Abstract
In this study, antibacterial effects of (+)-Medioresinol isolated from stem bark of Sambucus williamsii and its synergistic activities in combination with antibiotics such as ampicillin, cefotaxime, and chloramphenicol were tested by antibacterial susceptibility testing and checkerboard assay. (+)-Medioresinol possessed antibacterial effects against antibiotics-susceptible- or antibiotics-resistant strains. Most of combinations between (+)-Medioresinol and each antibiotic showed synergistic interaction (fractional inhibitory concentration index ≤0.5) against bacterial strains including antibiotics-resistant Pseudomonas aeruginosa. Furthermore, the antibiofilm effect of (+)-Medioresinol alone or in combination with each antibiotic was investigated. The results indicated that not only (+)-Medioresinol but also its combination with each antibiotic had antibiofilm activities. It concludes that (+)-Medioresinol has potential as a therapeutic agent and adjuvant for treatment of bacterial infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, infectious diseases have become the world’s leading cause of premature deaths [1]. The wide use of antibiotics in the treatment of bacterial infections has led to the emergence and spread of resistant strains [2]. Due to the emergence of antibiotic resistant bacteria, the search for new antimicrobial substances from natural sources including plants is important. In addition, it is now standard clinical practice to use a combination of two or more antibiotics with different mechanisms of action in an attempt to prevent the development of antibiotic resistance and improve the outcome of therapy [3]. Several studies concerning the enhanced effect of antibiotics in combination with natural compounds have been reported [4, 5], and there is a clinical interest in the use of combinations of natural products and antibiotics to improve the spectrum of drug activity.
Biofilm is also related with the conventional antibiotics resistance problem [6, 7]. Bacterial cells adhere to damaged tissue and medical devices including catheters, prosthetic heart valves, artificial hips, and contact lenses and form biofilm. Bacteria-produced biofilm is difficult to be eradicated by antibiotic treatment due to their inherent antibiotic resistance, protection from host responses, and facilitation of bacterial communication leading to the expression of virulence determinants [8].
Phytochemicals, which are the non-nutrient plant compounds, have been known to possess a variety of biological activities by protecting chronic disease [9]. (+)-Medioresinol is a furofuran-type lignan derivative from the stem bark of Sambucus williamsii, which is a folk medicinal plant. The genus Sambucus, widely distributed in Europe, Asia, and North Africa, has been used in traditional medicine as an analgesic, antivirus [10], anti-inflammatory [11], homoeostatic, and diuretic drug which are used to treat bruises, fractures, and edema [12]. Furofuran lignans have also been reported to exhibit various biological activities, including antifungal, anti-inflammatory, antimalarial activities; the inhibition of cyclic AMP phosphodiesterase; and the DNA cleavage effect [13]. In our previous study, (+)-Medioresinol showed antifungal activity with almost no hemolysis [14].
In this study, we investigated the in vitro antibacterial and antibiofilm effects of (+)-Medioresinol alone or in combination with conventional antibiotics (ampicillin, cefotaxime, and chloramphenicol) against bacterial strains.
Materials and Methods
Extraction and Isolation of (+)-Medioresinol from Sambucus williamsii
The air-dried stem bark of Sambucus williamsii (840 g) was cut and extracted with methanol (MeOH) at 80 °C for 4 h. The MeOH extract (57.10 g) was suspended in water and then partitioned sequentially with equal volumes of dichloromethane (CH2Cl2), ethyl acetate (EtOAc), and n-butanol (n-BuOH). The CH2Cl2 fraction (4.2 g) was subjected to column chromatography over a silica gel by eluting it with hexane:EtOAc (100:1→80:1→50:1→20:1→10:1→1:1) and CHCl3/MeOH/H2O (30:10:1→1:1:0.1→MeOH only) gradient system. Based on their TLC pattern, the fractions were combined to yield subfractions, which were designated D1–D8. The subgroup, D6 (1.27 g), was then purified by column chromatography on a silica gel eluting it with a CHCl3/MeOH/Me2CO/H2O (50:4:2:0.3) and was followed with repeated gel filtration column chromatography (MCI gel, MeOH/H2O = 3:8) to give (+)-Medioresinol (7.8 mg). The physicochemical data including the 1H NMR, 13C NMR, and HSQC of (+)-Medioresinol were identical to those reported in the literature [15, 16].
Bacterial Strains and Culture Medium
Enterococcus faecium (ATCC 19434), Staphylococcus aureus (ATCC 25923), Propionibacterium acnes (ATCC 6919), Escherichia coli O-157 (ATCC 43895), E. coli (ATCC 25922), and Pseudomonas aeruginosa (ATCC 27853) were obtained from the American Type Culture Collection (ATCC) (Manassas, VA, USA). Before use, all bacteria were stored in 30 % glycerol and frozen at −70 °C. The bacteria were cultured in Mueller–Hinton broth (MHB) and Mueller–Hinton agar (Difco Laboratories, Baltimore, MD, USA) and incubated at 37 °C. Cell growth was monitored by measuring the optical density (OD) at 620 nm.
Antimicrobial Susceptibility Assay
Bacterial strains were cultured in a MHB and the cell suspensions were adjusted to obtain standardized populations by measuring the turbidity with a spectrophotometer (DU530, Beckman, Fullerton, CA, USA). The bacterial strains at mid-log phase (1 × 106/mL) were inoculated into MHB and 0.1 mL was dispensed per well into 96-well microtiter plates. Susceptibility tests were performed by a twofold standard broth microdilution of the test compounds including (+)-Medioresinol, ampicillin, cefotaxime, and chloramphenicol following the Clinical and Laboratory Standards Institute (CLSI) guideline [17]. After 18 h of incubation at 37 °C, the minimum inhibitory concentration (MIC) required to prevent the growth of a given test organism was determined. The growth was assayed with a microtiter ELISA Reader (Molecular Devices Emax, CA, USA) by monitoring the OD at 620 nm.
Combination Assay
The MICs of each antibiotic alone or in combination with (+)-Medioresinol were determined by broth microdilution method in accordance with the National Committee for Clinical Laboratory Standards by using a cation-adjusted MHB modified for a broth microdilution checkerboard procedure [18, 19]. For the double treatment, a two-dimensional checkerboard with twofold dilutions of each drug was used for the study. A checkerboard with twofold dilutions of (+)-Medioresinol and the antibiotics (ampicillin, cefotaxime, and chloramphenicol) was set up as described above for the combined treatment. Control wells containing medium were included in each plate. Each test was performed in triplicate. For the first clear well in each row of the microtiter plate containing all antimicrobial agents, the fractional inhibitory concentration (FIC) was calculated as follows: FIC of drug A (FIC A) = MIC of drug A in combination / MIC of drug A alone, and FIC of drug B (FIC B) = MIC of drug B in combination / MIC of drug B alone [20]. The FIC index (FICI), calculated as the sum of each FIC, was interpreted as follows: FICI ≤ 0.5, synergy; 0.5 < FICI ≤ 4, no interaction; 4 < FICI, antagonism [21].
Determination of Biofilm Formation by the Tissue Culture Plate Method
To determine the efficacy of (+)-Medioresinol in the elimination of preformed biofilms, the tissue culture plate (TCP) method was carried out with few modifications [22]. Bacterial strains were cultured in a brain–heart infusion (BHI) broth and the cell suspensions were diluted with BHI broth containing 2 % sucrose. Individual wells in sterile, polystyrene, 96-well-flat bottom TCPs were filled with 190 μL of the bacterial populations (1 × 106/mL). After 18 h of overnight culture, 10 μL of (+)-Medioresinol, conventional antibiotics, and their combinations were added and the final concentration was the same for each of the MICs (×1, ×4, ×10) or FICs (×1, ×4, ×10). The preformed biofilms of the cells were incubated for 18 h at 37 °C and the wells were washed four times with phosphate-buffered saline to remove any free-floating bacteria. Biofilms formed by adherent organisms in the plate were fixed with sodium acetate (2 %) and stained with Crystal violet (0.1 %, w/v). Excess stain was rinsed thoroughly with deionized water and then the plates were left to dry. After drying, 95 % ethanol was added to the wells and the OD580 of the stained adherent bacteria was measured with a microtiter ELISA Reader. The OD was considered as an index of bacterial adherence to the surface and the formation of biofilms. The percentage of biofilm inhibition was calculated using the following equation: [1 − (OD580 of cells treated with (+)-Medioresinol / OD580 of non-treated control) × 100] [23]. Experiments were performed in triplicate, and the data were averaged and the standard deviation was calculated.
Results
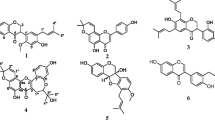
Purification and Structure Analysis of (+)-Medioresinol
We isolated the (+)-Medioresinol from the CH2Cl2 soluble fraction of the MeOH extract of Sambucus williamsii by repeated silica gel and column chromatography. The chemical structure of this compound was determined as (+)-Medioresinol by comparing their spectroscopic data (1H NMR, 13C NMR, HSQC) with those reported in the literature [15, 16].
Antibacterial Activity of (+)-Medioresinol Against Bacterial Strains
In this study, ampicillin, cefotaxime, and chloramphenicol were used to investigate combination effect with (+)-Medioresinol. Ampicillin and cefotaxime are β-lactam and cephalosporin antibiotics, respectively. They exert antibacterial effect by binding to penicillin-binding protein which is essential for the cross-linking of peptidoglycan, a major component of the bacterial cell wall [24, 25]. Chloramphenicol interferes with the production of functional proteins by acting as 50S ribosome inhibitors [24]. To examine the antimicrobial activity of (+)-Medioresinol and antibiotics, the antimicrobial susceptibility testing was conducted against E. faecium, S. aureus, P. acnes, E. coli O-157, E. coli, and P. aeruginosa using the CLSI method. The result showed that (+)-Medioresinol, with MIC values of 2.5–20.0 μg/mL, had remarkable antibacterial activity compared to antibiotics. The bacterial strains showed MIC values ranging from 0.6 to 200.0 μg/mL for ampicillin, 0.2–10.0 μg/mL for cefotaxime, and 2.5–100.0 μg/mL for chloramphenicol (Table 1). Among gram-negative bacteria, P. aeruginosa was less susceptible than E. coli to antibiotics and showed a high level of intrinsic resistance to ampicillin and chloramphenicol. However, (+)-Medioresinol was active against P. aeruginosa.
Synergistic Effect Between (+)-Medioresinol and Antibiotics
To investigate the synergistic effects between (+)-Medioresinol and conventional antibiotics such as ampicillin, cefotaxime, and chloramphenicol, the checkerboard method was done. The synergistic effect was evaluated in terms of a FICI between (+)-Medioresinol and each antibiotic. The combined activities of (+)-Medioresinol and each antibiotic from the in vitro checkerboard interactions against the bacterial strains were summarized in Table 2. All combinations showed the synergistic interactions against P. acnes and even antibiotics-resistant P. aeruginosa, while all combinations against E. faecium exhibited no interactions. Antagonism was not recorded for all the combinations. The combination of (+)-Medioresinol–cefotaxime and (+)-Medioresinol–chloramphenicol was boosting the antibacterial effect against E. coli, and the combination of (+)-Medioresinol–ampicillin and (+)-Medioresinol–cefotaxime showed a synergistic effect against S. aureus. Among each combination, (+)-Medioresinol was specifically synergistic with cefotaxime.
Antibiofilm Effects of (+)-Medioresinol Alone and in Combination with Antibiotics
To investigate the antibiofilm effects of agents, bacterial cells were grown to form biofilms, and then were treated with (+)-Medioresinol, conventional antibiotics, and their combinations. The antibiotic concentration was the MIC (×1, ×4, ×10) or the FIC (×1, ×4, ×10), and each treatment showed an inhibitory effect on preformed biofilm (Table 3). The results indicated that MIC of (+)-Medioresinol showed percentage of biofilm inhibition less than 30 % on the most part. Furthermore, the result showed that as antibiotic concentration increased, inhibitory effect on preformed biofilm increased. The degree of the biofilm inhibition by each treatment was different according to the bacterial strains.
Discussion
Antibiotic resistance is a worldwide public health problem that continues to grow. Seventy percent of bacteria that cause infections in hospitals are resistant to at least one of the conventional drugs most commonly used for treatment. Recently, phytochemicals, an enormous array of secondary metabolites, are considered as novel antibiotic agents [26]. Phytochemicals have also produced synergistic effects in combination with conventional antibiotics, and several studies have reported such findings [4, 5].
In this study, we investigated the antibacterial effect of (+)-Medioresinol and its combination effect with conventional antibiotics, such as ampicillin, cefotaxime, and chloramphenicol. Antibacterial susceptibility testing showed that (+)-Medioresinol caused a significant inhibitory effect against antibiotics-susceptible and antibiotics-resistant strains, such as P. aeruginosa. Combination therapy is used to expand the antimicrobial spectrum, to minimize toxicity, to prevent the emergence of resistant organisms during therapy, and to obtain synergistic antimicrobial activity [27]. Thus, to permit full exploitation of (+)-Medioresinol as new antimicrobial agents, it is important to investigate their interaction with the most common clinically used antibiotics in vitro. To examine the synergistic effect of a combination of two or more compounds, the checkerboard test is one of the most commonly used techniques and is relatively easy to apply [28]. The results of these drug combinations were classified as synergistic, antagonistic, or without influence on the antimicrobial activity if the effect of the combined drugs was better than, worse than, or the same as that of the individual drug activities, respectively. These results demonstrated that (+)-Medioresinol had potent antibacterial activity both alone and in combinations with each antibiotic against bacterial strains including antibiotics-resistant P. aeruginosa. Recently, P. aeruginosa remains a major pathogen due to intrinsic resistance, mainly caused by impermeable outer membrane and multidrug efflux pumps. They are especially important in critical care and burn units, as well as in patients with cystic fibrosis [29]. The intrinsic resistance of P. aeruginosa to antibiotics could be overcome using some compounds that permeabilize the outer membrane [30, 31]. The observed synergism in this study might be related to change in P. aeruginosa membrane permeability by (+)-Medioresinol. Although the mechanism of synergy needs further investigation, the synergistic effect between (+)-Medioresinol and antibiotics against antibiotics-resistant P. aeruginosa indicated that (+)-Medioresinol could restore the antibacterial activity of antibiotics (ampicillin, chloramphenicol) and represent a novel agent potentially valuable as an adjuvant for antimicrobial chemotherapy. In addition, the Crystal violet assay demonstrated that (+)-Medioresinol, each of the antibiotics, and their combinations exerted an antibiofilm effect against the bacterial organisms in a dose-dependent manner.
In conclusion, this study showed the antibacterial effects of (+)-Medioresinol and its synergistic interaction with each antibiotic. Additionally, we also observed the antibiofilm activity of (+)-Medioresinol and its combinations with conventional antibiotics against preformed biofilm. Therefore, this study suggests that (+)-Medioresinol has the potential as a therapeutic agent and adjuvant for the treatment of bacterial infectious diseases.
References
Mesaros, N., Nordmann, P., Plesiat, P., Van Roussel-Delvallez, M., Eldere, J., Glupczynski, Y. V., et al. (2007). Clinical Microbiology and Infection, 13, 560–5787.
Nishanth Kumar, S., Siji, J. V., Nambisan, B., & Mohandas, C. (2012). World Journal of Microbiology and Biotechnology, 28, 3143–3150.
Beringer, P. M. (1999). Current Opinion in Pulmonary Medicine, 5, 371–377.
Chung, P. Y., Parasakthi, N., & Chung, L. Y. (2011). Annals of Clinical Microbiology and Antimicrobials, 10, 1–6.
Lee, Y., Jang, K., & Cha, J. (2012). Journal of Biomedicine and Biotechnology, 618081, 1–7.
Hoiby, N., Bjarnsholt, T., Givskov, M., Molin, S., & Ciofu, O. (2010). International Journal of Antimicrobial Agents, 35, 322–332.
Lynch, S. V., Dixon, L., Benoit, M. R., Brodie, E. L., Keyhan, M., Hu, P., et al. (2007). Antimicrobial Agents and Chemotherapy, 51, 3650–3658.
Liaqat, I., & Sabri, A. N. (2008). Journal of Basic Microbiology, 49, 1–10.
Boyer, J., & Liu, R. H. (2004). Nutrition Journal, 3, 5.
Zakay-Rones, Z., Varsano, N., Zlotnik, M., Manor, O., Regev, L., Schlesinger, M., et al. (1995). Journal of Alternative and Complementary Medicine, 1, 361–369.
Ahmadiani, A., Fereidoni, M., Semnanian, S., Kamalinejad, M., & Saremi, S. (1998). Journal of Ethnopharmacology, 61, 229–235.
Xie, F., Wu, C. F., Zhang, Y., Yao, X. S., Cheung, P. Y., Chan, A. S., & Wong, M. S. (2005). Biological and Pharmaceutical Bulletin, 28, 1879–1885.
Yan, Z. H., Yang, C. H., Wu, X. H., & Xie, Y. Y. (2004). Chinese Chemical Letters, 15, 408–410.
Hwang, J. H., Hwang, I. S., Liu, Q. H., Woo, E. R., & Lee, D. G. (2012). Biochimie, 94, 1784–1793.
Li, C. Y., & Li, Y. C. (1999). Acta Pharmaceutica Sinica, 34, 605–607.
Zhou, L. X., & Dind, Y. (2000). Zhongguo Zhong Yao Za Zhi, 25, 541–543.
CLSI. (2005). Performance standards for antimicrobial susceptibility testing. Wayne: CLSI.
Eliopoulos, G. M., & Moellering, R. C. (1991). Antimicrobial combinations. In V. Lorian (Ed.), Antibiotics in laboratory medicine (pp. 432–492). Baltimore: Williams & Wilkins.
NCCLS. (2003) Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. National committee for clinical Laboratory Standards USA M7-A6.
Pankey, G. A., & Ashcraft, D. S. (2005). Antimicrobial Agents and Chemotherapy, 49, 2959–2964.
Odds, F. C. (2003). Journal of Antimicrobial Chemotherapy, 52, 1.
Christensen, G. D., Simpson, W. A., Younger, J. J., Baddour, L. M., Barrett, F. F., Melton, D. M., et al. (1985). Journal of Clinical Microbiology, 22, 996–1006.
Wei, G. X., Campagna, A. N., & Bobek, L. A. (2006). Journal of Antimicrobial Chemotherapy, 57, 1100–1109.
Kohanski, M. A., Dwyer, D. J., & Collins, J. J. (2010). Nature Reviews Microbiology, 8, 423–435.
William, F., Marshall, M. D., Janis, E., & Blair, M. D. (1999). Mayo Clinic Proceedings, 74, 187–195.
An, J., Zuo, G. Y., Haob, X. Y., Wanga, G. C., & Li, Z. S. (2011). Phytomedicine, 18, 990–993.
Gradelski, E., Valera, L., Bonner, D., & Fung-Tomc, J. (2001). Antimicrobial Agents and Chemotherapy, 45, 3220–3222.
White, R. L., Burgess, D. S., Manduru, M., & Bosso, J. A. (1996). Antimicrobial Agents and Chemotherapy, 40, 1914–1918.
Mushtaq, S., Ge, Y., & Livermore, D. M. (2004). Antimicrobial Agents and Chemotherapy, 48, 3086–3092.
Hancock, R. E. (1985). Antibiotics and Chemotherapy, 36, 95–102.
Buyck, J. M., Plésiat, P., Traore, H., Vanderbist, F., Van Tulkens, P. M., & Bambeke, F. (2012). Clinical Infectious Diseases, 55, 534–542.
Acknowledgments
This work was supported by the National Research Foundation of Korea grant funded by the Korea government (MEST) (no. 2008-0062618).
Author information
Authors and Affiliations
Corresponding author
Additional information
Ji Hong Hwang and Hyemin Choi contributed equally to this work and should be considered co-first authors.
Rights and permissions
About this article
Cite this article
Hwang, J.H., Choi, H., Hwang, Is. et al. Synergistic Antibacterial and Antibiofilm Effect Between (+)-Medioresinol and Antibiotics In Vitro. Appl Biochem Biotechnol 170, 1934–1941 (2013). https://doi.org/10.1007/s12010-013-0351-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12010-013-0351-7