Abstract
Effects of vitamin E and selenium supplementation on aldehyde oxidase (AO) and xanthine oxidase (XO) activities and antioxidant status in liver, kidney, and heart of streptozotocin (STZ)-induced diabetic rats were examined. AO and XO activities increased significantly after induction of diabetes in rats. Following oral vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg) intake once a day for 4 weeks, XO activity decreased significantly. AO activity decreased significantly in liver, but remained unchanged in kidney and heart of vitamin E- and selenium-treated rats compared to the diabetic rats. Total antioxidants status, paraoxonase-1 (PON1) and erythrocyte superoxide dismutase activities significantly decreased in the diabetic rats compared to the controls, while a higher fasting plasma glucose level was observed in the diabetic animals. The glutathione peroxidase activity remained statistically unchanged. Malondialdehyde and oxidized low-density lipoprotein levels were higher in the diabetic animals; however, these values were significantly reduced following vitamin E and selenium supplementation. In summary, both AO and XO activities increase in STZ-induced diabetic rats, and vitamin E and selenium supplementation can reduce these activities. The results also indicate that administration of vitamin E and selenium has hypolipidemic, hypoglycemic, and antioxidative effects. It decreases tissue damages in diabetic rats, too.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is the most significant chronic metabolic disease with the highest rate of prevalence and mortality worldwide. It is estimated that about 5% of the world population are affected by this metabolic disorder and the prevalence of adults with diabetes is estimated to increase by 122% from 135 million in 1995 to 300 million in 2025 [1].
According to a large body of evidence, reactive oxygen species (ROS) and oxidative stress may play a pivotal role in the development, pathogenesis, and complication of diabetes [2, 3]. However, the mechanism(s) of the oxidative stress and ROS formation in diabetes have not been fully understood [4].
There are several potential sources of ROS in diabetes such as auto-oxidative glycosylation, hyperketonemia, the induction of NAD(P)H oxidases, and xanthine oxidase activity [4–7]. Xanthine oxidase (EC 1.17.3.2, XO) is a cytosolic molybdenum-containing enzyme that exists originally as dehydrogenase form; however, it could be converted to the oxidase form in some conditions either irreversibly by proteolysis or reversibly by sulfhydryl oxidation of the protein molecule. The reactions catalyzed by xanthine oxidase/dehydrogenase involve generation of two electrons. Xanthine dehydrogenase (XDH) utilizes NAD+ as the electron acceptor, but XO uses molecular oxygen as an electron acceptor producing hydrogen peroxide and superoxide anion [8]. Therefore, XO can act as an important biological source of ROS, and the involvement of this enzyme in many pathological processes including diabetes have been well documented [4, 9–12]. According to previous studies, circulating and tissue XO levels are increased in experimental diabetes, and this contributes to superoxide production [13]. It has also been demonstrated that treatment of the diabetic animal models with allopurinol, a potent inhibitor of XO, could improve some diabetic complications such as endothelium-dependent vasodilation and reduce the circulating levels of superoxides and MDA, a well-known oxidative stress marker [7, 13] confirming the importance of XO activity in diabetes.
XO is closely related to another molybdenum hydroxylase, aldehyde oxidase (EC:1.2.3.1, AO). Both enzymes have many physicochemical properties such as cofactor composition, molecular weight, absorption spectrum, and subunit structure in common [14, 15]. The reaction catalyzed by AO also produces two electrons and molecular oxygen acts as the electron acceptor. ROS are, thus, generated during the oxidative activity of AO giving a potential to the enzyme to be involved in diabetes. However, unlike XO, AO activity in diabetes has not received enough attention.
On the other hand, antioxidant defense system is disturbed in diabetes, and therefore, antioxidant supplementation could contribute to prevention of diabetic complications by improving the antioxidant status. Vitamin E and selenium are two micronutrients with antioxidant properties that work codependently to protect the body from the harmful and destructive effects of free radicals. Accordingly, the effects of these two micronutrients in diabetes have been covered by some studies [16–25]. However, the existing literature data are controversial. There is a large body of evidence indicating the ability of selenium in the prevention of diabetes development [16–19]. It has also been reported that the serum concentration of selenium in diabetic patients is significantly lower than its level in the controls [20, 21]. More recently, no important differences for serum selenium levels in patients with type II diabetes and non-diabetic individuals have been reported [22]. No difference in the serum selenium levels of diabetic subjects with and without coronary artery disease has also been reported by Sotiropoulos et al. [23]. On the other hand, according to some other studies, there is a positive association between high serum selenium levels and the prevalence of diabetes [24]. It is possible that the elevated plasma levels of selenium in patients with diabetes II arise from the disease-related changes of the blood proteins. Thus, it seems that further studies are required to explore the functions of antioxidant micronutrients in diabetes, particularly with respect to in vivo source of ROS. Therefore, in the present study, AO and XO activities in streptozotocin (STZ)-induced diabetic rats have been investigated.
Materials and Methods
Experimental Design
Twenty-four female Sprague-Dawley rats weighing 200 ± 30 g (about 2–3 months of age), were kept in the animal house at temperatures of 23 ± 2°C and relative humidity of 50% under a lighting cycle of 7AM–7PM light and 7PM–7AM dark. They were fed with a standard laboratory diet ad libitum for an acclimatization period of 1 week prior to the experiment. All animals were handled in accordance with the National Institutes of Health Guidelines and the experimental procedure of the study was approved by the ethical committee of Tabriz University of Medical Sciences.
The animals were divided into three groups of: group I, normal control rats, C (n = 8); group II, STZ-induced diabetic rats, DM (n = 8); and group III, diabetic rats with orally administered vitamin E and selenium, DM + S (n = 8). The body weights of all the animals were determined weekly and water consumed was recorded daily.
Diabetes Induction
The experimental diabetes type 1 was induced in groups II and III by a single intraperitoneal injection of 60 mg/kg body weight STZ (Sigma), freshly dissolved in 0.01 M citrate buffer (pH 4.5) [26]. STZ-injected animals were fed 20% glucose solution for 24 h to prevent initial drug-induced hypoglycemic mortality [27]. Control rats received an injection of physiological serum. Six days after STZ injection, rats with blood glucose levels above 300 mg/dL, estimated with enzymatic method, were considered as diabetic and used for the study.
Vitamin E and Selenium Treatment
On the seventh day following STZ injection (first day of treatment), vitamin E as α-tocopherol acetate (Merck) dissolved in corn oil and selenium as sodium selenite (Merck) dissolved in water were administrated to group III at concentrations of 300 and 0.5 mg kg−1 day−1, respectively, by oral gavage once a day for 4 weeks. Group II rats received 0.5 ml corn oil and 0.5 ml physiological solution and were used as diabetic control group.
Sample Preparation
Blood Sampling
At the beginning and the end of the experimental period, blood samples were collected from the retro-orbital plexus of the eye in EDTA-containing tubes under light ether anesthesia after 12 h of fasting. Sera samples were prepared by 10 min centrifugation of blood at 3,000×g at 4°C and were stored at −76°C for further study.
Tissues Sampling
At the end of the experiment, rats were killed between 9 and 10 am after anesthesia with diethyl ether. The livers, kidneys, and hearts were removed, weighed, and then rapidly washed in 0.9% cold saline and placed in ice-cold isotonic potassium chloride solution (1.15% KCl w/v) containing 0.1 mM EDTA. The livers were then chopped into 4–5 volumes of 50 mM phosphate buffer (pH 7.4) and homogenized by a homogenizer fitted with a Teflon pestle. The homogenate was then centrifuged at 3,000×g for 10 min, the lipid layer was carefully removed, and the resulting supernatant fraction was further centrifuged at 15,000×g for 60 min at 4 ° C. The supernatant was stored at −80°C until use.
Determination of Aldehyde Oxidase and Xanthine Oxidase/Dehydrogenase Activities
Liver AO activity was determined spectrophotometrically in Sorenson’s phosphate buffer, pH 7.0 containing 0.1 mM EDTA at 37°C using phenanthridine as substrate as described before [28].
Due to low activity, AO activity in heart and kidney was analyzed by a reversed phase high performance liquid chromatography fluorescence method based on measurement of phenanthridinone produced from oxidation of phenanthridine by AO [29].
The XO and XDH activities were measured spectrophotometrically by monitoring the production of uric acid from xanthine according to Prajda and Weber’s method [30]. In the case of XDH, the assay mixture consisted of 50 μM xanthine, 50 μM phosphate buffer (pH 7.4), 200 μM NAD+, and 100 μl of the enzyme solution. After preincubation at 37 ° C for 15 min, the reaction was initiated by addition of the substrate solution. After 30 min, the reaction was terminated by adding 0.5 ml HCl (0.6 M), and the absorbance was measured at 290 nm using a Shimadzu 2550 UV/VIS spectrophotometer which was controlled by the Shimadzu UV Probe personal software package including kinetics software. The instrument was connected to a Shimadzu cell temperature control unit. XO activity was measured using a similar method described for XDH with the difference being that molecular oxygen was used in place of NAD+ as electron acceptor.
Measurement of Glucose and Lipid Profile
Plasma glucose, total cholesterol (TC) and triglyceride (TG) levels were measured by enzymatic colorimetric methods (Pars Azmune, Tehran, Iran), using an autoanalyzer Model Alcyon. Non-high-density lipoprotein cholesterol (non-HDL-C) lipoproteins in the plasma were precipitated by phosphotungstic acid and magnesium chloride [31], and the content of HDL-C was determined using an enzymatic colorimetric method (Pars Azmune, Tehran, Iran). The concentration of LDL-C was calculated according to the Friedewald formula for <400 mg/dL TG containing samples [32].
Measurement of Ox-LDL
The level of Ox-LDL was measured by using a Mercodia Oxidized LDL ELISA kit (lot no. 15904; Mercodia, Uppsala, Sweden). Mercodia Ox-LDL competitive ELISA is based on the monoclonal antibody 4E6. The Ox-LDL in the sample competes with a fixed amount of Ox-LDL bound to the microtiter well for the binding of the biotin-labeled specific antibodies. After a washing step that removes non-reactive plasma components, the biotin-labeled antibody bound to the well is detected by HRP-conjugated streptavidin. After a second incubation, unbound enzyme-labeled antibody is removed by a simple washing step and the bound conjugate is detected by reaction with 3,3′,5,5′-tetramethylbenzidine. Then, the reaction is stopped by addition of acid and the microtitration strips are read spectrophotometrically at 450 nm. The results are calculated using the computerized data reduction of absorbance for the standards versus the log concentration using a cubic spline regression and expressed as units per liter.
Measurement of GPx and SOD Activities
The hemoglobin content of the erythrocytes was determined using the cyanmethemoglobin method [33]. Erythrocyte GPx and superoxide dismutase (SOD) activities were determined using Randox kits (Randox Laboratories). GPx activity levels were measured using the method of Paglia and Valentine [34], in which GPx activity was coupled with the oxidation of NADPH by glutathione reductase. The oxidation of NADPH was followed spectrophotometrically at 340 nm. The reaction mixture comprised 50 mM/L potassium phosphate buffer (pH 7.2), 4.3 mM/L EDTA, 0.18 mM/L cumene hydroperoxide, 0.34 mM/L NADPH, 4 mM/L glutathione, and 0.5 U/L of glutathione reductase. The absorbance at 340 nm was recorded for 5 min, and the activity calculated from the slope of the line as micromolars of NADPH oxidized per minute. The results were expressed as units per gram of hemoglobin.
The determination of SOD activity was based on the production of O2− anions by the xanthine/xanthine oxidase system [35]. O2− reacts with 2-(4-iodophenyl)-3-(4-nitrophenol)-5-phenyltetrazolium chloride (INT) to form a red formazan dye. The SOD activity was measured by the degree of inhibition of this reaction in 505 nm. The results were expressed as units per gram of hemoglobin.
Measurement of Plasma TAS
Total antioxidant status (TAS) was measured in serum by means of a commercial kit (Randox Laboratories). The assay is based on the incubation of 2, 2′-azino-di-(3-ethylbenzthiazoline sulphonate) (ABTS) with a peroxidase (methmyoglobin) and hydrogen peroxide to produce the radical cation ABTS+, which has a relatively stable blue-green color, measured at 600 nm [36]. The suppression of the color is compared with that of the Trolox, which is widely used as a traditional standard for TAS measurement assays, and the assay results are expressed as Trolox equivalent (mM/L).
Measurement of Plasma MDA
Plasma MDA levels were determined by the thiobarbituric acid method and expressed as nanomoalars MDA formed per milliliter serum [37]. Briefly, 0.5 ml serum was shaken with 2.5 ml of 20% trichloroacetic acid in a 10 ml centrifuge tube. Then, 1 ml of 0.67 % thiobarbituric acid was added to the mixture, shaken, and warmed for 60 min in a boiling water bath followed by rapid cooling. It was then shaken into a 4 ml of n-butanol layer in a separation tube, and MDA content in the serum was determined at 532 nm by spectrophotometer against n-butanol. The standards of 0.1–20 μM/L tetraethoxypropane were used to obtain the calibration curve.
Analysis of PON1 Activities
PON1 activity toward paraoxon (O,O-diethyl-O-p-nitrophenylphosphate; Sigma Chemical Co.) was determined by adding plasma to Tris/HCl buffer (0.1 mol/L, pH 8.0) containing paraoxon (2 mmol/L) and CaCl2 (2 mmol/L). The rate of hydrolysis of paraoxon was measured spectrometrically (UV 1250, Shimadzu, Japan) by monitoring p-nitrophenol libration at 412 nm. The amount of generated p-nitrophenol was calculated from the molar absorptivity of 18,290 mol−1 cm−1 [38].
Statistical Analysis
All data were expressed as mean ± SEM. Variables between groups were compared using one-way analysis of variance (ANOVA) and Tukey honestly significantly difference. The relationship between XO, XDH, and AO activities and other parameters were estimated by Pearson correlation analysis. A value of p < 0.05 was considered statistically significant. Statistical analyses were carried out by SPSS (version 17).
Results
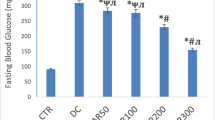
As expected, fasting blood sugar (FBS) was found to be significantly higher in the STZ-induced diabetic rats than in the control group (p < 0.01). Treatment of diabetic rats with vitamin E and selenium supplement resulted in a significant reduction in the FBS level of diabetic rats, although the glucose concentration was very different from that of healthy control rats. In addition, much more reduction was observed in FBS levels after 5 weeks of treatment indicating that vitamin E and selenium supplementation reduced FBS in a time-dependent manner (Table 1).
STZ-induced diabetic group lost weight and treatment with vitamin E and selenium increased the weight of the rats relative to DM group after 5 weeks but not 1 week; however, the increase was not statistically significant (Table 1).
Plasma triglyceride, total cholesterol, LDL-C, and LDL-Ox levels in STZ-induced diabetic rats significantly increased and HDL-C level decreased significantly compared to healthy control group after 5 weeks of treatment, as shown in Table 1. Supplementation with vitamin E and selenium decreased total cholesterol, LDL-C, and LDL-Ox levels significantly (p < 0.05) compared to DM group, but the differences in plasma triglyceride levels between diabetic and vitamin E + selenium-supplemented group were not statistically significant. HDL-C concentration also increased after supplementation with vitamin E and selenium for 4 weeks, and there was no significant difference between HDL-C level of healthy controls and DM + S group (p > 0.05) (Table 1).
Although STZ-induced diabetes did not affect the blood GPx activity, the level of this enzyme in treated diabetic group was found to be significantly higher than the control and diabetic animals after 5 weeks (Table 1). At the first week of treatment, a significant reduction was observed in erythrocyte SOD activity in both diabetic and treated diabetic groups; however, the enzyme activity increased to almost the control value after four weeks treatment with vitamin E and selenium.
A marked increase in the plasma MDA concentration, a secondary product of lipid peroxidation, was observed in STZ-induced diabetic rats compared to healthy control rats. Administration of vitamin E and selenium for 4 weeks reduced MDA significantly compared to DM rats (p < 0.01; Fig. 1).
Plasma malondialdehyde (MDA) level in streptozotocin (STZ)-induced diabetic rats (DM group), and diabetic rats with orally administered vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg) supplementation (DM + S group) after 1 and 5 weeks of oral supplementation with vitamin E (300 mg/kg/day) and sodium selenite (0.5 mg/kg/day). Values are expressed as mean ± SEM for eight rats in each group. Statistical comparison: aExperimental group vs. control; bWeek 1 vs. Week 5; cDM group vs. the corresponding DM + S group, Statistical significance: *p <0.05; **p <0.01
Plasma TAS levels significantly decreased in the diabetic group five weeks after STZ injection compared with the control group; the treatment with vitamin E and selenium was almost able to restore the TAS of the diabetic rats (Fig. 2).
Total antioxidant statuse (TAS) level in streptozotocin (STZ)-induced diabetic rats (DM group), and diabetic rats with orally administered vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg) supplementation (DM + S group) after 1 and 5 weeks of oral supplementation with vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg), Values are expressed as mean ± SEM for eight rats in each group. Statistical comparison: aExperimental group vs. control; bWeek 1 vs. Week 5; cDM group vs. the corresponding DM + S group, Statistical significance: *p <0.05; **p <0.01
PON1’s activity decreased significantly five weeks after diabetes induction (p < 0.01). However, in the diabetic group under treatment with vitamin E and selenium, PON1 activity was restored to near-normal level (Fig. 3).
Paraoxonase (PON1) activity in streptozotocin (STZ)-induced diabetic rats (DM group), and diabetic rats with orally administered vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg) supplementation (DM + S group) after 1 and 5 weeks of oral supplementation with vitamin E (300 mg/kg) and sodium selenite (0.5 mg/kg), Values are expressed as mean ± SEM for eight rats in each group. Statistical comparison: aExperimental group vs. control; bWeek 1 vs. Week 5; cDM group vs. the corresponding DM + S group, Statistical significance: *p <0.05; **p <0.01
Liver, kidney, and heart XO levels significantly increased in STZ-induced diabetic rats compared to healthy control rats (p < 0.01). Vitamin E + selenium-treated diabetic rats had significantly lower XO activity than untreated diabetic rats (p < 0.01), although in liver and kidney, the activity was not as low as healthy control group.
AO activity in liver, kidney, and heart of untreated diabetic rats increased significantly compared to healthy control group, but supplementation with vitamin E + selenium for 4 weeks reduced hepatic AO activity compared to DM controls (p < 0.05). No significant differences were observed in AO activities in kidney and heart of diabetic and vitamin E plus selenium-supplemented group (Table 2).
The correlation between different variables involved in the study was investigated (Table 3). Very strong positive correlations were found between liver, kidney, and heart AO activities and LDL-Ox levels in rats. Similarly, there were positive correlations between liver, kidney and heart XO activities and LDL-Ox levels in rats (p = 0.00). AO activities in liver and kidney were inversely correlated with plasma PON1 (p < 0.05). In addition, liver, kidney, and heart AO and XO activities negatively correlated with plasma TAS level in rats (p < 0.05).
Discussion
STZ-induced diabetes is a well-established experimental model for type 1 diabetes, extensively used to investigate the biochemical and histomorphological changes in diabetes. STZ-induced diabetic animals suffer from the most diabetic complications mediated through oxidative stress [39]. Increased generation of ROS and free radicals has been reported in both types of diabetes [40]. STZ-induced diabetes is usually characterized by severe weight loss [41] and an increase in FBS, and it is thought that chronic hyperglycemia plays an important role in oxidative stress in diabetic animals by depleting the antioxidative defense system [42].
As expected, induction of diabetes by STZ caused a significant reduction in the body weight with an increase in the concentration of FBS. It has been hypothesized that the decrease in the body weight of the diabetic rats might be the result of protein wasting, as carbohydrates are unavailable to be used as an energy source [43]. It has also been suggested that STZ can stimulate free radical production, which may be responsible for pancreatic β-cells damage [44]. A significant reduction in the FBS and the improvement of body weight of diabetic rats following 4 weeks of vitamin E + selenium supplementation observed in the present study could be indicative of the protective effect of the vitamin E + selenium supplementation on the protein damage. It is more likely that this protective effect rises from the antioxidative properties of vitamin E and selenium. This could be supported by comparing the effects of these two antioxidant micronutrients on the plasma LDL-Ox, MDA, and TAS levels in treated versus untreated diabetic rats (Table 1, Figs. 1 and 2). LDL-Ox and MDA as products of lipid peroxidation are generated under high levels of un-scavenged free radicals and can lead to the diabetes-associated pancreatic damage [45].
Vitamin E and selenium supplementation was also able to increase GPx activity of diabetic rats. GPx is one of the central enzymatic antioxidants, which is able to protect the tissue against oxidative stress and damage through breakdown of superoxide and inhibition of lipid peroxidation. It seems that vitamin E and/or selenium exert some of their antioxidant properties through enhancing enzymatic antioxidant defense mechanisms and subsequently protecting the pancreatic β-cells against STZ-induced oxidative damage. Since islet cells are much more exposed to free radicals’ attack due to relatively low activity of their antioxidant enzymes such as GPx, vitamin E, and selenium supplementation can be of value here [46].
It has been shown that XO is an important source of increased ROS levels in diabetic rat [47], and its activity in heart, kidney, and brain tissues increases in diabetic rats [48]. Besides, plasma XO activity is markedly elevated by diabetes, principally as a result of hepatic release [4, 13]. In the present study, XO and XDH activities in liver, heart, and kidney were found to be higher in the untreated group when compared to the vitamin E + selenium-treated group. Increased XDH and XO activities in diabetic rats (Table 2) may lead to enhanced oxidative stress in liver, heart, and kidney, leading to secondary organ damage associated with diabetes.
AO is also involved in the formation of ROS in both liver and lung extracts [49]. It is an important enzyme that catalyzes the oxidation of many aldehydes and N-heterocycles [15]. Endogenous aldehydes are principally generated through lipid peroxidation, glycation and amino acid oxidation. One of the most important lipid peroxidation products is MDA produced in the membrane lipid peroxidation. In disease states when aldehyde production is high, AO is the major enzyme responsible for the metabolism of endogenous aldehydes leading to ROS generation (such as O2- and hydrogen peroxide), which may explain the ROS-mediated oxidative liver injury. In our study, the levels of MDA and AO activity increased and as expected, significant positive correlations were observed between MDA levels and AO activity in liver and kidney (Table 3). Supplementation of the diabetic rats with vitamin E and selenium decreased plasma MDA level and hepatic AO activity, demonstrating the role of these two antioxidants in inhibition of lipid peroxidation. It has been previously reported that human liver AO activity was 23-fold higher than XO activity [50, 51]; however, our study showed that in rat liver AO activity was about 7-fold higher than XO activity. These studies demonstrate that AO is an important source of ROS generation in normal conditions. But in the diseases with high levels of aldehydes, AO plays an important role in ROS-mediated injury.
In conclusion, vitamin E and selenium supplementation decrease tissue damage in diabetic rats through displaying antioxidative properties. This implicates XO and AO as important sources of ROS in diabetes, and, therefore, potential therapeutic targets for future study in clinical trials of diabetes. The results of this study gave further evidence for the beneficial effects of vitamin E and selenium supplementation in diabetes. Taken into account the extensive antioxidative effects of vitamin E and selenium supplementation observed in this study in diabetic rats, use of these compounds in diabetes prevention and management could be recommended.
References
King H, Aubert RE, Herman WH (1998) Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 21:1414–1431
Strain JJ (1991) Disturbances of micronutrient and antioxidant status in diabetes. Proceedings of the Nutrition Society 50:591–604
Ramakrishna V, Jailkhani R (2008) Oxidative stress in non-insulin-dependent diabetes mellitus (NIDDM) patients. Acta Diabetol 45:41–46
Desco MC, Asensi M, Marquez R et al (2002) Xanthine oxidase is involved in free radical production in type 1 diabetes: Protection by allopurinol. Diabetes 51:1118–1124
Hunt JV, Dean RT, Wolff SP (1988) Hydroxyl radical production and autoxidative glycosylation. Glucose autoxidation as the cause of protein damage in the experimental glycation model of diabetes mellitus and ageing. Biochem J 256:205–212
Jain SK, McVie R, Jaramillo JJ, Chen Y (1998) Hyperketonemia (acetoacetate) increases the oxidizability of LDL + VLDL in Type-I diabetic patients. Free Radic Biol Med 24:175–181
Inkster ME, Cotter MA, Cameron NE (2007) Treatment with the xanthine oxidase inhibitor, allopurinol, improves nerve and vascular function in diabetic rats. Eur J Pharmacol 561:63–71
Kundu TK, Hille R, Velayutham M, Zweier JL (2007) Characterization of superoxide production from aldehyde oxidase: an important source of oxidants in biological tissues. Arch Biochem Biophys 460:113–121
Higgins P, Ferguson LD, Walters MR (2011) Xanthine oxidase inhibition for the treatment of stroke disease: a novel therapeutic approach. Expert Rev Cardiovasc Ther 9:399–401
Higgins P, Dawson J, Walters M (2009) The potential for xanthine oxidase inhibition in the prevention and treatment of cardiovascular and cerebrovascular disease. Cardiovasc Psychiatry Neurol 2009:282059.
Hanachi N, Charef N, Baghiani A et al (2009) Comparison of xanthine oxidase levels in synovial fluid from patients with rheumatoid arthritis and other joint inflammations. Saudi Med J 30:1422–1425
Lee BE, Toledo AH, Anaya-Prado R, Roach RR, Toledo-Pereyra LH (2009) Allopurinol, xanthine oxidase, and cardiac ischemia. J Investig Med 57:902–909
Matsumoto S, Koshiishi I, Inoguchi T, Nawata H, Utsumi H (2003) Confirmation of superoxide generation via xanthine oxidase in streptozotocin-induced diabetic mice. Free Radic Res 37:767–772
Turner NA, Doyle WA, Ventom AM, Bray RC (1995) Properties of rabbit liver aldehyde oxidase and the relationship of the enzyme to xanthine oxidase and dehydrogenase. Eur J Biochem 232:646–657
Rashidi MR, Nazemiyeh H (2010) Inhibitory effects of flavonoids on molybdenum hydroxylases activity. Expert Opin Drug Metab Toxicol 6:133–152
Gupta S, Sharma TK, Kaushik GG, Shekhawat VP (2011) Vitamin E supplementation may ameliorate oxidative stress in type 1 diabetes mellitus patients. Clin Lab 57:379–386
Pazdro R, Burgess JR (2010) The role of vitamin E and oxidative stress in diabetes complications. Mech Ageing Dev 131:276–286
Beales PE, Williams AJ, Albertini MC, Pozzilli P (1994) Vitamin E delays diabetes onset in the non-obese diabetic mouse. Horm Metab Res 26:450–452
Faure P (2003) Protective effects of antioxidant micronutrients (vitamin E, zinc and selenium) in type 2 diabetes mellitus. Clin Chem Lab Med 41:995–998
Ruíz C, Alegría A, Barberá R, Farré R, Lagarda J (1998) Selenium, zinc and copper in plasma of patients with type 1 diabetes mellitus in different metabolic control states. J Trace Elem Med Biol 12:91–95
Navarro-Alarcón M, López-G de la Serrana H, Pérez-Valero V, López-Martínez C (1999) Serum and urine selenium concentrations as indicators of body status in patients with diabetes mellitus. Sci Total Environ 228:79–85
Marcason W (2008) What is the latest research on the connection between selenium and diabetes? J Am Diet Assoc 108:188
Sotiropoulos A, Papadodima SA, Papazafiropoulou AK, Ioannidis A, Kokkinari A, Apostolou O, Spiliopoulou CA, Athanaselis S (2011) Serum selenium levels do not differ in type 2 diabetic subjects with and without coronary artery disease. BMC Res Notes 4:270
Bleys J, Navas-Acien A, Guallar E (2007) Serum selenium and diabetes in U.S. adults. Diabetes Care 30:829–834
Steinbrenner H, Speckmann B, Pinto A, Sies H (2011) High selenium intake and increased diabetes risk: experimental evidence for interplay between selenium and carbohydrate metabolism. J Clin Biochem Nutr 48:40–45
Fernandes AAH, Novelli ELB, Okoshi K et al (2010) Influence of rutin treatment on biochemical alterations in experimental diabetes. Biomedicine and Pharmacotherapy 64:214–219
Ramesh B, Pugalendi KV (2006) Antioxidant role of Umbelliferone in STZ-diabetic rats. Life Sciences 79:306–310
Pirouzpanah S, Hanaee J, Razavieh SV, Rashidi MR (2009) Inhibitory effects of flavonoids on aldehyde oxidase activity. Enz Inhibit Med Chem 24:14–21
Rashidi MR, Amini K, Khani MY, Faridi A, Hanaee J, Sorouraddin MS (2011) A highly sensitive HPLC-florescence method to study aldehyde oxidase activity. JAOAC Int 94:550–554
Prajda N, Weber G (1975) Malignant transformation linked imbalance: decreased xanthine oxidase activity in hepatomas. FEBS Letters 59:245–249
Burstein M, Scholnick HR, Morfin R (1970) Rapid method for isolation of lipoproteins from human serum by precipitation with polyanions. J Lipid Res 11(6):583–595
Chait A, Brazg RL, Tribble DL, Krauss RM (1993) Susceptibility of small, dense, low-density lipoproteins to oxidative modification in subjects with the atherogenic lipoprotein phenotype, pattern B. Am J Med 94(4):350–356
Drabkin DL (1965) The molecular weight of haemoglobin, its iron and nitrogen content and optical properties—their relevance in the problem of a reference standard for haemoglobin measurement. Bibl Haematol 21:33–42
Paglia DE, Valentine WN (1967) Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med 70:158–169
Ogura R, Ueta H, Sugiyama M, Hidaka T (1990) Distribution of superoxide dismutase activity in the epidermis: measurement with electron spin resonance spin trapping. J Invest Dermatol 94:227–229
Miller NJ, Rice-Evans C, Davies MJ, Gopinathan V, Milner A (1993) A novel method for measuring antioxidant capacity and its application to monitoring the antioxidant status in premature neonates. Clin Sci (Lond) 84(4):407–412
Gallou G, Ruelland A, Legras B, Maugendre D, Allannic H, Cloarec L (1993) Plasma malondialdehyde in type 1 and type 2 diabetic patients. Clinica Chimica Acta 214:227–234
Jafarnejad A, Bathaie SZ, Nakhjavani M, Hassan MZ (2008) Effect of spermine on lipid profile and HDL functionality in the streptozotocin-induced diabetic rat model. Life Sciences 82(5–6):301–307
Sathishsekar D, Subramanian S (2005) Antioxidant properties of Momordica charantia (bitter gourd) seeds on Streptozotocin induced diabetic rats. Asia Pacific Journal of Clinical Nutrition 14:153–158
Johansen JS, Harris AK, Rychly DJ, Ergul A (2005) Oxidative stress and the use of antioxidants in diabetes: linking basic science to clinical practice. Cardiovasc Diabetol 4:5
Akirav EM, Chan O, Inouye K, Riddell MC, Matthews SG, Vranic M (2004) Partial leptin restoration increases hypothalamic-pituitary-adrenal activity while diminishing weight loss and hyperphagia in streptozotocin diabetic rats. Metabolism 53:1558–1564
Ihara Y, Toyokuni S, Uchida K et al (1999) Hyperglycemia causes oxidative stress in pancreatic beta-cells of GK rats, a model of type 2 diabetes. Diabetes 48:927–932
Chen V, Ianuzzo CD (1982) Dosage effect of streptozotocin on rat tissue enzyme activities and glycogen concentration. Can J Physiol Pharmacol 60:1251–1256
Szkudelski T (2001) The mechanism of alloxan and streptozotocin action in B cells of the rat pancreas. Physiol Res 50:537–546
Xue S, Chen X, Lu J, Jin L (2009) Protective effect of sulfated Achyranthes bidentata polysaccharides on streptozotocin-induced oxidative stress in rats. Carbohydrate Polymers 75:415–419
Tiedge M, Lortz S, Drinkgern J, Lenzen S (1997) Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes 46:1733–1742
Aliciguzel Y, Ozen I, Aslan M, Karayalcin U (2003) Activities of xanthine oxidoreductase and antioxidant enzymes in different tissues of diabetic rats. J Lab Clin Med 142:172–177
Dedon PC, Plastaras JP, Rouzer CA, Marnett LJ (1998) Indirect mutagenesis by oxidative DNA damage: formation of the pyrimidopurinone adduct of deoxyguanosine by base propenal. Proc Natl Acad Sci USA 95:11113–11116
Garattini E, Fratelli M, Terao M (2008) Mammalian aldehyde oxidases: genetics, evolution and biochemistry. Cell Mol Life Sci 65:1019–1048
Krenitsky TA, Spector T, Hall WW (1986) Xanthine oxidase from human liver: purification and characterization. Arch Biochem Biophys 247:108–119
Rodrigues AD (1994) Comparison of levels of aldehyde oxidase with cytochrome P450 activities in human liver in vitro. Biochem Pharmacol 48:197–200
Acknowledgements
This work was supported by a grant from Nutrition Research Center, Medical Faculty and Students’ Research Committee, Tabriz University of Medical Sciences. This is a report of a database from thesis entitled “Effect of Vitamin E and Selenium on Lipid Peroxidation in Diabetic Rats”.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghaffari, T., Nouri, M., Saei, A.A. et al. Aldehyde and Xanthine Oxidase Activities in Tissues of Streptozotocin-Induced Diabetic Rats: Effects of Vitamin E and Selenium Supplementation. Biol Trace Elem Res 147, 217–225 (2012). https://doi.org/10.1007/s12011-011-9291-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-011-9291-7