Abstract
Boron, a vital micronutrient for plant metabolism, is not fully elucidated for embryonic and adult body development, and tissue regeneration. Although optimized amount of boron supplement has been shown to be essential for normal gestational development in zebrafish and frog and beneficial for bone regeneration in higher animals, effects of boron on myogenesis and myo-regeneration remains to be solved. In the current study, we investigated dose-dependent activity of boric acid on myogenic differentiation of human adipose-derived stem cells (hADSCs) using immunocytochemical, gene, and protein expression analysis. The results revealed that while low- (81.9 μM) and high-dose (819.6 μM) boron treatment increased myogenic gene expression levels such as myosin heavy chain (MYH), MyoD, myogenin, and desmin at day 4 of differentiation, high-dose treatment decreased myogenic-related gene and protein levels at day 21 of differentiation, confirmed by immunocytochemical analysis. The findings of the study present not only an understanding of boron’s effect on myogenic differentiation but also an opportunity for the development of scaffolds to be used in skeletal tissue engineering and supplements for embryonic muscle growth. However, fine dose tuning and treatment period arranging are highly warranted as boron treatment over required concentrations and time might result in detrimental outcomes to myogenesis and myo-regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Boron, a widely distributed semi-metal in nature, has been known to be essential for plants since 1925, but its biological roles in plants have recently been defined. Apart from plants, boron has also been claimed to be a beneficial element for animals and quite likely humans for bone regeneration, while the exact molecular mechanisms remain to be solved. A wide array of physiological and metabolic systems (lipid, mineral, bone, energy metabolism, and endocrine function) of the mammalian body are significantly affected by boron deprivation [1–6]. Furthermore, boron is involved in bone growth and maintenance, brain function, and reduces arthritis risk, regulates some steroid hormones, and coordinates immune response [7].
Besides all positive attributes, elevated levels of boron have occasionally deleterious outcomes. Recent studies reported that high amount of dietary boron intake may result in reproductive (26 mg boron/kg) and developmental (248 mg boric acid/kg) failure [8, 9]. Moreover, as it has been given in high doses (1000 mg boric acid/kg), accumulation of boron in various organs and tissues, including the muscle, bone, brain, liver, kidney, hypothalamus, blood, lymph node, prostate, and adrenal tissue has led to detrimental consequences such as edema, inflammation, unhealthy weight gain, irregular calcium metabolism, poor quality sperm production, defective ovarian development, and alopecia [10]. At the molecular level, significant reduction in glucose, lactic acid, glycogen, and ATP concentrations has been reported due to high-dose boron exposure and subsequent structural failure of mitochondrion in pectoral fiber has been observed. Although lack of boron in embryonic development has resulted in high mortality and malformations in embryos of frogs and zebrafish [7], excessive boron exposure has also come up with severe defects in early embryonic development and increased fetus mortality. However, these in vivo studies have not revealed the molecular mechanism of boron’s contribution and toxicity for the developmental stage yet.
The ability to harvest stem cells with multilineage differentiation capacity from embryo and adult body offers new possibilities to study different regulators and molecular mechanisms involved in embryonic development and tissue repair in in vitro conditions. Along with understanding molecular pathway, emergence of this unique era allows scientist to develop new drugs and supplements for tissue regeneration and fetal development rapidly and effectively. In this line, the most prominent and well-observed effect of boron on bone and teeth growth has been elucidated using in vitro approaches in which adult progenitor and mesenchymal stem cells has been differentiated into osteogenic cell lineage in the presence of boron [11–13]. Discovering positive contributions of such additives in in vitro would direct scientist to develop biocompatible and bioinductive scaffold system to be used in regenerative medicine. However, boron derivatives (even boric acid) have not been studied for myogenic stem cell differentiation to address possible roles and effects of boron in muscle regeneration and development. In the current study, we showed the effects of different concentrations of boric acid on myogenic cell transformation of human adipose-derived stem cells (hADSCs) using protein and gene expression analysis.
Materials and Methods
Isolation and Characterization
Human adipose tissue was obtained from a lipoaspirate of a 45-year-old female patient under local anesthesia. Ethical approval was obtained from the Ethics Committee, University of Acıbadem (decision no. 2013–529), and informed consent was received from the patient. Stromal vascular fraction (SVF) was separated from the raw lipoaspirate tissue according to the previously described protocol with slight modifications [14]. Briefly, adipose tissue was washed with phosphate-buffered saline (Invitrogen, UK) and minced with a scalpel into small pieces followed by a 40-min incubation at 37 °C in 0.2 % collagenase type II solution. Enzyme activity was stopped by adding equal volume of Dulbecco’s modified Eagle’s medium (DMEM) (Invitrogen, Carlsbad, CA) containing 10 % fetal bovine serum (FBS) and 1 % penicillin, streptomycin, and amphotericin (PSA) and the mixture was centrifuged at 300 g for 10 min. SVF pellet was resuspended in red blood cell (RBC) lysis buffer for 5 min and centrifuged again at 300 g for 10 min. Cell pellet was plated into cell culture plates (TPP, Switzerland) and incubated in a humidified incubator at 37 °C and 5 % CO2 atmosphere. The next day, nonadherent red blood cells were removed by subsequent phosphate-buffered saline (PBS) wash. After enough confluence was reached (80 %), human adipose-derived stem cell (hADSC) characterization was conducted as described previously [15]. Cells were removed from flasks with trypsin-ethylenediaminetraacetic acid (Invitrogen, Paisley, UK) and incubated with primary antibodies diluted in PBS for 1 h. Primary antibodies against CD14 (ab82434), CD29 (ab27314), CD34 (ab18227), CD45 (ab134202), CD90 (ab95700), CD105 (ab53321) and CD73 (ab157335) (Abcam, UK), and CD166 (sc-53551, Santa Cruz Biotechnology Inc, CA) were used. CD29, CD73, CD90, CD105, and CD 166 were used as positive cell surface markers, and CD14, CD34, and CD45 were used as negative cell surface markers. The flow cytometry analysis of cells was completed using a Becton Dickinson FACS Calibur (Becton Dickinson, San Jose, CA) flow cytometry system. Characterized cells were then differentiated into adipo-, chondro-, and osteogenic lineages to confirm mesenchymal stem cell (MSC) properties as described previously [16]. Briefly, cells were seeded on six well plates at a cell density of 5 × 104 cells/well. Cells were cultured with differentiation media specific to adipo- chondro-, and osteogenic transformation for 10 days in a humidified incubator at 37 °C and 5 % CO2 atmosphere. Differentiation media contents are shown in Table 1. All experiments were repeated three times.
Staining Assays
Cells were stained with von Kossa, Alcian Blue, and oil red to visualize osteo-, chondro-, and adipogenic characteristics of hADSCs, respectively. Cells were fixed with 2 % (w/v) paraformaldehyde for 30 min. Calcium depositions were identified by using von Kossa kit (Polysciences, Inc., Germany) according to the manufacturer’s recommendations. After chondrogenic differentiation, cells were stained with Alcian Blue staining solution for 30 min. To detect lipid droplets, adipogenically differentiated cells were treated with oil red O for 10 min. Prepared samples were observed under an invert light microscope (Zeiss Primo Vert, Göttingen, Germany).
Preparation of Boric Acid Solution
Boric acid was purchased from Biobasic Inc. (10043-35-3). Main stock solution was prepared in the culture medium (DMEM containing 10 % FBS and 1 % PSA) at a concentration of 10 mg/ml (163.9 mM). The stock solution was filtered through a 0.22-μm filter (Sartorius AG, Göttingen, Germany) and subsequently diluted to lower concentrations in culture medium for further analysis.
Cytotoxicity Assay
Eleven separate concentrations between 5 and 2000 μg/ml (5, 10, 20, 50, 100, 200, 250, 500, 700, 1000, 2000 μg/ml) of boric acid were prepared in culture medium. Culture medium was used as negative control (NC) for standard growth conditions and 20 % dimethyl sulfoxide (DMSO, Fisher Scientific, NJ) prepared in DMEM was used as positive control (PC). hADSCs (passage 3) were seeded onto 96-well plates (Corning Glasswork, Corning, NY) at a cell density of 3 × 103 cells/well. Cell viability was measured by the 3-(4,5-di-methyl-thiazol-2-yl)-5-(3-carboxy-methoxy-phenyl)-2-(4-sulfo-phenyl)-2H-tetrazolium (MTS)-assay (CellTiter96 AqueousOne Solution; Promega, Southampton, UK) according to the manufacturer’s instructions. Briefly, following the incubation periods of 24, 48, and 72 h, 10 μL of MTS reagent in 100 μL of growth medium was added to each well, and the plate was incubated for 2 h at 37 °C. Absorbance at 490 nm was detected using ELISA plate reader (Biotek, Winooski, VT).
Myogenic Differentiation of hADSCs
hADSCs were induced to differentiate into myogenic-like cells in the presence of boric acid as described previously [17]. Cells were seeded onto six well plates at a cell density of 5 × 104 cells/well. After 24 h, 5 (81.9 μM) and 50 μg/ml (819.6 μM) boric acid-containing differentiation media were added to respective wells and the media were changed every 3 days for 21 days. Differentiation media without boric acid supplement was used as negative control in all myogenic differentiation experiments for 21 days. Experiments were terminated at different time intervals (4–7 and 14–21 days) to observe the possible effects of boric acid in a time-dependent manner.
Immunocytochemistry Analysis
Immunocytochemistry assay was performed according to the protocol described previously [18]. Briefly, fixed cells were incubated with the primary antibodies against MyoD (sc-760), myosin heavy chain (MYH) (sc-20641), and α-smooth muscle actin (α-SMA) (ab5694) overnight at 4 °C. After labeling, cells were washed with PBS to remove unbound primary antibodies and subsequently incubated with AlexaFluor-488 goat anti-rabbit immunoglobulin G (Invitrogen, Carlsbad, USA) secondary antibody for 1 h at 4 °C. Cell nuclei were stained with diluted (1:1000) 4′,6-di-amidino-2-phenyl-indole (DAPI) (Applichem, Darmstadt, Germany). Stained cells were observed under a confocal microscope (LSM 700, Zeiss, Heidelberg, Germany). Fatty acid binding protein 4 (FABP4, #2120, Cell Signaling), collagen type II (Col II, sc-59772), and Osteocalcin (sc-30044) primary antibodies were used for characterization of hADSCs after osteo-, chondro-, and adipogenic differentiation of cells.
Real-Time PCR Analysis
Total RNAs from myogenically differentiated samples were isolated using High Pure RNA-isolation kit (Ambion, USA) according to the manufacturer’s suggestions. cDNA was synthesized by using High Fidelity cDNA Synthesis Kit (Roche, USA). Real-time (RT)-PCR using SYBR Green was utilized to quantify mRNA levels of targeted genes. cDNAs were mixed with primers and SYBR Premix (Applied Biosystem, UK) in a final volume of 20 μl. Sequences of primer used for RT-PCR analyses were shown in Table 2. The β-actin gene was used for normalization of data. All RT-PCR experiments were performed using iCycler RT-PCR system (Bio-Rad, CFX Real Time System, Singapore).
Western Blot Analysis
Total protein was isolated from myogenically differentiated cells using RIPA Buffer (Santa Cruz, USA). BCA protein assay (Thermo Scientific, USA) was used to determine protein concentration. Protein samples were loaded to the 10 % sodium dodecylsulfate-polyacrylamide gel at 30 μg/lane and transferred to polyvinylidene fluoride membranes. Membranes were then incubated with primary antibodies (dilution 1:1000) at 4 °C. After washing with tris-buffered saline and Tween 20 (TBST), membranes were incubated with secondary antibodies (HRP-conjugated) prepared in TBST for 1 h. β-actin antibody (#8884, dilution 1:1000, Cell Signaling Technology, MA) was used as control for normalization of results and images were taken by using the luminometer system (Bio-Rad). Band intensity was quantified by densitometric analysis using the image analysis system Image J (NIH, Bethesda, USA). Results were represented as fold change of control.
Statistical Analysis
The data were statistically analyzed using one-way analysis of variance by using Graph-PadPrism5 (GraphPad, LaJolla, CA) software. Differences were considered to be significantly different at P < 0.05.
Results
Isolation and Characterization of hADSCs
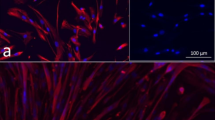
hADSCs which were successfully isolated and expanded from lipoaspirate tissues showed fibroblast-like cell morphology (Fig. 1a). Isolated cells at passage 3 were characterized for their mesenchymal stem cell (MSC) surface markers using flow cytometry analysis. Flow cytometry results revealed that hADSCs were positive for MSCs surface antigens (CD29, CD73, CD90, CD105, and CD166) and negative for hematopoietic markers (CD34, CD45, and CD14) (Fig. 1b). Differentiation assays confirmed that hADSCs could effectively differentiate into osteo-, adipo-, and chondrogenic cell types. Cells were positively immunostained with osteocalcin and calcium depositions were showed with von Kossa after osteogenic differentiation. Chondrogenic transformation was confirmed by Alcian Blue staining and Col II immunostaining. Lipid droplets were positively stained with oil red and FABP4, indicating the adipogenic transformation (Fig. 1c).
Characterization of human adipose-derived stem cells (hADSCs). a Fibroblast-like cell morphology of hADSCs, scale bar 400 μm. b hADSCs were found to be positive for mesenchymal stem cell surface markers (CD29, CD73, CD90, CD105, and CD 166), and negative for hematopoietic stem cell surface markers (CD14, CD34, and CD45). c von Kossa (scale bar 200 μm), Alcian Blue (scale bar 50 μm), and oil red (scale bar 200 μm) stainings proved differentiation capacity of hADSCs to mesenchymal cell lineages. In addition, osteo-, chondro- and adipogenic differentiation potential of hADSCs were confirmed by immunocytochemistrical analysis for osteocalcin, collagen type II and FABP4, respectively, scale bar 50 μm
Cell Viability Analysis
The impact of various boric acid concentrations on hADSCs viability was tested for 3 days (24, 48, and 72 h). No cytotoxicity was observed for any boric acid concentrations (Supplementary Figure 1). Five and 50 μg/ml boric acid concentrations were chosen for myogenic differentiation experiments to show effects of low and high dose of boron on hADSCs during differentiation procedure. Cell viability analysis for 21 days by using these two concentrations was completed to show whether they have toxic effect on myogenically differentiated cells (Fig. 2a). The results revealed that 5 and 50 μg/ml of boric acid significantly increased cell viability and did not exert any cytotoxicity.
a Cytotoxicity of boric acid treatment on human adipose-derived stem cells (hADSCs) during myogenic differentiation at day 4, 7, 14, and 21, *P < 0.05. b Morphologies of myogenically differentiated hADSCs in the presence and absence of boric acid, scale bar 50 μm. c Immunocytochemistrical analysis for MYH, MyoD, and α-SMA at day 4 and 21. Control only differentiated medium-treated cells, 5 μg/ml and 50 μg/ml indicated boron concentrations containing differentiation medium-treated cells, MYH myosin heavy chain, α-SMA alpha-smooth muscle actin
Differentiation and Immunocytochemistry Analysis
Adherent hADSCs differentiated into myogenic cells, grew larger, and gained muscle like fibrillar morphology after 21 days in all groups (Fig. 2b). In order to confirm myogenic differentiation of hADSCs treated with 5 and 50 μg/ml boric acid, immunocytochemical analysis for MyoD, MYH, and α-SMA monoclonal antibodies were conducted. Figure 2c shows the positive MyoD, MYH, and α-SMA staining of transformed cells; 50 μg/ml boric acid application exhibited slight decrease in protein expression for MyoD and α-SMA compared to the control and 5 μg/ml boric acid-treated groups.
RT-PCR analysis
Myogenic differentiation of hADSCs was analyzed by RT-PCR analysis in samples collected at different time intervals (4–21 days). While boric acid treatment (both low and high concentrations) increased myocyte-specific mRNA expression levels in the early stage of differentiation process; longer incubation times result in sharp decrease in mRNA levels especially for 50 μg/ml boric acid-treated cells. Boric acid application (5 μg/ml) significantly increased the MYH, MyoD, myogenin (MYOG), desmin, and α-SMA gene expression levels at day 4. However, mRNA levels of genes (except MYH) in 5 μg/ml boric acid-treated cells were not significantly different from those of control cells at day 21. Although downregulation of MYH, MyoD, and desmin genes was observed at day 21 in 50 μg/ml boric acid-treated cells, MYOG and α-SMA gene levels were not significantly different among the experimental groups (Fig.3).
mRNA levels of myogenic marker genes in boric acid-treated human adipose-derived stem cells at day 4 and 21, *P < 0.05. Control only differentiated medium-treated cells, 5 μg/ml and 50 μg/ml indicated boron concentrations containing differentiation medium-treated cells, MYH myosin heavy chain, MYOG myogenin, α-SMA alpha-smooth muscle actin
Western Blot Analysis
To confirm the effects of boric acid application on myogenic-related protein expression, MYH, MyoD, and α-SMA protein expression levels were detected. MYH and MyoD protein expression were significantly reduced in boric acid-treated groups regardless of the concentration at the end of 3 weeks differentiation period. Although 5 μg/ml boric acid administration did not change the α-SMA level compared to the control group, 50 μg/ml boric acid significantly reduced the α-SMA protein expression (Fig. 4).
Western blot analysis for MYH, MyoD, and α-SMA of boric acid-treated human adipose-derived stem cells at day 21, *P < 0.05. C only differentiated medium-treated cells, 5 μg/ml and 50 μg/ml indicated boron concentrations containing differentiation medium-treated cells, MYH myosin heavy chain, α-SMA alpha-smooth muscle actin
Discussion
Skeletal myogenesis as a vital embryonic development process proceeds during the adult organogenesis to maintain bone and muscle tissue integrity. This myogenic switch may be interrupted due to various reasons including aging, diseases, or physical conditions, which leads subsequently to severe bone and muscle tissue losses [19].
Implantation of appropriate scaffold systems to induce cell differentiation and tissue formation that can replace the defective tissue by degrading over time is a promising approach for bone and muscle tissue engineering. Many aspects including biocompatibility, mechanical resistant, antimicrobiality, porosity, shape, cost along with being biocompatible and bioinductive are required for the design of these complex systems [20]. Exogenous vitamin and mineral supplementation can increase the regeneration and slow down the tissue atrophy, supporting the idea that nutritional elements as modifiable factors might contribute to the bone healing or muscle recovery [21, 22]. In this line, incorporation of boron into such scaffolds to provide a favorable environment for cell proliferation and differentiation could be a new option for regenerative medicine. Boron as a readily available dietary supplement affects a great number of metabolic parameters and accumulates in bone tissue, providing fracture healing by regulating magnesium, calcium, and vitamin D turnover [23, 24]. Although the effect and possible mechanism of boron derivatives and their dietary products on bone growth has been reported in several studies [7], boron’s role in muscle development and regeneration remains unclear.
To investigate the potential role of boron in muscle tissue homeostasis and to improve nutritional strategies for musculoskeletal recovery, additional in vitro and in vivo analysis are highly required. Therefore, here we showed the effect of boric acid on myogenic differentiation of hADSCs in the current study. As one of the important multipotent MSC type, adipose tissue-derived stem cells (ADSCs) have been shown to differentiate into myo- [25], neuro- [26], osteo- [27], chondro- [28], and angiogenic [29] cell lineages. hADSCs were used in the current study because ADSCs has been reported to present better myogenic differentiation property than other MSCs due to having high proliferation capacity and notable stem cell marker expression [30]. Two doses (5 and 50 μg/ml) of boric acid were preferred as inductive concentrations for cell proliferation and did not impair myocyte transformation morphologically. However, 50 μg/ml boric acid reduced MYH, MyoD, and α-SMA at the protein level which was confirmed with immunocytochemical and Western blot analysis. Myogenic differentiation marker genes such as MYH, MYOG, MyoD, and desmin exerted a high expression pattern for 5 and 50 μg/ml at early stage of myogenic differentiation; however, significant downregulation was noted for 50 μg/ml boric acid at the end of 21 days, indicating dose- and exposure time-dependent activity of boron. Although the results proposed that low-dose boron could be used in muscle regeneration applications, a fine tuning in dose and time of exposure arrangement is strictly required.
The role of boron on organ development has been found to be strictly dependent on dose and duration of exposure. While dietary low-dose boron intake has improved organ indexes and tissue structure in rats, elevated levels of boron treatment (640 mg boric acid/L) has resulted in low organ weight and abnormal tissue structure [31]. Similarly, the results of the current study revealed that both low- and high-dose boron treatments increased myogenic lineage-specific gene expression in early stage of differentiation; high-dose boron treatment significantly decreased the myogenic differentiation potential of hADSCs. High boric acid concentration administration (4.5 mmol boron/kg) has resulted in reduced levels of important metabolites including glycogen, glucose, lactate, and ATP in chick muscles in both dose- and time-dependent manners [32]. Consistently, low glucose levels, necrotic and fragmented muscle fibers in excessive boron-fed broilers have been reported in a different study [10]. As restricted glucose levels and subsequent low intercellular ATP concentration inhibit skeletal myogenic differentiation of progenitor cells [33], one possible explanation for the adverse effect of boron on myogenic transformation might be inadequate levels of glucose and ATP in hADSCs. From a different point of view, boron has been proven to decrease calcium release by two independent in vitro studies [34, 35]. Several reports have underlined the importance of calcium signaling and homeostasis in myogenic transcription factors activation and myogenesis [36–38]. Therefore, interrupted calcium signaling due to high-dose boron treatment might have decreased the myogenic differentiation capacity of hADSCs. However, further studies are highly warranted to explore exact molecular mechanisms of effects of boron on myogenic differentiation. The findings of the study present not only an understanding of boron’s effect on myogenic differentiation but also an opportunity for the development of scaffolds to be used in skeletal tissue engineering and supplements for embryonic muscle growth. However, fine dose tuning and treatment period arranging are strictly necessary as boron treatment over required concentrations and time might result in detrimental outcomes to myogenesis and myo-regeneration.
References
Gallardo-Williams MT, Maronpot RR, Turner CH, Johnson CS, Harris MW, Jayo MJ, Chapin RE (2003) Effects of boric acid supplementation on bone histomorphometry, metabolism, and biomechanical properties in aged female F-344 rats. Biol Trace Elem Res 93(1–3):155–170. doi:10.1385/BTER:93:1-3:155
Hall IH, Spielvogel BF, Griffin TS, Docks EL, Brotherton RJ (1989) The effects of boron hypolipidemic agents on LDL and HDL receptor binding and related enzyme activities of rat hepatocytes, aorta cells and human fibroblasts. Res Commun Chem Pathol Pharmacol 65(3):297–317
Hunt CD, Herbel JL, Idso JP (1994) Dietary boron modifies the effects of vitamin D3 nutrition on indices of energy substrate utilization and mineral metabolism in the chick. J Bone Miner Res 9(2):171–182
Kurtoğlu F, Kurtoğlu V, Celik I, Kececi T, Nizamlioğlu M (2005) Effects of dietary boron supplementation on some biochemical parameters, peripheral blood lymphocytes, splenic plasma cells and bone characteristics of broiler chicks given diets with adequate or inadequate cholecalciferol (vitamin D3) content. Br Poult Sci 46(1):87–96
Kurtoĝlu V, Kurtoĝlu F, Coşkun B (2001) Effects of boron supplementation of adequate and inadequate vitamin D3-containing diet on performance and serum biochemical characters of broiler chickens. Res Vet Sci 71(3):183–187
Nielsen FH, Shuler TR, Zimmerman TJ, Uthus EO (1987) Dietary magnesium, manganese and boron affect the response of rats to high dietary aluminum. Magnesium 7(3):133–147
Nielsen FH, Meacham SL (2011) Growing evidence for human health benefits of boron. J Evid Based Complement Altern Med 16(3):169–180
Devirian TA, Volpe SL (2003) The physiological effects of dietary boron. Crit Rev Food Sci Nutr 43(2):219–231. doi:10.1080/10408690390826491
Fail PA, Chapin RE, Price CJ, Heindel JJ (1998) General, reproductive, developmental, and endocrine toxicity of boronated compounds. Reprod Toxicol 12(1):1–18
Meryem Eren FU, Berrin KG, Atasever A (2012) The influence of dietary boron supplementation on performance, some biochemical parameters and organs in broilers. Asian J Anim Vet Adv 7(11):1079–1089
Taşlı PN, Doğan A, Demirci S, Şahin F (2013) Boron enhances odontogenic and osteogenic differentiation of human tooth germ stem cells (hTGSCs) in vitro. Biol Trace Elem Res 153(1–3):419–427
Hakki SS, Bozkurt BS, Hakki EE (2010) Boron regulates mineralized tissue-associated proteins in osteoblasts (MC3T3-E1). J Trace Elem Med Biol 24(4):243–250
Ying X, Cheng S, Wang W, Lin Z, Chen Q, Zhang W, Kou D, Shen Y, Cheng X, Rompis FA (2011) Effect of boron on osteogenic differentiation of human bone marrow stromal cells. Biol Trace Elem Res 144(1–3):306–315
Waese EY, Kandel RR, Stanford WL (2008) Application of stem cells in bone repair. Skeletal Radiol 37(7):601–608
Yalvac ME, Ramazanoglu M, Gumru OZ, Sahin F, Palotás A, Rizvanov AA (2009) Comparison and optimisation of transfection of human dental follicle cells, a novel source of stem cells, with different chemical methods and electro-poration. Neurochem Res 34(7):1272–1277
Doğan A, Demirci S, Şahin F (2014) In vitro differentiation of human tooth germ stem cells into endothelial‐ and epithelial‐like cells. Cell Biol Int. doi:10.1002/cbin.10357
Yilgor Huri P, Cook C, Hutton D, Goh B, Gimble J, DiGirolamo D, Grayson W (2013) Biophysical cues enhance myogenesis of human adipose derived stem/stromal cells. Biochem Biophys Res Commun 438(1):180–185
Doğan A, Yalvaç ME, Şahin F, Kabanov AV, Palotás A, Rizvanov AA (2012) Differentiation of human stem cells is promoted by amphiphilic pluronic block copolymers. Int J Nanomedicine 7:4849–4860
Hespel P, Op’t Eijnde B, Van Leemputte M, Ursø B, Greenhaff PL, Labarque V, Dymarkowski S, Van Hecke P, Richter EA (2001) Oral creatine supplementation facilitates the rehabilitation of disuse atrophy and alters the expression of muscle myogenic factors in humans. J Physiol (Lond) 536(2):625–633
Rezwan K, Chen Q, Blaker J, Boccaccini AR (2006) Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 27(18):3413–3431
Ilich JZ, Brownbill R, Tamborini L (2003) Bone and nutrition in elderly women: protein, energy, and calcium as main determinants of bone mineral density. Eur J Clin Nutr 57(4):554–565
Hughes MS, Kazmier P, Burd TA, Anglen J, Stoker AM, Kuroki K, Carson WL, Cook JL (2006) Enhanced fracture and soft-tissue healing by means of anabolic dietary supplementation. J Bone Joint Surg Am 88(11):2386–2394
Gallardo-Williams MT, Chapin RE, King PE, Moser GJ, Goldsworthy TL, Morrison JP, Maronpot RR (2004) Boron supplementation inhibits the growth and local expression of IGF-1 in human prostate adenocarcinoma (LNCaP) tumors in nude mice. Toxicol Pathol 32(1):73–78
Gorustovich AA, Steimetz T, Nielsen FH, Guglielmotti MB (2008) Histomorphometric study of alveolar bone healing in rats fed a boron‐deficient diet. Anat Rec 291(4):441–447
Tang W, Zeve D, Suh JM, Bosnakovski D, Kyba M, Hammer RE, Tallquist MD, Graff JM (2008) White fat progenitor cells reside in the adipose vasculature. Science 322(5901):583–586
Zimmerlin L, Donnenberg VS, Pfeifer ME, Meyer EM, Péault B, Rubin JP, Donnenberg AD (2010) Stromal vascular progenitors in adult human adipose tissue. Cytometry A 77(1):22–30
Suga H, Matsumoto D, Eto H, Inoue K, Aoi N, Kato H, Araki J, Yoshimura K (2009) Functional implications of CD34 expression in human adipose-derived stem/progenitor cells. Stem Cells Dev 18(8):1201–1210
Mizuno H, Tobita M, Uysal AC (2012) Concise review: adipose‐derived stem cells as a novel tool for future regenerative medicine. Stem Cells 30(5):804–810
Bailey AM, Kapur S, Katz AJ (2010) Characterization of adipose-derived stem cells: an update. Curr Stem Cell Res Ther 5(2):95–102
Traktuev DO, Merfeld-Clauss S, Li J, Kolonin M, Arap W, Pasqualini R, Johnstone BH, March KL (2008) A population of multipotent CD34-positive adipose stromal cells share pericyte and mesenchymal surface markers, reside in a periendothelial location, and stabilize endothelial networks. Circ Res 102(1):77–85
Hu Q, Li S, Qiao E, Tang Z, Jin E, Jin G, Gu Y (2014) Effects of boron on structure and antioxidative activities of spleen in rats. Biol Trace Elem Res 158(1):73–80
Geyikoğglu F, Türkez H (2007) Acute toxicity of boric acid on energy metabolism of the breast muscle in broiler chickens. Biologia 62(1):112–117
Fulco M, Cen Y, Zhao P, Hoffman EP, McBurney MW, Sauve AA, Sartorelli V (2008) Glucose restriction inhibits skeletal myoblast differentiation by activating SIRT1 through AMPK-mediated regulation of Nampt. Dev Cell 14(5):661–673
Henderson K, Eckhert C (2008) Boric acid is a modulator of stored calcium release in DU-145 prostate cancer cells. FASEB J 22:1116–1181, 1_MeetingAbstracts
Henderson K, Stella SL Jr, Kobylewski S, Eckhert CD (2009) Receptor activated Ca2+ release is inhibited by boric acid in prostate cancer cells. PLoS One 4(6):e6009
Darbellay B, Arnaudeau S, König S, Jousset H, Bader C, Demaurex N, Bernheim L (2009) STIM1-and Orai1-dependent store-operated calcium entry regulates human myoblast differentiation. J Biol Chem 284(8):5370–5380
McKinsey TA, Zhang C-L, Lu J, Olson EN (2000) Signal-dependent nuclear export of a histone deacetylase regulates muscle differentiation. Nature 408(6808):106–111
Porter GA, Makuck RF, Rivkees SA (2002) Reduction in intracellular calcium levels inhibits myoblast differentiation. J Biol Chem 277(32):28942–28947
Acknowledgments
The study was supported by Yeditepe University. The authors would like to thank A. Burcin Asutay and Binnur K. Herand for their assistance during flow cytometry and confocal imaging analysis.
Conflict of Interest
The authors deny any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
The viability and proliferation of human adipose-derived stem cells (hADSCs) treated with different concentrations of boric acid (5-2000 μg/ml) over the course of three days, * P < 0.05. NC: Growth medium-treated cells, PC: 20 % DMSO containing growth medium-treated cells. NC cells were accepted as 100 % viable. (GIF 114 kb)
Rights and permissions
About this article
Cite this article
Apdik, H., Doğan, A., Demirci, S. et al. Dose-dependent Effect of Boric Acid on Myogenic Differentiation of Human Adipose-derived Stem Cells (hADSCs). Biol Trace Elem Res 165, 123–130 (2015). https://doi.org/10.1007/s12011-015-0253-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-015-0253-3