Abstract
To produce proinflammatory master cytokine IL-1β in macrophages, two stimulation pathways are needed including TLRs-NF-κB axis and NLRPs/ASC-caspase-1 axis. Different signals including exogenous and endogenous trigger inflammatory response distinctly. Among them, the role of endogenous stimulators of inflammation is poorly understood. As a component of hemoglobin, free heme is released when hemolysis or extensive cell damage occur which results in inflammatory response. Here, we find that heme induces IL-1β secretion through activating NLRP3 inflammasome in macrophages. Heme activates NLRP3 through P2X receptors, especially the P2X7R and P2X4R. Most importantly, significantly enhancement of heme level and activation of NLRPs/ASC-caspase-1 axis were observed in mice kidney after unilateral ureteral obstruction which could be inhibited by enforced expression of heme oxygenase-1 (HO-1). Our study proves that heme is a potential danger activator of NLRP3 inflammasome that plays an essential role in IL-1β secretion during kidney inflammation and provides new insight into the mechanism of innate immune initiation. Further investigation will be beneficial to develop new molecular target and molecular diagnosis indicator in therapy of kidney inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kidney inflammation is the major pathologic process of chronic kidney disease (CKD) and acute kidney injury (AKI) which cause significant morbidity and mortality in the general population [1]. Kidney inflammation always involves the innate immune system which is accompanied by cytokine expression and immune cell infiltration [2]. The mechanisms of innate immunity initiation have been studied extensively during the last decades. Two stimulation patterns are supposed to trigger innate immunity and inflammation including pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) [3, 4]. PAMPs are usually implicated in exogenous infection, in which the pattern recognition receptors (Toll-like receptors, retinoic acid-induced gene-like receptors, NOD-like receptors) recognize exogenous pathogen resulting the engagement of nuclear factor-κB (NF-κB) [5], IFN regulatory factors, and mitogen-activated protein kinase signaling pathways and ultimately lead to the proinflammatory factor secretion. In contrast to PAMPs, DAMPs are generally associated with endogenous dangerous signaling which can also induce inflammation with or without pathogen infection and thereby contribute to organ damage and dysfunction [6].
Recent studies have demonstrated that nucleotide-binding oligomerization-like receptor family members (NLRs) play essential role in the recognition of endogenous dangerous molecules released from damaged and lytic cells [7]. As a component of inflammasome, NLRP3 is the best characterized member of NLRs, which recruits and activates caspase-1 via the adapter molecule ASC (apoptosis-associated speck-like protein containing caspase activation and recruitment domain) [8, 9]. Activated caspase-1 cleaves the 35-kD pro-IL-1β to the mature and secreted form of the 17-kD cytokine [10]. IL-1β participates in a robust inflammatory response. Although activation of inflammasome has been implicated in Kidney inflammation [11–13], the exact mechanism of inflammasome activation is unknown, especially the role of endogenous inducers in inflammasome activation during inflammation is poorly understood.
Free heme is generated by intra- and extra-vascular hemolysis or extensive cell damage [14, 15]. Cell-free hemoglobin can be oxidized when exposed to reactive oxygen species (ROS), and the heme group was released. Free heme is a dangerous molecule which can be recognized and degenerated by stress-responsive enzyme oxygenase-1 (HO-1) [16] which plays an essential role in host defense against heme. Free heme has been proved possess pro-inflammatory activities, such as leukocyte activation, migration and infiltration, adhesion molecules activation, and cytokines and acute phase proteins induction [17, 18]. Therefore, we speculate that heme is involved in activation of NLRPs/ASC-caspase-1 axis in Kidney inflammation.
Here, we prove that heme can be recognized by P2X receptors in macrophages, which results in NLRP3/ASC inflammasome and caspase-1 activation and the release of mature IL-1β. Moreover, significantly enhancement of heme level and activation of NLRPs/ASC-caspase-1 axis was observed in mice kidney after UUO, and overexpression of HO-1 dramatically inhibit the immune response that UUO induced. Therefore, we propose that heme acts as a critical danger and stress signal, which can activate the NLRP3 inflammasome, causing caspase-1-dependent processing and release of IL-1β.
Materials and Methods
Mice
C57Bl/6 mice were kept at a constant temperature (25 °C) with free access to chow and water in a room with a 12-h light/dark cycle. The experiments were approved by the Institutional Animal Welfare Committee. NLRP3−/− mice on a C57Bl/620 background, wild-type, and heterozygote littermates were bred and housed in a pathogen-free facility. Healthy 6–8-week-old male mice underwent left UUO or sham surgery as described previously [19]. Mice were anesthetized using intraperitoneal injection of a mixture of ketamine (125 mg/kg) and xylazine (12.5 mg/kg); recovered under a warming lamp; and received analgesia, standard food, and water for the duration of the experiment.
Cell Culture and Stimulation
Peritoneal macrophages were obtained 4 days after intraperitoneal instillation of 2 ml of thioglycollate 3 % by peritoneal washing with chilled RPMI. For stimulation, cells were seeded at 2 × 105/well in 96-well plates in RPMI. Non-adherent cells were removed by washing, and adherent cells were stimulated by heme in the absence of serum, and after the indicated periods, the supernatant was collected and frozen until cytokine determination [20]. Heme and its analogs PPIX were obtained from Porphyrin Products. For caspase-1 inhibition, macrophages were preincubated for 1 h at 37 °C with Ac-Tyr-Val-Ala-Asp-chloromethylketone (Ac-YVAD-CMK; 10 μM; Bachem).
Cytokine Measurements
The concentrations of cytokine were determined using ELISA. All the measurements were performed in duplicate following the manufacturer’s instructions (Peprotec and R&D).
Heme Measurement
Heme was measured in mice kidney as described [16]. Kidney lysate was centrifuged (for 3 min at 4 °C at 16,000 μg), proteins were precipitated (10 % trichloroacetic; vol/vol, for 1 h on ice) and centrifuged (for 3 min at 4 °C at 14,000 μg), and free heme was measured in the protein-free supernatant as described [16].
Tissue Preparation
Tissue preparation was performed as previous study [21]. After 2, 8, or 16 days of UUO, mice were killed and the kidneys were removed. Kidneys were flash frozen or prepared for histology using 10 % buffered formalin fixation. Flash frozen samples were stored in OCT compound at −80 °C. Tissue protein lysate was prepared by weighing frozen tissue and placing the samples in an appropriate amount of lysis buffer (10 mMTris [pH 7.5], 1 % NP-40, and 150 mM NaCl) complete with protease inhibitors. Tissue homogenization was achieved with a handheld homogenizer (Kimble Kontes). Protein concentrations were determined using the Bradford protein assay.
P2X4R and NLRC4 Gene Silencing
P2X7R short hairpin RNA (shRNA) plasmid (sc42572SH), P2X4R shRNA plasmid (sc42570SH), negative controls (control shRNA plasmid B which encodes a scrambled shRNA sequence (sc108065), and control shRNA plasmid C which is an alternate negative scrambled shRNA sequence control (sc108066)), transfection medium, and reagents were obtained from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA), and the protocol for transfection was followed by the manufacturer’s recommendation. For silencing NLRC4 gene expression by small interfering RNA (siRNA), the siGENOME SMARTpool (M-055000-01, Dharmacon/Thermo Fisher Scientific) was used. siGENOME non-targeting siRNA 2 (D-001210-02-05; Dharmacon/Thermo Fisher Scientific) served as a negative control. Cells were transfected using the X-tremeGENE siRNA transfection reagent (Roche Applied Science), following instructions of the manufacturer. NLRC4 gene expression was verified by Quantitative TaqMan PCRs.
Recombinant Adenoviruses
The LacZ Rec.Ad and HO-1 Rec.Ad were constructed as previously described [22]. Mice were transduced with Rec.Ad. (i.p.; 3 × 108 pfu/mouse) 40 h before challenge with Pcc. Protein extraction and immunoblotting were performed as described previously [23].
Western Blotting Analysis
Elicited peritoneal macrophages were plated in 6-well plates at a density of 2.5 × 106 cells/well, non-adherent cells were removed by washing with medium, and adherent cells were stimulated with LPS or heme, as indicated in the figure legend. After 1 h, cells were lysed in a buffer consisting of Tris–HCl (50 mM), NaCl (150 mM), Nonidet P-40 1 %, sodium deoxycholate 0.25 %, EDTA (1 mM), aprotinin (5 μg/ml), leupeptin (5 μg/ml), pepstatin (5 μg/ml), phenylmethylsulfonyl fluoride (1 mM), sodium orthovanadate (1 mM), and NaF (1 mM); pH 7.5. Cell lysates were centrifuged, and the supernatants were boiled and subjected to electrophoresis in SDS–polyacrylamide gel (12 %) in reducing conditions. The proteins were transferred to a nitrocellulose membrane at 4 °C for 2 h. After this, the membranes were blocked with Tris-buffered saline solution with 0.05 % of Tween 20 (TBS-T) and 5 % of fat-free milk. The membranes were incubated for 2 h with primary antibody with appropriate dilution, diluted in blocking solution, washed in TBST. Then, membranes were incubated for 1 h with secondary antibody with appropriate dilution, and the bands were revealed by chemiluminescence using the ECL substrate.
Statistical Analysis
All data are presented as the mean value ± standard deviation (SD) of each group. Statistical differences between group means were evaluated using the Student’s t test, and P ≤ 0.05 was accepted as statistically significant.
Results
Heme Induces Maturation and Secretion of IL-1β in Macrophages
To investigate the effects of heme on macrophages, heme and heme analogs (PPIX) were take advantage to stimulate mouse peritoneal macrophages in a time- (up to 20 h) and dose-dependent (up to 40 μM) manner. The mature IL-1β was detected by ELISA and Western blotting. ELISA analysis displayed that the concentration of IL-1β in culture supernatants was significantly enhanced after stimulated by heme and PPIX. The effect of heme on IL-1β production initiated as early as 4 h after stimulation and displayed strict time- and dose-dependent manner (Fig. 1a–d). Western blotting further verified that matured IL-1β (17 kD) was presented in culture supernatant (Fig. 1e, f). These results demonstrate that heme could efficiently induce maturation and secretion of IL-1β in macrophages and primarily suggested that heme participates in immune response.
Heme induces IL-1β secretion by mouse macrophages. a Mouse peritoneal macrophages were stimulated with heme (0–40 μM) for 4 h with or without 10 % fetal calf serum (FCS), and IL-1β release was evaluated by ELISA. b Peritoneal macrophages were stimulated with the indicated concentrations of heme (30 μM) for 0–20 h, and IL-1β release was determined by ELISA. c Peritoneal macrophages were stimulated with PPIX (0–40 μM) for 4 h with or without 10 % fetal calf serum (FCS), and IL-1β release was evaluated by ELISA. d Peritoneal macrophages were stimulated with the indicated concentrations of heme (10 μM) for 0–20 h. Results represent mean ± S.E. for IL-1β determinations of stimuli performed in duplicates and are representative of three different experiments. e Mouse peritoneal macrophages were stimulated with heme (0–40 μM) for 4 h, and IL-1β release was evaluated by western blotting. f Peritoneal macrophages were stimulated with the indicated concentrations of heme (10 μM) for 0–20 h, and IL-1β release was determined by western blotting
Heme Activates NLRP3/ASC-Caspase-1 Axis for IL-1β Secretion
Since the activated caspase-1 is responsible for cleavage of IL-1β into mature 17-kDa, we asked whether stimulation of macrophages with heme could activate caspase-1 [24]. Western blotting results showed that the p10 active form of caspase-1 was detected in macrophages incubated with heme for 12 h. To further elucidate heme induces IL-1β via activating caspase-1, the inhibitor Ac-YVAD-CMK was used to block the activity of caspase-1. The results showed that mature IL-1β was significantly down-regulated in macrophages after incubating with heme plus Ac-YVAD-CMK. These results suggest that heme induces maturation and secretion of IL-1β in macrophages through activating caspase-1 (Fig. 2a).
Heme activates NLRP3/ASC-caspase-1 axis for IL-1β secretion. a Western blotting for caspase-1 and IL-1β of macrophages pretreated with caspase-1 inhibitor Ac-YVAD-CMK (YVAD; 10 μM) for 1 h, followed by stimulation with heme (30 μM) for 4 h. normalized to β-actin. b ELISA for IL-1β in media from ASC shRNA transfected macrophages, followed by stimulation with heme (30 μM) for 4 h. c ELISA for IL-1β in media from NLRP3−/−and NLRP3+/+ macrophages, followed by stimulation with heme (30 μM) for 4 h. d ELISA for IL-1β in media from NLRC4 shRNA transfected macrophages, followed by stimulation with heme (30 μM) for 4 h
It has been well studied that the activation of caspase-1 depends on the activation of Inflammation which requires adaptor protein ASC [25, 26]. To investigate whether the activation of caspase-1 and maturation of IL-1β is the results of Inflammation/ASC activation, siRNA-mediated ASC gene silence was performed, and macrophages were stimulated with heme. Mature IL-1β in supernatants was detected by western blotting. Knockdown of ASC significantly inhibits the secretion of IL-1β, which primarily suggests that Inflammation/ASC axis is involved in the heme-mediated maturation and secretion of IL-1β (Fig. 2b). Extensive studies demonstrate that NLRP3 is one of the best characterized Inflammations, especially during kidney diseases [2]. Therefore, the role of NLRP3 was determinated in our experiment. Peritoneal macrophages from NLRP3−/−and NLRP3+/+ mice were used to study this problem. As expected, NLRP3+/+ macrophages were efficiently stimulated to secrete IL-1β by heme, and displayed dose-dependent (up to 40 μM) manner. However, no obvious IL-1β was detected from NLRP3−/− macrophages (Fig. 2c). Meanwhile, to further determinate whether NLRC4 inflammasome could also be activated by heme, NLRC4 was silenced by siRNA and the secretion of IL-1β was detected after heme stimulating. The result shows that the secreted IL-1β dramatically increases from the macrophages that NLRC4 knockdown, which displayed on significant differences compared with non-targeting siRNA (Fig. 2d). These results demonstrate that free heme induces IL-1β through activating NLRP3 inflammasome via ASC and suggest that free heme plays an essential role in inflammation response as a dangerous signal.
Heme Activates NLRP3 Through P2X Receptors
In a further step, we asked how heme was recognized and results in NLRP3 activation. The previous studies showed that dangerous signals (such as ATP, biglycan, Uromodulin, etc.) activate NLRP3 through p2X receptor, which result in stimulation of Ca2-independent phospholipase A2 and activation of caspase-1 [6, 27, 28]. Furthermore, P2X7R was reported that participates in NLRP3 activation in renal inflammation and injury induced by high-fat diet [29]. Thereby, we focused on the role of P2X7R in heme recognization. In order to investigate the role of P2X7R in heme induced NLRP3 activation, shRNA-mediated knockdown of P2X7R was performed in macrophages and the secretion of IL-1β was determinated. Western blotting showed that deficiency of P2X7R partially inhibited the secretion of mature IL-1β that heme induced (Fig. 3c). We speculated that other P2X receptors may be also participate in this process. In mouse macrophages, P2X4R is another expressed member of P2X receptor except P2X7R [30]. Therefore, knockdown of P2X4R and double knockdown of P2X7R plus P2X4R were performed by shRNA in macrophages and the result showed that P2X4R knockdown also partially inhibit the heme induced IL-1β secretion and double knockdown of P2X7R plus P2X4R almost completely depressed the IL-1β secretion (Fig. 3d). These results strongly suggest that heme activates NLRP3 through P2X receptors, especially P2X4R and P2X7R.
Heme activates NLRP3 through P2X receptors. a Western blotting for P2X7R of macrophages transfected with scramble shRNA and P2X7R shRNA. b Western blotting for P2X4R of macrophages transfected with scramble shRNA and P2X4R shRNA. c Western blotting for IL-1β of macrophages transfected with scramble shRNA, P2X7R shRNA, P2X4R shRNA, P2X7R shRNA plus P2X4R shRNA
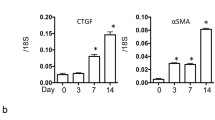
Heme Activates NLRP3-Caspase-1-IL-1β Axis in Kidney Inflammation After UUO
Given that heme is involve in NLRP3-Caspase-1-IL-1β pathway and that inflammasome-regulated cytokines such as IL-1β and IL-18 are implicated in animal models or human forms of CKD [2], we speculated that heme plays an essential role in kidney inflammation. Therefore, Mouse unilateral ureteral obstruction (UUO) model was constructed to investigate the role of heme in kidney inflammation. To determine whether the inflammasome and inflammatory factors were activated in UUO mouse kidney, mature IL-1β, and caspase-1 in kidney was detected at 2, 8, and 16 days after UUO. As expected, increasing amounts of cleaved IL-1β were observed in the lysates of ligated kidneys compared with not sham-operated or contralateral kidneys. Besides inflammatory factors, NLRP3 and Caspase-1 activation were also observed in ligated kidneys with progressively time course as detected by western blotting (Fig. 4a). These results suggest that heme induced activation of NLRP3-Caspase-1-IL-1β axis is involved in kidney inflammation in mice UUO model and that heme serves as a dangerous factor participates in this process.
Heme activates NLRP3-Caspase-1-IL-1β axis in kidney inflammation after UUO. a IL-1β, caspase-1 and NLRP3 activation in mice after UUO. Immunoblotting of kidney tissue lysates from C57Bl/6 mice at 2, 8, and 16 days after UUO. Contralateral (Ctrl) and sham kidneys are used as controls. The appearance of mature IL-1β and p10 subunit of active caspase-1 is observed in the ligated (Lig) kidneys at 2–16 days, consistent with NLRP3 inflammasome activation. b Total heme level in kidney tissue lysates after UUO. c Total heme level in kidney tissue lysates after UUO, followed by tranfected with HO-1 Rec.Ad in vivo. d Immunoblotting of kidney tissue lysates from C57Bl/6 mice at 8 days after UUO, followed by transfected with LacZ. Rec.Ad and HO-1 Rec.Ad in vivo. *P < 0.05, **P < 0.01 (t test)
To provide direct evidence, the heme participates in kidney inflammation, we further detected the free heme level of mice kidney. The heme in the lysates of ligated kidneys progressively increase from 2 to 16 days after UUO (Fig. 4b). Heme oxygenase-1 is a stress-responsive enzyme that converts the protoporphyrin IX ring of heme into biliverdin, releasing iron (Fe) and producing carbon monoxide (CO) [31]. Therefore, HO-1 is essential to clean this deleterious factor. In our experiment, an up-regulation of HO-1 was observed accompanied by the increasing heme during kidney injury. Considering this, HO-1 was overexpressed by transducing with a HO-1 Rec.Ad in vivo, and the heme level, NLRP3, Caspase-1, and IL-1β were detected after UUO (Fig. 4c, d). The results showed that enforced HO-1 could efficiently decline the heme level in the lysates of ligated kidneys, and inhibit kidney inflammation characterized by down-regulation of NLRP3-Caspase-1-IL-1β axis. These results suggest that heme plays an essential role in kidney inflammation via regulating NLRP3-Caspase-1-IL-1β axis.
Discussion
Inflammation is usually accompanied by kidney disease with the process of leucocyte infiltrates and cytokines release. In the past years, inflammatory response against infection has been extensively studied. However, recent studies demonstrate that endogenous molecules from damaged cells play essential role in the immune/inflammatory response [32, 33]. In addition, Various bacterial toxins, haemolysins and extracellular ATP, several crystals (such as hemozoin, silica and antibiotics), anti-fungal drugs, uromodulin, and calcium oxalate were also identified as activator of immune/inflammatory response [1, 27, 34–37]. However, knowledge about the mechanism of sterile inflammation and tissue remodeling after cell damage is relatively deficient.
Here, our study demonstrates that Heme as an endogenous dangerous signal that activates the NLRP3 inflammasome by interacting with P2X receptors. Thereby, the NLRP3/ASC inflammasome and caspase-1 axis are activated which promote maturation and secretion of IL-1β in macrophages. It is notable that heme level significantly enhances in non-infectious inflammatory renal injury (UUO) model, and the enforced expression of HO-1 efficiently inhibits the heme level and immune response after UUO. Therefore, we propose that heme is a potential dangerous signal, which plays an essential role in NLRP3-mediated immune response during kidney disease.
Two signals are needed to produce the proinflammatory master cytokine interleukin IL-1β. First one is the activation of TLRs, IL-1Rs, and TNFRs which results in the transcription and translation of NF-κB to produce pro-forms of IL-1β and IL-18. Another one is enzymatic cleavage by caspase-1, which involves the activation of NLRP3, with recruitment of the adaptor molecule ASC and pro-caspase-1, the later which undergoes autoproteolytic cleavage to produce active form of caspase-1, which in turn acts on their substrates (pro-IL-1β and pro-IL-18) to produce active cytokines [38]. In this report, we have characterized the functions of Heme in the activation of the NLPR3 inflammasome which results in secretion of mature IL-1β. It is intriguing that Heme was also identified as activator of Toll-like receptor 4 that functions on NF-κB or IκB pathway [39]. Therefore, the role of Heme in the innate immune response needs to be further elucidated.
Acute kidney injury or CKD is usually accompanied by kidney inflammation associated or not with the presence of the infectious agents. Intra- or extra-vascular hemolysis is one of the most common characteristics during this process. As a component of hemoproteins, heme induces the immune/inflammation response [40]. The enhanced level of heme in mice after UUO suggests that heme may be a potential molecular target and molecular diagnosis indicator in kidney inflammation therapy. Considering the serious complications during kidney injury, such as sepsis, further investigations will be beneficial to the development of heme-based clinical protocols for these diseases.
References
Collins, A. J., et al. (2009). The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol, 4(Suppl 1), S5–S11.
Anders, H. J., & Muruve, D. A. (2011). The inflammasomes in kidney disease. J Am Soc Nephrol, 22(6), 1007–1018.
Rock, K. L., et al. (2010). The sterile inflammatory response. Ann Rev Immunol, 28, 321–342.
Takeuchi, O., & Akira, S. (2010). Pattern recognition receptors and inflammation. Cell, 140(6), 805–820.
Sanz, A. B., et al. (2010). NF-kappaB in renal inflammation. J Am Soc Nephrol, 21(8), 1254–1262.
Babelova, A., et al. (2009). Biglycan, a danger signal that activates the NLRP3 inflammasome via toll-like and P2X receptors. J Biol Chem, 284(36), 24035–24048.
Ting, J. P., et al. (2008). The NLR gene family: a standard nomenclature. Immunity, 28(3), 285–287.
Schroder, K., & Tschopp, J. (2010). The inflammasomes. Cell, 140(6), 821–832.
Martinon, F., Mayor, A., & Tschopp, J. (2009). The inflammasomes: guardians of the body. Annu Rev Immunol, 27, 229–265.
Joshi, V. D., et al. (2002). Role of caspase 1 in murine antibacterial host defenses and lethal endotoxemia. Infect Immun, 70(12), 6896–6903.
Wang, C., et al. (2012). Quercetin and allopurinol ameliorate kidney injury in STZ-treated rats with regulation of renal NLRP3 inflammasome activation and lipid accumulation. PLoS ONE, 7(6), e38285.
Tsai, P. Y., et al. (2011). Epigallocatechin-3-gallate prevents lupus nephritis development in mice via enhancing the Nrf2 antioxidant pathway and inhibiting NLRP3 inflammasome activation. Free Radic Biol Med, 51(3), 744–754.
Hu, Q. H., et al. (2012). Allopurinol, quercetin and rutin ameliorate renal NLRP3 inflammasome activation and lipid accumulation in fructose-fed rats. Biochem Pharmacol, 84(1), 113–125.
Muller-Eberhard, U., et al. (1968). Plasma concentrations of hemopexin, haptoglobin and heme in patients with various hemolytic diseases. Blood, 32(5), 811–815.
Jacob, H. S. (1994). Newly recognized causes of atherosclerosis: the role of microorganisms and of vascular iron overload. J Lab Clin Med, 123(6), 808–816.
Pamplona, A., et al. (2007). Heme oxygenase-1 and carbon monoxide suppress the pathogenesis of experimental cerebral malaria. Nat Med, 13(6), 703–710.
Graca-Souza, A. V., et al. (2002). Neutrophil activation by heme: implications for inflammatory processes. Blood, 99(11), 4160–4165.
Wagener, F. A., et al. (2003). Different faces of the heme–heme oxygenase system in inflammation. Pharmacol Rev, 55(3), 551–571.
White, L. R., et al. (2007). The characterization of alpha5-integrin expression on tubular epithelium during renal injury. Am J Physiol Renal Physiol, 292(2), F567–F576.
Schaefer, L., et al. (2005). The matrix component biglycan is proinflammatory and signals through Toll-like receptors 4 and 2 in macrophages. J Clin Invest, 115(8), 2223–2233.
Vilaysane, A., et al. (2010). The NLRP3 inflammasome promotes renal inflammation and contributes to CKD. J Am Soc Nephrol, 21(10), 1732–1744.
Soares, M. P., et al. (2004). Heme oxygenase-1 modulates the expression of adhesion molecules associated with endothelial cell activation. J Immunol, 172(6), 3553–3563.
Seixas, E., et al. (2009). Heme oxygenase-1 affords protection against noncerebral forms of severe malaria. Proc Natl Acad Sci USA, 106(37), 15837–15842.
Martinon, F., & Tschopp, J. (2007). Inflammatory caspases and inflammasomes: master switches of inflammation. Cell Death and Differ, 14(1), 10–22.
Martinon, F., et al. (2007). NALP inflammasomes: a central role in innate immunity. Semin Immunopathol, 29(3), 213–229.
Mariathasan, S., et al. (2004). Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature, 430(6996), 213–218.
Darisipudi, M. N., et al. (2012). Uromodulin triggers IL-1beta-dependent innate immunity via the NLRP3 inflammasome. J Am Soc Nephrol, 23(11), 1783–1789.
Mariathasan, S., et al. (2006). Cryopyrin activates the inflammasome in response to toxins and ATP. Nature, 440(7081), 228–232.
Solini, A., et al. (2013). The purinergic 2X7 receptor participates in renal inflammation and injury induced by high-fat diet: possible role of NLRP3 inflammasome activation. J Pathol, 231(3), 342–353.
Guo, C., et al. (2007). Evidence for functional P2X4/P2X7 heteromeric receptors. Mol Pharmacol, 72(6), 1447–1456.
Tenhunen, R., Marver, H. S., & Schmid, R. (1968). The enzymatic conversion of hemetobilirubin by microsomal heme oxygenase. Proc Natl Acad Sci USA, 61, 748.
Matzinger, P. (1994). Tolerance, danger, and the extended family. Ann Rev Immunol, 12, 991–1045.
Beutler, B. (2004). Inferences, questions and possibilities in Toll-like receptor signalling. Nature, 430(6996), 257–263.
Hornung, V., et al. (2008). Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat Immunol, 9(8), 847–856.
Darisipudi, M. N., et al. (2011). Polyene macrolide antifungal drugs trigger interleukin-1beta secretion by activating the NLRP3 inflammasome. PLoS ONE, 6(5), e19588.
Allam, R., et al. (2011). Cutting edge: cyclic polypeptide and aminoglycoside antibiotics trigger IL-1beta secretion by activating the NLRP3 inflammasome. J Immunol, 186(5), 2714–2718.
Mulay, S. R., et al. (2013). Calcium oxalate crystals induce renal inflammation by NLRP3-mediated IL-1beta secretion. J Clin Invest, 123(1), 236–246.
Lorenz, G., Darisipudi, M. N., & Anders, H.J. (2013). Canonical and non-canonical effects of the NLRP3 inflammasome in kidney inflammation and fibrosis. Nephrol Dial Transplant.
Figueiredo, R. T., et al. (2007). Characterization of heme as activator of Toll-like receptor 4. Journal of Biological Chemistry, 282(28), 20221–20229.
Jeney, V., et al. (2002). Pro-oxidant and cytotoxic effects of circulating heme. Blood, 100(3), 879–887.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Qianwei Li and Weihua Fu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, Q., Fu, W., Yao, J. et al. Heme Induces IL-1β Secretion Through Activating NLRP3 in Kidney Inflammation. Cell Biochem Biophys 69, 495–502 (2014). https://doi.org/10.1007/s12013-014-9823-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-014-9823-9