Abstract
Background
Ankle fractures are common and can be associated with severe morbidity. Risk factors for short-term adverse events and readmission after open reduction and internal fixation (ORIF) of ankle fractures have not been fully characterized.
Questions/purposes
The purpose of our study was to determine patient rates and risk factors for (1) any adverse event; (2) severe adverse events; (3) infectious complications; and (4) readmission after ORIF of ankle fractures.
Methods
Patients who underwent ORIF for ankle fracture from 2005 to 2012 were identified in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP®) database using International Classification of Diseases, 9th Revision and Current Procedural Terminology codes. Patients with missing perioperative data were excluded from this study. Patient characteristics were tested for association with any adverse event, severe adverse events, infectious complications, and readmission using bivariate and multivariate logistic regression analyses.
Results
Of the 4412 patients identified, 5% had an adverse event. Any adverse event was associated with insulin-dependent diabetes mellitus (IDDM; odds ratio [OR], 2.05; 95% confidence interval [CI], 1.35–3.1; p = 0.001), age ≥ 60 years (OR, 1.97; 95% CI, 1.22–3.2; p = 0.006), American Society of Anesthesiologists classification ≥ 3 (OR, 1.69; 95% CI, 1.2–2.37; p = 0.002), bimalleolar fracture (OR, 1.6; 95% CI, 1.08–2.37; p = 0.020), hypertension (OR, 1.47; 95% CI, 1.04–2.09; p = 0.031), and dependent functional status (OR, 1.47; 95% CI, 1.02–2.14; p = 0.040) on multivariate analysis. Severe adverse events occurred in 3.56% and were associated with ASA classification ≥ 3 (OR, 2.01; p = 0.001), pulmonary disease (OR, 1.9; p = 0.004), dependent functional status (OR, 1.8; p = 0.005), and hypertension (OR, 1.65; p = 0.021). Infectious complications occurred in 1.75% and were associated with IDDM (OR, 3.51; p < 0.001), dependent functional status (OR, 2.4; p = 0.002), age ≥ 60 years (OR, 2.28; p = 0.028), and bimalleolar fracture (OR, 2.19; p = 0.030). Readmission occurred in 3.17% and was associated with ASA classification ≥ 3 (OR, 2.01; p = 0.017).
Conclusions
IDDM was associated with an increased rate of adverse events after ankle fracture ORIF, whereas noninsulin-dependent diabetes mellitus was not. IDDM management deserves future study, particularly with respect to glycemic control, a potential confounder that could not be assessed with the ACS-NSQIP registry. Increased ASA class was associated with readmission, and future prospective investigations should evaluate the effectiveness of increasing the discharge threshold, discharging to extended-care facilities, and/or home nursing evaluations in this at-risk population.
Level of Evidence
Level III, prognostic study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle fracture is the most common intraarticular fracture of a weightbearing joint, accounting for 9% of all fractures [16, 17, 27, 28]. Ankle fractures often are treated with open reduction and internal fixation (ORIF), and these procedures may be associated with risks, including infection, thromboembolic events, and poor wound healing [4, 5, 20, 24, 26, 27]. Recognition of potential risk factors for adverse outcomes after open reduction and internal fixation (ORIF) is essential for improving treatments and counseling patients.
Previous studies that have assessed risk factors for complications after ankle fracture ORIF have been limited by size, have only studied single risk factors, or have used potentially flawed, administratively coded data to capture adverse events [6, 15, 19, 20, 23, 24, 27, 30]. To further characterize these risks, further study of high-quality data collected from a large, nationwide sample was needed.
The American College of Surgeons National Quality Improvement Program (ACS-NSQIP®) database is a high-quality, prospectively collected database that captures surgical procedures from a national sample of hospitals [1]. The ACS-NSQIP has become widely used in the orthopaedic literature to analyze outcomes for many orthopaedic procedures, because the number of patients in the database confers greater power for analysis than single-surgeon or single-institution cohorts. By using a large, national patient sample for our study, generalizable conclusions could be drawn to better define postoperative expectations for surgeons and patients with operative ankle fracture.
The purpose of our study was to determine patient rates of and risk factors for (1) any adverse event; (2) severe adverse events; (3) infectious complications; and (4) readmission after ORIF of ankle fractures using the ACS-NSQIP database.
Patients and Methods
The ACS-NSQIP database was used to conduct a retrospective cohort study of patients who underwent ORIF of ankle fracture from 2005 to 2012. In the ACS-NSQIP, 150 patient variables are collected from more than 370 participating US hospitals [1]. Patients are prospectively identified, and information is obtained from operative reports, medical records, and patient interviews by trained clinical reviewers [1, 12]. Data are collected up to 30 days after surgery, including after discharge. Routine auditing of the database ensures high-quality data with interrater disagreement of approximately 2% for all assessed variables [1]. In addition, to participate in the ACS-NSQIP, institutions must maintain a 30-day followup rate (with no missing or incomplete data) of 80% or greater [1]. Furthermore, only patients with full 30-day followup are included in the final data set that was used for this study.
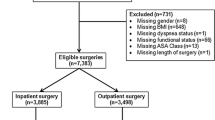
Initially, we selected patients by a postoperative diagnosis of ankle fracture (International Classification of Diseases, 9th Revision [ICD-9] codes 824.0–824.9). From the identified group, only patients with primary Current Procedural Terminology (CPT) codes 27766 (ORIF of medial malleolus fracture), 27769 (ORIF of posterior malleolus fracture), 27792 (ORIF of lateral malleolus fracture), 27814 (ORIF of bimalleollar fracture), and 27822/27823 (ORIF of trimalleollar fracture) were included in our analysis. Patients with incomplete perioperative data were excluded from the study. Our inclusion/exclusion criteria left 4412 patients remaining (of an initial 4785 identified by ICD-9 and CPT codes) for our analysis.
Patient demographics and comorbidities were collected from the ACS-NSQIP database (Appendix 1 [Supplemental materials are available with the online version of CORR®.]). History of diabetes is recorded as one of three groups in the database: insulin-dependent diabetes mellitus (IDDM), noninsulin-dependent diabetes mellitus (NIDDM), or no diabetes.
Adverse Events
The ACS-NSQIP tracks patients for individual adverse events that occur within the first 30 postoperative days (including while in the hospital and after discharge). All patients included in this study had full 30-day followup with no missing or incomplete data for each outcome studied. The occurrence of a serious adverse event was defined as the occurrence of any of the following: death, coma lasting more than 24 hours, on ventilator more than 48 hours, unplanned intubation, stroke/cerebrovascular accident, thromboembolic event (deep venous thrombosis or pulmonary embolism), cardiac arrest, myocardial infarction, acute renal failure, sepsis, septic shock, return to the operating room, wound dehiscence, deep surgical site infection (SSI), organ/space infection, graft/prosthesis/flap failure, or peripheral nerve injury.
A minor adverse event was defined as superficial SSI, urinary tract infection, pneumonia, or progressive renal insufficiency. Any adverse event was defined as the occurrence of any serious or minor adverse event.
Infectious complication was defined as an occurrence of any of the following: superficial SSI, deep SSI, organ/space infection, sepsis, or septic shock. Although included in the serious adverse event and minor adverse event categories, infectious complications were also grouped together for separate analyses, because this was thought to be of specific clinical interest.
Readmission
Beginning in 2011, the ACS-NSQIP began tracking readmissions after discharge for the first 30 postoperative days. Readmission was defined as a binary variable that was positive when a patient had an unplanned readmission one or more times after the initial postoperative discharge. Only patients who underwent ORIF for an ankle fracture in 2011 or 2012 were included in the readmission analysis (2521 patients, or 57% of the patient population).
Statistical Analysis
Patient and operative characteristics were tested for association with the occurrence of any adverse event, severe adverse event, infectious complication, and readmission using bivariate and multivariate logistic regression. Discharge destination and extended length of stay were included in the readmission analysis because this information was available at the time of initial discharge and would be useful to include in a model that predicts odds of readmission. Differences between study years were also assessed (Appendix 2 [Supplemental materials are available with the online version of CORR®.]).
Final multivariate models were constructed using a backward stepwise process that initially included all potential variables and sequentially excluded variables with the highest p values until only those with a p value < 0.20 remained. Variables with a p value > 0.05 but < 0.20 were left in the model to control for potential confounding but were not considered to be significantly associated with the outcome. Statistical significance was set at p < 0.05. Only factors that were significant in multivariate analyses are reported, and findings from exploratory bivariate analyses are not presented in the Results.
Study Population
A summary of patient characteristics is shown (Table 1). For the 4412 patients with ankle fractures who met study inclusion criteria, average patient age was 51 ± 18 years (mean ± SD) and average body mass index was 30 ± 8 kg/m2. Men comprised 40% of the cohort. A total of 235 patients (5%) had medial malleolus fracture; 1143 patients (26%) had lateral malleolus fracture; 1705 patients (39%) had bimalleollar fracture; and 1329 (30%) had trimalleollar fracture.
Results
Events meeting the definition of any adverse event were identified in 225 patients (5%; Table 2). After controlling for likely confounders, IDDM (odds ratio [OR], 2.05; 95% confidence interval [CI], 1.35–3.1; p = 0.001); age ≥ 60 years (OR, 1.97; 95% CI, 1.22–3.2; p = 0.006); American Society of Anesthesiologists (ASA) classification ≥ 3 (OR, 1.69; 95% CI, 1.2–2.37; p = 0.002); bimalleolar fracture (OR, 1.6; 95% CI, 1.08–2.37; p = 0.020); hypertension (OR, 1.47; 95% CI, 1.04–2.09; p = 0.031); and dependent functional status (OR, 1.47; 95% CI, 1.02–2.14; p = 0.040) were associated with the occurrence of any adverse event (Table 3).
Severe adverse events were noted for 157 patients (3.56%). After controlling for likely confounders (Table 3), ASA classification ≥ 3 (OR, 2.01; 95% CI, 1.34–3.03; p = 0.001); pulmonary disease (OR, 1.9; 95% CI, 1.23–2.94; p = 0.004); dependent functional status (OR, 1.8; 95% CI, 1.19–2.72; p = 0.005), and hypertension (OR, 1.65; 95% CI, 1.08–2.51; p = 0.021) were significantly associated with severe adverse events. Because IDDM and other factors were associated with any adverse event, but not severe adverse events, a post hoc secondary analysis was conducted to identify associations between patient factors and minor adverse events. After controlling for potential confounders, IDDM (OR, 3.96; p < 0.001), age ≥ 60 years (OR, 3.09; p = 0.001), and bimalleolar fracture (OR, 2.13; p = 0.021) were found to be associated with minor adverse events.
Infectious complications were noted for 77 patients (1.75%). Infectious complications occurred, on average, 18 ± 8 days after ORIF of an ankle fracture. After controlling for likely confounders (Table 3), IDDM (OR, 3.51; 95% CI, 1.85–6.64; p < 0.001); dependent functional status (OR, 2.4; 95% CI, 1.38–4.19; p = 0.002); age ≥ 60 years (OR, 2.28; 95% CI, 1.1–4.76; p = 0.028); and bimalleolar fracture (OR, 2.19; 95% CI, 1.08–4.44; p = 0.030) were independently associated with the occurrence of an infectious complication.
A total of 80 patients (3.17%) were readmitted within the first 30 postoperative days. Readmission occurred, on average, 12 ± 8 days after ORIF of an ankle fracture. After controlling for likely confounders (Table 3), only ASA classification ≥ 3 (OR, 2.01; 95% CI, 1.13–3.57; p = 0.017) was independently associated with readmission.
Discussion
ORIF of an ankle fracture is a common procedure that can be associated with significant postoperative complications [4, 5, 20, 24, 26, 27]. Characterizing risk factors for preoperative patient counseling and perioperative medical care is important for improving treatment outcomes for these patients. Using the ACS-NSQIP database, information from 4412 patients who had undergone ORIF was evaluated to identify preoperative risk factors for any adverse event, severe adverse events, infectious complication, and readmission in the 30 days after ankle fracture ORIF. Any adverse event was associated with IDDM, increased age, increased ASA classification, bimalleolar fracture, hypertension, and dependent functional status, whereas severe adverse events were associated with increased ASA classification, pulmonary disease, dependent functional status, and hypertension. Infectious complications were associated with IDDM, dependent functional status, increased age, and bimalleolar fracture. Readmission was associated with increased ASA classification.
Our study has several limitations as a result of the nature of the data source. First, the ACS-NSQIP only records the occurrence of adverse events and readmissions up to 30 days postoperatively, including after discharge. Although the occurrence of adverse events after the 30-day window may be missed, the database provides large improvement over much of the existing information in the literature, which has relied on administratively coded databases that only capture adverse events that occurred while an inpatient or were associated with a readmission. Second, fracture classification beyond medial malleolar, lateral malleolar, bimalleolar, and trimalleolar was unavailable, which prevented further subgroup analyses. Third, although many ankle fractures are treated with casting and closed methods, our study captured patients only treated operatively. The results of our study thus may only apply to ankle fractures treated with ORIF. Fourth, information beyond IDDM or NIDDM status was not available for the diabetic patients in this study such as glycemic control and/or the presence of end-organ damage. Because glycemic control may vary between patients with IDDM or NIDDM [13, 31], this represents a potential confounder that could not be controlled for in the present study. Fifth, for this study, adverse events were grouped into the aggregate outcomes “any adverse event,” “severe adverse events,” and “infectious complications.” Although these groupings were based on previous literature using the ACS-NSQIP [2], it is nonetheless difficult to combine adverse events so that study outcomes are clinically meaningful. Although imperfect, these groupings are our best attempt at stratifying the short-term outcomes after ankle fracture ORIF to differentiate between severe complications with likely long-term sequelae and minor complications. For infectious complications, we believed that host factors would leave a patient susceptible to SSIs as well as systemic infections.
For the occurrence of any adverse event, the strongest and most clinically important risk factor was IDDM, which doubled the risk of such an event. Diabetes has been associated with complications after ankle fractures previously [6, 7, 10, 20, 27]. Although these studies have described increased rates of complications with diabetes, no large study has differentiated IDDM and NIDDM. Results from our study indicate that the risks for adverse events in patients with ankle fracture who have IDDM are distinct from those with NIDDM. Furthermore, our results highlight that using binary definitions of “diabetes” or “nondiabetes” may be less specific than necessary for analyzing outcomes. Despite the present study differentiating between IDDM and NIDDM, additional information such as glycemic control and end-organ damage was not available in the database to be studied. Future investigations on the outcomes of ankle fracture surgery would benefit from controlling for these variables in their analyses. Moreover, clinical databases such as the ACS-NSQIP would benefit from collecting such information to enable these future studies. In addition to patients with IDDM, elderly patients, those with increased overall comorbidities, hypertension, or dependent functional status also had increased risk of any adverse event in our study. Increased age and medical comorbidity have also been previously linked to complications after ankle fracture in the literature [27].
Serious adverse events were most strongly associated with ASA classifications ≥ 3. Increased ASA classification has been previously described as a risk factor for postoperative complications after other orthopaedic procedures [3] and is likely not specific to ankle fractures. However, beyond this general risk factor, we also identified risk factors that are likely more specific to the ankle fracture population such as IDDM that have not been identified for other orthopaedic procedures [8]. Dependent functional status also contributed to the risk of severe adverse events in patients with ankle fracture, which we speculate may be related to difficulty with postoperative mobilization, a previously identified risk factor for thromboembolic events after ankle fracture [9, 11, 18, 21]. The risks associated with each of these patient and operative factors now can be more specifically discussed with patients preoperatively. Interestingly, a secondary analysis found that IDDM, age ≥ 60 years, and bimalleolar fracture were associated with minor adverse events, but not severe complications. These results suggest that ORIF of ankle fracture in these patients is not particularly risky; however, they may require increased healthcare use postoperatively as a result of their increased risk of minor complications.
Postoperative infections were most associated with IDDM. Diabetes has been previously linked to infection after operative fixation of ankle fractures [14]; however, results of our study indicate that patients treated with oral antiglycemic regimens may not be at much greater risk compared with patients without diabetes. This is an important distinction that to our knowledge has not been described before. Noninsulin-dependent diabetics can be advised that they are at no increased risk of complications after ankle fracture ORIF, and they should not require additional preoperative workup or postoperative care. These results support future research into the perioperative management of diabetic patients. Future studies would benefit from differentiating insulin-dependent patients from noninsulin-dependent diabetic patients as well as capturing further diabetes-specific information such as Type 1 versus Type 2, glycemic control, insulin regimen, and the presence of end-organ damage. As suggested, it would be beneficial for databases such as the ACS-NSQIP to begin recording these additional disease-specific variables to enable more detailed investigations in the future.
The only factor independently associated with readmission in the 30 days after ankle fracture ORIF was ASA classification ≥ 3. With increased attention being paid to 30-day readmission after orthopaedic surgery [29], it is now especially important to identify which patients are most likely to be readmitted. Readmission has not previously been assessed as an isolated outcome after ankle fracture, so there is little basis for comparison of our result; however, because increased comorbidity has been associated with complications after ankle fracture, both in our study and another [27], the relationship likely holds true for both pre- and posthospital discharge and may help explain the association of higher ASA classification and readmission. Increased ASA classification has also been associated with readmission after general orthopaedic trauma [25]. Patients with increased ASA class are therefore important targets for reducing readmission rates, and future study is needed to determine how to best accommodate this at-risk population. The threshold for discharge may need to be increased or perhaps discharge to extended-care facilities or home nursing evaluations may be necessary. The next step for evaluating the effectiveness of each of these options is to conduct prospective cohort studies in patients with ASA classification 3 or greater. These studies would be able to directly compare the relative risks of readmission for each of these potentially modifiable factors in patients with significant comorbidity.
Although multiple factors were found to be associated with short-term adverse events and readmission, several factors such as smoking and obesity were not associated with increased postoperative risks. This is notable, because smoking and obesity have been previously found to be associated with adverse events after other types of orthopaedic surgery [2, 3]. We speculate that these factors may lead to poorer long-term outcomes after ankle fracture ORIF but may not necessarily lead to complications in the immediate postoperative period. For example, one of the main concerns with smoking is the decreased rate of bone healing; however, this would not be fully evident within the first 30 postoperative days and is not captured by the ACS-NSQIP [23]. Similarly, although obesity may not increase immediate postoperative risk, obesity may complicate long-term rehabilitation after the procedure.
In summary, our study characterized the incidence of, and risk factors for, the occurrence of any adverse event, severe adverse events, infectious complications, and readmission after ankle fracture ORIF. Among the factors identified, IDDM was associated with both adverse events and infectious complications. Optimizing the perioperative care of diabetic patients is an important avenue for further research, and future studies should attempt to control for additional diabetic-specific parameters such as glycemic control and/or end-organ damage. Furthermore, it would be beneficial for large clinical databases such as the ACS-NSQIP to collect such information on diabetic patients to facilitate these further studies. We additionally identified other patient comorbidities associated with complications and readmissions, which are useful for defining the specific risks associated with surgical treatment of ankle fractures. Furthermore, because 30-day readmission is now being specifically targeted by healthcare administrators and policymakers as a quality measure, the association of readmission with ASA class suggests that these patients deserve particular attention. Future study is warranted to determine the most effective methods of managing these patients in the postoperative period to reduce the burden of readmission on the patient and healthcare system.
References
American College of Surgeons. User Guide for the 2012 Participant Use Data File. American College of Surgeons National Surgical Quality Improvement Program. Available at: http://site.acsnsqip.org/wp-content/uploads/2013/10/ACSNSQIP.PUF_.UserGuide.2012.pdf. Accessed September 10, 2014.
Basques BA, Webb ML, Bohl DD, Golinvaux NS, Grauer JN. Adverse events, length of stay, and readmission following surgery for tibial plateau fractures. J Orthop Trauma. 2014 Aug 26 [Epub ahead of print].
Belmont PJ Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am. 2014;96:20–26.
Brem H, Tomic-Canic M. Cellular and molecular basis of wound healing in diabetes. J Clin Invest. 2007;117:1219–1222.
Chaudhary SB, Liporace FA, Gandhi A, Donley BG, Pinzur MS, Lin SS. Complications of ankle fracture in patients with diabetes. J Am Acad Orthop Surg. 2008;16:159–170.
Costigan W, Thordarson DB, Debnath UK. Operative management of ankle fractures in patients with diabetes mellitus. Foot Ankle Int. 2007;28:32–37.
Dellenbaugh SG, Dipreta JA, Uhl RL. Treatment of ankle fractures in patients with diabetes. Orthopedics. 2011;34:385.
Golinvaux NS, Bohl DD, Basques BA, Baumgaertner MR, Grauer JN. Diabetes confers little to no increased risk of postoperative complications after hip fracture surgery in geriatric patients. Clin Orthop Relat Res. 2014 Sep 20 [Epub ahead of print].
Hanslow SS, Grujic L, Slater HK, Chen D. Thromboembolic disease after foot and ankle surgery. Foot Ankle Int. 2006;27:693–695.
Jones KB, Maiers-Yelden KA, Marsh JL, Zimmerman MB, Estin M, Saltzman CL. Ankle fractures in patients with diabetes mellitus. J Bone Joint Surg Br. 2005;87:489–495.
Kadous A, Abdelgawad AA, Kanlic E. Deep venous thrombosis and pulmonary embolism after surgical treatment of ankle fractures: a case report and review of literature. J Foot Ankle Surg. 2012;51:457–463.
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA Jr, Fink AS, Mentzer RM Jr, Neumayer L, Hammermeister K, Mosca C, Healey N. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008;248:329–336.
Koga M, Murai J, Morita S, Saito H, Kasayama S. Comparison of annual variability in HbA1c and glycated albumin in patients with type 1 vs type 2 diabetes mellitus. J Diabetes Complications. 2013;27:211–213.
Korim MT, Payne R, Bhatia M. A case-control study of surgical site infection following operative fixation of fractures of the ankle in a large UK trauma unit. Bone Joint J. 2014;96:636–640.
Koval KJ, Zhou W, Sparks MJ, Cantu RV, Hecht P, Lurie J. Complications after ankle fracture in elderly patients. Foot Ankle Int. 2007;28:1249–1255.
Leininger RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35:288–293.
Mandi DM. Ankle fractures. Clin Podiatr Med Surg. 2012;29:155–186, vii.
Mayle RE Jr, DiGiovanni CW, Lin SS, Tabrizi P, Chou LB. Current concepts review: venous thromboembolic disease in foot and ankle surgery. Foot Ankle Int. 2007;28:1207–1216.
Menendez ME, Neuhaus V, Bot AGJ, Ring D, Johnson AH. The impact of metabolic syndrome on inpatient outcomes after isolated ankle fractures. Foot Ankle Int. 2014;35:463–470.
Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J Bone Joint Surg Am. 2012;94:2047–2052.
Mizel MS, Temple HT, Michelson JD, Alvarez RG, Clanton TO, Frey CC, Gegenheimer AP, Hurwitz SR, Lutter LD, Mankey MG, Mann RA, Miller RA, Richardson EG, Schon LC, Thompson FM, Yodlowski ML. Thromboembolism after foot and ankle surgery. A multicenter study. Clin Orthop Relat Res. 1998;348:180–185.
Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–1529.
Nåsell H, Ottosson C, Törnqvist H, Lindé J, Ponzer S. The impact of smoking on complications after operatively treated ankle fractures—a follow-up study of 906 patients. J Orthop Trauma. 2011;25:748–755.
Ovaska MT, Makinen TJ, Madanat R, Huotari K, Vahlberg T, Hirvensalo E, Lindahl J. Risk factors for deep surgical site infection following operative treatment of ankle fractures. J Bone Joint Surg Am. 2013;95:348–353.
Sathiyakumar V, Molina CS, Thakore RV, Obremskey WT, Sethi MK. ASA score as a predictor of 30-day perioperative readmission in patients with orthopaedic trauma injuries: a NSQIP analysis. J Orthop Trauma. 2014 Jul 25 [Epub ahead of print].
SooHoo NF, Eagan M, Krenek L, Zingmond DS. Incidence and factors predicting pulmonary embolism and deep venous thrombosis following surgical treatment of ankle fractures. Foot Ankle Surg. 2011;17:259–262.
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Joint Surg Am. 2009;91:1042–1049.
Sporer SM, Weinstein JN, Koval KJ. The geographic incidence and treatment variation of common fractures of elderly patients. J Am Acad Orthop Surg. 2006;14:246–255.
US Department of Health and Human Services, Centers for Medicare & Medicaid Services (CMS). Hospital-level 30-day, all-cause risk-standardized readmission rate (RSRR) following elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA) (NQF #1551). Available at: www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=72187. Accessed September 10, 2014.
Wukich DK, McMillen RL, Lowery NJ, Frykberg RG. Surgical site infections after foot and ankle surgery: a comparison of patients with and without diabetes. Diabetes Care. 2011;34:2211–2213.
Yoshiuchi K, Matsuhisa M, Katakami N, Nakatani Y, Sakamoto K, Matsuoka T, Umayahara Y, Kosugi K, Kaneto H, Yamasaki Y, Hori M. Glycated albumin is a better indicator for glucose excursion than glycated hemoglobin in type 1 and type 2 diabetes. Endocr J. 2008;55:503–507.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (BAB) has received funding from the National Institutes of Health.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Basques, B.A., Miller, C.P., Golinvaux, N.S. et al. Morbidity and Readmission After Open Reduction and Internal Fixation of Ankle Fractures Are Associated With Preoperative Patient Characteristics. Clin Orthop Relat Res 473, 1133–1139 (2015). https://doi.org/10.1007/s11999-014-4005-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-4005-z