Abstract
Many clinical trials have demonstrated the effectiveness of subthreshold phototherapy with no visible damage in retinal vascular diseases, such as diabetic retinopathy. We aimed primarily to investigate the effect of subthreshold diode micropulse laser (SDM) treatment on mouse retinal pigmented epithelium (RPE) cells. The expression of angiogenesis-modulating cytokines in response to SDM was also explored. The least toxic laser dose was selected by measuring cell viability with MTT assay and 5 % duty cycle (DC) was chosen for use in further experiments. RPE cells were treated with laser-induced radiation ranging from 0 to 400 mW for 24 h. The apoptotic rate of RPE cells was assessed by flow cytometry. Expressions of vascular endothelial growth factor A (VEGF-A), transforming growth factor beta (TGF-β), basic fibroblast growth factor (bFGF), and pigment epithelium-derived factor (PEDF) were determined by Western Blotting and real-time PCR, respectively. After 24 h of laser irradiation, cell viability was reduced dose dependently and the effect was significant compared to the controls (P < 0.05). In addition, laser treatment with intensities of 100 and 200 mW with DC of 5 % produced no significant effect on cell viability and apoptosis as compared with the control group (P > 0.05). The protein and mRNA expressions of angiogenic stimulators (VEGF-A, TGF-β, and bFGF) were significantly down-regulated (P < 0.05), whereas those of the angiogenic inhibitor (PEDF) were up-regulated (P < 0.05). No significant difference was found between the cells treated with different intensities of laser radiation (P > 0.05). Our results showed that SDM treatment of the RPE cells suppressed the expression of choroid neovasculization-promoting cytokines and up-regulated the angiogenic inhibitor, PEDF without damaging the cells. Further investigation is needed to understand the mechanism and to optimize the use of SDM as a novel method of treatment for retinal vascular diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the years, micropulse laser photocoagulation has become the first-line treatment for various retinal diseases, including diabetic macular edema, proliferative diabetic retinopathy (PDR), central serous chorioretinopathy (CSR), macular edema secondary to branch retinal vein occlusion (BRVO), and glaucoma. Therapeutic laser photocoagulation abolishes oxygen utilizing photoreceptor cells and pigment epithelium that leads to retinal hypoxia. However, the use of conventional suprathreshold laser photocoagulation is associated with many complications, including reduced visual acuity, visual field, color vision, night vision, and contrast sensitivity. In addition, risks of CNV, hemorrhage, epiretinal fibrosis, and serous detachment of the peripheral retina are increased with conventional laser treatment. These adverse effects limit the treatment density and repeatability near the foveal center, the location of the most visually disabling form of diabetic macular edema (DME). It has been understood that the retinal damage can be minimized by modification of the laser parameters, such as wavelength, spot size of retinal irradiance, and pulse duration [1–9]. As a result of continuous efforts over the years, the technique has evolved to a more advanced, effective, and safe therapy for retinal disorders.
The new method, subthreshold micropulse (SDM) uses pulses of controlled laser radiations of longer wavelengths (810 nm) that produces therapeutic effects with minimal damage to the healthy retina, therefore it is also called retina-sparing laser therapy [1, 9–11, 13, 14]. The micropulse of low intensity infrared 810 nm diode laser is selectively absorbed by the retinal pigmented epithelium (RPE) and therefore it does not cause retinal damage [6]. Whereas the targeted cells receiving massive laser dose are burnt and undergo necrosis, the adjacent cells receiving sub-lethal photo-thermal effect respond with modified biological activities representing reversal of pathological conditions. Therefore, the excessive iatrogenic chorioretinal damage caused by visible endpoint coagulation has been replaced with non-lethal photo-thermal elevations obtained with minimum intensity photocoagulation (MIP) without intraoperative visible endpoint [15]. Thus, the retina-sparing MIP treatment utilizing reduced exposure and a subvisible endpoint seems to offer promising healing of retina with minimum iatrogenic harm [15, 16].
The vital role of vasoactive cytokine, the vascular endothelial growth factor (VEGF) in iatrogenic retinal damage has been accepted for almost five decades. An altered production of VEGF is known to reduce the metabolic demand, debulk diseased retina, increase intraocular oxygen tension, and promote neovascularization [3, 17, 18]. The laser photocoagulation has been found to suppress neovascularisation, vascular thrombosis, sclerosis, or leukostasis and it affects the permeability of vascular capillaries to control the edema. A complete elucidation of the mechanisms can assist to further optimize the technique [15]. The use of anti-VEGF agents has also been found to prevent from vision loss in various age- and diabetes-associated retinal diseases. However, the importance of laser treatment in combating retinal pathologies remains to be pivotal in clinical practice [6, 10].
In order to understand the mechanism of SDM in treating retinal vascular disease, we aimed to investigate response of mouse RPE cells to 810 nm diode laser exposure, focusing on the characteristics of the cell defense system against CNV. We measured apoptosis of RPE cell and expression of the angiogenesis-stimulating cytokines [vascular endothelial growth factor A (VEGF-A), transforming growth factor beta (TGF-β) and basic fibroblast growth factor (bFGF)], and pigment epithelium-derived factor (PEDF) the inhibitor of angiogenesis.
Materials and Methods
Animals
Forty C57BL/6 mice were purchased from Wuhan University Center for Animal Experiment Laboratory, China). All procedures were in compliance with the Association for Research in Vision and Ophthalmology (ARVO) Statement for the use of Animals in Ophthalmic and Visual Research was approved by the Committee on the Ethics of Wuhan University Center for Animal Experiment, China (Permit Number: SCXK 2008-0004).
Reagents
Dulbecco’s Modified Eagle’s Medium/Nutrient Mixture F-12 (DMEM/F12) and fetal bovine serum (FBS) were purchased from Invitrogen-Gibco. Phosphate buffer, gelatin, sucrose, and trypsin were from Beyotime, China. Mouse monoclonal anti-cytokeratin antibodies, mouse monoclonal antibodies against VEGF-A, TGF-β, bFGF, PEDF, and β-actin were purchased from BOSTER (Wuhan, China).
RPE Primary Culture
Forty C57BL/6 mice aged 3–5 weeks were used in this study. RPE cells were cultivated using a method with slight modification described previously [19]. Briefly, eyes were enucleated and cut into halves along a circumferential line posterior to the ciliary process, creating a ciliary body-free posterior eyecup. The eyecup was incubated in 0.2 % trypsin for 1 h. The RPE cells were triturated to make a single-cell suspension and then resuspended in DMEM/F12, seeded in 6-well plates, and incubated for 2 weeks. DMEM/F12 complete medium supplemented with 20 % FBS, penicillin/streptomycin (1:100), and 4 mM l-glutamine was used for the primary RPE cultures. Immunostaining of cytokeratin staining confirmed the epithelial origin of the cells.
Laser Treatment of the RPE Cells
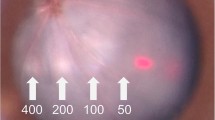
RPE cells cultivated in a culture dish (3 × 106 cells/well in a 6-well plate) with DMEM/F12 were treated with 810 nm diode laser radiation as a heat source. Both 5 % duty cycle (DC) and 10 % DC have been tested. Radiation intensity ranged from 0 to 400 mW with beam diameter of 75 μm, and 100 ms of exposure were applied to different groups.
The Micropulse mode consists of delivering the laser energy with a train of short pulses (100–300 μs) applied repetitively within an envelope of 0.1–0.5 s width which represents the exposure duration. The “ON” time constitutes the duration of each micropulse and the “OFF” time corresponding to the period between successive micropulses permits the heat to subside. The period T corresponds to the sum of “ON” and “OFF” times, whereas 1/T refers to the repetition rate in pulse per second (pps) also known as frequency f in hertz (Hz). DC expressed as % is the ratio between the “ON” time and the period T. The “isolation” or “additivity” of the thermal rise elicited by each single micropulse relies on the repletion rate and DC. Isolation of thermal rises is acquired by a relatively long “OFF” time and this means a relatively low repetition rate. The pulse-to-pulse thermal additivity is minimized by keeping the repetition rate below 500 ppc. As a result, the period T, the “OFF” time should not be less than 2, 1.7 ms respectively, whereas the DC should not exceed 15 % [20].
Cell Viability Assay
After the laser radiation treatment, cell viability was determined using a MTT kit following the instructions by the manufacturer (KeyGEN BioTECH, Nanjing, China). Briefly, the cells were collected and seeded in 96-well plate at a density of 2 × 105 cells/mL. Twenty-four hours later, the MTT reagent was added and the incubation was continued for 4 h. The medium was aspirated carefully from each well, and 150 µL of DMSO (Sigma, St. Louis, MO) was added to dissolve formazan, the end product and the absorbance was read at the wavelength of 568 nm using a plate reader. Cells treated with medium-only served to indicate 100 % cell viability, and the relative survival was defined as absorbance of treated wells divided by that of controls. All experiments were performed in triplicate.
Cell Apoptosis Assessed by Flow Cytometry
RPE cells incubated in serum free DMEM/F12 were treated with laser-induced radiation with intensity ranged from 0 to 400 mW, 5 % DC, with beam diameter of 75 μm and exposure duration of 100 ms. After 24 h of laser irradiation, the cell apoptosis was determined by the annexin V method using a commercial kit (KeyGEN BioTECH, Nanjing, China) according to manufacturer’s protocol. Briefly, after the treatment, the cells were collected using 0.25 % trypsin, and 106 RPE cells were stained with propidium iodide (PI) (5 mg/mL, analytical grade reagents, China) and annexin V (1 mg/mL, analytical grade reagents, China) for 30 min at 37 °C. The early (annexin V+/PI−) and late (annexin V+/PI+) apoptotic cells were sorted by fluorescence-activated cell sorting (FACS) (BD Biosciences FACS Calibur). All experiments were performed in triplicate.
Western Blot Analysis
Expressions of VEGF-A, TGF-β, bFGF, and PEDF were determined by Western Blotting after treating the cells for 24 h with 810 nm diode laser at 5 % DC. The cell lysate (30–50 μg) was electrophoretically separated in 10 % sodium dodecyl sulfate-polyacrylamide gel and thereafter transferred to PVDF membranes. After blocked in PBS containing 5 % bovine serum albumin (BSA), the membranes were incubated with primary antibodies against VEGF-A (1:100), TGF-β (1:500), bFGF (1:500), and PEDF (1:500) at 4 °C overnight, then incubated with their secondary antibodies. ECL detection reagents were used for blot detection and then densitometric comparison.
RT-PCR Analysis
After 24 h of laser irradiation (DC: 5 %), mRNA expressions of VEGF-A, TGF-β, bFGF, and PEDF were analyzed by RT-PCR. Total RNA was extract from cells using RNA simple Total RNA Kit (TIANGEN Co., Beijing, China) and 3 µg of RNA was converted into cDNA. Quantitative PCR (Q-PCR) was performed with the addition of SYBR Green I (Bio-Rad) intercalating dye, and data were collected using the iCycler (Bio-Rad). Fold changes in gene expression were calculated using the 2−ΔΔCt. Oligonucleotide primers for RT-PCR are listed in Table 1.
Statistical Analysis
Data were analyzed with SPSS 13.0 software. The results are expressed as mean ± standard deviation (SD). Statistical significance was determined using one-way ANOVA followed by a LSD-test. P < 0.05 was considered significant.
Results
Identification of RPE Cells
The black and circular primary RPE cells were plated and incubated in a humidified chamber at 37 °C. After 7 days, the adhered monolayer of the cells were subcultured, and in the third passage, the cells were identified and their epithelial origin was confirmed by cytokeratin immunohistochemistry (Fig. 1).
Laser-Induced Reduction in RPE Viability
We tried to determine RPE viability subjected to laser-induced radiation of different intensities at 5 and 10 % DC, respectively. As shown in Fig. 2, cell viability of 5 % DC group was significantly higher compared to 10 % DC group (P < 0.05). In 5 % DC group, 100 and 200 mW of laser radiation did not have any significant effect compared to the control (P > 0.05). Cell survival was significantly reduced in a power-dependent manner (P < 0.05) in both 5 % DC and 10 % DC group. Based on this result, the laser with 5 % DC was selected for the subsequent experiments.
Laser Application with Low DC and Power Did Not Induce Apoptosis in RPE Cells
The annexin V flow cytometry analysis was used to determine the apoptosis of RPE cells irradiated with 810 nm diode laser at 5 % DC. As shown in Fig. 3, at the power of 100 and 200 mW with 5 % DC, the laser-induced apoptosis was low (3.52 ± 0.36 and 3.55 ± 0.29 %, P > 0.05 respectively) and it was not different from that of the control Group (3.68 ± 0.27 %, P > 0.05). At the power of 300 and 400 mW, laser-induced apoptotic rate was increased in a power-dependent manner (9.31 ± 0.59 and 14.24 ± 0.45 %, respectively P < 0.05) and it was significantly higher than that of the control group (P < 0.05).
Angiogenic Stimulators were Down-Regulated and Inhibitor was Up-Regulated with Laser Treatment
As shown in Fig. 4, laser treatment induced a significant down-regulation of angiogenic stimulators (VEGF-A, TGF-β, and bFGF) (P < 0.05), and up-regulation of the inhibitor (PEDF) (P < 0.05). This response of the cells treated with different doses of laser was not significantly different (P > 0.05). Figure 5 shows that compared to the control group, laser treatment induced a significant (P < 0.05) decrease in the mRNA expression of for angiogenic stimulators (VEGF-A, TGF-β, and bFGF), whereas that of the inhibitor (PEDF) was significantly increased (P < 0.05). No significant difference was found between the groups treated with different intensities of laser (P > 0.05).
Discussion
Retinal laser photocoagulation is used to treat the proliferative retinopathy with a goal to shrink abnormal blood vessels formed during the process of neovascularization. The complications of photocoagulation treatment is determined by the manner, the laser energy is delivered and dissipated to bring about the thermal change. In general, the laser light is applied across the pupil, then after approximately 1 ms of starting the irradiation, heat generated is spread to the adjacent pigmented subretinal structures which were not directly targeted by the laser. The spread of released thermal energy causes a gradual decrease of the temperature to baseline body temperature [20]. In case of the conventional threshold photocoagulation, the appearance of grayish endpoint indicates that the thermal wave initiated in the RPE/choroid interface has arrived at the overlying neurosensory retina. This endpoint or laser lesion is a sign that the temperature is sufficiently high (20–30 °C above the baseline of 36 °C) to affect natural transparency leading to the scatter of the slit lamp illumination light. The overlying neural retina which is normally transparent to laser wavelength is damaged and loses its transparency causing scatter of the white ophthalmoscopic light back and therefore making the lesion visible. [20]. Whereas suprathreshold photocoagulation therapy is performed to a visible endpoint, the subthreshold therapy aims for a barely visible or subthreshold lesion [16]. The use of lower intensity or subthreshold laser aims to obtain the beneficial effect without damaging the retina. As reviewed by Dorin [15, 20], MicroPulse is a technique that allows a finely controlled laser emission delivered in the form of a train of repetitive short pulses (typically 100–300 μs in duration each) within an ‘‘envelope’’ whose width the exposure duration ranges 0.1–0.5 s. The period T is the sum of the ON and OFF times and the ratio between the ON time and the period T is the DC in percent. By principle, the short ON time of Micropulse limits the laser energy delivered and the consequent thermal elevation, whereas the long inter-pulse OFF time allows for thermal relaxation before the arrival of the next Micropulse. Thus, the key is to balance the proportion of ON time and OFF time, namely DC within specific power, and that limits the laser-induced heat rise and its spread to the adjacent tissues allowing effective therapy without a damage. In our study, when DC was set at 10 %, cell viability was found to decrease with increase in the power (Fig. 2a). However, irradiation with 810 nm diode laser at 5 % DC applied with powers of 100 and 200 mW did not affect the cell viability compared to the control group (P > 0.05). The rate of cell apoptosis was also not observed to be significantly different from that of the control Group (P > 0.05). Considering that cell harvesting with 0.25 % trypsin for annexin V flow cytometry analysis might have damaged the cells to a small extent, laser treatment (DC: 5 %, power: 100 and 200 mW) did not induce apoptosis of RPE cells. These results suggest that SDM photocoagulation therapy with beam diameter (75 μm), 100–200 mW intensity, exposure time of 100 ms, and DC at 5 % may produce effective therapeutic effect without a visible retinal damage. Choroidal neovascularization (CNV), a characteristic of age-related macular degeneration consists of abnormal growth of blood vessels that originate in choroid and grow through Bruch’s membrane into the subretinal space. The defective Bruch’s membrane is considered one of the causative factors for this condition and if left untreated, it may lead to vessel leak in retina and accounts for serious outcomes such as destruction of photoreceptors and rapid vision loss. Although the mechanism underlying the pathogenesis of CNV is not completely understood, RPE is considered to play a pivotal role in the genesis of this disorder [21]. Implication of cytokines produced by the RPE in the pathogenesis of retinal vascular disease such as DME has also been evidenced [22]. The highly specialized cells of RPE function as a blood−retinal barrier and allow selective transport of angiogenesis factors such as VEGF between choriocapillaries and neural retina [23, 24]. A dynamic balance between a pro-angiogenic (VEGF) and antiangiogenic (PEDF) factors has been evidenced to play a critical role in maintaining the normal physiological functions of retinal choroidal endothelial cells [21]. On the contrary, a disrupted balance due to oxidative conditions leading to decreased PEDF and increased VEGF is considered to promote a pathological condition that contributes to CNV [21, 25]. It has also been proposed that benefits of photocoagulation are derived from the cytokines released by the recovering RPE cells. The photodynamic therapy has been found to selectively damage the choroidal neovascular membranes; however, the effectiveness of treatment has been hindered by the rebound effect of triggering enhanced VEGF expression in RPE [26].
A key role of VEGF in promoting angiogenesis by increasing the permeability of capillary endothelium has been reported [17, 27–29]. However, the role of VEGF alone in angiogenesis has also been questioned as CNV and VEGF overexpression were not found to be correlated [30]. The involvement of other angiogenic factors such as TGF-β and bFGF in the development of CNV has also been suggested [31–33]. In addition to VEGF, bFGF has been identified as a mediator of retinal neovascular diseases such as diabetic retinopathy and the wet form of age-dependent macular degeneration [17]. Other studies showed an enhanced expression of TGF-α followed by increased VEGF expression in RPE cells suggesting the implication of both of these cytokines in age-related neovascular macular degeneration [34, 35]. The antiangiogenic factor PEDF has been found to antagonize the function of VEGF, that is, it stabilizes the endothelium of the choriocapillaries, inhibits cell proliferation, and suppresses the process of CNV [31–33]. A decrease in PEDF expression disrupting the critical balance between VEGF and PEDF has been suggested to permit the development of CNV in the eyes with AMD. As a consequence, the therapeutic use of PEDF analogs for the treatment of this disease has been proposed [36].
Low power laser irradiation (especially red and near-infrared wavelength) such as 810 nm diode has been found to mediate its beneficial effects by up- and down-regulation of biological activities of the sub-lethally injured RPE cells [20, 37]. Thus, laser photocoagulation-induced TGF-/5 production by the RPE cells has been shown to trigger regression of neovascularization and complications of laser treatment such as preretinal fibrosis. The photocoagulated RPE cells have also been evidenced to regress neovascularization through TGF-32 production [38]. The normalization of cell function and cytokine expression leading to reduced inflammation in response to SDM has been reported [12]. In our study, laser irradiation at 5 % DC for 24 h resulted in down-regulation of protein and RNA expressions of angiogenic stimulators (VEGF-A, TGF-β, and bFGF). The effect was significant (P < 0.05) compared to the controls. In contrast, the protein and RNA expressions of angiogenic inhibitor (PEDF) were significantly up-regulated (P < 0.05). These results suggest that micropulse laser treatment may regress CNV by modulating the balance of angiogenesis regulators.
Conclusion
Our results demonstrated that 810 nm diode laser at the power of 100 and 200 mW with 5 % DC can induce the expression of angiogenic inhibitor (PEDF) and reduce the expression of angiogenic stimulators (VEGF-A, TGF-β, and bFGF) without causing damage to RPE cells. The study suggests that by controlling the parameters of laser especially choosing the right DC and power, using invisible endpoint, SDM can be used for retinal vascular disease with maximum efficacy and minimum damage. Further studies to determine the in vivo effects SDM are required to find out adequate support for SDM in the treatment of retinal vascular disease.
References
Kiire, C., Sivaprasad, S., & Chong, V. (2011). Subthreshold micropulse laser therapy for retinal disorders. Retina Today, 1, 67–70.
Mainster, M. A. (1999). Decreasing retinal photocoagulation damage: Principles and techniques. Seminars in Ophthalmology, 14(4), 200–209.
Ferrara, N., Gerber, H. P., & LeCouter, J. (2003). The biology of VEGF and its receptors. Nature Medicine, 9, 669–676.
King, G. L., & Suzuma, K. (2000). Pigment-epithelium-derived factor—A key coordinator of retinal neuronal and vascular functions. New England Journal of Medicine, 342, 349–351.
The Diabetes Control and Complications Trial Research Group. (1993). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New England Journal of Medicine, 329, 977–986.
Shah, A. M., Bressler, N. M., & Jampol, L. M. (2011). Does laser still have a role in the management of retinal vascular and neovascular diseases? American Journal of Ophthalmology, 152, 332–339.
Schatz, H., Madeira, D., McDonald, H. R., & Johnson, R. N. (1991). Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Archives of Ophthalmology, 109, 1549–1551.
Early Treatment Diabetic Retinopathy Study Research Group. (1995). Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Archives of Ophthalmology, 113, 1144–1155.
Luttrull, J. K., Sramek, C., Palanker, D., Spink, C. J., & Musch, D. C. (2012). Long-term safety, high-resolution imaging, and tissue temperature modeling of subvisible diode micropulse photocoagulation for retinovascular macular edema. Retina, 32, 375–386.
Ohkoshi, K., & Yamaguchi, T. (2010). Subthreshold micropulse diode laser photocoagulation for diabetic macular edema in Japanese patients. American Journal of Ophthalmology, 149, 133–139.
Figueira, J., Khan, J., Nunes, S., Sivaprasad, S., Rosa, A., et al. (2009). Prospective randomised controlled trial comparing sub-threshold micropulse diode laser photocoagulation and conventional green laser for clinically significant diabetic macular oedema. British Journal of Ophthalmology, 93, 1341–1344.
Gao, X., & Xing, D. (2009). Molecular mechanisms of cell proliferation induced by low power laser irradiation. Journal of Biomedical Science, 16, 4.
Vujosevic, S., Bottega, E., Casciano, M., et al. (2010). Microperimetry and fundus autofluorescence in diabetic macular edema: subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina., 30(6), 908–916.
Laursen, M. L., Moeller, F., Sander, B., & Sjoelie, A. K. (2004). Subthreshold micropulse diode laser treatment in diabetic macular oedema. British Journal of Ophthalmology, 88, 1173–1179.
Dorin, G. (2004). Evolution of retinal laser therapy: minimum intensity photocoagulation (MIP). Can the laser heal the retina without harming it? Seminars in Ophthalmology, 19, 62–68.
Luttrull, J. K., Musch, D. C., & Mainster, M. A. (2005). Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular oedema. British Journal of Ophthalmology, 89, 74–80.
Meyer, C. H., & Holz, F. G. (2011). Preclinical aspects of anti-VEGF agents for the treatment of wet AMD: Ranibizumab and bevacizumab. Eye (London), 25, 661–672.
Schatz, H., Madeira, D., McDonald, H. R., & Johnson, R. N. (1991). Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Archives of Ophthalmology, 109, 1549–1551.
Akrami, H., Soheili, Z.-S., Khalooghi, K., Ahmadieh, H., Rezaie-Kanavi, M., Samiei, S., et al. (2009). Retinal pigment epithelium culture; a potential source of retinal stem cells. Journal of Ophthalmic & Vision Research, 4(3), 134–141.
Dorin, G. (2003). Subthreshold and micropulse diode laser photocoagulation. Seminars in Ophthalmology, 18, 147–153.
Ohno-Matsui, K., Morita, I., Tombran-Tink, J., Mrazek, D., Onodera, M., et al. (2001). Novel mechanism for age-related macular degeneration: An equilibrium shift between the angiogenesis factors VEGF and PEDF. Journal of Cellular Physiology, 189, 323–333.
Sohn, H. J., Han, D. H., Kim, I. T., Oh, I. K., Kim, K. H., et al. (2011). Changes in aqueous concentrations of various cytokines after intravitreal triamcinolone versus bevacizumab for diabetic macular edema. American Journal of Ophthalmology, 152, 686–694.
Hogan, M. J., Alvarado, J. A., & Weddell, J. E. (1971). The retinal pigment epithelium. In M. J. Hogan, J. A. Alvarado, & J. E. Weddell (Eds.), Histology of the human eye (pp. 405–423). Philadelphia: W.B. Saunders.
Marmor, M. F. (1998). Structure, function, and disease of the retinal pigment epithelium. In M. F. Marmor & T. J. Wolfenberger (Eds.), The retinal pigment epithelium (pp. 3–12). New York: Oxford Press.
Folkman, J. (1995). Angiogenesis in cancer, vascular, rheumatoid, and other diseases. Nature Medicine, 1, 27–31.
Tatar, O., Kaiserling, E., Adam, A., Gelisken, F., Shinoda, K., et al. (2006). Consequences of verteporfin photodynamic therapy on choroidal neovascular membranes. Archives of Ophthalmology, 124, 815–823.
Chapman, J. A., & Beckey, C. (2006). Pegaptanib: A novel approach to ocular neovascularization. Annals of Pharmacotherapy, 40, 1322–1326.
Frank, R. N., Amin, R. H., Eliott, D., Puklin, J. E., & Abrams, G. W. (1996). Basic fibroblast growth factor and vascular endothelial growth factor are present in epiretinal and choroidal neovascular membranes. American Journal of Ophthalmology, 122, 393–403.
Matsuda, S., Gomi, F., Oshima, Y., Tohyama, M., & Tano, Y. (2005). Vascular endothelial growth factor reduced and connective tissue growth factor induced by triamcinolone in ARPE19 cells under oxidative stress. Investigative Ophthalmology & Visual Science, 46, 1062–1068.
Okamoto, N., Tobe, T., Hackett, S. F., Ozaki, H., Vinores, M. A., LaRochelle, W., et al. (1997). Transgenic mice with increased expression of vascular endothelial growth factor in the retina. A new model of intraretinal and subretinal neovascularization. American Journal of Pathology, 151, 281–291.
Dawson, D. W., Volpert, O. V., Gillis, P., Crawford, S. E., Xu, H., et al. (1999). Pigment epithelium-derived factor: A potent inhibitor of angiogenesis. Science, 285, 245–248.
Ogata, N., Wada, M., Otsuji, T., Jo, N., Tombran-Tink, J., et al. (2002). Expression of pigment epithelium-derived factor in normal adult rat eye and experimental choroidal neovascularization. Investigative Ophthalmology & Visual Science, 43, 1168–1175.
Bhutto, I. A., McLeod, D. S., Hasegawa, T., Kim, S. Y., Merges, C., et al. (2006). Pigment epithelium-derived factor (PEDF) and vascular endothelial growth factor (VEGF) in aged human choroid and eyes with age-related macular degeneration. Experimental Eye Research, 82, 99–110.
Kliffen, M., Sharma, H. S., Mooy, C. M., Kerkvliet, S., & de Jong, P. T. (1997). Increased expression of angiogenic growth factors in age-related maculopathy. British Journal of Ophthalmology, 81, 154–162.
Pertovaara, L., Kaipainen, A., Mustonen, T., Orpana, A., Ferrara, N., Saksela, O., et al. (1994). Vascular endothelial growth factor is induced in response to transforming growth factor-beta in fibroblastic and epithelial cells. Journal of Biological Chemistry, 269, 6271–6274.
Renno, R. Z., Youssri, A. I., Michaud, N., Gragoudas, E. S., & Miller, J. W. (2002). Expression of pigment epithelium–derived factor in experimental choroidal neovascularisation. Investigative Ophthalmology & Visual Science, 43, 1574–1580.
Flaxel, C., Bradle, J., Acott, T., & Samples, J. R. (2007). Retinal pigment epithelium produces matrix metalloproteinases after laser treatment. Retina, 27, 629–634.
Matsumoto, Miho., Yoshimura, Nagahisa., & Honda, Yoshihito. (1994). Increased production of transforming growth factor-β2 from cultured human retinal pigment epithelial cells by photocoagulation. Investigative Ophthalmology & Visual Science, 35, 4245–4252.
Acknowledgments
This work was generously supported by grants from the National Natural Science Foundation of China (Nos. 61378084).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, Z., Song, Y., Chen, X. et al. Biological Modulation of Mouse RPE Cells in Response to Subthreshold Diode Micropulse Laser Treatment. Cell Biochem Biophys 73, 545–552 (2015). https://doi.org/10.1007/s12013-015-0675-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0675-8