Abstract
The ability of amiodarone to prevent pathological changes and oxidative stress after isoproterenol (ISO)-induced myocardial injury was investigated in rats. A better understanding of the processes involved in the pathophysiology of myocardial infarction has led to the search for drugs that can limit the extent of myocardial injury. Amiodarone was administered to groups of rats groups once per day for 30 days. On days 29 and 30, the rats of the ISO control and drug treatment groups were administered 180 mg/kg ISO subcutaneously at an interval of 24 h for two consecutive days. In the control groups, clinical indicators, such as creatine kinase-isoenzymes and troponin-I, were found to be statistically higher than in the drug groups. Parallel to this increase in indicators, a significant decrease in glutathione levels and activities of superoxide dismutase and an increase in malondialdehyde level were detected. Biochemical and histopathologic results in the ISO-induced model of myocardial injury emphasize the beneficial action of amiodarone as a cardioprotective agent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amiodarone {2-butyl-3-(3′;5′ diiodo-4′α-diethyl-aminoethoxy-benzoyl)-benzofuran} (AMD), one of the most effective antiarrhythmic agents, is a multiple ion (Ca++, Na+, K+) channel blocker, but it primarily inhibits K+ channels and is also a noncompetitive adrenergic antagonist that inhibits α- and β-receptors in cardiac cells. It is an effective antiarrhythmic agent and is used to treat a wide variety of ventricular and supraventricular tachyarrhythmias [1]; it is considered the gold standard for the pharmacological treatment of life-threatening ventricular tachyarrhythmias in high-risk patients [2]. This drug can also modulate phospholipid metabolism [3] and inhibit phospholipase A1, A2 and phospholipase C [4]. Phospholipase enzyme plays a role in the production of inflammatory mediators during arachidonic acid metabolism. Although amiodarone inhibits the phospholipase enzyme, blocks calcium channels, and is reported to exert antioxidant activity, antiulcerogenic activity and anti-inflammatory activity as other beneficial effects [5–7], clinical use of AMD is limited because of its potential for developing numerous adverse side effects. Of the greatest concern is amiodarone-induced pulmonary toxicity (AIPT), due to the potential for mortality. However, hepatotoxicity and other adverse effects are also of clinical importance. This drug can also modulate thyroid function and phospholipid metabolism [3].
It is now well recognized that isoproterenol (ISO), a synthetic catecholamine and β-adrenergic agonist, causes severe stress in the myocardium, resulting in infarct-like necrosis of the heart muscles and MI in supramaximal dosages [8]. The various mechanisms proposed to explain ISO-induced damage include hypoxia due to myocardial hyperactivity and coronary hypotension [9], calcium overload [10], depletion of energy reserves [11] and generation of highly cytotoxic free radical through auto-oxidation of catecholamines [12]. Free radicals are produced in cells by cellular metabolism and by exogenous agents.
A better understanding of the processes involved in the pathophysiology of MI has led to the search for drugs that can limit the extent of myocardial injury [13–15]. Proven cardioprotective and membrane stabilizing activity of many drugs in animal models of myocardial necrosis further strengthen this theory [13–15]. Drugs with multiple mechanisms of protective action, including antioxidant properties, may be one step forward in MI [12]. In this study, we chose the drug that most commonly used in the treatment of potentially fatal arrhythmias.
In evaluating the overall related literature, it is clear that there are not enough studies focusing on the effects of amiodarone on acute periods of ISO-induced myocardial injury in rats. The rat ISO-induced myocardial injury model in the present study was used to understand the role of ISO on the response of cardiac enzyme and oxidative response. The present study also determined whether amiodarone would protect against myocardial injury induced by ISO as evaluated by activities of superoxide dismutase (SOD), levels of glutathione (GSH), levels of lipid peroxidation (MDA) and histological examination of heart tissues dose dependently.
Materials and Methods
Drugs and Chemicals
Amiodarone (Cordarone, 100 mg tb) from Sanofi-Aventis-Turkey was obtained. Isoproterenol hydrochloride was purchased from Sigma Chemical (Germany). All other chemicals used were of analytical grade.
Experimental Animals
A total of 30 male Sprague–Dawley rats, weighing 180–200 g, were used in the study. The experiments were conducted according to the ethical norms approved by the Ethic Committee of Experimental Animal Teaching and Research Center. Rats were obtained from the Experimental Animal Laboratory of Medicinal and Experimental Application and Research Center, Erzurum, Turkey. They were kept in standard laboratory conditions under natural light and dark cycle. The animals were fed normal diet and water.
Experimental Protocols of Isoproterenol-Induced Myocardial Injury
In this study, a total of 30 rats were divided into five groups (n = 6 in each group); the experimental groups are summarized below:
Group 1, intact control; Group 2, ISO control; Group 3, amiodarone intact control; Group 4, ISO + amiodarone 30 mg/kg; Group 5, ISO + amiodarone 100 mg/kg.
Amiodarone 30 and 100 mg/kg were administered orally in the treatment groups once a day for 30 days. For induction of myocardial injury, we used ISO 180 mg/kg subcutaneously [16]. The intact control group (Group 1) was administered isotonic NaCl subcutaneously as a vehicle. For the myocardial injury model, on days 29 and 30 of the drug treatment, the rats of the ISO acute control (Group 2) and amiodarone (Groups 4 and 5) treatment groups were administered ISO (180 mg/kg) subcutaneously at an interval of 24 h.
Amiodarone (Group 3) was administered orally at an interval of 24 h for 30 days to healthy rats in the drug control group.
After the experimental period, the animals were killed using high-dose sodium thiopental (50 mg/kg). Blood was collected without anticoagulant for serum. Serum was separated by centrifugation. Hearts from all rat groups were removed then located on cold-ice bars. Then, definite sections of the rat hearts were separated for biochemical analyses and transferred to a −80°C refrigerator. The remaining sections of the heart tissues were transferred into 10% formaldehyde solution for histopathologic examination.
Histological Examination
The hearts were fixed in 10% formalin solution and embedded in paraffin. Sections of three different left ventricular locations measuring 4 μm were made and stained with hematoxylin and eosin (H&E) and observed microscopically. The severity and extent of MI were noted for each specimen. The pathologist was blinded to the treatment. The severity of changes was quantitated none (−) to severe (+++) based on the degree of inflammation, interstitial fibrosis, myocardial disorganization and interstitial edema. The scoring system was as follows: (0), no damage; (+), minimal inflammatory cell infiltration, focal minimal interstitial fibrosis and mild myocardial disorganization (less than 5%); (++), moderate inflammatory cell infiltration, patchy multifocal interstitial fibrosis and moderate myocardial disorganization (5–20%); (+++), widespread inflammatory cell infiltration, severe interstitial fibrosis and myocardial disorganization (more than 20%).
Biochemical Studies
Cardiac Marker Enzymes
The separated serums were used for the determination of CK-MB [17] activities with an autoanalyzer (Comas C-501) and levels of TnI [18] with another autoanalyzer (Vidas System). The measurements were expressed as U/L for CK-MB and ng/ml for TnI.
Measurements of SOD, MDA and GSH in Heart Tissue
After the macroscopic analysis, heart tissue homogenates were prepared to determine SOD enzyme activity, and the levels of GSH and lipid peroxidation were measured by the thiobarbituric assay for malondialdehyde (MDA) in all rat groups. Whole hearts of the individual rat groups were ground with liquid nitrogen in a mortar, and 0.5 g of the heart tissue was treated with 4.5 ml of appropriate buffer. The mixtures were homogenized on ice for 15 min, and the homogenates were filtered and centrifuged using a refrigerator centrifuge at 4°C. The supernatants were used in biochemical assays. All assays were carried out at room temperature in triplicate. SOD activity was measured according to Sun et al. [19], expressed as mmol/min/mg tissue. GSH was measured according to a previously reported method [20]. GSH levels in the heart tissue are expressed as nmol/g tissue. Heart tissue lipid peroxidation was determined by estimating levels of malondialdehyde (MDA) using the thiobarbituric acid test [21]. The results were expressed as nmol MDA/g tissue.
Statistical Analysis
Statistical analysis was done by one-way analysis of variance (ANOVA), followed by LSD’s multiple range test using the SPSS software package, version 12.00. P values <0.05 were considered as significant. All the results are expressed as mean ± standard deviation (SD) for six rats in each group.
Results
Histological Findings
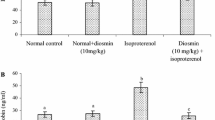
Figure 1 illustrates normal myocardial tissue in an intact control (group 1) and ISO-induced rat (group 2), respectively. Figure 2 shows sections of myocardial tissue from rats in Group 3; amiodarone intact control 100 mg/kg, Group 4; ISO + amiodarone 30 mg/kg, Group 5; ISO + amiodarone 100 mg/kg, respectively. Histological changes in heart of ISO-treated animals and after amiodarone administration were graded and summarized in Fig. 3.
Light microscopical sections of group 1 and 2. my Myocardium, i interstitium, in inflammatory cell infiltration and cm cardiac myocytes. In a normal aspect of myocardial tissue in control rat. In b acute extensive myofibrillary degeneration, which is related to infiltration with neutrophil granulocytes and interstitial edema that (marked myocardial injury) were seen in myocardial tissue of rat receiving isoproterenol only. Magnification bars: 25 μm
Light microscopical sections of group 3–5. my Myocardium, i interstitium, cm cardiac myocytes, in inflammatory cell infiltration and magnification bars: 25 μm. In a normal aspect of myocardial tissue in only amiodarone-treated rats. In b areas of focal myonecrosis, edema were seen in myocardial tissue of rat receiving amiodarone 30 mg/kg + isoproterenol. In c areas of mild myofibrillar degeneration, which is associated with interstitial edema were seen in myocardial tissue of rat receiving amiodarone 100 mg/kg + isoproterenol. Magnification bars: 25 μm
Intact Control Rat Group
In histological sections from the intact control group show the architecture of the normal cardiac tissue, normal cardiac fibers without any fraying or infarction (Fig. 1a).
ISO-Induced Rat Group
In histological analysis of the acute period of ISO-induced rat group, acute severe (+++) extensive myofibrillar degeneration, which was associated with infiltration of neutrophil granulocytes and interstitial edema (Fig. 1b). This myocardial damage was observed markedly in the subendocardial layer of the left ventricle. ISO alone-induced myocardium showed infarcted zone with edema and inflammatory cells. The myocardial fibers showed coagulative necrosis.
Amiodarone Intact Control 100 mg/kg Rat Group
Histological analysis showed the normal architecture of rat heart of amiodarone intact control group (Fig. 2a).
ISO + Amiodarone 30 mg/kg Rat Group
Treatment of amiodarone at a dose of 30 mg/kg showed areas of moderate (++) focal myonecrosis, edema with infiltration of neutrophil granulocytes (Fig. 2b).
ISO + Amiodarone 100 mg/kg Rat Group
Treatment of amiodarone at a dose of 100 mg/kg showed areas of mild (+) myofibrillar degeneration, which is associated with interstitial edema (Fig. 2c). The degree of cardiac damage exhibiting moderate and/or marked was found with higher ISO in the ISO + amiodarone 30 mg/kg rat group when compared with ISO + amiodarone 100 mg/kg rat group. One hundred milligram per kilogram of amiodarone pretreatment showed only mild edema without infarction, and the myocardial fibers were within normal limits.
Biochemical Results for CK-MB Activities TnI Levels in Serum
The effects of amiodarone (30 and 100 mg/kg) on cardiac markers CK-MB and TnI in serum in normal and ISO-induced rats are shown in Table 1. The CK-MB activity and TnI levels at acute periods after ISO-induced rats (group 2) increased significantly (P < 0.05) when compared with control group (group 1). It was found that the CK-MB enzyme and TnI level at acute treatment groups with amiodarone (group 4 and 5) decreased significantly (P < 0.05) when compared with that of acute MI group (group 2). The most decreased CK-MB activities and TnI level have shown by amiodarone 100 mg/kg + MI group when compared with amiodarone 30 mg/kg + MI. The results showed that there was no significant alteration at the CK-MB enzyme and TnI level of amiodarone control group (group 3) when compared with that of intact control group (group 1).
Results of SOD Activities in Heart Tissue
The effects of amiodarone (30 and 100 mg/kg) on the activity of the antioxidant enzyme SOD in heart tissue of ISO-induced rats are shown in Table 2. The activity of SOD in ISO-induced rats (Group 2) decreased significantly (P < 0.05) when compared with the control group (Group 1). It was found that the activity of SOD in the ISO groups pretreated with amiodarone (Groups 4 and 5) increased significantly (P < 0.05) when compared with that of the ISO control group (Group 2). The results showed that there was no significant alteration of the SOD enzyme activities of drug control groups when compared with that of the intact control group (Group 1).
Results of MDA Levels in Heart Tissue
The effects of amiodarone (30 and 100 mg/kg) on levels of MDA in heart tissue of ISO-induced rats are shown in Table 2. The levels of MDA in ISO-induced rats (Group 2) increased significantly (P < 0.05) when compared with the control group (Group 1). It was found that the level of MDA in ISO groups that were pretreated with amiodarone (Groups 4 and 5) decreased significantly (P < 0.05) when compared with that of the ISO control group (Group 2). The results showed that there was no significant alteration of the MDA level of amiodarone control group (group 3) when compared with that of intact control group (group 1).
Result of GSH Levels in Heart Tissue
The effects of amiodarone (30 and 100 mg/kg) on levels of GSH in heart tissue of ISO-induced rats are shown in Table 2. The level of GSH in ISO-induced rats (Group 2) decreased significantly (P < 0.05) when compared with the control group (Group 1). It was found that the level of GSH in ISO groups that were pretreated with amiodarone 100 mg/kg (Group 5) increased significantly (P < 0.05) when compared with that of the ISO group (Group 2). The results showed that there was no significant alteration of the MDA level of the drug control group (Group 3) when compared with that of the control group (Group 1).
Discussion
The strategies for the treatment of life-threatening MI have changed markedly over the past years. During the past decade, there has been active pharmacological research toward the development of agents that will combine the efficacy and low proarrhythmia rates of the prototype drug amiodarone. In the present study, we investigated the effects of amiodarone, a highly effective antiarrhythmic agent, on ISO-induced models of cardiotoxicity on acute ISO-induced models of cardiotoxicity in rats. Our study shows that amiodarone exhibited antioxidant effects in ISO-induced toxicity. Animals develop “myocardial infarction-like” lesions when injected with ISO, which acts through β-adrenergic receptors, stimulating calcium intracellular influx, increasing cAMP levels [22, 23] and exhausting high-energy phosphates [11]. These lesions are morphologically similar to myofibrillar degeneration, myocardial hypertrophy, myocyte damage and cardiomyopathy [16]—one of the findings described in acute myocardial infarction (MI) [24]. The studies of ISO-induced damage to the myocardium clearly demonstrate that ISO produces excessive generation of highly cytotoxic free radicals and oxidative stress in the pathology [25]. Therapeutic intervention that could improve impaired antioxidant defense mechanisms or diminish free radical production in the ischemic myocardium has been of great interest [26]. The cardiac damage markers of MI, such as CK-MB and TnI, are elevated in the serum of ISO-induced rats, which are the best markers of cardiac necrosis; these assays also have high sensitivity and specificity. This is in line with the results yielded in rats treated with ISO [27]. The increased activity of serum CK-MB observed in ISO-induced rats might be due to cardiac damage induced by ISO [28]. Thus, in the current study, the dosage of 150 mg/kg ISO was increased to produce early cardiac damage markers of MI in rats, such as CK-MB and TnI. When myocardial cells containing CK and TnI are damaged, the cell membrane becomes permeable, which results in the leakage of these products. Pretreatment with amiodarone seems to preserve structural and functional integrity of the myocardial membrane, which lowered the activity of CK-MB and level of TnI in the hearts of ISO-induced rats to near normal. This might be due to the protective effect of amiodarone on the heart, which reduced the extent of cardiac damage induced by ISO and thereby restricted the leakage of these products from the myocardium tissue when compared with the acute control MI group.
In the present study, treatment of amiodarone exhibited significant protection against ISO-induced histopathologic and biochemical changes. The cardioprotective mechanism(s) appear to be through modulation of various antioxidant/oxidant parameters, thereby improving the overall antioxidant defense of the myocardial tissue. ISO is proposed to be acting as a cardiotoxic agent via β-adrenoreceptor mechanism, which suggests that reactive oxygen-derived free radicals play a crucial role in the pathogenesis of ISO-induced myocardial injury [29–31]. The formation of free radicals in the myocardium during ISO administration might have exceeded the ability of the free radical-scavenging enzymes to dismutate the radicals, resulting in myocardial damage of the heart and reduction of scavengers [26].
Present data on GSH, SOD and MDA demonstrated that the antioxidant status of the myocardial cell in the ISO-treated group is significantly damaged. Significant decreases in GSH levels, which impaired SOD activity, together with increased MDA appears to be the initial insult to the tissue, making it more susceptible to oxidative damage. Glutathione (GSH) participates directly in the removing of hydrogen peroxides and also protects the “SH” group containing proteins from lipid peroxidation [32, 33]. GSH-dependent enzymes provide a second line of defense as they primarily detoxify the noxious by-products generated by ROS and help to prevent propagation of free radicals [34]. Decreased GSH levels observed in myocardial-infarcted rats might be due to its increased utilization in protecting SH groups containing proteins from the action of free radicals [35]. Pretreatment with amiodarone increased the concentration of GSH in ISO-treated rats during acute periods and restored the levels to near normal when compared to the acute ISO control groups. This effect may be due to the free radical-scavenging properties of amiodarone [5–7, 36].
Lipid peroxidation is an important pathogenic event that has been linked to altered membrane structure and enzyme inactivation in myocardial infarction [37]. In our current study, lipid peroxidation was measured by the thiobarbituric assay for malondialdehyde (MDA). The levels of MDA were significantly elevated with a concomitant decline in the level of reduced GSH in the heart tissue of acute periods of ISO-administered rats when compared to that of amiodarone-treated animals. Lipid peroxidation of membranes is regulated by the availability of inducers such as free radicals, and the increased levels of lipid peroxides in ISO-induced damage might be due to free radical-mediated chain reactions that could damage the myocardium [38]. Lipid peroxidation has been linked with altered membrane structure and is an indication of the severity of ISO-induced necrotic damage of the heart [39].
The elevated levels of MDA observed in ISO-treated rats might be due to comparatively low levels of antioxidant enzymes. Groups of rats that were treated with amiodarone showed reduced levels of lipid peroxidation when compared to ISO-treated rats. This shows the antilipoperoxidative effect of amiodarone. Also, the level of SOD was comparatively higher for this group. Also in our study, ISO-treated rats showed decreased activities of SOD in the heart. Superoxide dismutase reduces superoxide radical to hydrogen peroxide and oxygen. A decrease in the activity of this enzyme can lead to the formation of superoxide, which can be harmful to the myocardium [40]. The decrease in the activities of SOD and increase in the formation of superoxide might be due to myocardial cell damage.
The pathophysiological changes following ISO administration are comparable to those taking place in human myocardial alterations [41]. On histopathologic examination, the ISO 180 mg/kg group demonstrates focal myonecrosis and chronic infiltration of inflammatory cells. Marked vacuolar changes and edema were seen. One hundred milligram per kilogram of amiodarone pretreatment showed only mild edema without infarction, and the myocardial fibers were within normal limits. This indicates that amiodarone does not possess any adverse effects under normal conditions. Our data indicate that amiodarone may provide potential therapeutic value in the treatment of MI.
Conclusions
After this preliminary investigation, we conclude that ISO successfully induced cardiotoxicity in rat hearts. Biochemical and histopathologic results in the ISO-induced model of cardiotoxicity emphasize the beneficial action of amiodarone as a cardioprotective agent. The study has shown that use of pretreatment with the antiarrhythmic drug amiodarone decreases the biochemical and histopathologic injury during acute period in ISO-induced cardiotoxicity in rats dose dependently. The levels of antioxidant system enzymes superoxide dismutase and glutathione were adversely affected by cardiotoxicity. Amiodarone alleviated the adverse effects of cardiotoxicity on these enzymes and on the glutathione level. The cardioprotective properties of amiodarone could be related to its positive effects on the antioxidant system in ISO-induced cardiotoxicity in rats. However, further studies need to be carried out to ascertain whether these results can be reproduced in humans.
References
Singh, B. N. (2008). Amiodarone as paradigm for developing new drugs for atrial fibrillation. Journal of Cardiovascular Pharmacology, 52, 300–305.
Gonzalez, E. R., Kannewurf, B. S., & Ornato, J. P. (1998). Intravenous amiodarone for ventricular arrhythmias: Overview and clinical use. Resuscitation, 1, 33–42.
Vrobel, T. R., Miller, P. E., Mostow, N. D., & Rakita, L. A. (1989). General overview of amiodarone toxicity: Its prevention, detection, and management. Progress in Cardiovascular Diseases, 31, 393–426.
Wilson, B. D., Clarkson, C. E., & Lippmann, M. L. (1993). Amiodarone causes decreased cell-mediated immune responses and inhibits the phospholipase C signalling pathway. Lung, 171, 137–148.
Dengiz, G. O., Odabasoglu, F., Halici, Z., Suleyman, H., Cadirci, E., & Bayir, Y. (2007). Gastroprotective and antioxidant effects of amiodarone on indomethacin-induced gastric ulcers in rats. Archives of Pharmacal Research, 30, 1426–1434.
Dengiz, G. O., Halici, Z., Akpinar, E., Cadirci, E., Bilici, D., & Gursan, N. (2007). Role of polymorphonuclear leukocyte infiltration in the mechanism of anti-inflammatory effect of amiodarone. Pharmacological Reports, 59, 538–544.
Halici, Z., Dengiz, G. O., Odabasoglu, F., Suleyman, H., Cadirci, E., & Halici, M. (2007). Amiodarone has anti-inflammatory and anti-oxidative properties: An experimental study in rats with carrageenan-induced paw edema. European Journal of Pharmacology, 566, 215–221.
Wexler, B. C., & Greenberg, B. P. (1978). Protective effects of clofibrate on isoproterenol-induced myocardial-infarction in arteriosclerotic and non-arteriosclerotic rats. Atherosclerosis, 29, 373–395.
Yeager, J. C., & Iams, S. G. (1981). The hemodynamics of isoproterenol-induced cardiac failure in the rat. Circulatory Shock, 8, 151–163.
Bloom, S., & Davis, D. I. (1972). Calcium as mediator of isoproterenol-induced myocardial necrosis. American Journal of Pathology, 69, 459–470.
Fleckenstein, A., Janke, J., Döring, H. J., & Leder, O. (1974). Myocardial fiber necrosis due to intracellular Ca overload—A new principle in cardiac pathophysiology. Recent Advances in Studies on Cardiac Structure and Metabolism, 4, 563–580.
Sharma, M., Kishore, K., Gupta, S. K., Joshi, S., & Arya, D. S. (2001). Cardioprotective potential of ocimum sanctum in isoproterenol induced myocardial infarction in rats. Molecular and Cellular Biochemistry, 225, 75–83.
Hertog, M. G., Feskens, E. J., Hollman, P. C., Katan, M. B., & Kromhout, D. (1993). Dietary antioxidant flavonoids and risk of coronary heart-disease—The Zutphen elderly study. Lancet, 342, 1007–1011.
Gupta, S. K., Mohanty, I., Talwar, K. K., Dinda, A., Joshi, S., Bansal, P., et al. (2004). Cardioprotection from ischemia and reperfusion injury by Withania somnifera: A hemodynamic, biochemical and histopathological assessment. Molecular and Cellular Biochemistry, 3, 9–47.
Sumitra, M., Manikandan, P., Kumar, D. A., Arutselvan, N., Balakrishna, K., Manohar, B. M., et al. (2001). Experimental myocardial necrosis in rats: Role of arjunolic acid on platelet aggregation, coagulation and antioxidant status. Molecular and Cellular Biochemistry, 224, 135–142.
Rona, G., Chappel, C. I., Balazs, T., & Gaudry, R. (1959). An infarct-like myocardial lesion and other toxic manifestations produced by isoproterenol in the rat. AMA Archives of Pathology, 67, 443–455.
Lott, J. A., & Stang, J. M. (1980). Serum enzymes and isoenzymes in the diagnosis and differential diagnosis of myocardial ischemia and necrosis. Clinical Chemistry, 26, 1241–1250.
Wu, A. H., Feng, Y. J., Moore, R., Apple, F. S., McPherson, P. H., Buechler, K. F., et al. (1998). Characterization of cardiac troponin subunit release into serum after acute myocardial infarction and comparison of assays for troponin T and I. American association for clinical chemistry subcommittee on cTnI standardization. Clinical Chemistry, 44, 1198–1208.
Sun, Y., Oberley, L. W., & Li, Y. (1988). A simple method for clinical assay of superoxide-dismutase. Clinical Chemistry, 34, 497–500.
Sedlak, J., & Lindsay, R. H. (1968). Estimation of total, protein-bound, and nonprotein sulfhydryls groups in tissue with Ellman’s reagent. Analytical Biochemistry, 25, 192–205.
Ohkawa, H., Ohishi, N., & Yagi, K. (1979). Assay for lipid peroxides in animal-tissues by thiobarbituric acid reaction. Analytical Biochemistry, 95, 351–358.
Bhagat, B., Sullivan, J. M., Fischer, V. M., Nadel, E. M., & Dhalla, N. S. (1978). cAMP activity and isoproterenol induced myocardial injury in rats. Recent Advances in Studies on Cardiac Structure and Metabolism, 12, 465–470.
Dhalla, N. S., Ziegelhoffer, A., Singal, P. K., Panagia, V., & Dhillon, K. S. (1980). Subcellular changes during cardiac hypertrophy and heart failure due to bacterial endocarditis. Basic Research in Cardiology, 75, 81–91.
Karthikeyan, K., Bai, B. R., & Devaraj, S. N. (2009). Efficacy of grape seed proanthocyanidins on cardioprotection during isoproterenol-induced myocardial injury in rats. Journal of Cardiovascular Pharmacology, 53, 109–115.
Milei, J., Nunez, R. G., & Rapaport, M. (1978). Pathogenesis of isoproterenol induced myocardial lesions: Its relation to human coagulative myocytolysis. Cardiology, 63, 139–157.
Singal, P. K., Kapur, N., Dhillon, K. S., Beamish, R. E., & Dhalla, N. S. (1981). Role of free radicals in catecholamine induced cardiomyopathy. Canadian Journal of Physiology and Pharmacology, 60, 1390–1397.
Bertinchant, J. P., Robert, E., Polge, A., Marty-Double, C., Fabbro-Peray, P., Poirey, S., et al. (2000). Comparison of the diagnostic value of cardiac troponin I and T determination for detecting early myocardial damage and the relationship with histological findings after isoprenaline induced cardiac injury in rats. Clinica Chimica Acta, 298, 13–28.
Ahmed, K. K., Rana, A. C., & Dixit, V. K. (2004). Effect of Calotropis procera latex on isoproterenol induced myocardial infarction in albino rats. Phytomedicine, 11, 327–330.
Tappel, A. (1973). Lipid peroxidation and damage to cell components. Federation Proceedings, 32, 1870–1874.
Singal, P. K., Dhalla, A. K., Hill, M., & Thomas, T. P. (1993). Endogenous antioxidant changes in the myocardium in response to acute and chronic stress conditions. Molecular and Cellular Biochemistry, 129, 179–186.
Maulik, N., Engelman, D. T., Watanable, M., et al. (1995). Nitric oxide signalling in ischemic heart. Cardiovascular Research, 30, 593–601.
Martensson, J., & Meister, A. (1991). Glutathione deficiency decreases tissue ascorbate levels in new born rats: Ascorbate spares glutathione and protects. Proceedings of the National Academy of Sciences of the United States of America, 88, 4656–4660.
Halliwell, B. (1990). How to characterize a biological antioxidant? Free Radical Research, 9, 1–32.
Gumieniczek, A. (2005). Effects of rapaglinide on oxidative stres in tissues of diabetic rabbits. Diabetes Research and Clinical Practice, 68, 89–95.
Sasikumar, C. S., & Shyamaladevi, C. S. (2000). Protective effect of Abana—A polyherbal formulation, on isoproterenol induced myocardial infarction in rats. Indian Journal of Pharmacology, 32, 198–201.
Traupe, T., Keller, M., Fojtu, E., Bhattacharya, I., Lang, M., Ha, H. R., et al. (2007). Antioxidant activity and sex differences of acute vascular effects of amiodarone in advanced atherosclerosis. Journal of Cardiovascular Pharmacology, 50, 578–584.
Hamberg, M., Svensson, J., Wakabayashi, T., & Samuelsson, B. (1974). Isolation and structure of two prostaglandins endoperoxides that cause platelet aggregation. Proceedings of the National Academy of Science, 71, 345–359.
Anandan, R., Devi, K. P., Devaki, T., & Govindaraju, P. (1998). Preventive effects of Picrorhiza kurroa on D-galactosamine-induced hepatitis in rats. Journal of Clinical Biochemistry and Nutrition, 25, 87–95.
Chance, B., Sies, H., & Boveris, A. (1979). Hydroperoxide metabolism in mammalian organs. Physiological Reviews, 59, 527–605.
Liu, J., Simon, L. M., Philips, J. R., & Robin, E. D. (1977). Superoxide dismutase (SOD) activity in hypoxic mammalian systems. Journal of Applied Physiology, 42, 107–110.
Wexler, B. C. (1978). Myocardial infraction in young versus old male rats: Pathophysiological changes. American Heart Journal, 96, 70–80.
Acknowledgments
This research was conducted in the Laboratory of Pharmacology and Laboratory of Biochemistry at Ataturk University, School of Medicine, 25240 Erzurum/Turkey, and the Laboratory of Pathology, Education and Research Hospital, 25240 Erzurum/Turkey.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Albayrak, F., Bayir, Y., Halici, Z. et al. Preventive Effect of Amiodarone During Acute Period in Isoproterenol-Induced Myocardial Injury in Wistar Rats. Cardiovasc Toxicol 9, 161–168 (2009). https://doi.org/10.1007/s12012-009-9049-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12012-009-9049-z