Abstract
Objective
We aimed to investigate the effects of bone marrow derived mesenchymal stem cells (MSCs), minocycline, and these two therapies combined on functional and histological improvement in cerebral ischemic injury created rats.
Materials and methods
Twenty-eight Sprague Dawley female rats, weighing 250–300 g, were included in the study. Two male rats with similar properties were sacrificed for bone marrow derived MSC production. Group 1 was established as the control group. Group 2 was the group of only minocycline administered rats. Group 3 was the one of only MSCs administered rats. Group 4 was composed of the rats given the combination of MSCs and minocycline. Hematoxylin and eosin staining was done to assess the degeneration of the cells. Immunohistochemical staining was performed to evaluate the regeneration. Motor functions were examined by using Bederson’s score.
Results
Cell degeneration was the least in group 4. The cells stained with GFAP were observed mostly in group 4. The cells stained with Neu N in group 1 were statistically lower than in other groups. When the groups were ordered in terms of functional improvement at the end of the second week, group 4 had the most and group 1 had the least.
Conclusions
Bone marrow derived MSCs can lead to more histological and functional improvement when administered with minocycline, which is a neuroprotective agent as early as 24 h following the ischemic injury in a rat model. Minocycline therapy alone can be as effective as bone marrow derived MSCs therapy alone in ischemic cerebral rat model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic stroke is still a major health problem leading to high mortality and severe morbidity. Although intensive studies have been done in the area of stroke biology, few options are available that might be effective in the treatment of the disease. In clinical studies, most of neuroprotective strategies have failed to succeed because of insufficient effect or unexpected adverse side effects. Currently, clinical study models are aimed at understanding the process leading to brain damage and the way to determine the targets mediating to stroke [1]. Because of its complex pathology with damage including the neurons, glia, and endothelial brain cells, conventional treatment strategies target the first few hours immediately following the stroke to minimize the injury induced by the stroke. With its potential to repair the injured brain, cell transplantation may appear as a new treatment approach and might widen the therapeutic window for intervention, potentially leading to benefit from the treatment of more stroke patients [2]. Stem cells of different origins such as embryonic stem cells, fetal neural stem cells, human umblical cord derivated, and bone marrow derivated stem cells have all been tested in variable experimental stroke models and have been shown to increase the functional improvement [3–5]. Mesenchymal stem cells are multipotent cells that have the ability to renew themselves and to transform into the precusrors of bone, cartilage, and adipose tissue. They show immunomodulator properties, limit the local inflammatory response by decreasing the activations of microglia and macrophages, and impair the maturation of T lymphocytes [6]. Mesenchymal stem cells (MSCs) appear as potential treatment agents in stroke since they are easily obtainable from bone marrow and are rapidly ex vivo expandable for autologous transplantation. Because MSCs are allogenic and non-immunogenic, the risk of rejection dissappears [7]. To expand the therapautic effects of intravascular cell treatment, variable interventions have been performed. As an example, intravenous administration of MSCs structured to produce brain derived neurotrophic factor (BDNF) [8] or glial cell line derived factor(GDNF) [9] was preventive against cerebral ischemic damage in an adult rat model. It was reported that combination therapy of MSCs with nitric oxide donors or with erythropoietin was superior to the therapy of MSCs alone in rats with middle cerebral artery (MCA) occlusion [10].
Minocycline, which is a tetracycline derivative, draws great attention as a modifier of acute and chronic inflammation [11]. It was reported that minocycline decreased the infarct size after focal cerebral ischemia by attenuating microglial activation and by preventing the secondary damage originated from the neuroinflammation induced by stroke. Rueger et al. found that minocycline had a positive effect on survival of endogenous neural stem cells by attenuating the microglial activation, as mentioned before. These findings are promising for the development of new choices in stroke treatment[12]. In the light of all this information, we aimed to investigate the effects of bone marrow derived MSCs, minocycline, and combined therapy of these two on functional and histological improvement in cerebral ischemic injury created rats.
Material and Methods
Animal Model
Twenty-eight Sprague Dawley female rats, weighing 250–300 g, were included in the study. Two male rats with similar properties were sacrified for bone marrow derived mesenchymal stem cell production. The study was approved by the Ethical Committee for Animal Studies of Ankara Numune Education and Research Hospital.
Each of the four groups was composed of seven female rats. Group 1 was set as the control group. Group 2 was the group of minocycline only administered rats. Group 3 was the one of MSCs only administered rats. Group 4 was composed of the rats given the combination of MSCs and minocycline.
All the rats were anesthetized with ketamine. To induce permanent cerebral ischemic injury, the right carotis communis artery of each rat was tied at both ends and cut in the middle.
Twenty-four and 48 h after the surgical procedure, intraperitoneally phosphate buffer solution only was administered to the control group.
Rats in group 2 were given only minocycline (Sigma), intraperitoneally, dissolved in 0.1 mol/L of phosphate buffer with a pH of 7.4 for 1 week, with a dosage of 50 mg/kg for the first week and 25 mg/kg for the second week. The first dose was given 24 h after the surgical procedure.
Group 3 was given 1 × 106 of bone marrow derived MSCs of male rat intraperitoneally after 24 h of the procedure.
For group 4, the combination therapy group, 1 × 106 of MSCs and minocycline (Sigma) dissolved in 0.1 mol/L of phosphate buffer with a pH of 7.4 for 1 week with the dosage of 50 mg/kg was given intraperitoneally. MSCs were administered only once, but minocycline with the dosage of 50 mg/kg was injected through the first week and minocycline with a dosage of 25 mg/kg was injected through the second week.
Neurological motor functions were examined in the 24th hour, at the end of the first week, and at the end of the second week according to Bederson’s method [13].
All the rats were sacrificed at the end of the second week.
Method of Mesenchymal Stem Cell Production
Bone marrow was drawn from the femur and tibia bones of the male Sprague Dawley rats and mononuclear cells were separated by the density gradient method [14] . Mononuclear cells collected from the interphase were identified with flow cytometry [FACSCalibur TM (Becton, Dickinson, and Company, Vancouver, Canada)] using the hematopoietic and mesenchymal stem cell determinants [CD11b/c (+), CD45 (+), CD90 (-), CD44 (-) (BD Pharmingen, San Diego)]. Identified cells were incubated in the MSC medium and were propagated with subcultures after colony forming unit fibroblasts (CFU-F) became visible. Some of the MSCs produced were suspended and were identified once more with flow cytometry using bone marrow derived hematopoietic and mesenchymal stem cell surface determinants [CD11b/c (-), CD45 (-), CD90 (+),, CD44 (+)].
Histopathological Examination Method
After the brains of all the rats were removed and thin slices taken and fixated with formalin of 10 %, they were sampled for routine tissue follow-up. Then they were stained with hematoxylin and eosin (H&E). H&E staining was done to assess the degeneration of the cells. The stained specimens were evaluated. The scoring of the evalaution was done as follows:
-
1
point: normal view
-
2
points: presence of few degenerated neurons among normal neurons.
-
3
points: presence of multiple degenerated neurons among the scattered normal neurons.
-
4
points: presence of complete degeneration without normal neurons.
Scoring was done for hypocampal specimens.
Immunohistochemical staining was performed on the slices prepared from the paraffin blocks by peroxidase-antiperoxidase (PAP) procedure, using 3,3′ diaminobenzidine (DAB) chromogen. Rat brain tissue was used as a positive control for glial fibriler acidic protein (GFAP) and Neuro N (Neu N) antibodies. Immunohistochemically stained slices were evaluated by one pathologist only using a light microscope. The positivity for Neu N staining was determined as the number of staining cells under the biggest magnification of the microscope on hypocampal slices. The GFAP staining positivity assessment was done according to the diffusivity and severity of the staining on hypocampal slices.
Statistical Analysis
Statistical analysis was performed by using the SPSS 16.0 statistical package program. P value less than 0.05 was considered statistically significant. ANOVA was used for the variables in between groups 1, 2, 3 and 4. Also, chi-square was used for the appropriate variables between the groups. Continuous variables were expressed as mean ± standard deviation.
Results
There was a statistical significance between the groups in terms of H&E staining (p < 0.0001). One hundred percent of the cells in group 1 were stained 4 positively, 57 % of the cells in group 2 were stained 2 positively, and 42.9 % of the group 2 cells were stained 3 positively. None of the cells in group 2 were stained 4 positively. In group 3, 37.5 % of the cells were stained 2 positively and 62.5 % of them were stained 3 positively. One hundered percent of the cells in group 4 were stained 2 positively. Figure 1 shows the degenerated cells stained with H&E.
According to the results above, staining with H&E was statistically lower in group 4 than in group 1 and the other groups. This was meaningful as it marked the least degeneration in group 4. Also, these results showed that degeneration was less in group 2 than in group 3 and group 1, and less in group 3 than in group 1 (see Table 1).
In terms of staining positive with GFAP, there was statistical difference between the groups (p < 0.0001). All the cells (100 %) in group 1 were stained as 1 positive, all the cells (100 %) in groups 2 and 3 were stained as 2 positive, and all (100 %) in group 4 were stained as 3 positive. (Table 2)
Positive staining with GFAP was most in group 4 and least in group 1. The staining was equal in groups 2 and 3 (see Table 2). This means that the cells showing the properties of being astrocytes were found the most in group 4 and were found the least in group 1 (Fig. 2a, b, c, d).
When we assessed for staining with Neu N, the mean number of the cells was 54.9 ± 14.5 in group 1, 235 ± 16.3 in group 2, 239.3 ±36.5 in group 3, and 264.6 ± 89.8 in group 4. When compared with the other groups, the number of positive staining cells in group 1 was statistically lower (p < 0.0001). No statistical difference was present in groups 2, 3, and 4. Group 4 had the highest value according to mean values. Although there was no statistical significance, the cells showing the properties of being neurocyte were found most in group 4 (Fig. 3a, b, c, d).
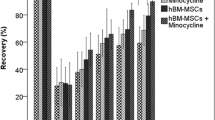
Whenever the groups were compared according to Bederson’s scores from the first day, no difference was found (p > 0.05). Bederson’s scores for the rats in groups 1, 2, and 3 were 2 in the first day of the surgical procedure, and 2 of 85.7 % of the rats and 1 of 14.3 % of the rats in group 4 (Table 3).
There was statistical difference between the groups (p < 0.001) in terms of Bederson’s scores for the first and second weeks.
Table 4 shows the Bederson’s score ratios of the groups at the end of the first week.
Of the rats in group 4, 71.4 % improved completely and 28.6 % improved partially at the end of the first week in terms of motor functions. When the groups were ordered according to the motor functionally improvement, the most improved was group 4, followed by group 2, group 3, and group 1.
The Bederson’s score ratios of the groups at the end of the second week are shown in Table 5. All of the rats in group 4 improved completely at the end of the second week in terms of motor functionally. Again, in terms of motor improvement, group 4 was most improved, followed by group 2, group 3, and group 1.
In Table 6, the comparison of the mean Bederson’s scores in first day, first week, and second week are shown. There was statistical difference between the groups in respect to mean Bederson’s scores in the first day, first week, and second week (p < 0.05). The control group showed statistical functional improvement, although not as much as the other groups.
The functional improvement of the groups was compared to histopathological characters (Table 7). The Bederson’s scores rose parallel to the increase in H&E staining, which was statistically significant (p < 0.04) and showed that the functional improvement was lower in the groups in which cell degeneration was higher.
The correlation between GFAP and Neu N staining positivity and mean Bederson’s scores was statistically significant at the end of the second week (p = 0.007, p = 0.008 respectively).
The GFAP and Neu N staining increased, while the mean Bederson’s scores decreased.
Discussion
The assumption that the cells of the central nervous system never regenerate began to change in the last decade when new stem cells were shown migrating to the brain in many rodent injury models, as well as new neuron findings in the adult hypocampus [15]. Potential positive effects of stem cell grafts in animal models and stroke clinical studies were made evident in various trials. It was determined that stem cells administered intravenously homed to the infarcted site and led to functional improvement in rats with chronic stroke [6]. Bone marrow derived MSCs have very good potential in stroke therapy since they are easily obtainable from the bone marrow and can be expanded quickly as ex vivo for autologous transplantation. MSCs are allogenic and non-immunogenic and therefore do not have the risk of being rejected [7].
We also evaluated the effects of bone marrow derived MSCs and minocycline whose neuroprotective property is known on functionally and histopathologically improvement by administrating intraperitoneally to the rats in whom secondary stroke was induced by producing cerebral ischemic insult. The neuroprotective effects of minocycline have been reported in neurological disorders like Parkinson’s disease, amyotrophic lateral sclerosis, spinal cord injury and cerebral ischemia[16, 17]. In our study, bone marrow derived MSCs, minocycline, and a combination of the two were injected intraperitoneally according to their groups after 24 h and at the end of the first week. Jin et al. suggested that the cells administered in various ways (e.g. intrastriatal, intraventricular, and intravenously) could arrive at the ischemic brain regions in middle cerebral artery occluded rats [18]. However, since there is no concept regarding an efficient way of cell transplantation, we chose the intraperitoneal method to inject the cells and the minocycline and phospate buffer solution.
According to our results, the best functional and histological improvement were observed with the combination therapy(MSCs and minocycline together). When the rats in this group were examined at the end of the second week, it was seen that all Bederson’s scores were zero, pointing to complete functional improvement. Ischemic injury observed histopathologically was also less in this group and the positive staining with Neu N and GFAP, which are markers to show the transformation of stem cells to the neurocytes and glial cells [19] respectively, were more appropriate in this group. These results were significant to show that the combined administration of MSCs and minocycline in the first day of ischemic cerebral insult was more effective. A study by Rueger et al. reported that in stroke induced rats minocycline, in specific concentrations, increased the numbers of stem cells significantly without increasing their proliferation, which was meaningful to show its positive effect on neural stem cell survival. Similar to the in vitro findings, they reported that minocycline caused a specific increase in neural stem cell activity, both in the subventricular zone and the hypocampus, as in the in vivo [12]. To our knowledge, our study is the first in the literature in which the bone marrow derived MSCs and minocyline were administered to the rats in whom ischemic stroke was induced by ligation and then cutting the carotid communis artery. One of the most interesting findings of our study was that the functional improvement was prominent, secondly, in the group in which only minocycline was injected. Whenever results of our study were evaluated in respect to new neurons occurring, it was seen that the numbers of Neu N expressing cells were similar in all three treatment groups, whereas GFAP expression was more prominent in the combined therapy group followed by treatment alone groups. These results were worthwhile in expressing that minocycline treatment alone was as efficacious as MSCs treatment alone in the ischemic stroke model if initiated in the first days of the event. Therefore, as Liu et al. showed, in addition to neuroprotective effect in the acute phase of cerebral ischemia, chronic treatment with minocycline also protected the new neurons induced by stroke thereafter and improved the neurological function [20]. Tang et al. reported that minocycline decreased the infarct volume and improved the sensorimotor function in the focal cerebral ischemia model they produced [21]. According to our study results, the most ideal method was combined treatment with MSCs and minocycline. Since MSCs and minocycline were administered within 24 h after the ischemia we induced, we thought that the lower damage and increased improvement were the positive results of early treatment. In a study done by Omori et al., administration of MSCs led to functional improvement and decreased the large infarct volume in the rat model of middle cerebral artery occlusion. It was reported that this improvement was greater when the MSCs were given just after the ischemia in high dosage as compared to lower dosage and time spanned treatment [22]. There are some points to be criticized in our study, including that we did not have a treatment group in which the MSCs and minocycline were initially administered not within 24 h but in the weeks following the induced ischemia. Therefore, the following conclusion can be reported: The MSCs obtained from human donors are in a very low amount, and almost one cell of 105 nuclear cells is MSC. Since they are found in very small amounts in bone marrow, only MSCs expanded in cultures can meet the need in clinical application [23]. Although some studies display partial effectiveness of MSCs in chronic stroke treatment [6], treating patients with ischemic cerebral damage with autologous MSCs in early phase seems more effective, but, as reported above, since MSCs are present in low quantities in bone marrow it is impossible to treat the patients with MSCs in the early phase. Thus, human simulation of our study seems difficult. However, we want to speculate that stem cell banks created from healthy individuals can be significant in terms of obtaining ready autologous MSCs in case of need.
Based on our results, we hypothesize that in the presence of ischemic cerebral injury, initiating the treatment with minocycline, which has the characteristics of antiapopitosis, antiinflammation, and neuroprotectivity and has the availability to be reached in early phase and subsequently adding the autologous MSCs expanded in culture will be useful in human ischemic stroke trials.
As conclusions: bone marrow derived MSCs can lead to more histological and functional improvement when administered with minocycline, which is a neuroprotective agent, as early as 24 h following ischemic injury in a rat model.
On the other hand; minocycline therapy alone can be as effective as bone marrow derived MSCs therapy alone in ischemic cerebral rat models. However, further and larger studies are needed in this field.
References
Jablonska, A., & Lukomska, B. (2011). Stroke induced brain changes:implications for stem cell transplantation. Acta Neurobiologiae Experimentalis, 71, 74–85.
Horie, N., Pereira, M. P., Niizuma, K., et al. (2011). Transplanted stem cell-secreted vascular endothelial growth factor effects poststroke recovery, inflammation, and vascular repair. Stem Cells, 29, 274–285.
Vora, N., Jovin, T., & Kondziolka, D. (2006). Cell transplantation for ischemic stroke. Neurodegenerative Diseases, 3(1-2), 101–105.
Bacigaluppi, M., Pluchino, S., Martino, G., et al. (2008). Neural stem/precursor cells for the treatment of ischemic stroke. Journal of Neurological Sciences, 265(1-2), 73–77.
Guzman, R., Choi, R., Gera, A., Los Angeles, A. De, et al. (2008). Intravascular cell replacement therapy for stroke. Neurosurgical Focus, 24(3–4), E15.
Bhasin, M. V. A., Srivastava, P., Kumaran, S. S., et al. (2011). Autologous mesenchymal stem cells in chronic stroke. Cerebrovascular Diseases Extra, 1, 93–104.
Dharmasaroja, P. (2009). Bone marrow-derived mesenchymal stem cells for the treatment of ischemic stroke. Journal of Clinical Neuroscience, 16, 12–20.
Nomura, T., Honmou, O., Harada, K., et al. (2005). I.V. infusion of brain-derived neurotrophic factor gene-modified human mesenchymal stem cells protects against injury in a cerebral ischemia model in adult rat. Neuroscience, 136(1), 161–169.
Horita, Y., Honmou, O., Harada, K., et al. (2006). Intravenous administration of glial cell line-derived neurotrophic factor gene-modified human mesenchymal stem cells protects against injury in a cerebral ischemia model in the adult rat. Journal of Neuroscience Research, 84(7), 1495–1504.
Hicks, A., & Jolkkonen, J. (2009). Challenges and possibilities of intravascular cell therapy in stroke. Acta Neurobiologiae Experimentalis, 69, 1–10.
Fox, C., Dingman, A., Derugin, N., et al. (2005). Minocycline confers early but transient protection in the immature brain following focal cerebral ischemia-reperfusion. Journal of Cerebral Blood Flow and Metabolism, 25(9), 1138–1149.
Rueger, M. A., Muesken, S., Walberer, M., et al. (2012). Effects of minocycline on endogenous neural stem cells after experimental stroke. Neuroscience, 26(215), 174–183.
Bederson, J. B., Pitts, L. H., Tsuji, M., et al. (1986). Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination. Stroke, 17, 472–476.
Ma, L., Scheers, W., & Vandenberghe, P. (2004). A flow cytometric method for determination of absolute counts of myeloid precursor dendritic cells in peripheral blood. Journal of Immunological Methods, 285(2), 215–221.
Joyce, N., Annett, G., Wirthlin, L., et al. (2010). Mesenchymal stem cells for the treatment of neurodegenerative disease. Regenerative Medicine, 5(6), 933–946.
Tikka, T. M., & Koistinaho, J. E. (2001). Minocycline provides neuroprotection against N-methyl-D-aspartate neurotoxicity by inhibiting microglia. Journal of Immunology, 166, 7527–7533.
Tikka, T. M., Vartiainen, N. E., Goldsteins, G., et al. (2002). Minocycline prevents neurotoxicity induced by cerebrospinal fluid from patients with motor neurone disease. Brain, 125, 722–731.
Jin, K., Sun, Y., Xie, L., et al. (2005). Comparison of ischemia-directed migration of neural precursor cells after intrastriatal, intraventricular, or intravenous transplantation in the rat. Neurobiology of Disease, 18(2), 366–374.
Keum, S. B., & Joon, B. P. (2011). Neuron-like differentiation of bone marrow-derived mesenchymal stem cells. Yonsei Medical Journal, 52(3), 401–412.
Liu, Z., Fan, Y., Won, S. J., et al. (2007). Chronic treatment with minocycline preserves adult new neurons and reduces functional impairment after focal cerebral ischemia. Stroke, 38, 146–152.
Tang, X. N., Wang, Q., Koike, M. A., et al. (2007). Monitoring the protective effects of minocycline treatment with radiolabeled annexin V in an experimental model of focal cerebral ischemia. Journal of Nuclear Medicine, 48(11), 1822–1828.
Omori, Y., Honmou, O., Harada, K., et al. (2008). Optimization of a therapeutic protocol for intravenous injection of human mesenchymal stem cells after cerebral ischemia in adult rats. Brain Research, 1236, 30–38.
Ma, T. (2010). Mesenchymal stem cells: from bench to bedside. World Journal of Stem Cells, 2(2), 13–17.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ersin Fadillioglu and Tuncay Delibasi are supported by the Turkish Academy of Sciences.
The study was funded by The Ministry of Health of Turkey.
Rights and permissions
About this article
Cite this article
Bilen, S., Pinarli, F., Ak, F. et al. Treatment Efficacy with Bone Marrow Derived Mesenchymal Stem Cells and Minocycline in Rats After Cerebral Ischemic Injury. Stem Cell Rev and Rep 9, 219–225 (2013). https://doi.org/10.1007/s12015-012-9422-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-012-9422-3