Abstract
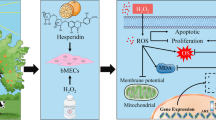
This experiment was conducted to investigate the effects and mechanism of selenium (Se) on antioxidant and immune function of bovine mammary epithelial cells (BMEC) damaged by nitric oxide (NO). The third-generation BMEC was randomly divided into eight treatments with six replicates. The BMEC in the control group was cultured in the medium without Se and diethylenetriamine/NO (DETA/NO) for 30 h. For the DETA/NO group and Se protection group BMEC were exposed to different concentrations of Se (0, 10, 20, 50, 100, 150, and 200 nmol/L) for 24 h, followed by treatment with DETA/NO (1000 μmol/L) for 6 h. Compared with the control group, DETA/NO decreased proliferation rate and activity of thioredoxin reductase (TrxR; P < 0.05). Additionally, DETA/NO decreased the gene expression of both nuclear factor-E2-related factor 2 (Nrf2) and TrxR, as well as the protein expression level of TrxR. However, the activity, and expression levels of inducible nitric oxide synthase (iNOS), as well as the concentration and gene expression level of interleukin-1β (IL-1β) and the concentration of NO significantly increased (P < 0.05). The gene expression levels of indexes related to the mitogen-activated protein kinase (MAPK) signaling pathway showed similar changes. Treatment of BMEC with Se significantly reversed DETA/NO-induced changes in a linear or quadratic dose-dependent manner (P < 0.05), with greatest benefit at 50 nmol/L. These data suggests that Se improves the antioxidant function of BMEC, and protects cells from DETA/NO-induced oxidative damage, primarily by enhancing the activity of TrxR and decreasing the concentration of NO through modulation of Nrf2 and MAPK signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introductions
Dairy cattle experience oxidative stress due to the high metabolic rate of bovine mammary epithelial cell (BMEC) during lactation. This oxidative stress leads to decreased immune function, milk production, and milk quality, and ultimately results in economic losses [1]. Our previous studies indicated that selenium (Se) treatment protects dairy cows and BMEC from oxidative damage [2, 3]; however, the exact mechanism by which Se maintains the redox state is still unclear. Nitric oxide (NO), one of the smallest known bioactive products of mammalian cells, can be produced by almost all cells and mediates several biological effects. At some concentrations, NO can have a positive physiological function; however, excessive NO formation is thought to contribute to oxidative stress and blocks antioxidant signaling pathways. Due to high metabolic requirements, dairy cows produce a great deal of NO during lactation, leading to oxidative stress and resultant cell toxicity [4]. Obata et al. indicated that activation of p38 mitogen-activated protein kinase (p38MAPK) can promote the production of tumor necrosis factor-alpha (TNF-α), interleukin-1β (IL-1β), and interleukin-6 (IL-6) in RAW 264.7 cells, resulting in the production of NO [5]. Studies of human chondrocytes indicated that selenomethionine (SeMet) inhibited gene expression of IL-1β-induced inducible nitric oxide synthase (iNOS) with corresponding reductions in NO production [6]. Ferret et al. observed an inverse correlation between cell susceptibility to NO damaging effects and thioredoxin (Trx) and Trx reductase (TrxR) expression. The correlating relation suggests that the Trx system may prevent NO-mediated cellular injury in monocytic macrophage cells [7]. Changes in the redox status of Trx activates apoptosis signal-regulating kinase-1 (ASK-1) and the MAPK pathway [8]. Previous studies from our research group demonstrated that Se can effectively improve antioxidant status and increase TrxR activity [2]. Nuclear factor-E2-related factor 2 (Nrf2) plays an important role in the regulation of the cellular Trx system, which consists of Trx and TrxR [9]. Choi et al. found that baicalein effectively enhances cellular antioxidant defense capacity through the inhibition of ROS generation, the activation of the Nrf2 signaling pathway and the increase in TrxR1 expression, which protected C6 cells from oxidative stress [10]. Therefore, our hypothesis is that Se protects BMEC from oxidative stress through upregulation of Nrf2, resulting in increased TrxR activity, which inhibits MAPK signaling pathway and prevents overproduction of NO.
An ideal exogenous NO donor to induce cell injury is diethylenetriamine (DETA)/NO [11]. Previous studies from our research group investigated the suitable condition for oxidative damage model of BMEC induced by DETA/NO [4]. The present study was carried out to investigate the protective effect of varying concentrations of Se on oxidative stress in BMEC caused by DETA/NO. Additionally, the study was designed to elucidate the underlying mechanism of the antioxidative effects of Se, and whether it was due to increased TrxR activity, and modulation to the MAPK signaling pathway resulting in downregulation of NO production.
Materials and Methods
All experiments for the projects using mammary tissues were reviewed and approved by the Animal Care and Use Committee at the Inner Mongolia Agricultural University, Hohhot, China.
BMEC Isolation and Primary Cell Culture
Mammary tissue was collected from healthy lactating Holstein cows. Samples of mammary tissue had outer layers removed and the inner tissue was placed in phosphate-buffered saline (PBS) supplemented with 300 U/mL of antibiotic-antimycotic solution. The tissues were sequentially washed three times with PBS + 300 U/mL of antibiotic-antimycotic solution, then tissues were transferred to 75% ethanol for 30 s, followed by washing three times with PBS + 100 U/mL of antibiotic-antimycotic solution. The tissues were transferred into a culture dish, trimmed, and cut into pieces the size of rice grains. Pieces of tissue that were rich with acini were transferred into a 5-mL centrifuge tube containing 0.05% collagenase type II (0.5%, Gibco BRL, Grand Island, NY) and the tissues were minced thoroughly, allowing separation of BMEC from erythrocytes. The cell suspension was incubated for 1 h at 37 °C in a CO2 constant temperature incubator (Heal Force Bio-Meditech Holdings Ltd., China) and the suspension was shaken every 20 min. The digested suspension was filtered through an 80-mesh sieve, and the dispersed cells were collected by centrifugation at 400×g for 5 min. The precipitate was resuspended in PBS and then centrifuged at 400×g for 3 min. After centrifugation, the cell pellet was resuspended in 5 mL of growth DMEM/F12 medium containing 10% fetal bovine serum (FBS) (Sigma Chemical Co., St. Louis, MO, USA); 5 μg/mL insulin transferrin Se (Sigma Chemical Co., St. Louis, MO, USA); 10 ng/mL epidermal growth factor (Sigma Chemical Co., St. Louis, MO, USA); 1 μg/mL hydrocortisone (Sigma Chemical Co., St. Louis, MO, USA); 5 μg/mL prolactin (Sigma Chemical Co., St. Louis, MO, USA); 2.5 μg/mL amphotericin B (Sigma Chemical Co., St. Louis, MO, USA); 100 IU/mL penicillin (Sigma Chemical Co., St. Louis, MO, USA), 100 μg/mL streptomycin (Sigma Chemical Co., St. Louis, MO, USA); and basal medium (15.6 g DMEM/F12 powder, 1000 mL ultra-pure water and 2.4 g sodium bicarbonate). Cell counts were determined by cytometry (ECI Inc., Yokohama, Japan). The BMEC was seeded into 25-cm2 cell culture flasks at an approximate density. The cells were then incubated in an atmosphere of 5% CO2 at 37 °C. When the confluence of BMECs reached 80 to 90%, the BMECs were subcultured twice. Third-generation BMECs were seeded at approximate densities of 1 × 104, 1 × 105, 3 × 105, and 5 × 105 cells/well into 96-well plates (200 μL per well), 6-well plates (2.5 mL per well), 60-mm culture dishes (3.5 mL per well), and 25-cm2 culture flasks (3.5 mL per flask). Cells were incubated with DMEM/F12 growth medium supplemented with 10% FBS in an atmosphere of 5% CO2 at 37 °C for 24 h. The medium was decanted when the confluence of BMECs reached 80 to 90%, and then the cells were serum starved for 24 h.
Experimental Design
After cells were serum starved for 24 h, BMECs were randomly divided into eight treatments, each containing six replicates. Group 1 was the control group (CON, cultured in medium without SeMet and DETA/NO for 30 h); group 2 was the DETA/NO treatment group (DETA/NO, pretreated with the medium without SeMet for 24 h followed by treatment with 1000 μmol/L DETA/NO for 6 h); and groups 3–8 were the Se prevention group (NSe10, NSe20, NSe50, NSe100, NSe150, NSe200), pretreated with 10, 20, 50, 100, 150, and 200 nmol/L SeMet for 24 h followed by treated with 1000 μmol/L DETA/NO for 6 h). The concentration of Met in culture medium was 115,704.69 nmol/L, and the added concentrations of Met in the SeMet-treatment groups were relatively low and same with corresponding concentrations of Se (10, 20, 50, 100, 150, and 200 nmol/L); thus, Met has little effect on this trial. The dose and processing time of DETA/NO were determined based on previous research [4].
Cell Viability Assay
Cell viability was assessed by the mitochondrion-dependent reduction of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide salt (MTT) to formazan. After the various incubation times indicated, cells in 96-well plates were exposed to 20 μL of 5 mg/mL MTT and incubated at 37 °C for 4 h. The medium was removed from each well, and 100 μL dimethyl sulfoxide (DMSO; Sigma Chemical Co., St. Louis, MO, USA) was added to lyse the cells. The 96-well plate was shaken for 10 min then analyzed with an automatic microplate reader (Synergy H4, BioTek Co., Japan) at 490 nm. Cell viability of the control group was expressed as 100%, while cell viability of the treatment group was expressed as percent (%) viability = OD treatment group/OD control group × 100.
Measurement of Antioxidant and Immune Parameters
The cell culture medium was collected in 1.5-mL centrifuge tubes and centrifuged at 10,000×g for 5 min at 4 °C. The supernatant was transferred into new tubes and stored at − 80 °C until subsequent analysis. The activities of superoxide dismutase (SOD), catalase (CAT), and total antioxidant capacity (T-AOC) were measured using commercial colorimetric assay kits (Nanjing Jiancheng Bioengineering Institute, Nanjing, China). The activities of iNOS, selenoprotein P (SelP), and the concentrations of NO, TNF-α, IL-1β, and IL-6 were analyzed using commercial ELISA kits (Neobioscience Co., Beijing, China). The absorbance was measured using a spectrophotometer at the appropriate wavelengths.
After the medium were collected, the cells in 60-mm culture dishes were scraped and lysed for 30 min in 600 μL of lysis buffer followed by centrifugation (10,000×g, 10 min, 4 °C). The supernatant was collected into 1.5-mL Eppendorf tubes and stored at − 80 °C for analysis of TrxR and glutathione peroxidases (GPx) activities and reactive oxygen species (ROS) and malondialdehyde (MDA) concentrations. Activity of GPx was measured using commercial colorimetric assay kits (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) according to the manufacturer’s instructions. The TrxR activity and ROS levels were analyzed using commercial ELISA kits (Neobioscience Co., Beijing, China). The concentration of MDA was measured using thiobarbituric acid positive reactant (TBAR) assay. The absorbance was measured using a spectrophotometer at the appropriate wavelengths.
Relative Expression of Selenoprotein mRNA in BMECs
Total RNA extraction was carried out according to the manufacturer’s instructions for the RNAiso™ Plus extraction kit (Takara Bio. Inc., Dalian, China). After the cells were cultured for 26 h in 6-well plates, the medium was decanted, plates were washed twice with PBS, and 1-mL Trizol Plus lysate was added to each well and repeatedly pipetted to ensure thorough lysis of the cells. The cell suspension was collected in 1.5-mL Eppendorf tubes. The cDNA probes were created using a PrimeScript™ reverse transcription kit (Takara Bio. Inc., Dalian, China) according to the manufacturer’s instructions. The PCR primers were designed using Oligo and Premier software using data obtained from GenBank. Relative mRNA expression of GPx1, GPx4, SelP, TrxR1, Nrf2, iNOS, IL-1β, IL-6, TNF-α, p38MAPK, c-Jun N-terminal kinase (JNK), and extracellular signal-regulated kinase (ERK1/2) in BMECs were determined by fluorescence-based real-time PCR (SYBR Green I) using a SYBR Premix Ex Taq™ kit (Takara Bio. Inc., Dalian, China), according to the manufacturer’s instructions. Housekeeping genes used were β-actin, UXT, and 18SrRNA, and the qPCR data were normalized using the geometric mean of the three internal control genes. The 2−△△Ct method was used to analyze the data. Information on primers used in the real-time quantitative PCR is described in Table 1. The PCR products were electrophoresed on 2% agarose gels (100 V, 20 min), photographed under UV light, and compared with a DNA Marker. Sequence analysis was carried out by Shanghai Sangon Biotech.
Western Blots
After the cells were cultured for 24 h in 25-cm2 culture flasks, the medium was decanted, and the culture flasks were washed twice with PBS. Cells were scraped, lysed for 5 min in RIPA lysis at 4 °C, and centrifuged (10,000×g, 10 min, 4 °C). The cell suspension was collected in 1.5-mL Eppendorf tubes and used for protein expression of related indices in cells. Protein expressions of TrxR1, GPx1, and iNOS in cells were determined using Western blotting with the internal reference gene β-actin. Cell lysates containing 30 μg of protein were boiled in 1/4 volume of 4× sample loading buffer at 95 °C for 5 min and separated on 12% SDS-PAGE with a 5% stacking gel in electrophoretic buffer. Proteins were electro transferred to a polyvinylidene fluorine membrane in electrophoresis buffer at 100 V for 50 min. The membrane was then incubated with blocking buffer for 1 h at room temperature, followed by washing three times for 2 min with PBST. The blocked membrane was then incubated with diluted polyclonal rabbit anti-β-actin (1:2000; Proteintech Co. Ltd. Shanghai, China); polyclonal rabbit anti-iNOS (1:500; Proteintech Co., Chicago, China); polyclonal rabbit anti-TrxR1 (1:500; Abcam Co., Cambridge, MA, USA); and polyclonal rabbit anti-GPx1 (1:1000; Abcam Co., Cambridge, MA, USA) overnight at 4 °C. Following overnight incubation, the membrane was washed three times for 5 min with PBST, followed by incubation with goat anti-rabbit IgG (1:1000; KPL Co., Gaithersburg, MD, USA) for 1 h at room temperature. The membrane was then washed three times for 8 min with PBST. Color development was carried out with the ECL ultra-sensitive luminescence kit according to manufacturer’s instructions. The membrane was kept in the dark for 2 min and then photographed with an ImagQuant (GE Healthcare Co., Fairfield, Connecticut, USA). The image intensity was analyzed with Quantity One software (Bio-Rad Laboratories Inc., Hercules, CA, USA), and the relative expression of the target protein was calculated (relative expression of target protein = objective protein gray value/reference protein gray value).
Statistical Analysis
Data were analyzed using the general linear model procedure of SAS software (Statistical Analysis System, Version 9.0) to test the significance of the treatment groups by regression analysis. Regression analysis was conducted to evaluate linear and quadratic effects of Se on all response criteria except for negative controls. Differences between means were determined using Duncan’s multiple comparisons to test for significance. Differences were considered to be significant when P < 0.05, and a statistical trend was indicated when 0.05 < P < 0.1.
Results
Effect of Se on the Proliferation of Cells Damaged by DETA/NO
Treatment of BMEC with 1000 μmol/L DETA/NO for 6 h resulted in a loss of cellular viability (26.10%) compared with the control cells (Fig. 1). However, the cytotoxic effect of DETA/NO was blocked by pretreatment with Se in a quadratic dose-dependent manner (P < 0.01). Cell proliferation in the NSe20, NSe50, and NSe100 group was significantly greater than that in the DETA/NO group, especially in the NSe50 group (P < 0.01).
Effects of Se on viability, antioxidant indexes, and inflammatory cytokine concentrations in NO-induced BMEC. RGR = relative growth rate. Data are expressed as the mean ± SEM. a–e Means in the treatment groups not followed by the same letter differ significantly (P < 0.05) whereas the differences were considered to be a statistical trend when 0.05 < P < 0.10
Effect of Se on the Antioxidative and Immune Parameters of Cells Damaged by DETA/NO
The activities of T-SOD, T-AOC, CAT, GPx, and TrxR, as well as the concentration of SelP significantly decreased in the DETA/NO group (P < 0.05) compared with the control group. Compared to the DETA/NO treatment group, Se treatment significantly reversed DETA/NO induced changes in a quadratic dose-dependent manner (P < 0.01). The activities of T-AOC, GPx, and TrxR in the NSe50 and NSe100 groups were significantly greater than the DETA/NO group (P < 0.05); however, there was no difference between the DETA/NO, NSe10, and NSe200 groups (P > 0.05). The activities of CAT in the NSe10, NSe20, and NSe50 groups were significantly greater than the DETA/NO group, particularly in the NSe50 group (P < 0.01). T-SOD activities in all the prevention groups were higher than that in the DETA/NO group, especially in the NSe50 group (P < 0.05). As expected, increased ROS, MDA, NO, TNF-α, IL-1β, and IL-6 generation was detected in BMECs after stimulation with DETA/NO alone (P < 0.05). Change in iNOS activity exhibited the similar pattern. However, pretreatment with 50 nmol/L Se significantly reduced DETA/NO-induced ROS and MDA production (P < 0.05). There was a significant decrease in NO concentrations and iNOS activities in the NSe10, NSe20, and NSe50 groups as compared with those in the DETA/NO group (P < 0.05), and the minimum concentration was observed at 50 nmol/L Se. TNF-α and IL-1β concentrations in the NSe20 and NSe50 groups and IL-6 concentration in the NSe100 group were lower than in the DETA/NO group; however, there was no significant change in the other Se prevention groups compared with the control group (P > 0.05) (Table 2).
Effect of Se on Gene and Protein Expressions in BMEC Damaged by DETA/NO
A significant decrease in the gene expression of Nrf2 and SelP and the gene/protein expression of GPx1 and TrxR1 was observed after 6 h of incubation with 1000 μmol/L DETA/NO compared to the control (P < 0.05). However, gene expression levels of TNF-α, IL-1β, and IL-6 as well as the gene and protein expression levels of iNOS increased dramatically in response to DETA/NO injury (P < 0.05). A similar augment was also observed in the gene expression of three mitogen-activated protein kinases (p38MAPK, JNK, ERK1/2) in DETA/NO group when compared with the control (P < 0.05). However, Se treatment significantly upregulated the gene expression of Nrf2, TrxR1, SelP, and GPx1 relative to those in DETA/NO group in a quadratic dose-dependent manner (P < 0.01), and the greatest increase in those gene expressions were in BMEC treated with 50 nmol/L Se compared with the other Se prevention groups. Changes in GPx1 and TrxR1 protein expressions exhibited the similar patterns. There was a significant decrease in IL-1β and iNOS gene expressions in the NSe20, NSe50 group as compared with those in the DETA/NO group (P < 0.05), and the minimum concentration was observed at 50 nmol/L Se. TNF-α and IL-6 gene expressions and iNOS protein expression in all the Se prevention group were significantly lower than those in the DETA/NO group (P < 0.05), especially in the NSe50 group. As we have noticed, the gene expression levels of p38MAPK (NSe10, NSe20, NSe50, NSe100, NSe150 groups) and JNK (NSe20, NSe50, NSe100, NSe150 groups) in Se-treated cells were significantly elevated with respect to those of DETA/NO in a quadratic dose-dependent manner (P < 0.05), the minimum level was observed at 50 nmol/L Se. The gene expression of ERK1/2 did not differ significantly among groups (P > 0.05) (Table 3 and Figs 2, 3, 4, 5).
Discussion
Changes in cell viability, antioxidant indices, and proinflammatory cytokine are the primary indicators of cell antioxidant and immune status. Under physiological conditions, free radicals participate in signal transduction, while excess free radicals are removed by the antioxidant defense system. Exposure to exogenous stimulus leads to the release and accumulation of large amounts of free radicals. Excessive generation of free radicals promotes DNA, protein, as well as organelle damage and triggers apoptosis as well as cytokine release [12, 13]. Cellular events occurring during oxidative stress are always associated with inflammatory responses. At the site of an acute inflammatory reaction, pro-inflammatory substances and inflammatory mediators can also induce the synthesis and release of NO [14]. Excessive production of NO leads to the formation of reactive and toxic intermediates generically termed reactive nitrogen species (RNS) [15], the blocking of signaling pathway in cells and the occurrence of uncontrolled systemic inflammation, resulting in further tissue damage. Jin et al. found that Se supplementation protected against cadmium-induced apoptosis and reduced the production of NO as well as the activity and expression of iNOS in chicken pancreas [16]. On the contrary, Se deficiency induced higher inflammatory damage in chicken intestinal tissues, which were accompanied by higher levels of iNOS and NO [17], and even led to hepatocyte apoptosis in broiler by overexpressing micro-RNA-193b-3p and increasing apoptosis-related gene expression [18], indicating that Se played protective effects against tissue damage in chickens. The study of Hua et al. showed that IL-1β induced pronounced expression of iNOS, and stimulated production of NO, leading to more aggravated inflammation [19]. The related study of murine macrophages suggested that Se decreased the expression of genes and proteins of inflammatory factors [20], which reduced the release of inflammatory factors, playing a protective role in improving the anti-oxidation and anti-inflammatory function of cells. The current results indicated that the presence of DETA/NO significantly inhibited the cell proliferation and activities of antioxidant enzymes (TrxR, GPx, SelP, SOD, CAT, T-AOC) in BMEC, but increased the release of MDA; free radicals (ROS, NO); cytokines (TNF-α, IL-1β, IL-6); and expression of iNOS, suggesting that DETA/NO induced cell oxidative damage and cytokines produced further exacerbated oxidative stress. However, the Se prevention group exhibited changes that were reversed compared to the changes associated with the parameters described above for the DETA treatment group, indicating that Se protected BMEC from DETA/NO-induced oxidative damage, but little data on the protection mechanism is available.
MAPK family consists of three types of protein kinase: p38MAPK, JNK and ERK; they can be activated by the diverse upstream kinases. An upstream kinase of the MAPK signaling pathway is apoptosis signal-regulating kinase-1 (ASK-1); therefore, a reduction in ASK-1 activity due to TrxR activity will result in the subsequent inhibition of MAPK signaling pathway [8]. Under normal circumstances, the reduced form of Trx binds to the N-terminal region of ASK-1 and inhibits kinase activity. Change in the redox status of Trx induces ASK-1 activation, and subsequent activation of the MAPK pathway. The MAPK cascade is one of the important signaling pathways in oxidative stress responses and responds to various types of stress [21]. It is said that activation of MAPK signaling pathway can induce the expression of a multitude of genes related to pro-inflammatory mediators such as chemokines, adhesion molecules, and cytokines. These pro-inflammatory mediators can regulate the expression of iNOS, which results in the release of large amounts of NO [22, 23]. The excessive release of NO activates MAPK, resulting in a positive feedback loop leading to an inflammatory response, and damage of articular chondrocytes in rabbits [24]. The addition of Se may inhibit MAPK signaling pathway by upregulating the expression of selenoprotein, resulting in downregulation of the expression of inflammatory factors. This downregulation of inflammatory factors promotes the restoration of immune homeostasis and restoration of bovine health [25]. According to the present results, DETA/NO treatment significantly decreased the activities, gene and protein expression of TrxR and GPx, while activating the p38MAPK and JNK pathways. It is important to note that the ERK1/2 pathway was not activated by the DETA/NO treatment. Most of the DETA/NO-induced changes were significantly reversed in the Se prevention group. Therefore, we inferred that the ability of Se to protect BMEC from NO-induced oxidative damage and apoptosis was due to inhibition of the MAPK signaling pathway by increased TrxR activity. The inhibition of the MAPK pathway results in decreased IL-1β, IL-6, and TNF-α concentrations, which reduced the production of NO, and the activity and expression of iNOS.
The Nrf2 pathway reduces inflammation by activating antioxidant cascades. Under homeostatic conditions the transcriptional activity of Nrf2 is suppressed by association with Kelch-like ECH-associated protein 1 (Keap1). However, under oxidative stress conditions, Nrf2 undergoes a rapid nuclear translocation, binding to electrophile response element (EpRE) and antioxidant response element (ARE). The ARE locates in the promoter regions of target antioxidant genes, which include heme oxygenase-1 (HO-1), NAD(P)H/quinone oxidoreductase 1 (NQO1), glutamate cysteine ligase catalytic subunit (GCLC), and TrxR1. Therefore, activation of the Nrf2 pathway induces the transcription of the above antioxidant genes [26]. Our results indicate that Se treatment can protect BMEC through upregulation of the Nrf2 pathway. Upregulation of the pathway resulted in increased expression and activity of TrxR, which promoted the antioxidative function of BMEC. In the current study, we did not silence the TrxR gene; therefore, the exact mechanism by which Se acts needs to be explored further.
At nutritional concentrations, Se can promote cell proliferation and enhance antioxidant ability and immune function. However, excessive Se results in decreased immunity, increased oxidative damage, and a series of clinical pathology changes [27]. Based on our results, the protective effect of Se is related to dose; where 10 nmol/L Se had no significant protective effects, while 20–100 nmol/L Se had some protective effects. The greatest antioxidant effect was observed when Se was included at 50 nmol/L. At Se concentrations greater than 50 nmol/L, the antioxidant effect appeared to plateau, or decrease; particularly at 200 nmol/L, where no protective effect was observed, and cell damage was occurring. The cell damage was likely caused by Se toxicity, which can damage the cellular membrane and proteins due to Se-generated ROS [28, 29]. One of the main mechanisms of Se toxicity that has been hypothesized is that sulfur components of proteins are being substituted with Se, which disrupts trace mineral balance [28]. Still another route to SeMet toxicity could be the replacement of Met by SeMet which may influence the activity of enzymes if SeMet replaces Met in the vicinity of the active site [30]. This substitution may interrupt metabolic pathways and cascades in the organism, leading to metal disruption and increased oxidative stress [31]. Moderate concentrations of selenium can be stored in the organism and are used to maintain homeostatic functions. Due to the narrow concentration range between essentiality and toxicity, Se represents an important toxicological hazard [32]. Potentially toxic dietary concentrations in ruminant feeds are considered to be 2 to 5 ppm, which is about 10- to 20-fold greater than dietary levels considered to be adequate [33]. Therefore, appropriate addition of Se is the basic prerequisite in order to obtain antioxidant and anti-inflammatory effects of Se, without toxicity occurring.
The addition of Se improves the antioxidant function of BMEC and protects cells from oxidative damage induced by DETA/NO. This is the result of upregulation of Nrf2, enhancing the activity of TrxR, which inhibiting the activation of MAPK signaling pathway. The inhibition of MAPK signaling pathway results in decreased concentrations of NO. Optimal Se dose is at 50 nmol/L, but antioxidant effects are observed when Se is included at 20 to 100 nmol/L. Greater concentrations of Se can cause damage to cells due to Se toxicity.
References
Sordillo LM, Aitken SL (2009) Impact of oxidative stress on the health and immune function of dairy cattle. Vet Immunol Immunopathol 128:104–109
Gong J, Ni L, Wang D, Shi BL, Yan SM (2014) Effect of dietary organic selenium on milk selenium concentration and antioxidant and immune status in midlactation dairy cows. Livest Sci 170:84–90
Guo YM, Yan SM, Gong J, Jin L, Shi BL (2017) The protective effect of selenium on bovine mammary epithelial cell injury caused by depression of thioredoxin reductase. Biol Trace Elem Res 2017:1–8
Guo YM, Zhang BQ, Shi HY, Yan SM, Shi BL, Guo XY (2016) Establishment of oxidative damage model of bovine mammary epithelial cells induced by diethylenetriamine/nitric oxide adduct. J Anim Sci 28:2378–2384 In Chinese
Obata T, Brown GE, Yaffe MB (2000) MAP kinase pathways activated by stress: the p38 MAPK pathway. Crit Care Med 28:N67–N77
Cheng AWM, Stabler TV, Bolognesi M, Kraus VB (2009) Selenomethionine inhibits IL-1β inducible nitric oxide synthase (iNOS) and cyclooxygenase 2 (COX2) expression in primary human chondrocytes. Osteoarthr Cartil 17:118–125
Ferret PJ, Soum E, Negre O, Wollman EE, Fradelizi D (2000) Protective effect of thioredoxin upon NO-mediated cell injury in THP1 monocytic human cells. Biochem J 346:759–765
Soga M, Matsuzawa A, Ichijo H (2012) Oxidative stress-induced diseases via the ASK1 signaling pathway. Int J Cell B 2012:439587
Sakurai A, Nishimoto M, Himeno S, Imura N, Tsujimoto M, Kunimoto M, Hara S (2005) Transcriptional regulation of thioredoxin reductase 1 expression by cadmium in vascular endothelial cells: role of NF-E2-related factor-2. J Cell Physiol 203:529–537
Choi EO, Jeong JW, Park C, Hong SH, Kim GY, Hwang HG, Cho EJ, Choi TH (2016) Baicalein protects C6 glial cells against hydrogen peroxide-induced oxidative stress and apoptosis through regulation of the Nrf2 signaling pathway. Int J Mol Med 37:798–806
Keefer LK, Nims RW, Davies KM, Wink DA (1996) “NONOates” (1-substituted diazen-1-ium-1,2-diolates) as nitric oxide donors: convenient nitric oxide dosage forms. Methods Enzymol 268:281
Mo C, Wang L, Zhang J, Numazawa S, Tang H, Tang XQ, Han XJ, Li JH, Yang M, Wang Z, Wei DD, Xiao HG (2014) The crosstalk between Nrf2 and AMPK signal pathways is important for the anti-inflammatory effect of berberine in LPS-stimulated macrophages and endotoxin-shocked mice. Antioxid Redox Signal 20:574–588
Kunz A, Dirnagl U, Mergenthaler P (2010) Acute pathophysiological processes after ischaemic and traumatic brain injury. Best Pract Res Clin Anaesthesiol 24:495–509
Pacher P, Beckman JS, Liaudet L (2007) Nitric oxide and peroxynitrite in health and disease. Physiol Rev 87:315–424
Wissel J, Kaňovský P, Růžička E, Bares M, Hortova H, Streitova H, Jech R, Roth J, Brenneis C, Müller J, Schnider P, Auff E, Richardson A, Poewe W (2012) Efficacy and safety of standardised 500 unit dose of dysport (Clostridium botulinum toxin type a haemaglutinin compplex) in a heterogenous cervical dystonia popupation: results of a prospective, multicentre, randomised, double-blind, placebo-controlled, parallel group study. Antioxid Redox Signal 17:992–1012
Jin X, Jia T, Liu R, Xu S (2018) The antagonistic effect of selenium on cadmium-induced apoptosis via PPAR-γ/PI3K/Akt pathway in chicken pancreas. J Hazard Mater 357:355–362
Yu J, Yao H, Gao X, Zhang Z, Wang JF, Xu SW (2015) The role of nitric oxide and oxidative stress in intestinal damage induced by selenium deficiency in chickens. Biol Trace Elem Res 163(1–2):144–153
Liu T, Yang T, Xu Z, Tan S, Pan T, Wan N, Li S (2018) MicroRNA-193b-3p regulates hepatocyte apoptosis in selenium-deficient broilers by targeting MAML1. J Inorg Biochem 186:235–245
Hua WB, Zhang YK, Wu XH, Kang L, Tu J, Zhao KC, Li S, Wang K, Song Y, Luo RJ, Shao ZW, Yang SH, Yang C (2017) Icariin attenuates interleukin-1β-induced inflammatory response in human nucleus pulposus cells. Curr Pharm Des 23
Kim SH, Johnson VJ, Shin TY, Shin TY, Sharma RP (2004) Selenium attenuates lipopolysaccharide-induced oxidative stress responses through modulation of p38 MAPK and NF-kappaB signaling pathways. Exp Biol Med 229:203–213
Korbecki J, Baranowskabosiacka I, Gutowska I, Chlubek D (2013) The effect of reactive oxygen species on the synthesis of prostanoids from arachidonic acid. J Physiol Pharmacol 64:409
Karrasch T, Jobin C (2008) NF-kappaB and the intestine: friend or foe? Inflamm Bowel Dis 14:114–124
Xu LK, Wang XM, Tan XM, Xing XF, Tang QF, Luo JB (2017) Ephedra-cinnamomi attenuates cerebral ischemia-induced memory deficits via TLR4/MyD88/p38 MAPK pathway. Biomed Res 28:8309–8315
Wang H, Wang Z, Chen J, Wu J (2007) Apoptosis induced by NO via phosphorylation of p38 MAPK that stimulates NF-κB, p53 and caspase-3 activation in rabbit articular chondrocytes. Cell Biol Int 31:1027–1035
Zhang W, Zhang R, Wang T, Jiang H, Guo M, Zhou E, Yong S, Yang Z, Xu S, Cao Y, Zhang N (2014) Selenium inhibits LPS-induced pro-inflammatory gene expression by modulating MAPK and NF-κB signaling pathways in mouse mammary epithelial cells in primary culture. Inflammation 37(2):478–485
Lee SE, Son GW, Park HR, Jin YH, Park CS, Park YS (2015) Induction of thioredoxin reductase 1 by crotonaldehyde as an adaptive mechanism in human endothelial cells. Mol Cell Toxicol 11:433–439
Wang YC, Jiang L, Li YF, Luo XG, He J (2016) Effect of different selenium supplementation levels on oxidative stress, cytokines, and immunotoxicity in chicken thymus. Biol Trace Elem Res 172:488–495
Spallholz JE, Hoffman DJ (2002) Selenium toxicity: cause and effects in aquatic birds. Aquat Toxicol 57:27–37
Silva MAOD, Andrade SALD, Mazzafera P, Arruda MAZ (2011) Evaluation of sunflower metabolism from zinc and selenium addition to the culture: a comparative metallomic study. Int J Mass Spectrom 307:55–60
Schrauzer GN (2000) Selenomethionine: a review of its nutritional significance, metabolism and toxicity. J Nutr 130(7):1653–1656
Hauser-Davis RA, Silva JAN, Rocha RCC, Pierre TS, Ziolli RL, Arruda MAZ (2015) Acute selenium selenite exposure effects on oxidative stress biomarkers and essential metals and trace-elements in the model organism zebrafish (Danio rerio). J Trace Elem Med Biol 33:68
Tuzen M, Pekiner OZ (2015) Ultrasound-assisted ionic liquid dispersive liquid-liquid microextraction combined with graphite furnace atomic absorption spectrometric for selenium speciation in foods and beverages. Food Chem 188:619–624
Hafla A (2015) Micro-Minerals: selenium. Agri-King Web. https://www.agriking.com/micro-minerals-selenium/. Accessed 8 January 2015
Acknowledgments
Yongmei Guo and Xiaoyu Guo contributed equally to this article. The authors are also grateful to Boqi Zhang for his assistance during the experiments and to Dr. Christine Rosser for her modification to this manuscript.
Funding
The authors acknowledge the support of the National Natural Science Foundation of China (Project No. 31560650).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guo, Y., Guo, X., Yan, S. et al. Mechanism Underlying the Protective Effect of Selenium on NO-Induced Oxidative Damage in Bovine Mammary Epithelial Cells. Biol Trace Elem Res 191, 104–114 (2019). https://doi.org/10.1007/s12011-018-1603-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-018-1603-8