Abstract
The activated renin–angiotensin–aldosterone system increases blood pressure and intracellular signals, thus leading to cardiac fibrosis. Whether increased blood pressure or angiotensin II-activated signaling is responsible for elevated angiotensin II–induced cardiac remodeling is unknown. Here, we aimed to determine whether lowering blood pressure with hydralazine might prevent inflammation and cardiac fibrosis in response to angiotensin II. We used the C57/BL6 mouse model of angiotensin II infusion (1,500 ng/kg per minute) for 7 days; 40 male mice (6 weeks old) were randomly assigned to 4 groups for treatment: mice with angiotensin II or vehicle infusion were given hydralazine in drinking water (250 mg/l per day). Heart sections were stained with hematoxylin and eosin and Masson trichrome and examined by immunohistostaining. The levels of proinflammatory cytokines were measured by real-time PCR and western blot analysis. The blood pressure of the control group began to increase on day 4 of angiotensin II infusion, and hydralazine treatment prevented angiotensin II–induced hypertension. Compared with the control, hydralazine treatment to lower blood pressure blocked angiotensin II–induced fibrosis and reduced Mac-2+ inflammatory cell infiltration and proinflammatory cytokine expression. The accumulation of blood-borne CD45+ cells and α-smooth muscle actin-positive myofibroblasts was also significantly reduced. Our results indicate that elevated blood pressure is essential for inflammatory cell infiltration and myofibroblast formation, which contribute to angiotensin II infusion–induced cardiac fibrosis. Hydralazine treatment attenuates cardiac fibrosis in response to angiotensin II. Lowering pressure could be an effective therapeutic target for cardiac fibrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Angiotensin II, the key effector of the renin–angiotensin–aldosterone system (RAAS), is an important pro-fibrotic factor [1]. Angiotensin II, acting via its AT1 receptor (AT1R), contributes to the development of hypertension primarily by activating sympathetic nerves, causing contraction of vasculature and stimulating release of aldosterone from the adrenal cortex, which in turn acts on the kidneys to increase sodium and fluid retention [2]. A large body of evidence has shown that activation of the RAAS is associated with both inflammation and interstitial fibrosis [3, 4].
The development of fibrosis is always associated with inflammation [5, 6]. The traditional view is that resident cardiac fibroblasts activated by inflammatory responses are thought to play a major role in fibrosis [7, 8]. However, recent studies describe an important role for blood-borne, monocytic fibroblast precursors that express CD34 and CD45 in angiotensin II infusion–induced or other pathological interstitial cardiac fibrosis [9]. Angiotensin II infusion results in the appearance of bone marrow-derived CD34+/CD45+ fibroblast precursor cells that express collagen type I and the cardiac fibroblast marker DDR2, whereas structural fibroblasts are CD34−/CD45− [10]. Moreover, growing evidence indicates that angiotensin II influences all stages of the inflammatory response involved in inflammatory cell recruitment and activation via AT1 and AT2 receptors [11, 12]. The importance of inflammation in fibrosis was demonstrated by reports of knockout of MCP-1 blocking ischemia/reperfusion- or angiotensin II infusion–induced cardiac fibrosis [9, 13].
Therapeutic manipulation of the renin–angiotensin system through an angiotensin-converting enzyme inhibitor (ACEI) or angiotensin II receptor blocker (ARB) to inhibit the activity of angiotensin II is effective in treating hypertension and its complications (i.e., blocking the process of cardiac remodeling) [14]. Because angiotensin II stimulates the central nervous system (sympathetic nerve) [15, 16] and multiple intracellular signaling pathways and elevates blood pressure, it is not surprising that ARB but not lowering blood pressure by hydralazine blocks flow-induced remodeling of resistance artery [17]. Moreover, lowering blood pressure with hydralazine did not prevent accelerated atherosclerosis and aortic aneurysm formation in apolipoprotein E/endothelial nitric oxide synthase double knockout animals [18]. However, in a model of mice with angiotensin II infusion, hydralazine abrogated the increase in circulating activated T cells and vascular infiltration of leukocytes caused by angiotensin II [19]. Several studies have reported that hydralazine dose-dependently lowered blood pressure in mice [19, 20].
We aimed to study whether lowering elevated blood pressure could prevent angiotensin II infusion–induced inflammation, infiltration of blood-borne CD45+ monocytic fibroblast precursor cells, and cardiac fibrosis.
Methods
Animal Model
Wild-type mice (C57/BL6) 6 weeks old were purchased from the Academy of Military Sciences (Beijing). All procedures were performed according to experimental protocols approved by the Capital Medical University Institutional Committee for Use and Care of Laboratory Animals. Male mice were randomly divided into 4 groups for treatment (n = 10 each): acetic acid saline infusion; acetic acid saline plus angiotensin II; acetic acid saline infusion with hydralazine in drinking water; and acetic acid saline plus angiotensin II with hydralazine in drinking water. The mice were anesthetized with sodium pentobarbital (50 mg/kg intraperitoneally). Angiotensin II (Sigma, St Louis, MO) was dissolved in 0.01 N sterile acetic acid saline solution. By a sterile technique, osmotic minipump (Alzet MODEL 1007D, DURECT, Cupertino, CA) filled with angiotensin II or acetic acid saline (vehicle) was placed subcutaneously in the intra-scapular area to deliver angiotensin II at an infusion rate of 1,500 ng/kg per minute for 7 days. The vasodilator hydralazine was purchased from Barr Pharmaceuticals (Montvale, NJ, USA). Pilot experiments indicated that 250 mg/l hydralazine reduced the blood pressure of C57/BL6 mice. We therefore used 250 mg/l hydralazine in drinking water for 3 days before angiotensin II infusion in all experiments.
Blood Pressure Measurement
Mice were trained daily for 3 days to have systolic blood pressure (SBP) as determined by a computerized mouse tail-cuff system (BP-98A Softron, Japan). Ten to 20 repeated values were averaged at each determination point, and SBP was determined before and at days 4–7 of the angiotensin II infusion.
Cardiac Echocardiography
Mice were anesthetized with isoflurane and analyzed for anatomy and function on a Vivid 7 Dimension cardiovascular ultrasound system with a 12-MHz microprobe (GE Healthcare, UK). Echocardiographic measurements were taken in M-mode in triplicate from all mice as described [21].
Preparation of Tissue Sections and Histopathology
Hearts were cut at the midline into transverse blocks and embedded in paraffin as reported [22]. Serial sections of 5 μm were cut and placed on polylysine-coated glass slides. Tissue sections were deparaffinized in xylene solution for 5 min, then fresh xylene solution for an additional 5 min. Sections were rehydrated by sequential incubation in 100, 95, and 70% ethanol for 5 min each at room temperature and then washed in distilled water and phosphate-buffered saline for 5 min. Heart sections were then stained with hematoxylin and eosin (H&E) and Masson’s trichrome reagent. Cardiac fibrosis was quantitated in a blinded fashion by measuring the total blue area (mm2) by use of a NIS-ELEMENTS quantitative automatic program (Nikon, Japan) in the Masson’s trichrome-stained heart sections.
Immunohistostaining
Immunohistostaining was performed as we described [23, 24]. Deparaffinized heart sections (5 μm) were incubated with avidin and biotin (Maixin, Fuzhou, China) for 15 min. After the inactivation of endogenous peroxides, sections were incubated with anti-mouse monoclonal antibodies against Mac-2 (1:400 dilution), IL-1β (1:200 dilution, both Santa Cruz Biotechnology, Santa Cruz, CA), CD45 (1:200 dilution) collagen I (1:800 dilution), and α-smooth muscle actin (α-SMA) (1:200 dilution, all Abcam, Cambridge, MA) at 4°C overnight. The sections were then incubated with biotinylated secondary antibodies for 20 min at room temperature. After being incubated with diaminobenzidine tetra hydrochloride, sections were counterstained with H&E, dehydrated through gradient alcohols, and mounted on cover slips. Images were obtained by the use of a CCD camera under a microscope (ECLIPSE80i/90i, Nikon, Japan) with a ×200 lens, and 10–20 fields/section were chosen randomly from 10 mice per group.
RNA Extraction and Real-Time PCR
Total RNA was isolated by Tri-reagent (Invitrogen) and real-time PCR was carried out as described [24, 25]. The housekeeping gene GAPDH was used as control. Primers used in the research were for collagen I, forward 5-GAGCGGAGAGTACTGGATCG-3 and reverse 5-TACTCGAACGGGAATCCATC-3; IL-1β, forward 5-CTTCAGGCAGGCAGTATCACTCAT-3 and reverse 5-TCTAATGGGAACGTCACACACCAG-3; IL-6, forward 5-CTTCCATCCAGTTGCCTTCTTG-3 and reverse 5-AATTAAGCCTCCGACTTGTGAAG; TGF-β, forward 5-CAACAATTCCTGGCGTTACCTTGG-3 and reverse 5-GAAAGCCCTGTATTCCGTCTCCTT-3; AT1R, forward 5-GTTTGCGCTTTTCATTACGAGT-3 and reverse 3-TCTTGGTTAGGCCCAGTCCT-5; AT2R, forward 5-CCACCAGCAGAAACATTACC-3 and reverse 3-GGACTCATTGGTGCCAGTT-5 and GAPDH, forward 5-CCTGGAGAAACCTGCCAAGTATGA-3 and reverse 5-TTGAAGTCACAGGAGACAACCTGG-3. Real-time PCR was carried out with the use of Bio-Rad iQ5.
Western Blot Analysis
Mice hearts were removed after angiotensin II infusion at day 7. Fresh tissue was lysed with lysis buffer [20 mM Tris (pH 7.5), 1 mM EDTA, 150 mM NaCl, 1 mM EGTA, 1 mM β-glycerophosphate, 1% Triton X-100, 2.5 mM sodium pyrophosphate, 1 mM Na3VO4, 4 μg/ml aprotinin, 4 μg/ml leupeptin, 4 μg/ml pepstatin, and 1 mM PMSF]. Western blot analysis was carried out as we described previously [26]. Eighty micrograms of tissue protein were loaded on SDS–PAGE gels, transferred to nitrocellulose membrane, and probed with primary antibodies against TGF-β (1:1,000 dilution, Santa Cruz Biotechnology), α-SMA (1:4,000 dilution, Sigma, NY), and GAPDH (1:3,000 dilution, Santa Cruz Biotechnology). Membranes were incubated with specific antibodies as described [27]. The signals were visualized by an enhanced chemiluminescence system (Amersham, Piscataway, NJ). The levels of signaling proteins were normalized to the levels of GAPDH.
Tissue Angiotensin II Concentration
Level of angiotensin II was measured by use of a radioimmunoassay (RIA) kit as reported [28]. Briefly, heart sections were homogenized with a specific inhibitor mixture. Samples were incubated with antiserum (anti-rabbit) for 6 h, then 125I-labeled angiotensin II for 18 h at 4°C. With use of donkey anti-rabbit coated cellulose in suspension, antibody-bound angiotensin II was separated from free angiotensin II. After incubation for 30 min at RT and centrifugation at 5,000 rpm for 15 min at 4°C, the concentration of angiotensin II in each sample was read with a prepared standard curve.
Plasma Renin Activity
Renin activity was measured with a commercially available RIA kit as described [29]. The blood samples were collected from the retro-orbital plexus. Plasma was incubated with rabbit angiotensinogen at 37°C for 60 min. Renin concentration was measured according to the standard protocol of the RIA kit and expressed as nanograms per milliliter per hour.
Statistical Analysis
All data are presented as mean ± SEM. Comparison between groups involved one-way ANOVA; P < 0.05 was considered statistically significant.
Results
Hydralazine Treatment Blocked Angiotensin II Infusion–Induced Increase in Blood Pressure and Left Ventricular Mass
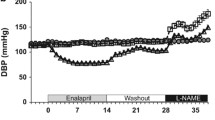
To avoid the variance in blood pressure measurement in mice caused by panic, mice were trained for 3 days before SBP was measured. As shown in Fig. 1, systolic blood pressure began to increase on day 4 of angiotensin II infusion as compared with vehicle, whereas hydralazine blocked the increase in SBP in angiotensin II-infused mice at day 6 (106 ± 9 vs. 147 ± 10, P < 0.01). Echocardiography revealed that left ventricular mass was lower after hydralazine treatment than with angiotensin II infusion (P < 0.01). However, hydralazine did not affect ejection fraction after angiotensin II infusion (Fig. 2).
Blood pressure measurement of the angiotensin II (Ang II) infusion group and hydralazine group. Hydralazine was given in drinking water at day −3 (before angiotensin II infusion), and angiotensin II infusion was on day 0. Mouse tail-cuff systemic blood pressure (SBP) was measured 3 days before and after angiotensin II infusion. Histogram shows the mean blood pressure of the 2 groups during training and during days 4–6 of angiotensin II infusion. Data represent the mean ± SEM for a group of 10 mice. *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle control group; ## P < 0.01, ### P < 0.001 vs. Ang II control group
Effect of hydralazine on the left ventricular (LV) ejection fraction in response to angiotensin II infusion. Echocardiography was performed at day 7 after angiotensin II infusion. Hydralazine treatment had no effect on LV ejection fraction after angiotensin II infusion at day 7. Data represent the mean ± SEM for a group of 10 mice. **P < 0.01 vs. vehicle control group; ## P < 0.01 vs. Ang II control group; †P < 0.05 vs. vehicle + hydralazine group
Hydralazine Lowering Blood Pressure Prevented Angiotensin II Infusion–Induced Cardiac Fibrosis
To examine the effect of lowering blood pressure on cardiac fibrosis, we harvested the hearts of each group at the end (day 7) of angiotensin II infusion and detected cardiac fibrosis using Masson’s trichrome staining. As shown in Fig. 3a, angiotensin II infusion induced significant perivascular and interstitial fibrosis, whereas hydralazine treatment markedly attenuated the angiotensin II–induced effects (P < 0.01). Cardiac fibrosis did not differ with or without hydralazine after vehicle infusion. Collagen I deposition and increased TGF-β expression are the two main factors of fibrosis (Fig. 3b–f). Angiotensin II infusion significantly increased collagen I deposition and TGF-β expression, and hydralazine suppressed these effects.
Angiotensin II infusion induces fibrosis, and hydralazine inhibits the effect. a Representative photomicrographs from histological sections of hearts stained with Masson’s trichrome at day 7 of angiotensin II infusion in each group (n = 10). With a Masson’s staining, the myocardial was stained red, while the fibrotic area was blue. Magnification: ×40 (top), ×200 (bottom). b Representative photomicrographs from histological sections of hearts undergoing immunostaining for collagen I in each group (left). The arrows indicate positive staining. Magnification: ×200 (top), ×400 (bottom). Histogram shows less collagen I positive area in the hydralazine + angiotensin II group compared with that of control (right) (n = 10). Hydralazine reduces increased mRNA level of collagen I (c) and TGF-β (d) induced by angiotensin II infusion by real-time PCR (n = 10). e Hydralazine reduces increased protein level of TGF-β induced by angiotensin II infusion. The protein levels of TGF-β and GAPDH were determined by western blot analysis, and bar graph shows densitometric analysis of intensities of TGF-β relative to that of GAPDH (n = 4). *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle control group; # P < 0.05, ## P < 0.01 vs. Ang II control group; †P < 0.05 vs. vehicle + hydralazine group. No significant differences of fibrosis area, TGF-β mRNA, and protein expression between vehicle + hydralazine group and Ang II + hydralazine group
Hydralazine Treatment Prevents Inflammatory Cell Infiltration in Angiotensin II-Infused Hearts
We and others have previously reported that inflammation plays an important role in cardiac fibrosis [9, 10]. We therefore examined the role of blood pressure lowering on infiltration of inflammatory cells in the hearts of angiotensin II-infused mice. As shown in Fig. 4a, H&E staining showed a large number of inflammatory cells infiltrated around the vasculature, with fewer inflammatory cells infiltrating with hydralazine treatment (P < 0.001). No inflammatory cell infiltration was observed without angiotensin II infusion.
Hydralazine prevents angiotensin II infusion–induced infiltration of inflammatory cells and expression of inflammatory cytokines. a Representative photomicrographs from histological sections of hearts with hematoxylin–eosin staining at day 7 of angiotensin II infusion in each group. Arrows indicate positive staining for inflammatory cells. Note infiltrated inflammatory cells have small cytoplasm and large nuclear staining. Magnification: ×100 (top), ×400 (bottom). Histogram shows less inflammatory cell infiltration in the hydralazine + angiotensin II group (n = 10). b Representative photomicrographs from histological sections of hearts immunostained with anti-Mac-2 in each group. Arrows indicate brown staining for Mac-2 positive macrophages. Magnification: ×200 (top), ×400 (bottom). Histogram shows less Mac-2-positive macrophage infiltration in the hydralazine + angiotensin II group (n = 10). c Representative photomicrographs from histological sections of hearts immunostained for IL-1β in each group. Brown areas represent secreted IL-1β. Magnification: ×200 (top), ×400 (bottom). Histogram shows less IL-1β expression in the hydralazine + angiotensin II group (n = 10). Hydralazine suppresses the increase in mRNA level of IL-1β (d) and IL-6 (e) induced by angiotensin II infusion (n = 10). *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle control group; # P < 0.05, ## P < 0.01, ### P < 0.001 vs. Ang II control group; †P < 0.05 vs. vehicle + hydralazine group. No significant differences in infiltrating cell number and IL-1β expression between vehicle + hydralazine group and Ang II + hydralazine group
Because Mac-2+ cells play an important role in transverse aortic constriction- or angiotensin II–induced fibrosis [9, 30], we then examined infiltrated inflammatory cells with anti-Mac-2 antibody (a cell surface marker of macrophage). As shown in Fig. 4b, Mac-2 immunohistostaining demonstrated macrophage infiltration of the heart prominent in angiotensin II-infused mice and markedly reduced by lowering the blood pressure with hydralazine (P < 0.001).
We next measured the expression of IL-1β and IL-6 in the heart by immunostaining and real-time PCR. As shown in Fig. 4c–e, angiotensin II infusion–induced expression of IL-1β and IL-6 was significantly suppressed by hydralazine.
Hydralazine Treatment Decreased α-SMA+ Myofibroblast Formation in Angiotensin II-Infused Heart
Previously, we showed that bone marrow, blood-borne CD45+ cells can differentiate into monocytic, fibroblast precursor cells that express α-SMA and produce collagens [9]. Therefore, we examined whether lowering blood pressure with hydralazine could prevent the accumulation of CD45+ cells in hearts. Immunohistochemical analysis revealed angiotensin II infusion–induced accumulation of CD45+ cells, and hydralazine treatment reduced the number of CD45+ cells in the hearts of angiotensin II-infused mice (Fig. 5a).
Hydralazine suppresses angiotensin II infusion–induced CD45+ cell infiltration and α-SMA-positive cell accumulation. a Representative photomicrographs from histological sections of hearts immunostained for CD45 in each group. Arrows indicate brown staining for CD45 positive cells. Magnification: ×200 (top), ×400 (bottom). b Representative photomicrographs from histological sections of hearts immunostained for α-SMA in each group. Magnification: ×200 (top), ×400 (bottom). Histogram shows that less α-SMA-positive myofibroblast formation after hydralazine treatment compared with the control (n = 10). c Hydralazine reduces increased protein level of α-SMA induced by angiotensin II infusion. The protein levels of α-SMA and GAPDH were determined by western blot analysis (left), and bar graph shows results of densitometric analysis of intensities of TGF-β relative to that of GAPDH (n = 4) (right). *P < 0.05, **P < 0.01, ***P < 0.001 vs. vehicle control group; # P < 0.05, ### P < 0.001 vs. Ang II control group, †P < 0.05 vs. vehicle + hydralazine group. No significant difference in CD45-positive cell infiltration between vehicle + hydralazine group and Ang II + hydralazine group
Myofibroblasts are characterized by the increased expression of α-SMA and are key cellular events in cardiac fibrosis and synthesis of extracellular matrix (ECM) proteins, such as collagen type I and fibronectin. To determine the effect of hydralazine treatment on myofibroblast formation, we measured the level of α-SMA in the heart sections by immunostaining and western blot analysis. As shown in Fig. 5b–c, the number of α-SMA+ cells was markedly increased in the angiotensin II infusion–induced cardiac fibrosis model, and lowering the blood pressure with hydralazine significantly reduced the proportion of myofibroblasts (P < 0.01). Myofibroblast numbers did not differ between the 2 groups after vehicle infusion.
Hydralazine Treatment Increased Plasma Renin Activity, but Made No Effect on Angiotensin AT1R and AT2R Expression and Angiotensin II Concentration in Heart Tissue
Renin–angiotensin–aldosterone system plays a critical role in hypertension and hypertensive cardiac damage via angiotensin II binding to specific receptors (AT1R and AT2R) on the cell surface. To determine whether hydralazine treatment would change RAAS effects, we measured the levels of AT1R, AT2R, and angiotensin II in heart and plasma renin activity by real-time PCR and radioimmunoassay. We found that hydralazine treatment increased plasma renin activity (Fig. 6d), but did not make any effect on the levels of AT1R and AT2R and angiotensin II concentration in heart tissue (Fig. 6a–c).
Effect of hydralazine on angiotensin II receptor expression, angiotensin II concentration, and renin activity. Hydralazine treatment did not change the mRNA levels of AT1R (a) and AT2R (b) and angiotensin II concentration in heart (c), but increased plasma renin activity (d). *P < 0.05 vs. vehicle control group; ### P < 0.001 vs. Ang II control group; †P < 0.05 vs. vehicle + hydralazine group
Discussion
Hypertension is a major risk factor for cardiovascular mortality and morbidity because it induces target organ damage on the brain, kidney, and heart [31, 32]. As a major effector of RAAS, elevated angiotensin II induces hypertension and also activates the intracellular signaling pathway, including the production of reactive oxygen species and the activation of proinflammatory transcription factors such as nuclear factor NF-κB or Egr-1, which play a key role in cardiovascular remodeling [33–35]. The deleterious effects of elevated angiotensin II may become apparent only in combinations with an increase in blood pressure [36]. However, whether the elevated blood pressure or AT1R-mediated intracellular signaling pathways are important in cardiac fibrosis is unknown.
In contrast to the use of antagonists of the angiotensin II receptor or angiotensin II production, which lower blood pressure and prevent angiotensin II receptor-mediated proinflammation, hydralazine is a direct-acting smooth muscle relaxant by acting as a vasodilator primarily in arteries and arterioles. By relaxing vascular smooth muscle, vasodilators act to decrease peripheral resistance, thereby lowering blood pressure and decreasing afterload. Hydralazine’s effect is independent of angiotensin II and is not an antagonist of the RAAS [37]. We aimed to investigate the mechanisms by which elevated angiotensin II stimulates monocytic fibroblast precursor infiltration and cardiac fibrosis and the effect of hydralazine. Hydralazine, which prevented the hypertensive response to angiotensin II infusion, blocked monocytic fibroblast precursor cell infiltration (Figs. 4, 5), and cardiac fibrosis (Fig. 3). The angiotensin II–induced cardiac fibrosis was likely a result of the blood pressure-lowering effects rather than direct actions of via its receptor-mediated inflammatory signaling pathway or activation of central nerve system. In our studies, angiotensin II infusion induced an elevated blood pressure, along with the persistent inflammation, showed as a high level of pro-inflammatory cytokines (e.g.IL-1β, IL-6, TGF-β) expression and inflammatory cells (e.g., macrophages) infiltration in hearts (Figs. 3, 4, 5). However, the cellular interaction and mechanisms of which specific type cells expressing cytokines need to be further studied. Recent studies suggested that apoptotic and necrotic cells activate macrophages and neutrophils leading to increased expression of multiple cytokines. This process may involve mitochondria damage and ROS production among necrotic cells and inflammatory cells [38].
Recently, several studies suggested that monocytic fibroblast precursor cells play an important role in cardiac fibrosis. Haudek et al. reported that ischemia/reperfusion or angiotensin II infusion resulted in the formation of distinctive small, spindle-shaped, bone marrow-derived CD34+/CD45+ fibroblasts that expressed collagen type I and the cardiac fibroblast marker DDR2, which is responsible for cardiac fibrosis [9, 10]. Prior to our present study, it was unknown whether infiltration of monocytic cells in angiotensin II–induced cardiac fibrosis was attributable to the direct effects of angiotensin II on its receptor-mediated signaling or the increase in arterial pressure. Our present results demonstrate that pressure is essential for monocytic CD45+ inflammatory cell infiltration (Fig. 5a).
Angiotensin II primarily involved in myocardial and vascular inflammation through the activation of different cell types and the secretion of cytokines and chemokines [39, 40], and the inflammation is closely associated with the process of cardiac fibrosis [41]. Our study showed that inflammation caused by angiotensin II infusion was also suppressed by lowering the blood pressure (Figs. 4, 5).
Cardiac myofibroblasts, which express α-SMA [42], can respond to proinflammatory cytokines (e.g., TNF-α, IL-1, IL-6, TGF-β, secreted by multiple of inflammatory cells) and produce collagen and fibronectin [43–45]. Our results show that hydralazine treatment decreased the α-SMA+ myofibroblast formation (Fig. 5b, c). Therefore, lowering the blood pressure in angiotensin II-infused mice suppressed the inflammation, decreased the α-SMA+ myofibroblast formation, and reduced fibrosis in the heart.
It is known that hypertension induces cardiac fibrosis, while the underlined mechanisms to cause remodeling are different in different types of arterial pressure. Recently, Marvar et al. found that angiotensin II infusion induced T-lymphocyte activation and vascular inflammation, and these effects depended on the elevated blood pressure through a central and pressor effect [19]. Similarly, in a study by Klanke et al., the expression of collagens, chemokines, adhesion molecules, and pro-fibrotic cytokines was elevated in a model of kidney of DOCA-salt sensitive rats with hypertension and decreased by hydralazine (alone with hydrochlorothiazide and reserpine to normalize blood pressure) [46]. Our conclusions that angiotensin II infusion–induced inflammation was pressure-dependent were consistent with these results.
However, in a model of spontaneously hypertensive rats for 12 weeks, Watanabe et al. found that lowering blood pressure with ARB mitigated the renal damage while hydralazine has less effect, despite the similar decrease in blood pressure [47]. Interestingly, Mario et al. found that blockade of mineralocorticoid receptors with spironolactone inhibited angiotensin II–induced aortic hypertrophy, upregulation of downstream inflammatory markers, and collagen deposition, thus preventing angiotensin II–induced cardiovascular damage. They also found that hydralazine treatment did not prevent angiotensin II–induced left ventricular interstitial collagen type I/III deposition and cardiac hypertrophy. However, hydralazine treatment prevents angiotensin II–induced cardiac fibrosis and inflammatory response [48]. In a model of rat mesenteric resistance arteries remodeling induced by chronic increase in flow, Maud Cousin et al. found that it was angiotensin-converting enzyme inhibition and angiotensin II type 1 receptor blockade that prevented mesenteric resistance arteries remodeling induced by chronic increase in flow; however, hydralazine did not prevent this remodeling, suggesting mechanisms to cause remodeling are different in different types of arterial pressure [49].
ACE2 is known to convert angiotensin II into Ang 1–7, and Ang 1–7 has a strong anti-inflammatory effect. Inhibition of ACE2 exacerbating cardiac fibrosis could be attributed to the reduced Ang 1–7 anti-inflammatory effect, which acts downstream of increasing blood pressure along with the AT1R-mediated proinflammatory pathway. Interestingly, we found that hydralazine treatment increases the level of renin in plasma (Fig. 6d), while elevated renin may drive increased levels of Ang 1–7. Ang 1–7 also stimulates the production of vasodilator nitric oxide and prostaglandins [50]. Therefore, the consequence of hydralazine treatment on angiotensin II infusion–induced fibrosis could also be mediated by potential increases in production of in Ang 1–7 which counteracts the vasoconstricting activity of angiotensin II. Our study indicates that angiotensin II infusion–induced fibrosis is blood pressure dependent. Furthermore, study by Liao et al. showed that angiotensin II infusion failed to elicit cardiac inflammation/fibrosis in CCR2−/− mice but increased blood pressure equally in wild-type and CCR2−/− mice [13], and a study of deletion of the mineralocorticoid receptors (MR) on hematopoietic cells markedly decreased cardiac fibrosis [51]. With these results, our working model is that an acute increase in blood pressure along with an AT1R-mediated proinflammatory effect stimulates vascular inflammation (e.g., production of chemokines) to recruit monocytes such as blood-borne monocytic fibroblast precursor cells; therefore, deficiency of CCR2, MR, or other inflammatory signals in monocytes will affect their ability to respond to chemokines and infiltration into the heart.
In conclusion, blood pressure is an independent risk factor for inflammation and cardiac fibrosis with elevated angiotensin II. Our results of the effects of lowering blood pressure on cardiac inflammation and fibrosis suggest that increase in blood pressure is a critical event triggering vascular damage and leading to platelet aggregation and secondary leukocyte infiltration and inflammation. Lowering blood pressure can reduce angiotensin II infusion–induced inflammation and the cardiac fibrosis.
References
Brassard, P., Amiri, F., & Schiffrin, E. L. (2005). Combined angiotensin II type 1 and type 2 receptor blockade on vascular remodeling and matrix metalloproteinases in resistance arteries. Hypertension, 46(3), 598–606.
Katragadda, S., & Arora, R. R. (2010). Role of angiotensin-converting enzyme inhibitors in vascular modulation: Beyond the hypertensive effects. American Journal of Therapeutics, 17(1), e11–e23.
Mann, D. L. (2002). Angiotensin II as an inflammatory mediator: Evolving concepts in the role of the renin angiotensin system in the failing heart. Cardiovascular Drugs and Therapy, 16(1), 7–9.
Sekiguchi, K., Li, X., Coker, M., Flesch, M., Barger, P. M., Sivasubramanian, N., et al. (2004). Cross-regulation between the renin-angiotensin system and inflammatory mediators in cardiac hypertrophy and failure. Cardiovascular Research, 63(3), 433–442.
Wynn, T. A. (2007). Common and unique mechanisms regulate fibrosis in various fibroproliferative diseases. Journal of Clinical Investigation, 117(3), 524–529.
Wynn, T. A. (2008). Cellular and molecular mechanisms of fibrosis. Journal of Pathology, 214, 199–210.
Camelliti, P., Borg, T. K., & Kohl, P. (2005). Structural and functional characterisation of cardiac fibroblasts. Cardiovascular Research, 65(1), 40–51.
Gabbiani, G. (2003). The myofibroblast in wound healing and fibrocontractive diseases. Journal of Pathology, 200(4), 500–503.
Haudek, S. B., Cheng, J., Du, J., Wang, Y., Hermosillo-Rodriguez, J., Trial, J., et al. (2010). Monocytic fibroblast precursors mediate fibrosis in angiotensin-II-induced cardiac hypertrophy. Journal of Molecular and Cellular Cardiology, 49(3), 499–507.
Haudek, S. B., Xia, Y., Huebener, P., Lee, J. M., Carlson, S., Crawford, J. R., et al. (2006). Bone marrow-derived fibroblast precursors mediate ischemic cardiomyopathy in mice. Proceedings of the National Academy of Sciences USA, 103(48), 18284–18289.
Marchesi, C., Paradis, P., & Schiffrin, E. L. (2008). Role of the renin-angiotensin system in vascular inflammation. Trends in Pharmacological Sciences, 29(7), 367–374.
Piqueras, L., Kubes, P., Alvarez, A., O’Connor, E., Issekutz, A. C., Esplugues, J. V., et al. (2000). Angiotensin II induces leukocyte-endothelial cell interactions in vivo via AT(1) and AT(2) receptor-mediated P-selectin upregulation. Circulation, 102(17), 2118–2123.
Liao, T. D., Yang, X. P., Liu, Y. H., Shesely, E. G., Cavasin, M. A., Kuziel, W. A., et al. (2008). Role of inflammation in the development of renal damage and dysfunction in angiotensin II-induced hypertension. Hypertension, 52, 256–263.
Braunwald, E., Domanski, M. J., Fowler, S. E., Geller, N. L., Gersh, B. J., Hsia, J., et al. (2004). Angiotensin-converting-enzyme inhibition in stable coronary artery disease. New England Journal of Medicine, 351(20), 2058–2068.
Zimmerman, M. C., Lazartigues, E., Sharma, R. V., & Davisson, R. L. (2004). Hypertension caused by angiotensin II infusion involves increased superoxide production in the central nervous system. Circulation Research, 95, 210–216.
Paton, J. F., Waki, H., Abdala, A. P., Dickinson, J., & Kasparov, S. (2007). Vascular-brain signaling in hypertension: Role of angiotensin II and nitric oxide. Current Hypertension Reports, 9(3), 242–247.
Cousin, M., Custaud, M. A., Baron-Menguy, C., Toutain, B., Dumont, O., Guihot, A. L., et al. (2010). Role of angiotensin II in the remodeling induced by a chronic increase in flow in rat mesenteric resistance arteries. Hypertension, 55(1), 109–115.
Chen, J., Kuhlencordt, P. J., Astern, J., Gyurko, R., & Huang, P. L. (2001). Hypertension does not account for the accelerated atherosclerosis and development of aneurysms in male apolipoprotein e/endothelial nitric oxide synthase double knockout mice. Circulation, 104(20), 2391–2394.
Marvar, P. J., Thabet, S. R., Guzik, T. J., Lob, H. E., McCann, L. A., Weyand, C., et al. (2010). Central and peripheral mechanisms of T-lymphocyte activation and vascular inflammation produced by angiotensin II-induced hypertension. Circulation Research, 107, 263–270.
Vidrio, H., Medina, M., Gonzalez-Romo, P., Lorenzana-Jimenez, M., Diaz-Arista, P., & Baeza, A. (2003). Semicarbazide-sensitive amine oxidase substrates potentiate hydralazine hypotension: Possible role of hydrogen peroxide. Journal of Pharmacology and Experimental Therapeutics, 307, 497–504.
Wang, J., Xu, N., Feng, X., Hou, N., Zhang, J., Cheng, X., et al. (2005). Targeted disruption of Smad4 in cardiomyocytes results in cardiac hypertrophy and heart failure. Circulation Research, 97(8), 821–828.
Singla, D. K., Lyons, G. E., & Kamp, T. J. (2007). Transplanted embryonic stem cells following mouse myocardial infarction inhibit apoptosis and cardiac remodeling. American Journal of Physiology Heart Circulatory Physiology, 293, H1308–H1314.
Cheng, J., & Du, J. (2007). Mechanical stretch simulates proliferation of venous smooth muscle cells through activation of the insulin-like growth factor-1 receptor. Arteriosclerosis, Thrombosis, and Vascular Biology, 27(8), 1744–1751.
Wu, X., Cheng, J., Li, P., Yang, M., Qiu, S., Liu, P., et al. (2010). Mechano-sensitive transcriptional factor Egr-1 regulates insulin-like growth factor-1 receptor expression and contributes to neointima formation in vein grafts. Arteriosclerosis, Thrombosis, and Vascular Biology, 30(3), 471–476.
Ma, Y., Zhang, L., Peng, T., Cheng, J., Taneja, S., Zhang, J., et al. (2006). Angiotensin II stimulates transcription of insulin-like growth factor I receptor in vascular smooth muscle cells: Role of nuclear factor-kappaB. Endocrinology, 147(3), 1256–1263.
Wang, W., Huang, X. R., Li, A. G., Liu, F., Li, J. H., Truong, L. D., et al. (2005). Signaling mechanism of TGF-beta1 in prevention of renal inflammation: Role of Smad7. Journal of the American Society of Nephrology, 16(5), 1371–1383.
Zhang, L., Cheng, J., Ma, Y., Thomas, W., Zhang, J., & Du, J. (2005). Dual pathways for nuclear factor kappaB activation by angiotensin II in vascular smooth muscle: Phosphorylation of p65 by IkappaB kinase and ribosomal kinase. Circulation Research, 97(10), 975–982.
Kobori, H., Ichihara, A., Suzuki, H., Takenaka, T., Miyashita, Y., Hayashi, M., et al. (1997). Role of the renin-angiotensin system in cardiac hypertrophy induced in rats by hyperthyroidism. American Journal of Physiology, 273(2 Pt 2), H593–H599.
Xu, J., Carretero, O. A., Lin, C. X., Cavasin, M. A., Shesely, E. G., Yang, J. J., et al. (2007). Role of cardiac overexpression of ANG II in the regulation of cardiac function and remodeling postmyocardial infarction. American Journal of Physiology Heart Circulatory Physiology, 293(3), H1900–H1907.
Xia, Y., Lee, K., Li, N., Corbett, D., Mendoza, L., & Frangogiannis, N. G. (2009). Characterization of the inflammatory and fibrotic response in a mouse model of cardiac pressure overload. Histochemistry and Cell Biology, 131(4), 471–481.
Lip, G. Y. (2000). Target organ damage and the prothrombotic state in hypertension. Hypertension, 36(6), 975–977.
Polichnowski, A. J., & Cowley, A. W. (2009). Pressure-induced renal injury in angiotensin II versus norepinephrine-induced hypertensive rats. Hypertension, 54, 1269–1277.
Paravicini, T. M., & Touyz, R. M. (2006). Redox signaling in hypertension. Cardiovascular Research, 71, 247–258.
Zahradka, P., Werner, J. P., Buhay, S., Litchie, B., Helwer, G., & Thomas, S. (2002). NF-kappaB activation is essential for angiotensin II-dependent proliferation and migration of vascular smooth muscle cells. Journal of Molecular and Cellular Cardiology, 34(12), 1609–1621.
Schiffrin, E. L. (2005). Vascular endothelin in hypertension. Vascular Pharmacology, 43(1), 19–29.
Danser, A. H. (2010). Cardiac angiotensin II: Does it have a function? American Journal of Physiology Heart Circulatory Physiology, 299(5), H1304–H1306.
Muller, D. N., Mervaala, E. M., Schmidt, F., Park, J. K., Dechend, R., Genersch, E., et al. (2000). Effect of bosentan on NF-kappaB, inflammation, and tissue factor in angiotensin II-induced end-organ damage. Hypertension, 36, 282–290.
Chen, G. Y., & Nunez, G. (2010). Sterile inflammation: Sensing and reacting to damage. Nature Reviews Immunology, 10, 826–837.
Brasier, A. R., Recinos, A., I. I. I., & Eledrisi, M. S. (2002). Vascular inflammation and the renin-angiotensin system. Arteriosclerosis, Thrombosis, and Vascular Biology, 22(8), 1257–1266.
Jiang, B., Xu, S., Hou, X., Pimentel, D. R., & Cohen, R. A. (2004). Angiotensin II differentially regulates interleukin-1-beta-inducible NO synthase (iNOS) and vascular cell adhesion molecule-1 (VCAM-1) expression: Role of p38 MAPK. Journal of Biological Chemistry, 279(19), 20363–20368.
Kai, H., Kuwahara, F., Tokuda, K., & Imaizumi, T. (2005). Diastolic dysfunction in hypertensive hearts: Roles of perivascular inflammation and reactive myocardial fibrosis. Hypertension Research, 28(6), 483–490.
Gabbiani, G. (1998). Evolution and clinical implications of the myofibroblast concept. Cardiovascular Research, 38(3), 545–548.
Porter, K. E., Turner, N. A., O’Regan, D. J., & Ball, S. G. (2004). Tumor necrosis factor alpha induces human atrial myofibroblast proliferation, invasion and MMP-9 secretion: Inhibition by simvastatin. Cardiovascular Research, 64(3), 507–515.
Petrov, V. V., Fagard, R. H., & Lijnen, P. J. (2002). Stimulation of collagen production by transforming growth factor-beta1 during differentiation of cardiac fibroblasts to myofibroblasts. Hypertension, 39, 258–263.
Siwik, D. A., Chang, D. L., & Colucci, W. S. (2000). Interleukin-1beta and tumor necrosis factor-alpha decrease collagen synthesis and increase matrix metalloproteinase activity in cardiac fibroblasts in vitro. Circulation Research, 86(12), 1259–1265.
Klanke, B., Cordasic, N., Hartner, A., Schmieder, R. E., Veelken, R., & Hilgers, K. F. (2008). Blood pressure versus direct mineralocorticoid effects on kidney inflammation and fibrosis in DOCA-salt hypertension. Nephrology, Dialysis, Transplantation, 23(11), 3456–3463.
Watanabe, D., Tanabe, A., Naruse, M., Morikawa, S., Ezaki, T., & Takano, K. (2009). Renoprotective effects of an angiotensin II receptor blocker in experimental model rats with hypertension and metabolic disorders. Hypertension Research, 32(9), 807–815.
Mario, F. N., Farhad, A., Agostino, V., Quy, N. D., & Ernesto, L. S. (2005). Role of aldosterone in angiotensin II-induced cardiac and aortic inflammation, fibrosis, and hypertrophy. Canadian Journal of Physiology and Pharmacology, 83, 999–1006.
Maud, C., Marc-Antoine, C., Céline, B. M., Bertrand, T., Odile, D., Anne-Laure, G., et al. (2010). Role of angiotensin II in the remodeling induced by a chronic increase in flow in rat mesenteric resistance arteries. Hypertension, 55, 109–115.
Ferrario, C. M., Chappell, M. C., Tallant, E. A., Brosnihan, K. B., & Diz, D. I. (1997). Counter regulatory actions of angiotensin-(1–7). Hypertension, 30, 535–541.
Rickard, A. J., Morgan, J., Tesch, G., Funder, J. W., Fuller, P. J., & Young, M. J. (2009). Deletion of mineralocorticoid receptors from macrophages protects against deoxycorticosterone/salt-induced cardiac fibrosis and increased blood pressure. Hypertension, 54(3), 537–543.
Acknowledgments
This project is supported by grants from National Science Foundation of China (30888004 and 81070090). Dr. Jizhong Cheng is a visiting professor from Baylor College of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qi, G., Jia, L., Li, Y. et al. Angiotensin II Infusion–Induced Inflammation, Monocytic Fibroblast Precursor Infiltration, and Cardiac Fibrosis are Pressure Dependent. Cardiovasc Toxicol 11, 157–167 (2011). https://doi.org/10.1007/s12012-011-9109-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-011-9109-z