Abstract
Background
Although metal-on-metal (MoM) bearing surfaces provide low rates of volumetric wear and increased stability, evidence suggests that certain MoM hip arthroplasties have high rates of complication and failure. Some evidence indicates that women have higher rates of failure compared with men; however, the orthopaedic literature as a whole has poorly reported such complications stratified by gender.
Questions/purposes
This systematic review aimed to: (1) compare the rate of adverse local tissue reaction (ALTR); (2) dislocation; (3) aseptic loosening; and (4) revision between men and women undergoing primary MoM hip resurfacing arthroplasty (HRA).
Methods
Systematic MEDLINE and EMBASE searches identified all level I to III articles published in peer-reviewed journals, reporting on the outcomes of interest, for MoM HRA. Articles were limited to those with 2-year followup that reported outcomes by gender. Ten articles met inclusion criteria. Study quality was evaluated using the Modified Coleman Methodology Score; the overall quality was poor. Heterogeneity and bias were analyzed using a Mantel-Haenszel statistical method.
Results
Women demonstrated an increased odds of developing ALTR (odds ratio [OR], 5.70 [2.71–11.98]; p < 0.001), dislocation (OR, 3.04 [1.2–7.5], p = 0.02), aseptic loosening (OR, 3.18 [2.21–4.58], p < 0.001), and revision (OR, 2.50 [2.25–2.78], p < 0.001) after primary MoM HRA.
Conclusions
A systematic review of the currently available literature reveals a higher rate of complications (ALTR, dislocation, aseptic loosening, and revision) after MoM HRA in women compared with men. Although femoral head size has been frequently implicated as a prime factor in the higher rate of complication in women, further research is necessary to specifically probe this relationship. Retrospective studies of data available (eg, registry data) should be undertaken, and moving forward studies should report outcomes by gender (particularly complications).
Level of Evidence
Level III, therapeutic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of metal-on-metal (MoM) bearing surfaces gained popularity over a decade ago. These articulations were thought to minimize wear and subsequent osteolysis, allow for larger head sizes, and decrease dislocation rates. MoM bearing surfaces also led to the reintroduction of hip resurfacing arthroplasty (HRA), a more bone-conserving procedure, which in the past had performed poorly with metal-on-polyethylene bearing surfaces [8, 35]. At its height, the use of MoM THA and HRA accounted for approximately 35% of all hip arthroplasties with nearly 31% of HRA being implanted in women [36]. A number of studies showed low rates of dislocation and high rates of function with both MoM THA and HRA. However, other publications have shown unacceptably high rates of revision and complications (eg, adverse local tissue reaction [ALTR], osteolysis, etc) [1, 26, 30]. Furthermore, studies have indicated that women experience a higher rate of complications compared with men, particularly after HRA. However, many have speculated this is the result of differences in component sizing. Despite a vast literature describing HRA clinical outcomes, outcomes stratified by gender are limited [2, 4, 11, 12, 14, 16, 36, 38].
Underreporting of gender differences in orthopaedic outcomes is not unique to MoM arthroplasty. Several orthopaedic leaders have stressed the importance of reporting gender differences in orthopaedic studies [22, 24]. Thus, to more fully evaluate the rate of complications after MoM arthroplasty, we sought to perform a systematic review of the literature. A systematic review provides the ideal method to aggregate all available evidence in a rigorous manner, minimizing bias as well as issues surrounding insufficient sample size. It further provides insight into potential directions for new research on the topic.
The specific aims of our systematic review were to: (1) compare the rate of ALTR; (2) dislocation; (3) aseptic loosening; and (4) revision between men and women undergoing primary MoM HRA.
Search Strategy and Criteria
Our original aim was to perform a systematic review of all papers evaluating MoM hip arthroplasty (including both THA and HRA). Thus, a systematic review of peer-reviewed English language literature was conducted using the MEDLINE and EMBASE search engines on July 10, 2014 (Prospero registration number CRD42014012906). Inclusion criteria were levels I to III articles that reported clinical outcomes after primary MoM hip arthroplasty (THA or HRA) with minimum 2-year followup. Articles needed to specifically evaluate for the complications in question (ALTR, dislocation, aseptic loosening, and revision). To be included in the final analysis, outcomes needed to be reported as discrete numbers as opposed to relative risks or odds ratios. Furthermore, outcomes as well as demographic variables needed to be reported specifically by gender for both the treatment and control groups. Exclusion criteria included review articles (such as systematic reviews and meta-analyses), level IV to V evidence, no gender reporting, less than 2-year followup, and previously reported data (ie, duplicate data). In the event of a duplicate subject publication, the article with a greater number of subjects was included. The specific Boolean search term used was: ‘(((“hip resurfacing” OR “hip arthroplasty”) AND (“metal-on-metal” OR “metal on metal”)) AND English [Language])’.
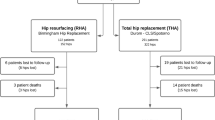
An initial search yielded 971 potential articles on MoM hip arthroplasty (THA and HRA) for inclusion (Fig. 1). Articles were screened by two independent reviewers (BDH, BJE) using the aforementioned inclusion and exclusion criteria. After our screening, the bibliographies of all included studies were screened for potential articles, which yielded four additional articles for inclusion. In total, 13 articles met inclusion criteria for our systematic review. Of the available articles, 10 discussed HRA outcomes, whereas three outlined MoM THA outcomes. Given the paucity of data evaluating MoM THA [3, 25, 28], the systematic review was narrowed to only include HRA studies. At the outset of the systematic review, the author’s hope was that pooled data evaluating clinical outcomes scores could be reviewed. However, a singular study [27] included such data, and subsequently the decision to exclude this analysis from the review was made as well.
Data Extraction
Two independent reviewers (BDH, BJE) collected data from each included article using data abstraction forms. Abstracted data included study publication year, authors, country of publication, enrollment dates, level of evidence, component type, number of patients, number of men and women, age, body mass index, surgical approach, functional outcomes scores (eg, Harris hip score), followup duration, and complications (ALTR, dislocation, aseptic loosening, and revisions) (Table 1). Study methodological quality was assessed using the Modified Coleman Methodology Score [7]. The Modified Coleman Methodology Score is a score used to evaluate a study’s methodology with scores ranging from 0 to 100. A Modified Coleman Methodology Score of “excellent” studies range from 85 to 100, good studies range from 70 to 84, fair studies range from 55 to 69, and poor studies from 0 to 55. Overall the quality of research was poor with an average Modified Coleman Methodology Score of 41.7 ± 5.9 (Table 2).
Statistical Methods
Weighted demographic data and complication rates were calculated for males and females (Tables 1, 3). To determine the effect of gender on the rates of complications, unadjusted females/males odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. The reported p values refer to a one-sided (likelihood ratio) test for difference in complication rates between genders. Probability values of < 0.05 were considered significant. A Mantel-Haenszel statistical method was used to evaluate for any heterogeneity among the included studies as well as the presence of any publication bias. For those subanalyses with possible bias, a random effects model was used. All statistical tests were performed using Review Manager (RevMan, Version 5.3; Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration; 2011).
Note on Language Use
In general, the term sex refers to biological phenomena, and gender refers to phenomena in which there might be an element of cultural overlay. In this study, it is likely that some endpoints were related to sex (such as the frequency of ALTR), whereas others almost certainly are gender (such as the frequency of revision surgery for any reason), and some are uncertain in that they may have both social and biological components. For simplicity, we use the term gender as well as gender-related terms (such as “woman” rather than “female”) throughout the article.
Results
Adverse Local Tissue Reaction
When comparing rates of ALTR between genders, our systematic review showed a higher rate of ALTR reaction in women (OR, 5.70 [2.71–11.98]; p < 0.001) (Fig. 2). A heterogeneity analysis indicated that our ALTR data were moderately uniform (I2 = 46%, p = 0.13), and thus a random effects model was used. In total, four articles reported gender differences in ALTR rates. This included a total of 9296 patients (68.7% men; n = 6389) with 66 women (2.3%) and 97 men (1.5%) experiencing an ALTR.
Dislocation
Although dislocation was a rare event in our cohort, women had to have a higher rate of dislocation compared with men (OR, 3.04 [1.2–7.5]; p = 0.02) (Fig. 3). A heterogeneity analysis indicated that our dislocation data may be affected by mild heterogeneity (I2 = 37%, p = 0.20). Dislocation rates were reported by gender in four included articles. These papers represented a total of 6565 patients (n = 4480; 68.2% men), including 10 dislocations (0.50%) occurring in women and nine dislocations (0.2%) occurring in the male cohort.
Aseptic Loosening
Women had to have higher rates of aseptic loosening compared with men (OR, 3.18 [2.21–4.58]; p < 0.001) (Fig. 4). A heterogeneity analysis indicated that our aseptic loosening data were uniform (I2 = 0%, p = 0.97). Five articles reported rates of aseptic loosening by gender. This included 11,247 patients of whom 7802 were men (69.4%). Aseptic loosening was present in 68 women (2.0%) and 54 men (0.70%).
Revision
Women demonstrated a higher rate of revision compared with men in our systematic review (OR, 2.50 [2.25–2.78], p < 0.001) (Fig. 5). A heterogeneity analysis indicated that our revision data were uniform (I2 = 8%, p = 0.36). Nine articles reported rates of aseptic loosening by gender, representing 44,713 patients including 30,778 men (68.8%). Revisions were observed in 724 women (5.2%) and in 669 men (2.2%).
Discussion
Hip arthroplasty has revolutionized the treatment of end-stage degenerative processes affecting the hip. Because this intervention has expanded its indications to higher-demand patient populations, including younger and more active individuals, there is an increasing need to develop implants with improved longevity and durability. In comparison to conventional metal-on-polyethylene bearing surfaces, MoM bearing surfaces have demonstrated diminished volumetric wear while allowing larger femoral head sizes and thereby decreased dislocation risk [8, 35]. This led to early adoption and high rates of use [31, 32, 36]. Unfortunately, data emerged demonstrating early failure and high rates of complications in certain devices [26, 30]. These complications appeared to be more common in women, although results were mixed [4, 9, 11, 14, 18]. This could in part be explained by the lack of gender-specific outcomes in the orthopaedic literature, a reporting bias called into question in recent years [22, 24]. No prior hip arthroplasty reviews have reported their data stratified by gender. Therefore, to further probe the role of gender in complication rates after MoM hip arthroplasty, we performed a systematic review to compare the rate of complications (eg, ALTR, dislocation, aseptic loosening, and revision) after primary MoM HRA. Our findings underscore the importance of reporting gender-specific outcomes.
Like with all systematic reviews, our findings are limited by the data available. In an attempt to provide a higher quality review, we included only studies of levels I through III evidence. Furthermore, given our specific aims of probing the role of gender in complication rates after MoM hip arthroplasty, we were limited by the studies that reported clinical outcomes stratified by gender, which, unfortunately, was a low number. Although it is not ideal to include retrospective literature in a pooled analysis such as this, only two of the included studies were prospective, and we thus decided to include level III studies in our analysis. Although our original intention was to include a review of both MoM THA as well as HRA, as a result of the limited research evaluating gender differences in MoM THA outcomes, we were unable to include these studies in our analysis. This too was the case with functional outcomes after either MoM THA or HRA, because a singular study reported functional outcomes by gender. Despite the attempt to include high-quality literature, the overall quality, as evidenced by our Modified Coleman Methodology Score, remained poor. Finally, perhaps the biggest limitation of our review provides the greatest opportunity for future research, namely the causative factors behind our findings of increased complications in women. Although our data have demonstrated higher rates of complications in women after MoM HRA, the cause of this finding remains elusive; unfortunately, a causative relationship cannot be explored with the data available. Suggested causes for higher rates of failure in women have included an increased incidence of metal allergy in women, gender differences in ligamentous laxity, bone quality, anatomical differences between the male and female hips, the latter having a higher prevalence of developmental dysplasia, and finally the most commonly implicated etiology is related to femoral head and acetabular component sizing (which could lead to suboptimal lubrication regimes and/or edge loading from suboptimal contact geometries) [11–13, 15, 29, 33, 34]. Of note, we could not control for component design or size, because the included studies did not provide this information in such a manner in which it could be explored. Furthermore, our heterogeneity analysis indicates that there was variable clinical heterogeneity among the studies included and the individual outcomes analyzed.
When specifically evaluating rates of ALTR between genders, our data demonstrated an increased rate of complication in women; however, a paucity of data specifically evaluating this finding exists [4, 5, 11, 23]. With the available evidence, conclusions are limited as to the cause of our observed findings. However, authors have speculated the increased rate of ALTR may be related to a number of factors including differences in femoral head-neck anatomy, acetabular anatomy (eg, hip dysplasia), femoral head size, age, component malpositioning, and component design [4, 5, 11, 12, 37]. Increased preoperative femoral head-neck ratio (HNR), particularly those greater than 1.3 (a finding more common in women), has been shown to be a risk factor for subsequent ALTR and failure. This was thought to be the result of downsizing of the femoral heads at the time of surgery, leading to greater rates of impingement and edge loading [12]. Acetabular anatomy has also been implicated as a cause of failure in HRA, because Glyn-Jones et al. demonstrated higher rates of failure in patients with hip dysplasia, a more common diagnosis in women [11]. Furthermore, malpositioned acetabular components (particularly those cups with increased abduction angles) and resultant edge loading are felt to have an association with ALTR [5]. Perhaps the most consistently implicated factor, in the studies included in this particular analysis, was component size. Smaller femoral heads have been shown in numerous series to be related to high rates of ALTR, a finding corroborated by the Australian Arthroplasty Registry [4, 5, 11, 12, 31]. However, although it is tempting to attribute the relationship of increased rates of ALTR solely to smaller head sizes in women, the Canadian Arthroplasty Registry demonstrated an independent effect of gender on increased rates of ALTR regardless of head size [4].
Although an uncommon complication after primary MoM HRA, dislocation appeared to occur more frequently in women in the few studies reporting this outcome by gender [2, 5, 14, 19]. Authors of the included studies provided little discussion of gender differences in dislocation rates; however, much has been made of the smaller femoral head sizes in women as it relates to other complications (eg, revision and ALTR) [4, 5, 11, 12, 31]. Similarly, as previously mentioned, authors have demonstrated the influence of HNR as well as acetabular geometry on MoM HRA impingement, altered kinematics, and subsequent failure. With the given data we are unable to determine if gender is an independent risk factor for dislocation after HRA because we could not control for head size in our analysis. In the THA literature, however, it has clearly been shown that larger heads have lower rates of dislocation [20, 21]. Another potential cause of dislocation may be related to ALTR, a more common complication seen in women. Damage to the soft tissue envelope of the hip, and particularly the abductor musculature, has been implicated as a potential cause of increased dislocation in the setting of ALTR [6, 10]. Moving forward, if the relationship between gender and dislocation is real, future studies should explore causative factors for a potential increased rate of dislocations in women.
Low rates of aseptic loosening were observed among the studies reporting outcomes by gender, much lower than rates of loosening seen in registry data, which are as high as 33% [2, 4, 5, 14, 27, 31]. Nevertheless, even with the low rates of aseptic loosening in our sample, women appeared to have higher rates of loosening with the data available. At this point, a rationale for the higher rates of aseptic loosening observed in women remains speculative. Implicated factors among the included studies included an increased rate of metal allergy among women, smaller femoral head sizes used in women, and a higher rate of cup malposition (possibly related to higher rates of hip dysplasia) [2, 5]. Current registry data available do not parse out the rates of aseptic loosening by gender; thus, correlations are not possible at this time. However, the Australian registry does appear to show a correlation between smaller femoral head sizes (≤ 50 mm) and higher rates of aseptic loosening [31]. Unfortunately, their analysis did not control for gender. In future iterations of registry data, it would be interesting to see if this relationship remains despite gender or if there is truly a relationship with gender.
Among the included studies, revision was the most commonly reported complication with nearly all of the included studies reporting revision rates by gender. With the included data, women had a higher rate of revision. This finding has been corroborated by the most recent Australian registry data from 2013 that demonstrated a threefold increase in the rate of revision among women at 1-year post-HRA implantation [31]. However, on further analysis of the Australian data, they demonstrate that this relationship appears to be related to femoral component head size with equivalent rates of revision regardless of gender in femoral head sizes greater than or equal to 50 mm [31]. Smaller femoral head size was frequently cited as a likely explanation for the increased rate of failure among the included studies. However, similar to previously discussed complications, femoral as well as acetabular geometry, metal allergy, and component malpositioning were all cited as possible explanations for the increased of revision in women. An additional factor worth investigating in further studies includes the modes of failure stratified by gender, because this was not uniformly reported in the current studies. This would provide insights into possible causes for failure and surgical technique as well as implant improvements for the future.
Although mixed results have been reported with regard to gender differences in complications after MoM HRA, these findings are skewed by the general lack of gender-specific outcome reporting. Our systematic review of levels I through III studies demonstrated increased rates of ALTR, dislocation, aseptic loosening, and revision in women after MoM HRA. Although these findings shed light on the differential complication rate between genders, further study is necessary to elucidate the root causes of these findings. Moving forward, we would encourage researchers to investigate gender as a possible risk factor for complications and furthermore to report demographic data for all patients enrolled in studies (particularly those who experience complications).
References
Alberta Hip Improvement Project, MacKenzie JR, O’Connor GJ, Marshall DA, Faris PD, Dort LC, Khong H, Parker RD, Werle JR, Beaupre LA, Frank CB. Functional outcomes for 2 years comparing hip resurfacing and total hip arthroplasty. J Arthroplasty. 2012;5:750–757.e2.
Amstutz HC, Wisk LE, Le Duff MJ. Sex as a patient selection criterion for metal-on-metal hip resurfacing arthroplasty. J Arthroplasty. 2011;2:198–208.
Bosker BH, Ettema HB, Boomsma MF, Kollen BJ, Maas M, Verheyen CC. High incidence of pseudotumour formation after large-diameter metal-on-metal total hip replacement: a prospective cohort study. J Bone Joint Surg Br. 2012;6:755–761.
Canadian Arthroplasty Society. The Canadian Arthroplasty Society’s experience with hip resurfacing arthroplasty. An analysis of 2773 hips. Bone Joint J. 2013;8:1045–1051.
Carrothers AD, Gilbert RE, Jaiswal A, Richardson JB. Birmingham hip resurfacing: the prevalence of failure. J Bone Joint Surg Br. 2010;10:1344–1350.
Cooper HJ, Deirmengian C, Rodriguez J, Urban RM, Jacobs JJ, Paprosky WG. Taper corrosion presenting as late instability following metal-on-polyethylene total hip arthroplasty. 24th Annual Meeting of the American Association of Hip and Knee Surgeons, Dallas, TX, November 2014.
Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;8:1693–1699.
Cross MB, Nam D, Mayman DJ. Ideal femoral head size in total hip arthroplasty balances stability and volumetric wear. HSS J. 2012;3:270–274.
de Steiger RN, Hang JR, Miller LN, Graves SE, Davidson DC. Five-year results of the ASR XL acetabular system and the ASR hip resurfacing system: An analysis from the Australian Orthopaedic Association National Joint Replacement Registry. J Bone Joint Surg Am. 2011;24:2287–2293.
Fox CM, Bergin KM, Kelly GE, McCoy GF, Ryan AG, Quinlan JF. MRI findings following metal on metal hip arthroplasty and their relationship with metal ion levels and acetabular inclination angles. J Arthroplasty. 2014;8:1647–1652.
Glyn-Jones S, Pandit H, Kwon YM, Doll H, Gill HS, Murray DW. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br. 2009;12:1566–1574.
Grammatopoulos G, Pandit H, Oxford Hip and Knee Group, Murray DW, Gill HS. The relationship between head-neck ratio and pseudotumour formation in metal-on-metal resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2010;11:1527–1534.
Granchi D, Cenni E, Trisolino G, Giunti A, Baldini N. Sensitivity to implant materials in patients undergoing total hip replacement. J Biomed Mater Res B Appl Biomater. 2006;2:257–264.
Gross TP, Liu F. Comparative study between patients with osteonecrosis and osteoarthritis after hip resurfacing arthroplasty. Acta Orthop Belg. 2012;6:735–744.
Gross TP, Liu F. Incidence of adverse wear reactions in hip resurfacing arthroplasty: a single surgeon series of 2,600 cases. Hip Int. 2013;3:250–258.
Hart AJ, Matthies A, Henckel J, Ilo K, Skinner J, Noble PC. Understanding why metal-on-metal hip arthroplasties fail: a comparison between patients with well-functioning and revised Birmingham hip resurfacing arthroplasties. AAOS exhibit selection. J Bone Joint Surg Am. 2012;4:e22.
Hug KT, Watters TS, Vail TP, Bolognesi MP. The withdrawn ASR THA and hip resurfacing systems: how have our patients fared over 1 to 6 years? Clin Orthop Relat Res. 2013;471:2.
Jameson SS, Baker PN, Mason J, Porter ML, Deehan DJ, Reed MR. Independent predictors of revision following metal-on-metal hip resurfacing: a retrospective cohort study using national joint registry data. J Bone Joint Surg Br. 2012;6:746–754.
Jameson SS, Langton DJ, Nargol AV. Articular surface replacement of the hip: a prospective single-surgeon series. J Bone Joint Surg Br. 2010;1:28–37.
Lachiewicz PF, Soileau ES. Dislocation of primary total hip arthroplasty with 36 and 40-mm femoral heads. Clin Orthop Relat Res. 2006;453:153–155.
Lachiewicz PF, Soileau ES. Low early and late dislocation rates with 36- and 40-mm heads in patients at high risk for dislocation. Clin Orthop Relat Res. 2013;471:439–443.
Ladd AL. Let’s talk about sex, baby: gendered innovations in orthopaedic science. Clin Orthop Relat Res. 2014;472:793–795.
Langton DJ, Sidaginamale RP, Joyce TJ, Natu S, Blain P, Jefferson RD, Rushton S, Nargol AV. The clinical implications of elevated blood metal ion concentrations in asymptomatic patients with MoM hip resurfacings: a cohort study. BMJ Open. 2013;3:10.1136/bmjopen-2012-001541.
Leopold SS, Beadling L, Dobbs MB, Gebhardt MC, Lotke PA, Manner PA, Rimnac CM, Wongworawat MD. Fairness to all: gender and sex in scientific reporting. Clin Orthop Relat Res. 2014;472:391–392.
Lubbeke A, Rothman KJ, Garavaglia G, Barea C, Christofilopoulos P, Stern R, Hoffmeyer P. Strong association between smoking and the risk of revision in a cohort study of patients with metal-on-metal total hip arthroplasty. J Orthop Res. 2014;6:762–768.
Marshall DA, Pykerman K, Werle J, Lorenzetti D, Wasylak T, Noseworthy T, Dick DA, O’Connor G, Sundaram A, Heintzbergen S, Frank C. Hip resurfacing versus total hip arthroplasty: a systematic review comparing standardized outcomes. Clin Orthop Relat Res. 2014;472:2217–2230.
McBryde CW, Theivendran K, Thomas AM, Treacy RB, Pynsent PB. The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am. 2010;1:105–112.
Migaud H, Jobin A, Chantelot C, Giraud F, Laffargue P, Duquennoy A. Cementless metal-on-metal hip arthroplasty in patients less than 50 years of age: comparison with a matched control group using ceramic-on-polyethylene after a minimum 5-year follow-up. J Arthroplasty. 2004;8(Suppl 3):23–28.
Milavec-Puretic V, Orlic D, Marusic A. Sensitivity to metals in 40 patients with failed hip endoprosthesis. Arch Orthop Trauma Surg. 1998;6:383–386.
Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:523–528.
National Joint Replacement Registry. Hip and knee arthroplasty annual report. 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/127202/Annual%20Report%202013?version=1.2&t=1385685288617. Accessed February 22, 2015.
National Joint Replacement Registry. Metal on metal total conventional hip arthroplasty supplementary report. 2013. Available at: https://aoanjrr.dmac.adelaide.edu.au/documents/10180/172288/Metal%20on%20Metal%20Total%20Conventional%20Hip%20Arthroplasty. Accessed February 22, 2015.
Pandit H, Glyn-Jones S, McLardy-Smith P, Gundle R, Whitwell D, Gibbons CL, Ostlere S, Athanasou N, Gill HS, Murray DW. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;7:847–851.
Rogers BA, Garbedian S, Kuchinad RA, Backstein D, Safir O, Gross AE. Total hip arthroplasty for adult hip dysplasia. J Bone Joint Surg Am. 2012;19:1809–1821.
Singh G, Meyer H, Ruetschi M, Chamaon K, Feuerstein B, Lohmann CH. Large-diameter metal-on-metal total hip arthroplasties: a page in orthopedic history? J Biomed Mater Res A. 2013;11:3320–3326.
Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW, National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet. 2012;9822:1199–1204.
van der Weegen W, Sijbesma T, Hoekstra HJ, Brakel K, Pilot P, Nelissen RG. Treatment of pseudotumors after metal-on-metal hip resurfacing based on magnetic resonance imaging, metal ion levels and symptoms. J Arthroplasty. 2014;2:416–421.
Win HL, Yang S, Wimalaratne HK, Weihua X, Shunan Y, Ze R. Chinese experience with metal-on-metal hip resurfacing. J Arthroplasty. 2012;6:968–975.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors (JJJ) certifies that he has or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Medtronics Sofamor Danek (Memphis, TN, USA), an amount of USD 10,000 to USD 100,000 from Nuvasive (San Diego, CA, USA), and an amount of USD 10,000 to USD 100,000 from Zimmer (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
About this article
Cite this article
Haughom, B.D., Erickson, B.J., Hellman, M.D. et al. Do Complication Rates Differ by Gender After Metal-on-metal Hip Resurfacing Arthroplasty? A Systematic Review. Clin Orthop Relat Res 473, 2521–2529 (2015). https://doi.org/10.1007/s11999-015-4227-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-015-4227-8