Abstract
The trace elements studied in this work (Se, Cu, Zn) are the essential constituents or cofactors required to activate numerous enzymes and proteins, playing crucial role in various physiological processes. The disturbed levels of abovementioned elements may adversely affect the endocrine system, resulting in various thyroid disorders among other upsets. The aim of this study was to investigate possible associations between them and parameters of redox balance, thyroid function indices as well as clinical records (duration of disease and therapy, lag time between thyroid surgery and this study examination, LT4 dosage) in patients with different thyroid disorders, including malignant diseases of the gland. In the group of patients with papillary carcinoma, we found a statistically significant higher Cu concentration compared with controls and patients with Hashimoto disease. In the same groups, the parameter of Zn/Cu ratio demonstrated reciprocally arranged statistically significant differences. For the group of papillary cancer patients, there was a negative correlation between lag time since thyroid operation and GPX3 activity. Our data support hypothesis of indirect involvement of Zn and Cu in thyroid regulation. For selenium, lack of simple correlation between its serum level and thyroid indices implies the need for further research on other selenium status parameters more adequately depicting changes in endocrine system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The trace elements studied in this work (Se, Cu, Zn) are the essential constituents or cofactors required to activate numerous enzymes and proteins, playing crucial role in various physiological processes [1–3]. All of these elements are directly or indirectly involved in protection against deleterious effects of reactive oxygen species (ROS) on cell components and in the development of inflammatory responses and stress reaction. Particularly, Se is a constituent of glutathione peroxidase family consisting of several enzymes catalyzing reduction of hydrogen peroxide and lipid and phospholipid hydroperoxides. Three other selenoenzymes thioredoxin reductases detoxify peroxides and control redox-related cellular processes. These two families of selenoenzymes protect the thyrocytes from oxidative stress caused by overproduction of H2O2 and lipid hydroperoxides under thyroid-stimulating hormone (TSH) or stimulating TSH receptor autoantibodies. Being able to decrease H2O2 concentrations in the follicular lumen, glutathione peroxidase is involved in down-regulation of thyroid hormone synthesis, too [4–6]. Selenium is also present in the active centre of iodothyronine deiodinases. They are involved in the regulation of thyroid hormone synthesis, the production of T3 and control of active thyroid hormone levels in peripheral tissues, and modification of the inflammatory and immune responses in autoimmune thyroiditis. Through the expression of the deiodinases, selenium is also associated with injury response, tissue repair, hypothalamic function, and energy homeostasis [7, 8]. Hence, there is a broad spectrum of interactions between selenoenzymes and the thyroid hormone axis.
Major functions of copper metalloproteins involve redox-cycling reactions. Most known cuproenzymes react directly with molecular oxygen and participate in defence mechanisms against oxidative damage [2]. Copper and zinc are both cofactors of cellular and extracellular isoforms of superoxide dismutase. Antioxidant properties of zinc, an element possessing great variety of biological functions, exerted by about 300 Zn-requiring enzymes, comprise protection of sulfhydryl groups against oxidation and inhibition of ROS production by transition metals. Zinc is also necessary in the development and maintenance of proper immune responses [9].
The disturbed levels of all these elements may adversely affect the endocrine system. In particular, the disruption of oxidant–antioxidant balance and impairment of immune function are considered the possible factors in a wide range of pathological conditions, including different thyroid disorders, e.g., Hashimoto disease, endemic goiter, and different cancers of the gland [10–12]. The baseline levels of Se, Cu, and Zn may have clinical relevance for supplementation efficacy [13]. However, data concerning the influence of trace elements (other than iodine) on thyroid failure or thyroid hormones secretion and activity in humans are still limited and difficult to generalize, as they differ in clinical subjects.
The aim of present study was to investigate possible associations between trace elements (Se, Cu, Zn) and other parameters of redox balance: ferric reducing ability of plasma (FRAP), serum glutathione peroxidase (GPX3); thyroid function indices: TSH, free thyroxine (fT4), free triiodothyronine (fT3), antithyroid peroxidase antibodies (anti-TPO), antithyroglobulin (anti-Tg) as well as clinical records (duration of disease and therapy, lag time between thyroid surgery and this study examination, LT4 dosage) in patients with different thyroid disorders, including malignant diseases of the gland.
Patients and Methods
All the patients were female. First group consisted of 17 subjects with Hashimoto disease, aged 35.8 ± 11.7 years, who attended outpatient clinic in the Department of Endocrinology at the Jagiellonian University Medical College, Kraków, Poland. Nine of them were newly diagnosed, and eight had been treated previously, with substitutive dose of levothyroxine (LT4) in the range 25 to 75 μg/day for the period of 1 to 24 months. Apart from clinical picture, they were diagnosed by the following criteria: elevated anti-TPO, anti-Tg, and basal TSH levels as well as decreased or nonhomogenous echogenicity of the thyroid. Two patients presented overt hypothyroidism (TSH: 47.97 and 77.82 μIU/L, respectively), next three presented mild hypothyroidism (TSH in the range 5.70–17.20, fT4 below normal range, fT3 in normal range), and three others were diagnosed with subclinical hypothyroidism (i.e., fT4 and fT3 levels within their respective reference ranges, TSH in the range 5.59–10.18 μIU/L).
Next two groups of participants comprised patients with papillary cancer (n = 25, aged 51.6 ± 13.4 years) and patients with follicular cancer (n = 13, aged 52.5 ± 15.3 years), respectively. The tumours were diagnosed histologically on routine basis, after surgery. The lag time between surgery and this study examination ranged between 8 and 120 months, with mean ± SD of 42.9 ± 25.3 months. Patients with cancers were receiving suppressive dose of LT4 in the range 100 to 200 μg/day. Control groups of female individuals (n = 20, aged 37.7 ± 9.3 years) were recruited among volunteers from the abovementioned medical unit and their acquaintances. They were apparently healthy with no history of chronic illness or infectious/inflammatory processes.
Diagnosis distribution within different age groups of patients was depicted on Fig. 1.
The exclusion criteria adopted in this study were as follows: (1) supplementation with multivitamin or trace element preparations, (2) use of oral contraceptives, (3) nonregular menstrual cycle, (4) smoking, (5) dieting, (6) alcohol abuse, (7) pregnancy or lactation, (8) diabetes. None of the patients received antidepressive or anti-psychotic drugs. Blood samplings were coordinated to occur on 5 to 7 days before menstruation. Ethical committee of Jagiellonian University approved the protocol of study, and an informed consent was obtained from each subject.
All subjects underwent thyroid evaluation including physical examination, thyroid ultrasonography, and evaluation of serum thyroid hormones. The ultrasonographic screening of the thyroid was performed with Aloka ProSound SSD 4000 PHD with 7.5 MHz linear real-time transducer. The hormone (TSH, fT4, fT3) and antibody (anti-TPO, anti-Tg) analyses were done using the electrochemiluminescence immunoassays and the Elecsys 2010 Analyser (Roche Diagnostics GmbH, Germany), according to the manufacturer's instructions. Serum concentrations of sex hormones were determined with the Immunoassay Analyser Immulite 2000 and chemiluminescent immunoassays (P4, E2) or chemiluminescent immunometric assays (LH, FSH), as appropriate, using materials from Diagnostic Products Corporation (DPC) Biermann GmbH, Germany (Immulite® 2000), according to manufacturer's instructions. Serum anti-TPO, anti-TG, fT4, fT3, and sex hormones were determined only in subjects with Hashimoto disease and controls, in luteal phase of menstrual cycle. Ferric reducing ability of plasma was determined by means of the modified method of Benzie and Strain [14]. We used 150 mL of plasma and 2 mL of reaction mixture. Change of absorbance was measured after 8 min of incubation. Glutathione peroxidase activity in plasma was evaluated with hydrogen peroxide as the substrate, as described previously [15]. Se in serum was determined by graphite furnace atomic absorption spectrometry (Perkin Elmer 5100ZL, Norwalk, CT, USA) as described elsewhere [16, 17]. Zn and Cu in serum were determined by flame atomic absorption spectrometry employing the same spectrometer and the method of direct specimen dilution with deionized water. The ratios between the concentrations of serum Se, Cu, and Zn were calculated. The validity and accuracy of the trace element determination was checked by certified reference material Seronorm™ Trace Elements Serum. Results indicated that analytical procedures were reliable.
Statistical Approach
Statistical analyses were carried out by Statistica PL v.6 (StatSoft, Tulsa, OK, USA) programme. Differences between the diagnostic groups for each parameter were tested by the Mann–Whitney nonparametric test, as several parameters demonstrated nonnormal distribution. For the same reason, the analysis of correlation was conducted by calculating the Spearman correlation coefficients (R s) for the pairs of parameters. A p value of 0.05 was considered significant.
Results
The main descriptive statistics of all clinical and biochemical parameters in the study groups and in healthy volunteers are shown in Table 1, while Table 2 comprises data for parameters determined only in subjects with Hashimoto disease and controls. The statistically significant differences for TSH were revealed for the following groups: Hashimoto vs. control group, p < 0.001; Hashimoto vs. papillary cancer, p < 0.001; Hashimoto vs. follicular cancer, p < 0.001; control group vs. papillary cancer, p < 0.001; control group vs. follicular cancer, p < 0.001. Serum anti-TPO and anti-TG were higher in Hashimoto group as compared with control group (p < 0.001), whereas fT4 was lower (p = 0.003). Within each group of patients, there were no significant differences for trace element concentrations between untreated patients and patients on or off treatment. In particular, we did not find any differences between patients with Hashimoto disease who presented hypothyroidism, subclinical hypothyroidism, or Hashimoto patients being euthyroid, in respect of any trace element or any other parameter connected with antioxidant status. Similarly, there was no difference for these parameters between patients with Hashimoto disease treated previously with LT4 and patients newly diagnosed for this disease (results not shown). However, the former ones had higher FRAP level than the latter (Fig. 2).
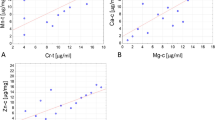
In the group of patients with papillary carcinoma, we found a statistically significant higher Cu concentration compared with control group and patients with Hashimoto disease, p < 0.020 and p < 0.010, respectively. In the same groups, the parameter of Zn/Cu ratio indicated reciprocally arranged statistically significant differences (Fig. 3). No other differences among patient groups were discovered in respect of remaining parameters.
For the group of papillary cancer patients, there was a negative correlation between lag time since thyroid operation and GPX3 activity (n = 25, R s = −0.522, p = 0.007, Fig. 4). We did not find such correlation for follicular cancer patients. We did not find any other associations between clinical records and parameters under study. The revealed correlations between age and other parameters were summarised in Table 3. No correlations with age were found in control group and patients with papillary cancer. Only for patients with follicular cancer, there was a strong positive correlation between age and FRAP. The sex hormones did not differ significantly between control group and patients with Hashimoto disease (results not shown). They also did not correlate with Zn and Cu. We attempted to describe complex interactions among sex hormones, selenium status parameters, and thyroid function indices using multivariate statistical approach in our earlier work [18].
Discussion
Thyroid-stimulating hormone directly regulates thyroid function in numerous ways, including generation of reactive oxygen intermediates, which occur in relatively high concentrations in the gland. On the other hand, the interaction between TSH and expression of antioxidant selenoenzyme glutathione peroxidase in thyrocytes was also demonstrated [19]. From thyroid diagnostics' point of view, TSH is a sensitive parameter, the changes of which reflect the abnormality of gland function. The lower values of TSH in cancer patients as compared with control group were in accordance with our expectations, as they simply expressed the effects of maintained suppressive therapy with LT4. In turn, persistently elevated TSH levels in some of Hashimoto patients indicate subclinical hypothyroidism, which is a typical clinical manifestation in the course of this disease [20]. The increase of TSH concentration is relevant for predicting the development of gland impairment. Taken together, aforementioned findings consist biochemical confirmation of either thyroid dysfunction or the course of medical treatment.
Being aware that thyroid function is mainly influenced by the underlying thyroid disease, we claim that the variations in trace element concentrations may either contribute to this gland disturbance or be implicated during the course of disease. To which extent, it may depend on the type of disturbance. The mutual interaction between thyroid physiology and trace elements presumably includes thyroid hormones, which induced alterations in trace element bioavailability and distribution and, conversely, trace element influence on thyroid hormones secretion and activity [21]. Several studies confirmed low erythrocyte zinc concentration in hyperthyroidism, caused by inhibition of zinc enzyme carbonic anhydrase-I synthesis in erythrocytes at high concentrations of thyroid hormones [22–24]. As erythrocytes have long half-life, zinc concentration in erythrocytes is regarded as a suitable marker for distinguishing between preexisting and transient hyperthyroidism, whereas the clinical implications and the use of the changes of serum Cu and Zn as a diagnostic tool for evaluation of different thyroid status are still a controversial issue, and the influence of these elements (Cu, Zn) on cancer pathogenesis is also equivocal. Lack of differences for Cu, Zn, and Zn/Cu ratio among control group, Hashimoto patients, and follicular cancer patients in this study is consistent with the results of Chen et al. [25], who also found no significant difference for these parameters among women with altered thyroid status. Similarly, Aihara et al. [26] did not observe a significant difference in plasma zinc levels between patients with thyroid diseases (hyperthyroidism, hypothyroidism, euthyroidism with previous hyper- or hypothyroidism) and healthy controls. According to Erdal et al. [27], there were no significant differences for Zn and Cu between healthy controls and patients with subclinical hypothyroidism. Moncayo et al. [28] failed to demonstrate any significant association between serum Zn levels and immunogenic thyroid disease or subacute thyroiditis. Furthermore, Al-Sayer et al. [29] revealed the restoration of previously lower serum zinc levels in patients with cancer after surgical removal of the tumour. After excision of cancerous thyroid tissue, the serum zinc levels in patients equalised those in normal subjects.
In present study, we did not observe in both groups of cancer patients any direct differences related to histologic subtype of tumour. However, in contrast to the patients with follicular cancer, both parameters, serum Cu and Zn/Cu ratio, were able to discriminate between patients with papillary carcinoma and subjects from control group as well as patients with Hashimoto disease. One hypothetical explanation for higher serum Cu concentration in papillary cancer patients is the disturbance in copper-chelating amino acid metabolism and the shift between copper ultrafilterable fraction and protein bound due to the course of the disease. This requires further studies to be clarified, but it is worth to note that Kucharzewski et al. [30] reported significantly increased copper level in whole blood of patients with thyroid carcinoma.
With only one exception (selenium in patients with Hashimoto disease), there was no correlation between trace elements and age, which corresponds well with results reported by other authors [28, 31]. The positive association between age and Se, GPX3, and FRAP in Hashimoto patients may indicate the growth of oxidative stress with course of this disease (see also Fig. 2). The same explanation may be applied to the positive association between age and FRAP in patients with follicular cancer. On the other hand, negative correlation between lag time since thyroid operation and GPX3 activity in the group of papillary cancer patients points to either lesser stimulation of enzymatic antioxidant defence in those patients or depletion of selenium stores following aging of patients.
A few investigators claimed that low Se could have diagnostic value for thyroid cancer development [32, 33]. Indeed, Kucharzewski et al. [30] found decreased whole blood selenium levels in thyroid carcinomas. Recently, Moncayo et al. [28] revealed significantly decreased serum selenium levels in patients with follicular and papillary thyroid carcinoma and in subjects with subacute silent thyroiditis. Furthermore, Erdal et al. [27] observed significantly lower basal levels of serum selenium in patients with subclinical hypothyroidism as compared with control group. In a similar fashion, other authors reported lower values of this parameter (or erythrocyte selenium) in patients with hyperthyroidism [23, 33–35].
In contrast to aforementioned results, but in accordance with our previous reports [36, 37], we did not find any differences for serum selenium or for selenium/other trace element ratios between studied groups. Hence, we were not able to confirm selenium deficiency (at least on the level reflected by serum Se and GPX3) in patients with Hashimoto disease (even in those with subclinical or overt hypothyroidism), nor in cancer patients. Other study reported no difference for erythrocyte selenium between groups of hyperthyroid, hypothyroid, critical (with one of thyroid hormones abnormal), and normal patients [38]. The possible reasons for the apparent discrepancies between these findings and the observations of other authors are not fully explained, but—as we asserted previously—the difference for calculated selenium intake between patients and control group is extremely tiny and several other confounding factors (e.g., differences in the stage of pathology, genetic predisposition) may also influence selenium status [18]. Other reasons, which yielded discrepant results, may be also related with a selection bias of patients and different laboratory methods used. Serum selenium did not correlate with measures of thyroid function, which is in accord with results of Thomson et al. [39] who also failed to show any significant associations between plasma Se and measures of thyroid status (TSH, T4, T3) in New Zealand residents.
This study has some limitations. First of all, it must be emphasised that the methods used for determining Se, Cu, and Zn status do not give sufficient indication of the their availability, tissue distribution, and mechanisms of homeostasis within the human organism. With more adequate measures of their function and status, e.g., selenoprotein P, ceruloplasmin, or zincuria, for Se, Cu, and Zn, respectively, one may expect further improvement in evaluating their influence on thyroid metabolism efficacy and disturbances in health and disease. Secondly, we did not have detailed information about dietary habits of subjects or the influence of dietary intake on trace element status, but all subjects declared to consume ordinary diet, based on staple food. Thirdly, the limited number of patients studied implicates caution in drawing final considerations. More extensive and systematic studies, including animal experimental models, should be devised to provide diagnostic or prognostic relevance to the alterations in the trace elements copper and zinc. However, it must be also borne in mind that it is not entirely possible to apply the results obtained in animal studies, based on chemically induced thyroid carcinogenesis, to much more complex pathological human thyroid tissues.
Nevertheless, both data from the literature as well as from our study support hypothesis of indirect involvement of Cu and Zn in thyroid regulation. For selenium, whose close biochemical ties with thyroid metabolism are well established, lack of simple correlation between its serum level and thyroid indices implies the need for further research on other selenium status parameters more adequately depicting changes in endocrine system.
References
Köhrle J, Brigelius-Flohé R, Böck A et al (2000) Selenium in biology: facts and medical perspectives. Biol Chem 381:849–864
Krupanidhi S, Sreekumar A, Sanjeevi CB (2008) Copper & biological health. Indian J Med Res 128:448–461
Prasad AS (2008) Clinical, immunological, anti-inflammatory and antioxidant roles of zinc. Exp Gerontol 43:370–377
Brown KM, Arthur JR (2001) Selenium, selenoproteins and human health: a review. Public Health Nutr 4:593–599
Arnér ES (2009) Focus on mammalian thioredoxin reductases—important selenoproteins with versatile functions. Biochim Biophys Acta 1790:495–526
Howie AF, Walker SW, Akesson B, Arthur JR, Beckett GJ (1995) Thyroidal extracellular glutathione peroxidase: a potential regulator of thyroid hormone synthesis. Biochem J 308:713–717
Köhrle J, Jakob F, Contempré B, Dumont JE (2005) Selenium, the thyroid, and the endocrine system. Endocr Rev 26:944–984
Gereben B, Zavacki AM, Ribich S, Kim BW, Huang SA (2008) Cellular and molecular basis of deiodinase-regulated thyroid hormone signaling. Endocr Rev 29:898–938
Prasad AS (1995) Zinc: an overview. Nutrition 11:93–99
Henkin RI (1976) Trace metals in endocrinology. Med Clin North Am 60:779–797
Neve J (1992) Clinical implications of trace elements in endocrinology. Biol Trace Elem Res 32:173–185
Ozata M, Salk M, Aydin A, Sayin S, Oktenli C et al (1999) Iodine and zinc, but not selenium and copper, deficiency exists in a male Turkish population with endemic goiter. Biol Trace Elem Res 69:211–216
Galan P, Briançon S, Favier A, Bertrais S, Preziosi P et al (2005) Antioxidant status and risk of cancer in the SU.VI.MAX study: is the effect of supplementation dependent on baseline levels? Br J Nutr 94:125–132
Benzie IFF, Strain JJ (1996) The ferric reducing ability of plasma (FRAP) as a measure of “antioxidant power”: the FRAP assay. Anal Biochem 239:70–76
Zagrodzki P, Nicol F, McCoy MA et al (1998) Iodine deficiency in cattle: compensatory changes in thyroidal selenoenzymes. Res Vet Sci 64:209–211
Neve J, Chammart S, Molle L (1987) Optimization of a direct procedure for the determination of selenium in plasma and erythrocytes using Zeeman effect atomic absorption spectroscopy. Trace Elem Anal Chem Med Biol 4:349–358
Zagrodzki P, Bartoń H, Walas S et al (2007) Selenium status indices, laboratory data, and selected biochemical parameters in end stage renal disease patients. Biol Trace Elem Res 116:29–42
Zagrodzki P, Przybylik-Mazurek E (2010) Selenium and hormone interactions in female patients with Hashimoto disease and healthy subjects. Endocr Res 35:24–34
Beckett GJ, Arthur JR (2005) Selenium and endocrine systems. J Endocrinol 184:455–465
Fatourechi V (2000) Demystifying autoimmune thyroid disease. Which disorders require treatment? Postgrad Med 107:127–134
Zhang F, Liu N, Wang X, Zhu L, Chai Z (2004) Study of trace elements in blood of thyroid disorder subjects before and after 131I therapy. Biol Trace Elem Res 97:125–134
Lao TT, Chin RK, Swaminathan R, Panesar NS, Cockram CS (1987) Erythrocyte zinc in differential diagnosis of hyperthyroidism in pregnancy: a preliminary report. Br Med J 294:1064–1065
Tiran B, Lorenz O, Tiran A, Buchinger W, Eber O (1993) Comparison of direct versus indirect determination of zinc concentration in erythrocytes in euthyroid and hyperthyroid subjects. Eur J Clin Chem Clin Biochem 31:239–244
Liu N, Liu P, Xu Q, Zhu L, Zhao Z et al (2001) Elements in erythrocytes of population with different thyroid hormone status. Biol Trace Elem Res 84:37–43
Chen MD, Song YM, Tsou CT, Lin WH, Sheu WHH (1999) Leptin concentration and the Zn/Cu ratio in plasma in women with thyroid disorder. Biol Trace Elem Res 75:99–105
Aihara K, Nishi Y, Hatano S, Kihara M, Yoshimitsu K et al (1984) Zinc, copper, manganese, and selenium metabolism in thyroid disease. Am J Clin Nutr 40:26–35
Erdal M, Sahin M, Hasimi A et al (2008) Trace element levels in Hashimoto thyroiditis patients with subclinical hypothyroidism. Biol Trace Elem Res 123:1–7
Moncayo R, Kroiss A, Oberwinkler M et al (2008) The role of selenium, vitamin C, and zinc in benign thyroid diseases and of selenium in malignant thyroid diseases: low selenium levels are found in subacute and silent thyroiditis and in papillary and follicular carcinoma. BMC Endocr Disord 8:2–13
Al-Sayer H, Mathew TC, Asfar S, Khourshed M, Al-Bader A et al (2004) Serum changes in trace elements during thyroid cancers. Mol Cell Biochem 260:1–5
Kucharzewski M, Braziewicz J, Majewska U, Gózdz S (2003) Copper, zinc, and selenium in whole blood and thyroid tissue of people with various thyroid diseases. Biol Trace Elem Res 93:9–18
Clark NA, Teschke K, Rideout K, Copes R (2007) Trace element levels in adults from the west coast of Canada and associations with age, gender, diet, activities, and levels of other trace elements. Chemosphere 70:155–164
Glattre E, Thomassen Y, Thoresen SO (1989) Prediagnostic serum selenium in a case-control study of thyroid cancer. Int J Epidemiol 18:45–49
Jellum E, Andersen A, Lund-Larsen P, Theodorsen L, Orjasaeter H (1993) The JANUS serum bank. Sci Total Environ 139–140:527–535
Beckett GJ, Peterson FE, Choudhury K et al (1991) Inter-relationships between selenium and thyroid hormone metabolism in the rat and man. J Trace Elem Electrolytes Health Dis 5:265–267
Reglinski J, Smith WE, Wilson R et al (1992) Selenium in Graves' disease. Clin Chim Acta 211:189–190
Zagrodzki P, Nicol F, Arthur JR, Słowiaczek M (2001) Selenoproteins in human thyroid tissues. Biofactors 14:223–227
Zagrodzki P, Nicol F, Arthur JR et al (2010) Selenoenzymes, laboratory parameters, and trace elements in different types of thyroid tumour. Biol Trace Elem Res 134:25–40
Liu N, Liu P, Xu Q et al (2001) Elements in erythrocytes of population with different thyroid hormone status. Biol Trace Elem Res 84:37–43
Thomson CD, McLachlan SK, Grant AM, Paterson E, Lillico AJ (2005) The effect of selenium on thyroid status in a population with marginal selenium and iodine status. Brit J Nutr 94:962–968
Acknowledgements
This work was supported in part by grant no. K/ZDS/000594.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Przybylik-Mazurek, E., Zagrodzki, P., Kuźniarz-Rymarz, S. et al. Thyroid Disorders—Assessments of Trace Elements, Clinical, and Laboratory Parameters. Biol Trace Elem Res 141, 65–75 (2011). https://doi.org/10.1007/s12011-010-8719-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-010-8719-9