Abstract
The hypoxia-inducible factor-1α (HIF-1α)/vascular endothelial growth factor (VEGF) pathway is involved in skeletal development, bone repair, and postmenopausal osteoporosis. Inhibitors of prolyl hydroxylases (PHD) enhance vascularity, increase callus formation in a stabilized fracture model, and activate the HIF-1α/VEGF pathway. This study examined the effects of estrogen on the HIF-1α/VEGF pathway in osteoblasts and whether PHD inhibitors can protect from bone loss in postmenopausal osteoporosis. Osteoblasts were treated with estrogen, and expressions of HIF-1α and VEGF were measured at mRNA (qPCR) and protein (Western blot) levels. Further, osteoblasts were treated with inhibitors of the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) pathway, and levels of VEGF mRNA and protein expression were detected. In addition, ovariectomized rats were treated with PHD inhibitors, and bone microarchitecture and bone mechanical strength were assessed using micro-CT and biomechanical analyses (lower ultimate stress, modulus, and stiffness). Blood vessel formation was measured with India Ink Perfusion and immunohistochemistry. Estrogen, in a dose- and time-dependent manner, induced VEGF expression at both mRNA and protein levels and enhanced HIF-1α protein stability. Further, the estrogen-induced VEGF expression in osteoblasts involved the PI3K/Akt pathway. PHD inhibitors increased bone mineral density, bone microarchitecture and bone mechanical strength, and promoted blood vessel formation in ovariectomized rats. In conclusion, estrogen and PHD inhibitors activate the HIF-1α/VEGF pathway in osteoblasts. PHD inhibitors can be utilized to protect bone loss in postmenopausal osteoporosis by improving bone vascularity and angiogenesis in bone marrow.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by an imbalance between bone resorption and bone formation, both occurring in bone multicellular units (BMU) [1, 2]. In each BMU, blood supply and bone vascularity play an important role for bone metabolism. Decreased bone formation and bone mass are associated with insufficient or inappropriate blood vessels in and around the bone [3]. New vessels are involved in osteogenesis, and intramembranous and endochondral bone formation process [4]. Postmenopausal and senile osteoporoses are associated with decreased skeletal blood flow [5], reduced capillary networks [6] and impaired endothelial function of the vessels in bone [7].
The hypoxia-inducible factor-1 (HIF-1) is a heterodimeric transcription factor consisting of inducible α and constitutively expressed β subunits. This transcription factor is best known for regulating the expression of vascular endothelial growth factor (VEGF) and a wide range of other genes in response to hypoxia [8]. The HIF-1α/VEGF pathway can induce osteogenesis and angiogenesis during skeletal development [9] and increase bone vascularity and regeneration during bone repair [10]. Activation of the HIF-1α/VEGF signaling pathway in osteoblasts may prevent the bone loss and decrease of blood vessels in bone marrow induced by estrogen deficiency [11]. Therefore, the HIF-1α/VEGF pathway is not only involved in skeletal development and bone repair, but also in postmenopausal osteoporosis.
HIF-1α is rapidly degraded under normoxic conditions. This degradation is biochemically defined by hydroxylation of proline residue by one of three HIF prolyl hydroxylases (PHD), the process requiring oxygen, iron, and 2-oxyglutarate as cofactors [12]. Small molecule inhibitors of PHD can be used to block HIF-1α degradation and thereby activate the pathway. In general, these molecules interfere with the required cofactors for PHD as either iron chelators (e.g., desferrioxamine, DFO) or 2-oxyglutarate analogues (e.g., dimethyloxalylglycine, DMOG), l-mimosine (l-mim) [13–15]. PHD inhibitors enhance vascularity, increase callus formation in a stabilized fracture model, and increase HIF-1α and VEGF activation in vitro [16]. In the present study, we examined whether PHD inhibitors can also increase vascularity and protect from bone loss caused by estrogen deficiency in ovariectomized rats.
Estrogen activates the phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) pathway in target cell. Inhibition of either PI3K/Akt activity or p130 Cas expression blocks the estrogen-induced cyclin D1 expression in breast cancer cells [17, 18]. Estrogen activation of the PI3K/Akt pathway has also been shown to protect cultured neurons from glutamate-induced apoptosis [19]. Osteoblasts are one of the target cells for estrogen, as estrogen can modulate osteoblast activity in vitro by direct receptor-mediated mechanism [20]. In addition to the afore-mentioned study objective, we examined whether estrogen can also activate the PI3K/Akt signaling pathway in osteoblasts, and how the HIF-1α/VEGF and PI3K/Akt pathways are involved in VEGF expression modulated by estrogen.
Materials and Methods
Osteoblast Culture
Osteoblasts were isolated from calvarias of newborn Sprague–Dawley rats obtained from Laboratory Animal Center, Si Lai Ke Co., Ltd. (Shanghai, China) by serial digestion in 0.2 mg/ml collagenase type I (Worthington, Lakewood, LA, USA). Digestions 3–5 containing the osteoblasts were centrifuged, washed with α-minimal essential medium (α-MEM; Mediatech, Herndon, VA, USA) containing 10 % fetal bovine serum and 1 % penicillin/streptomycin, and cultured for 48 h at 37° C. All procedures involving mice were approved by the Institutional Animal Experiment Committee of Shanghai Jiaotong University School of Medicine.
E2 Treatment
Primary osteoblasts from rat calvarias were cultured under 21 % O2 to 80–90 % confluence and treated with estradiol (E2) at different concentrations (0, 10−9, 10−7, or 10−5 M). After 24 h of treatment, total RNA was extracted using Trizol (Invitrogen, Carlsbad, CA, USA).
Expression of HIF-1α and VEGF mRNAs was quantified by qPCR as described below. Protein was extracted using the NE-PER kit (Pierce, Rockford, IL, USA) according to the manufacturer’s instructions. The HIF-1α and VEGF protein expression were detected using Western blot, as described below.
Osteoblasts were also treated with E2 at 10−7 M for 0, 6, 12, or 24 h to examine time-dependent changes of the effect of E2 on HIF-1α, VEGF mRNA, and protein expressions. To study the involvement of the PI3K/Akt pathway in the E2-induced VEGF expression, osteoblasts were treated with E2 (10−7 M) in the presence or absence of signaling inhibitors (25 μM LY294002 or 20 μM wortmannin, both from Sigma-Aldrich, St. Louis, MO, USA), and VEGF mRNA and protein expression were quantified with, respectively, qPCR and Western blot.
qPCR
The SuperScript first-strand synthesis Reverse Transcription (RT) kit (Invitrogen) was used to synthesize cDNA, which was subsequently amplified by qPCR. Primers were designed to yield 150–250 bp sequences within the coding sequences of VEGF and β-actin. The primer sequences were as follows: HIF-1α forward 5′-GAAGACAACGCGGGCACCGA-3′, reverse 5′-TGCTTCGCCGAGATCTTGCTGC-3′, VEGF forward 5′-CCCGGGCCTCGGTTCCAG-3′, reverse 5′-GTCGTGGGTGCAGCCTGGG-3′, and β-actin forward 5′-TTCGTTGCCGGTCCACACCC-3′, reverse 5′-GCTTTGCACATGCCGGAGCC-3′. For qPCR, we utilized SYBR Green kit (Applied Biosystems, Hercules, CA, USA) and RG-3000 qPCR machine (Corbett Research, Cambridge, UK). Reaction conditions were optimized for each of the genes by varying the annealing temperature (50–55 °C) and cDNA load (1–5 ng/reaction).
Western Blot Analysis
Protein concentrations were determined using BCA assay kit (Pierce). Primary monoclonal antibodies against HIF-1α (Novus Biologicals, Inc, Littleton, CO, USA), VEGF (R&D Systems, Minneapolis, MN, USA), and β-actin (Abcam, Cambridge, UK) were used in conjunction with secondary fluorescence-conjugated goat anti-mouse IgG antibodies (Cell Signaling Technologies, Boston, MA, USA). Equal amounts of protein (20 μg) were resolved on 10 % SDS-PAGE and transferred onto a PVDF membrane. Blots were incubated in blocking buffer (TBST with 10 % nonfat milk) for 3 h at room temperature with agitation, followed by the addition of the primary antibody diluted in blocking buffer as recommended by the manufacturer. The blot was incubated overnight at 4 °C with agitation. The Odyssey fluorescent scanning system (Odyssey LI-COR Inc., Lincoln, OR, USA) was used to visualize the bands.
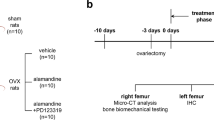
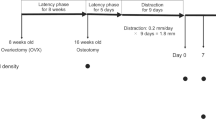
Rats and Treatments
Three-month-old female rats were divided randomly into three groups: saline group (bilaterally ovariectomized and supplemented with saline; n = 24), DFO group (bilaterally ovariectomized and supplemented with DFO, n = 24), and DMOG group (bilaterally ovariectomized and supplemented with DMOG, n = 24). For interventions, rats were intraperitoneally injected with, respectively, 20 μL of saline, DFO (200 μM), or DMOG (500 μM) [16]. The injections were carried out for 5 days/week. After 12 weeks of treatment, the rats were euthanized by overdose with pentobarbital sodium. After that, the femur and tibiae were isolated for subsequent studies.
Micro-computed Tomography (Micro-CT)
Micro-CT analysis was performed on the distal femur [21] using Lotus SP imager (GE Medical System, London, UK) with an X-ray tube voltage of 70 kV and a current of 100 A, with a 1 mm aluminum filter. Fixed right femurs were located in cylindrical sample tubes and scanned with micro-CT. Three-dimensional analyses were carried out. For each sample, bone mineral density (BMD) as well as trabecular structural parameters, such as bone volume per total volume (BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), and trabecular separation (Tb.Sp), were measured within a region of 100 scan slices (3,200 μm) proximal to the growth plate at the distal ends of the femur.
Immunohistochemistry
Tibiae sections were quenched with 3 % hydrogen peroxide for 15 min to reduce endogenous peroxide activity and blocked with 3 % normal goat serum in Tris-buffered saline. The sections were then incubated with rabbit anti-rat CD31 polyclonal antibodies (Santa Cruz Biotechnology, Dallas, TX, USA) at 4 °C overnight, followed by biotinylated secondary antibodies and the peroxidase-labeled streptavidin–biotin staining kit (DAB kit, Invitrogen). The slides that were not incubated with secondary antibody were used as negative controls. The number of CD31 positive cells within four visual fields of each slice of tissue under light microscope was counted with LEICA QWIN Software by a systematic random-sampling [22].
India Ink Perfusion of Bone
To quantify the vessel numbers in metaphyseal zone, we perfused rats with India ink as previously described [23]. In brief, rats were anesthetized with 2.5 % pentobarbital sodium and placed supine on a dissecting stage. Blood was cleared by inserting a catheter into the left ventricle and washed with heparinized saline followed by India ink perfusion (Speedball 3398, Hunt Manufacturing, Statesville, NC, USA). All perfusions were performed at a pressure of 90–100 mmHg and continued until all rat tissues appeared dark. The tissues were then infused with a 4 % paraformaldehyde solution (20 mL) to fix the vasculature. Following perfusion, the distal femurs were resected and fixed in 10 % buffered formalin for 48 h, decalcified in 10 % EDTA (pH 7.0) for 20 days, and embedded in paraffin. The 5-μm thick cross sections of the femur metaphysis zone were obtained for eosin staining. The blood vessel numbers in the metaphysis zone were quantified in a blinded manner according to established methods described previously [24].
Biomechanical Analyses
Femurs were thawed at room temperature, and three-point bending of the right femora was carried out by an Instron 5569 materials testing machine (Instron, Norwood, OH, USA). The femur was placed with the posterior side facing down between two supports that were 6 mm apart. The load was applied at the mid-span which caused bending to occur near the anteroposterior axis. Load–displacement curves were recorded at a crosshead speed of 1 mm/s.
Statistical Analysis
All values are expressed as mean ± SD. The Graphpad PRISM version 4.0 (GraphPad Software, Lo Jolla, CA, USA) was used for analyses, and intergroup variance was evaluated by one-way ANOVA. Differences with the p value of less than 0.05 were considered statistically significant.
Results
E2 Induces HIF-1α and VEGF Expression in Osteoblasts in a Dose- and Time-Dependent Manner
To explore possible relationship between estrogen and the HIF-1α/VEGF pathway, osteoblasts were cultured and treated with increasing E2 concentrations (0–10−5 M) for 24 h, or with a fixed concentration (10−7 M) for different periods of time (0–24 h). Results showed that E2 increased HIF-1α protein stability and VEGF protein expression in a dose- (Fig. 1a) and time-dependent (Fig. 1c) manner. With regard to mRNA level, E2 was able to also increase VEGF mRNA expression in a dose- and time-dependent manner, while HIF-1α mRNA expression was not changed (Fig. 1b and d). This meant that E2 acts by inhibiting HIF-1α protein degradation rather via induction of expression of its mRNA.
E2 induces HIF-1α and VEGF protein expression in a dose- and time-dependent manner. Primary osteoblasts from rat calvarias were cultured and treated with different concentrations of E2. a Western blot analysis demonstrates that E2 induces HIF-1α protein stability and VEGF protein expression in a dose-dependent manner. b Real-time PCR analysis demonstrates that VEGF mRNA expression was changed in a dose-dependent manner after the 24 h treatment with increasing E2 concentrations (0–10−5 M). However, HIF-1α mRNA expression did not change. filled square VEGF, filled diamond HIF-1α, *p < 0.05 versus 0 M. c Western blot analysis demonstrates that E2 induces HIF-1α protein stability and VEGF protein expression in a time-dependent manner after treatment with 10−7 M for 0, 6, 12, 24 h. d Real-time PCR shows that VEGF mRNA expression is up-regulated in a time-dependent manner after treatment with E2 (10−7 M). However, HIF-1α mRNA expression did not change. filled square VEGF, filled diamond HIF-1α, *p < 0.05 versus E2 treatment at 0 h. Data are shown either as representative images or mean ± SD of three independent experiments
The E2-Induced VEGF Expression in Osteoblasts is Mediated by PI3K/Akt Pathway
After we observed that E2-induced VEGF expression in osteoblasts in a dose- and time-dependent manner, we further studied whether this involved the PI3K/Akt pathway. As shown in Fig. 2, VEGF mRNA and protein levels were significant up-regulated after E2 treatment. Inhibition of the PI3K/Akt pathway via pre-treatment of osteoblasts with inhibitor LY294002 significantly decreased VEGF mRNA and protein expression levels. Similar to LY294002, wortmannin also blocked the E2-induced VEGF expression. These results demonstrated that the PI3K/Akt pathway is involved in the E2-induced VEGF expression. Further, blocking of the PI3K/Akt pathway with LY294002 and wortmannin was capable of inhibiting the E2-induced VEGF expression in osteoblasts.
The E2-induced VEGF expression is mediated by the PI3K/Akt pathway. Primary osteoblasts from rat calvarias were treated with PI3K inhibitor (a, b: 25 μM LY294002, LY; c, d: 20 μM wortmannin, Wort) for 1 h before treatment with E2 (10−7 M) for further 24 h. VEGF protein expression was analyzed by Western blot analysis (a and c), while VEGF mRNA expression levels were analyzed by real-time PCR (b and d). Data in b are presented as mean ± SD of three independent experiments. *p < 0.05, **p < 0.01. Data in d are presented as mean ± SD of three independent experiments. *p < 0.05, **p < 0.01
PHD Inhibitors Protect from the Ovariectomy-Induced Bone Loss
To examine bone mass and trabecular architecture, the femurs of all groups were compared by three-dimensional measurement using micro-CT. We observed that the bone mass and architecture in the saline group deteriorated after 12 weeks, while these indices were better in the DFO and DMOG groups (Fig. 3a). BMD, an important indicator of bone mass and architecture, was significantly (p < 0.05) increased in both DFO and DMOG groups compared with saline group (Fig. 3b). Consistent with these findings, trabecular BV/TV, Tb.Th, and Tb.N of the distal femur were significantly (p < 0.05) increased, whereas Tb.Sp was significantly (p < 0.05) decreased in the DFO and DMOG group compared with the saline group (Fig. 3c–f).
PHD inhibitors protect from the ovariectomy-induced bone loss. a Reconstructed 3D images in all groups of the trabecular bone at the femur show that treatment with DFO and DMOG provided better bone mass and trabecular architecture than treatment with saline. b BMD in the DFO and DMOG groups was significantly higher than in the saline group (*p < 0.05). c–e Ratios of bone volume per total volume (BV/TV), trabecular thickness (Tb.Th), and trabecular number (Tb.N) in the DFO and DMOG groups were significantly higher than in the saline group (*p < 0.05). f Trabecular separation (Tb.Sp) was significantly lower in the DFO and DMOG groups compared with saline group (*p < 0.05)
PHD Inhibitors Induce CD31 Protein Expression in Bone Marrow and Increase Bone Vascularity
Immunohistochemistry of sections of proximal tibia indicated that CD31 protein expression in bone marrow was markedly higher in the DFO and DMOG groups than in saline group, where it was expressed at a relatively low level (Fig. 4a). The quantitation further verified that the observed differences in the number of CD31 positive cells between the DFO and DMOG groups and saline group were statistically different (p < 0.05; Fig. 4c).
PHD inhibitors induce CD31 protein expression in bone marrow and increase bone vascularity. a CD31 protein expression in bone marrow was higher in DFO and DMOG groups compared with saline group (immunohistochemistry of sections of proximal tibia). b Vascular numbers were increased in the DFO and DMOG groups as shown by India ink perfusion of the metaphysis zone of the femur. c The number of CD31 positive cells in the DFO and DMOG groups were significantly (*p < 0.05) higher than in saline group. d The number of blood vessels in the DFO and DMOG groups was significantly (*p < 0.05) higher than in saline group
We further used India ink perfusion to assess the difference of bone vascularity in study groups. The blood vessel number was increased in DFO and DMOG groups (Fig. 4b); quantitation of blood vessels in metaphysis zone of the femur further confirmed a significant increase in both DFO and DMOG groups compared with saline group (p < 0.05; Fig. 4d).
PHD Inhibitors Protect from the Ovariectomy-Induced Decrease in Mechanical Strength
The femoral mechanical properties were evaluated by the three-point bending test after 12 weeks of treatment. All femora displayed a load–displacement curve typical for a long bone. As expected, saline group displayed weaker mechanical properties of femurs reflected by lower ultimate stress, modulus, and stiffness. By contrast, DFO and DMOG treatments were effective in increasing the femoral mechanical properties compared with saline group (Fig. 5).
PHD inhibitors protected from the ovariectomy-induced decrease in mechanical strength. The femoral mechanical properties were evaluated by the three-point bending test after 12 weeks of treatment. Treatment with DFO or DMOG was significantly (*p < 0.05) more effective in increasing mechanical properties of femoral modulus, stiffness, and ultimate stress compared with saline group
Discussion
The skeleton is a dynamic organ in which mineralized bone is continuously resorbed by osteoclasts and a new bone is formed by osteoblasts. Osteoporosis is characterized by an imbalance between bone resorption and bone formation, which takes place in BMU [1, 2]. In this anatomically discrete compartment, new osteoblasts appear only at sites recently vacated by osteoclasts, a phenomenon called “coupling” [4]. The presence of vessels in the center of the BMU is strategically well-suited for participation in coupling. There is an increasing body of evidence implicating the vasculature in the mechanism of coupling [25, 26]. In postmenopausal women, histological analyses made on osteoporotic bone of patients with primary osteoporosis showed decreased numbers of arterial capillaries and sinuses per unit area [3]. Moreover, expression of VEGF, a major angiogenic stimulator, was found to be significantly reduced in the bones of ovariectomized mice [27]. Several risk factors for vascular diseases, such as hypertension, diabetes, smoking, and alcoholism, are also associated with osteoporosis suggesting that vascular component plays a vital role in the pathogenesis of osteoporosis. Mice with activated HIF-1α signaling pathway in osteoblasts showed increased angiogenesis and osteogenesis and were protected from the ovariectomy-induced bone loss indicating that activation of the HIF-1α signaling pathway in osteoblasts prevented the estrogen deficiency-induced bone loss and decrease in blood vessels in bone marrow [11]. DFO and DMOG are the inhibitors of the PHD and can be used to block HIF-1α degradation and thereby activate the HIF-1α pathway [13, 14]. DFO and DMOG induce expression of VEGF mRNA in marrow mesenchymal stromal cells (MSCs) in vitro and increase capillary sprouting in a stabilized fracture model in vivo. This suggests that DFO and DMOG may increase vascularity and bone formation following skeletal trauma [16]. In this paper, we explored the effect of DFO and DMOG on ovariectomized rats.
Our studies demonstrated that E2 induce VEGF mRNA and protein expression and also increases the HIF-1α protein stability in a dose- and time-dependent manner, thus implicating estrogen as a key modulator of angiogenesis. Estrogen exerts a significant protective effect on the skeleton, and the loss of estrogen predisposes to the development of postmenopausal osteoporosis [28]. Postmenopausal and senile osteoporoses are associated with decreased skeletal blood flow [5], reduced capillary networks [6], and impaired endothelial function of the vessels in bone [7]. Estrogens stimulate VEGF expression in renal tubular cells [29] and stromal endometrial cells [30]. Chromatin immunoprecipitation analysis demonstrated that estrogen regulation of VEGF expression in the rat uterus involves rapid recruitment of both estrogen receptor-alpha (ER-α) and HIF-1α to the VEGF promoter [31, 32]. In ovariectomized Gottingen miniature pig model, VEGF expression in trabecular is reduced and VEGF in the supernatant of osteoblasts after incubation with estrogen is increased [33].
Our study results also confirmed that the E2-induced VEGF expression in osteoblasts was mediated by PI3K/Akt pathway. Estrogen can activate the PI3K/Akt signaling pathway in target cell, i.e., primary rodent neurons [19, 34] and ER-positive human breast cancer cells [17, 19, 32–35]. In the uterus, estrogen can induce the activation of HIF-1α and up-regulate VEGF expression, as demonstrated by the PI3K/Akt chromatin immunoprecipitation analysis [31, 32]. Estrogen activation of PI3K/Akt is also observed in the rat and mouse endometrium, specifically, in the epithelial cells in vivo [36]. Phospho-Akt levels are also the highest in human endometrial glandular epithelial cells during the late proliferative phase, when estrogen levels are the highest [37]. Osteoblast is one of the target cells for estrogen; our results further reveal that estrogen can also activate the PI3K/Akt pathway.
We used ovariectomized rats to study effects of DFO and DMOG on bone quality in a postmenopausal osteoporosis state. Ovariectomy was shown to successfully induce menopause-like osteoporosis in female rats, and this osteoporosis was characterized by rapid trabecular bone loss [38]. The micro-CT results showed that DFO and DMOG groups significantly increase BMD and bone structural parameters at the distal metaphysic of femur. Furthermore, mechanical quality of the bone was also increased in DFO and DMOG groups. These experimental results verified that PHD inhibitors can prevent the bone loss in ovariectomy rats.
The expression of CD31, the endothelial cell marker, was used to evaluate the angiogenesis in bone marrow [39]. Our results demonstrate that DFO and DMOG treatment could increase the angiogenesis in bone marrow in ovariectomy rats. Our findings also suggested that DFO and DMOG treatment induce bone vascularity in ovariectomy rats. A tentative mechanism of PHD inhibitors is linked to their facilitation of bone vascularity and angiogenesis in bone marrow.
Finally, our findings suggest that estrogen is associated with the HIF-1α/VEGF pathway in osteoblasts and that small molecule inhibitors of PHD can be utilized in protecting from the bone loss induced by estrogen deficiency in postmenopausal osteoporosis. Our studies further highlight the use of these compounds in postmenopausal osteoporosis as well as bone injury for which bone vascularity is critical.
References
Harada, S., & Rodan, G. A. (2003). Control of osteoblast function and regulation of bone mass. Nature, 423, 349–355.
Boyle, W. J., Simonet, W. S., & Lacey, D. L. (2003). Osteoclast differentiation and activation. Nature, 423, 337–342.
Burkhardt, R., Kettner, G., Bohm, W., Schmidmeier, M., Schlag, R., Frisch, B., et al. (1987). Changes in trabecular bone, hematopoiesis and bone marrow vessels in aplastic anemia, primary osteoporosis, and old age: A comparative histomorphometric study. Bone, 8, 157–164.
Parfitt, A. M. (2000). The mechanism of coupling: A role for the vasculature. Bone, 2000(26), 319–323.
Vogt, M. T., Cauley, J. A., Kuller, L. H., & Nevitt, M. C. (1997). Bone mineral density and blood flow to the lower extremities: The study of osteoporotic fractures. Journal of Bone and Mineral Research, 12, 283–289.
Street, J. T., de Schrijver, K., Wang, J. H., Wu, Q. D., & Redmond, H. P. (2005). Hypoxia regulates the paracrine coupling of angiogenesis and bone formation. European Journal of Orthopaedic Surgery & Traumatology, 2005, 214–225.
Sanada, M., Taguchi, A., Higashi, Y., Tsuda, M., Kodama, I., Yoshizumi, M., et al. (2004). Forearm endothelial function and bone mineral loss in postmenopausal women. Atherosclerosis, 176, 387–392.
Semenza, G. L. (2003). Targeting HIF-1 for cancer therapy. Nature Reviews Cancer, 2003(3), 721–732.
Wang, Y., Wan, C., Deng, L., Liu, X., Cao, X., Gilbert, S. R., et al. (2007). The hypoxia-inducible factor alpha pathway couples angiogenesis to osteogenesis during skeletal development. The Journal of Clinical Investigation, 117, 1616–1626.
Wan, C., Gilbert, S. R., Wang, Y., Cao, X., Shen, X., Ramaswamy, G., et al. (2008). Activation of the hypoxia-inducible factor-1alpha pathway accelerates bone regeneration. Proceedings to the National Academy of Science USA, 105, 686–691.
Zhao, Q., Shen, X., Zhang, W., Zhu, G., Qi, J., & Deng, L. (2012). Mice with increased angiogenesis and osteogenesis due to conditional activation of HIF pathway in osteoblasts are protected from ovariectomy induced bone loss. Bone, 50, 763–770.
Ivan, M., Kondo, K., Yang, H., Kim, W., Valiando, J., Ohh, M., et al. (2001). HIFalpha targeted for VHL-mediated destruction by proline hydroxylation: Implications for O2 sensing. Science, 292, 464–468.
Wang, G. L., & Semenza, G. L. (1993). Desferrioxamine induces erythropoietin gene expression and hypoxia-inducible factor 1 DNA-binding activity: Implications for models of hypoxia signal transduction. Blood, 82, 3610–3615.
Warnecke, C., Griethe, W., Weidemann, A., Jurgensen, J. S., Willam, C., Bachmann, S., et al. (2003). Activation of the hypoxia-inducible factor-pathway and stimulation of angiogenesis by application of prolyl hydroxylase inhibitors. FASEB Journal, 17, 1186–1188.
Chau, N. M., Rogers, P., Aherne, W., Carroll, V., Collins, I., McDonald, E., et al. (2005). Identification of novel small molecule inhibitors of hypoxia-inducible factor-1 that differentially block hypoxia-inducible factor-1 activity and hypoxia-inducible factor-1alpha induction in response to hypoxic stress and growth factors. Cancer Research, 65, 4918–4928.
Shen, X., Wan, C., Ramaswamy, G., Mavalli, M., Wang, Y., Duvall, C. L., et al. (2009). Prolyl hydroxylase inhibitors increase neoangiogenesis and callus formation following femur fracture in mice. Journal of Orthopaedic Research, 27, 1298–1305.
Castoria, G., Migliaccio, A., Bilancio, A., Di, D. M., de Falco, A., Lombardi, M., et al. (2001). PI3-kinase in concert with Src promotes the S-phase entry of oestradiol-stimulated MCF-7 cells. EMBO Journal, 20, 6050–6059.
Cabodi, S., Moro, L., Baj, G., Smeriglio, M., Di, S. P., Gippone, S., et al. (2004). p130Cas interacts with estrogen receptor alpha and modulates non-genomic estrogen signaling in breast cancer cells. Journal of Cell Science, 117, 1603–1611.
Honda, K., Sawada, H., Kihara, T., Urushitani, M., Nakamizo, T., Akaike, A., et al. (2000). Phosphatidylinositol 3-kinase mediates neuroprotection by estrogen in cultured cortical neurons. Journal of Neuroscience Research, 60, 321–327.
Yen, M. L., Su, J. L., Chien, C. L., Tseng, K. W., Yang, C. Y., Chen, W. F., et al. (2005). Diosgenin induces hypoxia-inducible factor-1 activation and angiogenesis through estrogen receptor-related phosphatidylinositol 3-kinase/Akt and p38 mitogen-activated protein kinase pathways in osteoblasts. Molecular Pharmacology, 68, 1061–1073.
Tivesten, A., Moverare-Skrtic, S., Chagin, A., Venken, K., Salmon, P., Vanderschueren, D., et al. (2004). Additive protective effects of estrogen and androgen treatment on trabecular bone in ovariectomized rats. Journal of Bone and Mineral Research, 19, 1833–1839.
Parfitt, A. M., Drezner, M. K., Glorieux, F. H., Kanis, J. A., Malluche, H., Meunier, P. J., et al. (1987). Bone histomorphometry: Standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. Journal of Bone and Mineral Research, 2, 595–610.
Shepherd, B. R., Chen, H. Y., Smith, C. M., Gruionu, G., Williams, S. K., & Hoying, J. B. (2004). Rapid perfusion and network remodeling in a microvascular construct after implantation. Arteriosclerosis, Thrombosis, and Vascular Biology, 24, 898–904.
Kennedy, J. M., & Zochodne, D. W. (2002). Influence of experimental diabetes on the microcirculation of injured peripheral nerve: Functional and morphological aspects. Diabetes, 51, 2233–2240.
Parfitt, A. M. (1994). Osteonal and hemi-osteonal remodeling: The spatial and temporal framework for signal traffic in adult human bone. Journal of Cellular Biochemistry, 1994(55), 273–286.
Parfitt, A. M. (1998). Osteoclast precursors as leukocytes: Importance of the area code. Bone, 1998(23), 491–494.
Ding, W. G., Wei, Z. X., & Liu, J. B. (2011). Reduced local blood supply to the tibial metaphysis is associated with ovariectomy-induced osteoporosis in mice. Connective Tissue Research, 52, 25–29.
Richelson, L. S., Wahner, H. W., Melton, L. J., I. I. I., & Riggs, B. L. (1984). Relative contributions of aging and estrogen deficiency to postmenopausal bone loss. New England Journal of Medicine, 311, 1273–1275.
Kang, D. H., Yu, E. S., Yoon, K. I., & Johnson, R. (2004). The impact of gender on progression of renal disease: Potential role of estrogen-mediated vascular endothelial growth factor regulation and vascular protection. American Journal of Pathology, 164, 679–688.
Sugino, N., Kashida, S., Takiguchi, S., Karube, A., & Kato, H. (2000). Expression of vascular endothelial growth factor and its receptors in the human corpus luteum during the menstrual cycle and in early pregnancy. Journal of Clinical Endocrinology and Metabolism, 85, 3919–3924.
Kazi, A. A., Jones, J. M., & Koos, R. D. (2005). Chromatin immunoprecipitation analysis of gene expression in the rat uterus in vivo: Estrogen-induced recruitment of both estrogen receptor alpha and hypoxia-inducible factor 1 to the vascular endothelial growth factor promoter. Molecular Endocrinology, 19, 2006–2019.
Kazi, A. A., & Koos, R. D. (2007). Estrogen-induced activation of hypoxia-inducible factor-1alpha, vascular endothelial growth factor expression, and edema in the uterus are mediated by the phosphatidylinositol 3-kinase/Akt pathway. Endocrinology, 2007, 2363–2374.
Pufe, T., Claasen, H., Scholz-Ahrens, K. E., Varoga, D., Drescher, W., Franke, A. T., et al. (2007). Influence of estradiol on vascular endothelial growth factor expression in bone: A study in Göttingen miniature pigs and human osteoblasts. Calcified Tissue International, 2007, 184–191.
Ivanova, T., Mendez, P., Garcia-Segura, L. M., & Beyer, C. (2002). Rapid stimulation of the PI3-kinase/Akt signalling pathway in developing midbrain neurones by oestrogen. Journal of Neuroendocrinology, 14, 73–79.
Sun, M., Paciga, J. E., Feldman, R. I., Yuan, Z., Coppola, D., Lu, Y. Y., et al. (2001). Phosphatidylinositol-3-OH kinase (PI3K)/AKT2, activated in breast cancer, regulates and is induced by estrogen receptor alpha (ERalpha) via interaction between ERalpha and PI3K. Cancer Research, 61, 5985–5991.
Lengyel, F., Vertes, Z., Kovacs, K. A., Kornyei, J. L., Sumegi, B., & Vertes, M. (2004). Expression and activation of Akt/protein kinase B in sexually immature and mature rat uterus. Journal of Steroid Biochemistry and Molecular Biology, 91, 285–288.
Guzelogli Kayisli, O., Kayisli, U. A., Luleci, G., & Arici, A. (2004). In vivo and in vitro regulation of Akt activation in human endometrial cells is estrogen dependent. Biology of Reproduction, 2004(71), 714–721.
Bain, S. D., Bailey, M. C., Celino, D. L., Lantry, M. M., & Edwards, M. W. (1993). High-dose estrogen inhibits bone resorption and stimulates bone formation in the ovariectomized mouse. Journal of Bone and Mineral Research, 8, 435–442.
Jeong, B. C., Kim, H. J., Bae, I. H., Lee, K. N., Lee, K. Y., Oh, W. M., et al. (2010). COMP-Ang1, a chimeric form of Angiopoietin 1, enhances BMP2-induced osteoblast differentiation and bone formation. Bone, 46, 479–486.
Acknowledgments
This work was supported by National Natural Science Foundation of China (NSFC, No.81372015), Shanghai Natural Science Foundation (No. 11ZR1434100) and Shanghai Municipal Health Bureau Project (No. 2013214).
Conflict of interest
The authors have no conflict of interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, X., Tu, Y., Zhang, L. et al. Prolyl Hydroxylase Inhibitors Protect from the Bone Loss in Ovariectomy Rats by Increasing Bone Vascularity. Cell Biochem Biophys 69, 141–149 (2014). https://doi.org/10.1007/s12013-013-9780-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-013-9780-8