (2017). In vitro differentiation of human embryonic stem cells into ovarian follicle-like cells. Nature Communications, 8, 15680.
Lawrenson, K., Benjamin, E., Turmaine, M., Jacobs, I., Gayther, S., & Dafou, D. (2009). In vitro three-dimensional modelling of human ovarian surface epithelial cells. Cell Proliferation, 42, 385–393.
Ohtake, H., Katabuchi, H., Matsuura, K., et al. (1999). A novel in vitro experimental model for ovarian endometriosis: The three-dimensional culture of human ovarian surface epithelial cells in collagen gels. Fertility and Sterility, 71, 50–55.
Girda, E., Huang, E. C., Leiserowitz, G. S., et al. (2017). The use of endometrial cancer patient-derived organoid culture for drug sensitivity testing is feasible. The International Journal of Gynecological Cancer, 27, 1701–1707.
Shuang, Z., Igor, D., Tao, Z., et al. (2019). Both fallopian tube and ovarian surface epithelium are cells-of-origin for high-grade serous ovarian carcinoma. Nature Communications, 10, 5367.
Paik, D. Y., Janzen, D. M., Schafenacker, A. M., et al. (2012). Stem-like epithelial cells are concentrated in the distal end of the fallopian tube: A site for injury and serous cancer initiation. Stem Cells, 30, 2487–2497.
Abbas, Y., Oefner, C. M., Polacheck, W. J., et al. (2017). A microfluidics assay to study invasion of human placental trophoblast cells. The Journal of the Royal Society Interface, 14, 20170131.
Ma, L., Li, G., Cao, G., et al. (2017). dNK cells facilitate the interaction between trophoblastic and endothelial cells via VEGF-C and HGF. Immunology and Cell Biology, 95, 695–704.
McConkey, C. A., Delorme-Axford, E., Nickerson, C. A., et al. (2016). A three-dimensional culture system recapitulates placental syncytiotrophoblast development and microbial resistance. Science Advances, 2, e1501462.
Kotomi, S., Yasuhisa, M., Michiya, S., et al. (2018). Aggregation of human trophoblast cells into three-dimensional culture system enhances anti-inflammatory characteristics through cytoskeleton regulation. The International Journal of Molecular Sciences, 19, 2322.
Wong, M. K., Shawky, S. A., Aryasomayajula, A., et al. (2018). Extracellular matrix surface regulates self-assembly of three-dimensional placental trophoblast spheroids. PLoS One, 13, e199632.
Kalkunte, S., Huang, Z., Lippe, E., et al. (2017). Polychlorinated biphenyls target Notch/Dll and VEGF R2 in the mouse placenta and human trophoblast cell lines for their anti-angiogenic effects. Scientific Reports, 7, 39885.
Nhan, P., Hong, J. J., Tofig, B., et al. (2019). A simple high-throughput approach identifies actionable drug sensitivities in patient-derived tumor organoids. Communications Biology, 2, 78.
Jabs, J., Zickgraf, F. M., Park, J., et al. (2017). Screening drug effects in patient-derived cancer cells links organoid responses to genome alterations. Molecular Systems Biology, 13, 955.
Moore, C. A., Shah, N. N., Smith, C. P., et al. (1842). 3D bioprinting and stem cells. Methods in Molecular Biology, 2018, 93–103.
Zhang, Y. S., Arneri, A., Bersini, S., et al. (2016). Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials, 110, 45–59.
Han, F., Utkan, D., & Pu, C. (2019). Emerging organoid models: leaping forward in cancer research. Journal of Hematology & Oncology, 12, 142.
Mittal, R., Woo, F. W., Castro, C. S., et al. (2019). Organ-on-chip models: Implications in drug discovery and clinical applications. Journal of Cellular Physiology, 234, 8352–8380.
Acknowledgements
No funding or financial support has been received.
No manuscript preparation assistance was provided or paid for.
All persons who contributed to the work reported in the manuscript are included as authors.
The contents of this manuscript have never been presented at a meeting.
No earlier version of this manuscript has been published on a preprint server.
All tables and figures are original, and no material has been adapted or modified from another source.
Disclaimer
The ideas and opinions expressed herein are those of the authors. The views expressed in the review are those of the authors and do not necessarily reflect the official policy or position of the Department of Maternal and Child Health of the National Health and Family Planning Commission of the People’s Republic of China.
Contributors
All authors contributed to the conception and design of this review. Cui drafted the first version of the article, and Zhao, Wu, and Li revised it critically for important intellectual content. Final approval of the version to be published was given by all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest Disclosures
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cui, Y., Zhao, H., Wu, S. et al. Human Female Reproductive System Organoids: Applications in Developmental Biology, Disease Modelling, and Drug Discovery. Stem Cell Rev and Rep 16, 1173–1184 (2020). https://doi.org/10.1007/s12015-020-10039-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-020-10039-0