Abstract
To investigate the changes in arterial oxygenation and intrapulmonary shunt during one-lung ventilation (OLV) with intravenous infusion of dexmedetomidine combined with isoflurane inhalation. ASA I–II 60 patients aged 18–70 year, undergoing OLV during elective thoracic surgery were randomly allocated to two groups: (1) isoflurane + saline (group NISO, n = 30) and (2) isoflurane + dexmedetomidine (group DISO, n = 30). After induction, anesthesia was maintained with intravenous infusion of remifentanil 0.1–0.2 μg kg−1 min−1 and inhalation isoflurane (1.0–2.0 %). In addition, anesthesia was maintained with intravenous infusion of dexmedetomidine 0.7 μg kg−1 h−1 in DISO group and saline 0.25 ml kg−1 h−1 in NISO group. Bispectral Index values were maintained within 40–60 by changing the concentration of isoflurane in all groups. Arterial blood gas samples and central venous blood gas samples were taken as follows: during two-lung ventilation before OLV and during the first 40 min of OLV. 45 Patients completed the study, with 23 patients in DISO group and 22 patients in NISO group. The two groups were comparable in terms of demographic variables, hemodynamic, PaO2, Qs/QT, end expiration isoflurane and BIS levels during the operation. Compared with patients in the group NISO, there were significant increases with PaO2, significant decrease with Qs/QT, significant decrease with end expiration isoflurane, and significant decrease with HR in the group DISO during the first 40 min of OLV (P < 0.05). Dexmedetomidine infusions decrease the requirement for isoflurane, decrease intrapulmonary shunt, and moderate the change in PaO2 and may be useful in managing OLV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoxemia is the most common phenomenon in single-lung ventilation (one-lung ventilation, OLV) anesthetic management, caused by pulmonary arteriovenous shunt in the non-ventilated lung, leading to the decrease of PaO2 and SaO2. Pulmonary shunt is affected by many factors, including hypoxic pulmonary vasoconstriction (HPV), which is one of the most important protective mechanism in which small pulmonary arteries of the non-ventilated part contracts, thus decreasing the pulmonary shunt [1]. Inhalation anesthetics may inhibit HPV, increase hypoxemia [2]. Dextral Dexmedetomidine (Dex) is a new highly selective a2 adrenergic receptor agonist and it has been shown that Dex could reduce the dose of the inhalation and intravenous anesthetics [3]. The purpose of this study is to evaluate the pulmonary shunt fraction during one-lung ventilation and arterial oxygenation when intravenous infusion of Dex is combined with inhalation of isoflurane, and to explore the safety and feasibility in the application of Dex in one-lung ventilation.
Materials and Methods
General Information
Hospital Ethics Committee approval and the patients’ and their families’ signed consent were obtained prior to the study. 60 General thoracic surgery patients were selected, ASA I–II, aged 18–70 years old, weighing 49–73 kg, height 151–175 cm. No serious heart and lung disorders, liver and kidney dysfunction were seen in these patients. Exclusion criteria: long-term alcohol, opioid, or sedative hypnotic drug addiction and dependency history, history of drug allergy, neuropsychiatric diseases.
Quality Control and Test Groups
All patients were randomly divided into two groups, intravenous infusion of the dexmedetomidine combined with isoflurane inhalation (DISO group) and the intravenous infusion of normal saline with isoflurane inhalation (NISO group) with 30 patients in each group. All operations and intraoperative anesthetic management were performed by the same physician and blood sample collection and analysis were done by a nurse anesthetist, and these analysts were blind to the group category of the patients; drugs were prepared by specialized staff, who did not participate in the process of anesthesia and the subsequent statistical analysis. All the data analysis and statistics were completed by professional assistant.
Anesthesia
All the patients recruited in this study did not use any premedication. After patients were in the operating room, left upper extremity peripheral venous access (16 or 18G IV catheter) was established, with the use of Philips monitors (IntelliVue MP50, Philips company) and routine monitoring of ECG, NIBP, SPO2, and temperature. Using 20G arterial needle (BD company) line of left radial artery cannulation continuous monitoring of blood pressure was performed; arterial blood samples were drawn for the first blood gas analysis. All patients received module and electrodes monitor for bispectral index (BIS, Aspect Medical Systems), the anesthesia machine was prepared (Drager GS, Germany, Drager companies) and the thread mask of oxygen intravenous midazolam 2 mg, fentanyl 4 μg kg−1, propofol 2 mg kg−1, and vecuronium 0.1 mg kg−1 was administered, followed by 3–5 min of bronchial intubation, the left or right into the Robertshaw double-lumen tube 35–39 #, positioned straight after the fixed bronchial tube by bronchoscopy microscope (Olympus LF-DP, Japan Olympus Corporation). Intermittent positive pressure ventilation (IPPV) mechanical ventilation is used during one-lung ventilation: TV 6 ml kg−1, RR 12 bpm, I:E = 1:2, FiO2 100 %, PEEP is not used in surgery. Concentrations of isoflurane in the inhalation gas (FiIso), and in the exhaled gas (EEIso) and end-tidal carbon dioxide concentration (PETCO2) were measured by Drager PM8030. Central venous catheter was inserted into internal jugular vein lumen insertion, 15–18 cm deep, equivalent to the level of the right atrium. After bronchial intubation positioning, DISO group immediately started intravenous infusion of Dex 1.0 μg kg−1 h−1 (d-Dexmedetomidine liquid: Jiangsu Hengrui Medicine Co., Ltd. production, 100 μg ml−1, diluted with normal saline to 50 ml), 10 min later adjusted to 0.7 μg kg−1 h−1; NISO group began intravenous infusion of saline 0.25 ml kg−1 h−1, 10 min later adjusted to 0.18 ml kg−1 h−1. During maintenance of anesthesia, all patients had continuous intravenous infusion of remifentanil 0.1–0.2 μg kg−1 min−1, and isoflurane 1.0–2.0 %, intermittent recovery Garvey rocuronium to maintain muscle relaxation. Anesthesia depth was monitored with BIS values, which was controlled between 40 and 60. Under the premise of satisfactory depth of anesthesia, intraoperative vasoactive drugs were used to maintain hemodynamic stability. Doses of the use of vasoactive drugs (atropine, ephedrine, and urapidil) of two groups were documented. Correct location of bronchial tube was verified by bronchoscopy after lateral position. One-lung ventilation started after thoracotomy. If SpO2 < 90 % after OLV immediately re-application of assisted ventilation technology lung ventilation or the depth of anesthesia BIS values is <40 or >60 intraoperative, both occasions were withdrew from the study.
Outcome Measures
Pulmonary function tests and arterial blood gas analysis for all patients were done before operation, lung ventilation (TLV) 15 min (TLV-15 min); OLV once every 10 min after the start until 40 min of OLV, arterial blood gases were drawn, central venous blood gas, HR, MAP, BIS values, EEIso value, intrapulmonary shunt according to the formula Qs/Qt = [(Cc′O2 − CaO2)/(Cc′O2 − CvO2)] × 100 %, which CvO2 replaced by the CcvO2 [4], the end of operation records the amount of transfusion during surgery.
Statistical Analysis
Measurement data as mean ± SD that meet the data analysis of variance between groups compared using ANOVA, pairwise comparison between groups by SNK test, the data do not meet the analysis of variance with rank sum test; one-lung ventilation blood gas analysis of data comparing different times using repeated measures analysis of variance, P < 0.05 was considered statistically significant.
Results
Age, sex, height, pulmonary function tests, and arterial blood gas analysis before the operation were not statistically significant (P > 0.05) (Table 1). In DISO group there were 3 patients with BIS value over the range, and another 4 cases were observed with SpO2 less than 90 % during one-lung ventilation. Therefore, 7 cases in total were excluded in this study and the remaining 23 cases were included in the actual study; in NISO group, 2 cases with BIS value over the range, 6 cases with SpO2 < 90 % were observed during one-lung ventilation, and thus in total 8 cases were excluded with 22 cases included actually in this study.
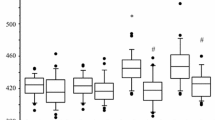
Interestingly, the patients’ arterial oxygen pressure and partial flow were significantly different between single-lung ventilation and TLV 15 min time points, with significantly decreased PaO2 (P < 0.05), and significantly increased Qs/QT (P < 0.05). During one-lung ventilation, PaO2 increased significantly in DISO group compared to NISO group (P < 0.05), and Qs/QT decreased (P < 0.05) (Table 2). Besides, during the observation period, compared to NISO group, FETIso in DISO group was significantly reduced (P < 0.05), with significantly decreased heart rate (P < 0.05). However, mean arterial blood pressure and the use of vasoactive drugs were not significantly different (P > 0.05) (Table 2).
Discussion
QS/QT ratio is about 2–5 % during normal breathing and about 10 % after general anesthesia and lying sideward, but increased more seriously, up to 40–50 %, after one-lung ventilation [5]. The results from this study indicated that after the start of one-lung ventilation, patients in both the groups had significant increase in shunt. At OLV-10 min, DISO group QS/QT is about 30.4 ± 2.5 in DISO group and is 38.7 ± 1.7 in NISO group, in agreement with earlier reported values [6, 7]. In addition, after the start of OLV, PaO2 started to decrease significantly in both the groups, down to the valley about 30 min later, and started to rise slowly after about 40 min due to the role of HPV. Since there were no significant differences in age, weight, surgical site, lung function, and other factors between the two groups, the results of this study further confirmed that changes in ventilation perfusion ratio occurred in patients during single-lung ventilation, and that the trend of change was consistent with the previous reports in literature.
Dex is a new highly selective a2 adrenergic receptor agonist, with a strong sedative, analgesic, and anti-sympathetic effect. In addition, it also protects lung by inhibiting the release of IL-6 to reduce ventilator-associated lung injury and by inhibiting endothelin-induced inflammatory reaction [8]. In the OLV, HPV is one of the body’s protective mechanisms, inducing the contraction in the small pulmonary arteries in non-ventilated part of lung, decreasing pulmonary shunt, and resulting in normalization of ventilation/perfusion ratio [5]. HPV is affected by many factors, such as body temperature, trauma, anesthesia drugs, and all of those that can inhibit the HPV increase hypoxia. Most of the current view suggests that volatile anesthetics have some degree of inhibition on HPV, in which inhibition of one-lung HPV by isoflurane is in a dose-dependent manner [9]. The results from this study showed that patients in the NISO had a significant increase in intrapulmonary shunt and decrease in PaO2 after the start of OLV; interestingly, although the DISO group also had increased pulmonary shunt and decreased PaO2, compared with NISO, the rate of increase in the shunt was gentle, so is the extent of PaO2 decrease. Reasons for this may be the following: First, Dex attenuates the local inflammation caused by hypoxic vasodilator effect in OLV; second, Dex may have a direct role in the pulmonary artery, and promote the occurrence of HPV; third, Dex, as a general anesthetic auxiliary drug, reduced the application of inhaled anesthetics, reducing its inhibition of HPV [10]; this study also showed that the continuous infusion of Dex reduced dose of isoflurane in DISO group. The above mechanisms were based solely on pathophysiologic speculations and need to be further ascertained.
Dex, as a new anesthetic adjuvant, could save the application of sedation, analgesia drugs, and reduce stress reaction; however, the main drawback is bradycardia. Researchers have reported that it may cause cardiac arrest [11]. The results from our study indicated that compared with the NISO, DISO group had significantly slower heart rates, hemodynamics in both groups remained stable, and the application of two vasoactive drugs has no significant difference. This may be explained by the fact that the depth of anesthesia was guided by BIS regulation, therefore, maintaining a stable and adequate depth of anesthesia; compared to the impact of drugs on the cycle, the impact of depth of anesthesia on the circulation may be more apparent. Thus, intravenous infusion of Dex can be safely used in one-lung ventilation.
Therefore, according to the findings and related theoretical basis, intravenous infusion of the dexmedetomidine along with isoflurane inhalation for one-lung ventilation can significantly reduce the arterial oxygen pressure drop, reducing the degree of the increase in intrapulmonary shunt, reducing isoflurane dose, and confirming its safety and feasibility in one-lung ventilation. In addition, due to the feasibility of clinical research and limitations of experimental conditions, and other factors, the study design also has certain shortcomings, such as the lack of long-term observation of the impact of the cycle of one-lung ventilation and pulmonary arterial oxygen pressure.
References
Mark Evans, A., & Ward, J. P. (2009). Hypoxic pulmonary vasoconstriction–invited article. Advances in Experimental Medicine and Biology, 648, 351–360.
Wang, J. Y., Russel, G. N., Page, R. D., et al. (1998). A comparison of the effects of sevoflurane and isoflurane on arterial oxygenation during one-lung anesthesia. British Journal Anaesthesia, 81, 850–853.
Tan, J. A., & Ho, K. M. (2010). Use of dexmedetomidine as a sedative and analgesic agent in critically ill adult patients: a meta-analysis. Intensive Care Medicine, 36, 926–939.
Zhou, S. M., Zhao, N. F., Huang, A. J., et al. (2007). Influence of general anesthesia combined with epidural block on arterial blood gas during one—lung ventilation in patients undergoing thoracic surgery. International Journal of Anaesthetic Resuscitation, 28, 342–398.
Miller RD, ed. Anesthesia for Thoracic Surgery. Amsterdam: Elsevier/Churchill Livingstone. Miller’s Anesthesia, 6th edition: 2005: 1847-1939.
Sun, Y., Feng, Y., & Yang, B. X. (2004). Effects of four different anesthetic techniques on oxygenation and intrapulmonary shunt during prolonged one-lung ventilation. Chinese Journal Anaesthesia, 24, 339–344.
Jiang, H., & Hou, Y. S. (2010). Effects of tidal volume on arterial oxygenation and intrapulmonary shunt during one lung ventilation. The Journal of Clinical Anaesthesia, 26, 206–208.
Yang, C. L., Tsai, P. S., Huang, C. J., et al. (2008). Effects of dexmedetomidine on regulating pulmonary inflammation in a rat model of ventilator-induced lung injury. Acta Anaesthesiologica Taiwanica, 46, 151–159.
Schwarzkopf, K., Schreiber, T., Bauer, R., et al. (2001). The effects of increasing concentrations of isoflurane and desflurane on pulmonary perfusion and systemic oxygenation during one-lung ventilation in pigs. Anesthesia and Analgesia, 93, 1434–1438.
Aantaa, R., Jaakola, M. L., Kallio, A., et al. (1997). Reduction of the minimum alveolar concentration of isoflurane by dexmedetomidine. Anesthesiology, 86, 1055–1060.
Nagasaka, Y., Machino, A., Fujikake, K., et al. (2009). Cardiac arrest induced by dexmedetomidine. Masui, 58, 987–989.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xia, R., Yin, H., Xia, Zy. et al. Effect of Intravenous Infusion of Dexmedetomidine Combined with Inhalation of Isoflurane on Arterial Oxygenation and Intrapulmonary Shunt During Single-Lung Ventilation. Cell Biochem Biophys 67, 1547–1550 (2013). https://doi.org/10.1007/s12013-013-9659-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-013-9659-8