Abstract
Background
Several construct options exist for transverse acetabular fracture fixation. Accepted techniques use a combination of column plates and lag screws. Quadrilateral surface buttress plates have been introduced as potential fixation options, but as a result of their novelty, biomechanical data regarding their stabilizing effects are nonexistent. Therefore, we aimed to determine if this fixation method confers similar stability to traditional forms of fixation.
Questions/purposes
We biomechanically compared two acetabular fixation plates with quadrilateral surface buttressing with traditional forms of fixation using lag screws and column plates.
Methods
Thirty-five synthetic hemipelves with a transverse transtectal acetabular fracture were allocated to one of five groups: anterior column plate + posterior column lag screw, posterior column plate + anterior column lag screw, anterior and posterior column lag screws only, infrapectineal plate + anterior column plate, and suprapectineal plate alone. Specimens were loaded for 1500 cycles up to 2.5x body weight and stiffness was calculated. Thereafter, constructs were destructively loaded and failure loads were recorded.
Results
After 1500 cycles, final stiffness was not different with the numbers available between the infrapectineal (568 ± 43 N/mm) and suprapectineal groups (602 ± 87 N/mm, p = 0.988). Both quadrilateral plates were significantly stiffer than the posterior column buttress plate with supplemental lag screw fixation group (311 ± 99 N/mm, p < 0.006). No difference in stiffness was identified with the numbers available between the quadrilateral surface plating groups and the lag screw group (423 ± 219 N/mm, p > 0.223). The infrapectineal group failed at the highest loads (5.4 ± 0.6 kN) and this was significant relative to the suprapectineal (4.4 ± 0.3 kN; p = 0.023), lag screw (2.9 ± 0.8 kN; p < 0.001), and anterior buttress plate with posterior column lag screw (4.0 ± 0.6 kN; p = 0.001) groups.
Conclusions
Quadrilateral surface buttress plates spanning the posterior and anterior columns are biomechanically comparable and, in some cases, superior to traditional forms of fixation in this synthetic hemipelvis model.
Clinical Relevance
Quadrilateral surface buttress plates may present a viable alternative for the treatment of transtectal transverse acetabular fractures. Clinical studies are required to fully define the use of this new form of fixation for such fractures when accessed through the anterior intrapelvic approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Operative reduction and stabilization of displaced acetabular fractures are now considered the accepted treatment for these injuries to decrease the risk of posttraumatic arthritis and allow early mobilization and improved functional outcome. Reduction of acetabular fractures can be performed through posterior (Kocher-Langenbeck or Gibson) or anterior (ilioinguinal or anterior intrapelvic) approaches. Some fractures such as the transtectal transverse fracture pattern can be addressed through either approach depending on the surgeon’s individual preference [10]. The anterior intrapelvic approach offers the benefit of less surgical exposure than both the ilioinguinal and the posterior approaches because fracture fixation through this approach can often be done without the need to open the lateral or middle windows.
Standard methods of fixation include various combinations of pelvic reconstruction plates and lag screws applied to the anterior and posterior columns from either an anterior or posterior approach [1]. When fixing these fractures through a posterior or an ilioinguinal approach, the surgeon has direct access to only one column, allowing buttress plate fixation of the accessed column and indirect lag screw fixation of the other column. The advantage of the anterior intrapelvic approach is that the surgeon has direct access to both the anterior column and medial surface of the posterior column allowing for buttress plate fixation of both columns. Newer buttress plate constructs that span the posterior and anterior columns through the quadrilateral surface have been developed to take advantage of the exposure of both columns provided with this surgical approach. To date, there have been no studies comparing the biomechanical stability of these newly developed quadrilateral surface buttress plates with traditional constructs that consist of standard pelvic reconstruction plates and lag screws for the fixation of transverse acetabular fractures.
Therefore, in this biomechanical study, we evaluated the construct stability provided by the newer forms of fixation using column-spanning plates with quadrilateral surface buttressing and compared them with the traditional forms of fixation that use single-column buttress plates and lag screws or lag screws only.
Materials and Methods
Specimens
Thirty-five fourth-generation composite hemipelves (Sawbones®; Pacific Research Laboratories, Vashon, WA, USA) were used in this investigation. A synthetic tissue surrogate was chosen because of standardized geometry, homogeneous material properties, and prior laboratory work that has validated the surrogates against cadaveric human bone with comparative results for axial, torsional, and four-point bending stiffness as well as failure mechanism and failure load under different loading conditions [3, 4, 6, 7, 16, 17]. Additionally, the use of a tissue surrogate eliminates potentially confounding variables associated with fresh-frozen cadaveric tissue, including bone quality and anatomic heterogeneity, which may affect biomechanical results and their interpretation.
Fracture Creation
Using a custom-designed stabilizing fixture, a thin oscillating saw was used to create an identical transtectal osteotomy that began at the midportion of the greater sciatic notch and traveled across the posterior column, through the roof of the acetabulum, exiting through the anterior column at the level of the iliopectineal eminence. The same author (IRS) performed all osteotomies. After fracture creation, fine-grained sandpaper was used to smooth the fracture surfaces before hardware application.
Instrumentation
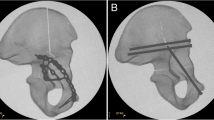
All instrumentations were performed in accordance with manufacturer recommendations and instrumentation sets. Fluoroscopy (GE FlexiView 8800; GE Healthcare, Waukesha, WI, USA) was used to confirm appropriate hardware application and fracture fixation. The osteotomy was reduced anatomically and fixed in one of five ways (Fig. 1): (1) one 10-hole anterior column 3.5-mm pelvic reconstruction buttress plate supplemented with one 8.0-mm cannulated posterior column lag screw; (2) one eight-hole posterior column 3.5-mm pelvic reconstruction buttress plate supplemented with one 8.0-mm anterior column lag screw; (3) one 8.0-mm cannulated anterior column lag screw plus one 8.0-mm cannulated posterior column lag screw; (4) one 10-hole anterior column 3.5-mm pelvic reconstruction buttress plate supplemented with an infrapectineal quadrilateral surface buttress plate; and (5) one suprapectineal posterior column/quadrilateral surface buttress plate . Nonlocking 3.5-mm cortical screws were used (length range: 26–145 mm) and all fixation was provided by Stryker Trauma (Kiel, Germany). Fixation torque for the cortex and lag screws was standardized at 3 Nm (DigiTorque screwdriver [1.0–5.0 Nm]; PB Swiss Tools, Gainesville, GA, USA).
The various fixation methods are shown: (A) a 10-hole anterior column pelvic reconstruction buttress plate with a posterior column lag screw; (B) an eight-hole posterior column pelvic reconstruction buttress plate with a posterior column lag screw; (C) a 10-hole anterior column pelvic reconstruction buttress plate supplemented with an infrapectineal quadrilateral surface buttress plate; and (D) a suprapectineal posterior column/quadrilateral surface buttress plate.
A sample size of seven specimens per fixation group was based on an a priori power analysis using the biomechanical data published by Khajavi et al. [9]. Using their stiffness mean and variance estimates from Sawbones constructs with simulated acetabular fractures instrumented with similar forms of fixation to those used here, a minimum of sample size of six was required for each experimental group assuming a significance level of α = 0.05, a desired power of β = 0.80, and an anticipated large effect size between groups. A sample size of seven per group afforded us an experimental design powered at the 0.875 level.
Biomechanical Testing
We adopted a testing methodology similar to those previously published by Olson et al. [11] and Khajavi et al. [9], in which the acetabulum was compressively loaded in a mediosuperior direction (Fig. 2). Compressive load was applied to the reconstructed pelvis with the femoral head of a fourth-generation composite tissue surrogate (Model 3404, Sawbones®; Pacific Research Laboratories) that was coupled to the actuator of a servohydraulic test frame (MTS Bionix®; MTS, Inc, Eden Prairie, MN, USA). As part of the test setup, the ilium was potted in high-strength resin (Bondo body filler; 3 M Collision Repair Solutions, St Paul, MN, USA) and coupled to a passive, lockable x-y table to facilitate proper specimen orientation before load application. To approximate boundary conditions similar to those experienced in vivo, the pubic symphysis was placed on a ball joint to freely allow for rotation. This ball joint rested on a separate nonlocked, passive x-y linear slide allowing the inferior fragment to translate with any concomitant rotation. The test fixture was rigidly coupled to a 10-kN load cell (MTS, Inc).
Photographs demonstrate the biomechanical test model. (A) Anterior and (B) lateral views of the anatomic hip orientation are shown. (C) The force vector acts in a mediosuperior direction to load the acetabulum. (D) For testing, each hemipelvis was mounted horizontally while maintaining the correct joint and applied force orientation. (E) The synthetic tissue surrogate is shown in the test frame.
Specimen loading consisted of 10 cycles of preconditioning to 0.25 × body weight (BW) (assuming 70-kg BW) at 1 Hz under load control (17.5–175 N). Force and displacement data from the 10th cycle were used to determine the repaired construct’s baseline stiffness. Constructs were then cyclically loaded using an incrementally increasing stair step protocol (Table 1) at 1 Hz. The dynamic portion of testing was intended to determine whether any progressive femoral head subluxation occurred as a function of fixation treatment, as quantified through permanent displacement across the fracture surfaces. After each cyclic loading interval, the specimen was loaded to 0.25 × BW (175 N) and stiffness and displacement across the fracture surface were quantified. All 35 constructs survived the incrementally increasing cyclic loading protocol with no evidence of permanent deformation or failure. Thereafter, they were loaded to catastrophic failure at 1 mm/second. Force and displacement data (derived from the test frame’s linear variable differential transducer output) were collected at 50 Hz.
Preliminary Validation Study
In an effort to validate the synthetic hemipelvis model, a preliminary study was undertaken comparing the progressive failure mechanism in two synthetic specimens and two fresh-frozen human cadaveric hemipelves with dual lag screw fixation. The donor pelvis tested as part of the validation study was retrieved from a 63-year-old man (weight: 130 pounds [59 kg]). Bone mineral density was quantified in the femoral head using dual x-ray absorptiometry (GE Lunar® Prodigy®; GE Healthcare) on receipt of the specimen and before dissection. The femoral neck bone mineral density was 0.577 g/cm2 and the associated T-score was −3.7, indicative of osteoporosis. The validation specimen was sectioned into right and left hemipelves and the specimens were exposed to the same biomechanical sequence as just described. The validity of the synthetic model was determined based on failure mechanism documented in the cadaveric specimens.
Validation Study Results
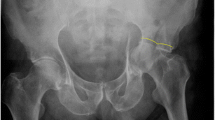
The baseline stiffness values for the synthetic tissue surrogates (n = 2) and cadaveric specimens (n = 2) were 927 and 894 N/mm and 541 and 535 N/mm, respectively. Both cadaver specimens failed during cyclic testing at 1.5 × BW (1050 N). Failure of the specimens was manifested as progressive medial subluxation of the femoral head associated with displacement of the distal fracture fragment medially and rotation of the distal fracture fragment posteriorly about the osteotomy line. Failure occurred progressively as the head of the posterior column lag screw plowed through the osteoporotic trabecular bone and cortex beneath the quadrilateral surface (Fig. 3A–B). The failure mechanisms were identical for the two cadaveric specimens. The synthetic specimens both survived the incrementally increasing load protocol. When loaded to failure, these specimens failed in a manner identical to that of the cadaveric specimens. Fracture was evident on the quadrilateral surface for both specimens and initiated on the ilium side of the osteotomy at the posterior column lag screw/cortical bone interface (Fig. 3B–C).
Statistical Analysis
Biomechanical parameters included baseline stiffness (in Newtons per millimeter) before cyclic loading and when loaded to 0.25 × BW after the last loading level (2.5 × BW). Stiffness was defined as the slope of the force versus displacement curve. Additionally, progressive deformation under nondestructive cyclic loading was quantified and was determined from the test frame’s linear variable differential transducer output (in millimeters). This parameter was defined as the maximum measured displacement when the specimens were loaded to 0.25 × BW (175 N) after each progressively increasing load interval. Finally, failure load (in Newtons) was quantified for each specimen and compared between fixation groups. We defined final stiffness and failure load as the primary biomechanical parameters of interest. Baseline stiffness, final stiffness, progressive construct deformation, and failure loads were compared between groups with a one-way analysis of variance (ANOVA) and Bonferroni post hoc multiple comparison procedure. All analyses were conducted with SPSS® Version 20 (IBM Corp, Armonk, NY, USA) at a significance level of 0.05. ANOVA tests of between-subjects effects for final stiffness and failure load indicated the following: final stiffness: F = 6.5, p = 0.001; η2 (effect size) = 0.465, observed power: 0.979; failure load: F = 18.8, p < 0.001; η2 (effect size) = 0.715, observed power: 1.00. Mechanism of failure was also noted and documented with digital images.
Results
Lag screw fixation displayed the highest baseline stiffness (660 ± 83 N/mm). This was not different with the numbers available from the infrapectineal (484 ± 184 N/mm, p = 0.110) or suprapectineal (576 ± 128 N/mm, p = 0.747) groups but greater than posterior (397 ± 104 N/mm, p = 0.006) and anterior buttress plating (447 ± 136 N/mm, p = 0.035) with supplemental lag screw fixation (Table 2). Baseline stiffness was not different with the numbers available between the infrapectineal and suprapectineal groups (p = 0.678).
After 1500 cycles, final stiffness not different with the numbers available between the infrapectineal (568 ± 43 N/mm) and suprapectineal groups (602 ± 87 N/mm, p = 0.988) (Table 2). The infrapectineal group demonstrated a final stiffness greater than the posterior buttress plate with anterior column lag screw group (311 ± 99 N/mm, p = 0.006) but not different with the numbers available from the anterior column buttress plate with posterior column lag screw (390 ± 119 N/mm, p = 0.093) or lag screw groups (423 ± 219 N/mm, p = 0.233). On average, the suprapectineal group demonstrated the greatest stiffness, which was greater than the posterior and anterior buttress plating with supplemental lag screw fixation groups (p = 0.002 and p = 0.031, respectively) but not the lag screw group (p = 0.091) with the numbers available.
After 1500 cycles, the infrapectineal group demonstrated less medial femoral head subluxation (1.2 ± 0.4 mm) when compared with the anterior buttress plate with posterior column lag screw (2.1 ± 0.4 mm, p = 0.017) and lag screw (2.7 ± 0.4 mm, p < 0.001) groups, but there was no difference with the numbers available between the infrapectineal and posterior buttress plate with anterior column lag screw groups (p = 0.993). The suprapectineal group also demonstrated less medial subluxation (1.8 ± 1.4 mm) when compared with the lag screw group (p = 0.020) but was not different with the numbers available from the posterior (p = 0.661) or anterior (p = 0.741) buttress plate groups with supplemental lag screw fixation. Subluxation was not different based on the numbers available between the infrapectineal and suprapectineal groups (p = 0.232) after cyclic loading.
The infrapectineal group (5.4 ± 0.6 kN; 95% confidence interval [CI], 4.9–5.8 kN) failed at greater loads than the lag screw (2.9 ± 0.8 kN; 95% CI, 2.4–3.3 kN; p < 0.001), anterior buttress plate with posterior column lag screw (4.0 ± 0.6 kN; 95% CI, 3.5–4.4 kN; p = 0.001), and suprapectineal groups (4.4 ± 0.3 kN; 95% CI, 3.9–4.8 kN; p = 0.023; Fig. 4). Failure loads were not different between the infrapectineal and posterior buttress plate with anterior column lag screw groups (4.9 ± 0.9 kN; 95% CI, 4.5–5.8 kN; p = 0.614). The suprapectineal group failed at higher loads than the lag screw group (p < 0.001). There was no difference in failure load with the numbers available between the suprapectineal group and the posterior or anterior buttress plate groups (p = 0.387 and p = 0.766, respectively).
Load to failure results show (a) significantly lower failure load relative to the infrapectineal (IP) group (p < 0.023) and (b) significantly lower failure load relative to the suprapectineal (SP) group (p < 0.001). ANOVA effect size = 0.715. LS = lag screw; PBAL = posterior column buttress plate + anterior column lag screw; ABPL = anterior column buttress plate + posterior column lag screw.
The failure mechanism was identical for all specimens in the lag screw group and manifested as a fracture that initiated on the superior fracture fragment adjacent to the head of the posterior column lag screw (Fig. 5). The failure mechanism was the same for all constructs in the posterior buttress plate with lag screw group and manifested as screw pullout and bone fracture inferior to the fracture line on the posterior column. Constructs in the anterior buttress plate with lag screw group all failed through cortical bone fracture that initiated at the most superior screw hole of the buttress plate. In the infrapectineal group, failure occurred through one of two mechanisms: (1) pubic bone fracture that initiated at an adjacent screw hole (n = 5 [71%]); or (2) screw pullout immediately superior to the osteotomy line (n = 2 [29%]). In the suprapectineal group, all constructs failed in similar fashion through screw pullout and fracture at the first screw hole in the quadrilateral surface extension just superior to the osteotomy line.
Representative failure mechanisms (arrows) are shown for (A) posterior and (B) anterior column plating with supplemental lag screw fixation, (C) infrapectineal, and (D) suprapectineal fixation. The failure mechanism of the lag screw constructs is depicted in Fig. 3.
Discussion
The purpose of acetabular fracture reduction and fixation is to (1) allow early, pain-free mobility and (2) mitigate the potential for posttraumatic arthritis by anatomically reducing the articular surface. Ostensibly, the ability to maintain this reduction will be, at least in part, dictated by the stability of the fixation construct used. The transtectal transverse acetabular fracture is a particularly difficult fracture for two reasons. First, it involves the critical weightbearing portion of the acetabulum, increasing the risk of posttraumatic arthritis. Second, the entire medial wall of the acetabulum is detached from the superior aspect of the dome, and therefore, there is no bony structure to prevent medial subluxation of the femoral head. For this reason, traditional fixation techniques have used plates and/or screws to stabilize both the anterior and posterior columns in hopes of preventing any loss of reduction during the healing process [10]. Typically, posterior or anterior approaches that allow direct access to one column have been used to address such fractures. The anterior intrapelvic approach allows for direct visualization of both the anterior column and medial surface of the posterior column allowing for buttress plate fixation of both columns. Newer buttress plate constructs that span both columns through the quadrilateral surface have been developed to take advantage of this surgical approach. However, as a result of their novelty, biomechanical data regarding their stabilizing effects are nonexistent. We therefore aimed to determine if this fixation method confers similar stability to traditional forms of fixation.
This study had several limitations. First, the nature of our experimental design and methods used can only describe the acute biomechanics of repaired transverse acetabular fractures. As such, the results reported here cannot take into account the biological changes that occur in vivo and, therefore, cannot be reasonably extrapolated to time periods beyond the acute postoperative. However, we did choose a rigorous cyclic loading scenario (up to 2.5 × BW) that may be considered worst case, because the loads experienced in vivo after fracture repair may be considerably less, especially in the early postoperative course. Second, we chose to use a synthetic tissue surrogate. Although cadaveric tissue testing may be considered the gold standard in producing results with the highest level of clinical translation and acceptance, prior studies have validated the surrogates against human tissue from a mechanical perspective [3, 4, 6, 7, 16, 17]. The use of synthetic specimens also eliminates bone quality and heterogeneous geometry as confounding factors, which we considered to be an important a priori consideration to adequately interrogate biomechanical differences between the methods of fixation. The fact that our investigation could not be performed in matched pairs renders the choice of a Sawbones tissue surrogate more appropriate. Otherwise, it would have been necessary to allocate 35 cadaveric hemipelvis specimens to five fixation groups such that each was similar in age, bone mineral density, size, and geometry, which would have been a difficult task. Adding validity to our use of the synthetic tissue surrogate was our preliminary validation study, in which we were able to determine that our biomechanical model and loading conditions resulted in identical failure mechanisms between synthetic and cadaveric specimens. Third, because all studies are susceptible to type II errors, ours is likely no exception. We designed our study with a sample size of seven per experimental group, which may be considered relatively small and, resultantly, we may have not been unable to identify all biomechanically meaningful differences as statistically significant. However, a review of our findings indicates that even if we had been able to conclude that all meaningful biomechanical differences were also of statistical significance, this would not have altered the major findings of our study: that the two forms of quadrilateral surface buttress plate designs are biomechanically comparable to traditional forms of transverse acetabular fracture fixation. Thus, we contend that the relatively small sample size used here was of limited consequence when considering the overall study findings and our resultant conclusions.
Our results confirm those of other published reports [1] that lag screw fixation of both columns provides the weakest fixation after cyclical loading and results in the greatest medial subluxation of the femoral head. Additional biomechanical studies using both cadaveric and urethane testing specimens have confirmed that bicolumnar fixation provides the greatest construct stiffness and stability in a transverse acetabular fracture model [9, 14, 15]. In fact, the data show that plate fixation of one column (posterior) and lag screw fixation of the other column (anterior) provide the stiffest construct [9, 15]. Small clinical studies have disputed the fact that bicolumnar fixation is necessary in a transverse fracture model when the symphysis pubis is intact and fixation is placed on the reduced posterior column [5]. Nevertheless, we can agree that a transtectal transverse acetabular fracture is a difficult fracture to obtain and maintain anatomic reduction and has a high propensity for posttraumatic arthritis if reduction is lost and joint incongruity results. For the purpose of this study, we assumed, based on traditional teachings and current biomechanical data, that bicolumnar fixation with a plate and lag screw is the most used and accepted treatment for this fracture pattern and was most appropriate for comparison to the newer quadrilateral surface buttress plate designs. Importantly, our results showed that final stiffness after cyclical loading and resistance to medial subluxation with plates that span the columns and provide quadrilateral surface buttressing were comparable to or better than traditional fixation constructs. In particular, the infrapectineal plate construct demonstrated less medial subluxation when compared with anterior column buttress plating and lag screw fixation and was comparable to the posterior column plating construct. Additionally, the infrapectineal plate construct was stiffer (less motion at the fracture surfaces) than the posterior column plating construct after cyclical loading. The suprapectineal plate construct, although equivalent to single-column plating with lag screws in resisting medial subluxation, was stiffer and resulted in the least fracture surface motion.
Poor bone quality results in atypical fracture patterns that involve the quadrilateral surface (medial wall) of the acetabulum and inability to achieve solid and reliable fixation. Thus, loss of reduction and medial subluxation of the femoral head are not uncommon occurrences in these circumstances. Recent advances in acetabular fracture surgery have involved both novel surgical approaches and fixation constructs, in part to meet the demands posed by an aging osteoporotic patient population. Less invasive surgical exposures with lower morbidity to the patient such as the anterior intrapelvic (modified Stoppa) approach were developed to give access to the posterior column, quadrilateral surface, and anterior column through a single midline incision [2, 8, 13]. With improved access to the quadrilateral surface and the medial aspect of the posterior column, more effective means of buttress plating the medial wall and spanning fixation from the posterior to anterior columns became possible [12]. Thus, the impetus is for newer plate designs that function both to (1) provide a buttress to the quadrilateral surface and prevent medial subluxation of the femoral head and (2) span fixation from the posterior to the anterior column. In this biomechanical study, we compared the strength, rigidity, and construct stiffness of two such plate designs with the traditional methods of bicolumnar fixation using lag screws and column plates and were able to demonstrate that these newer forms of fixation are biomechanically viable options when the less invasive anterior intrapelvic approach is used clinically to address these fractures.
In conclusion, posterior column plating with anterior column lag screw fixation through a posterior approach for transtectal transverse acetabular fractures remains the standard. However, in situations in which a less invasive anterior approach is desired, the use of newer plate designs that span both the anterior and posterior columns and provide a quadrilateral surface buttress presents an alternative method of fixation that is at least comparable to and, in some cases, superior to standard forms of fixation in resisting motion at the fracture and medial subluxation. Although in vitro studies such as ours are requisite to defining baseline efficacy to proposed clinical interventions for the treatment of challenging transverse acetabular fractures, clinical studies are ultimately necessary to confirm the benchtop findings reported here, which are supportive of quadrilateral surface buttressing when an anterior intrapelvic approach is used.
References
Chang JK, Gill SS, Zura RD, Krause WR, Wang GJ. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Relat Res. 2001;392:433–441.
Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123.
Cristofolini L, Viceconti M, Cappello A, Toni A. Mechanical validation of whole bone composite femur models. J Biomech. 1996;29:525–535.
Gardner MP, Chong AC, Pollock AG, Wooley PH. Mechanical evaluation of large-size fourth-generation composite femur and tibia models. Ann Biomed Eng. 2010;38:613–620.
Giordano V, do Amaral NP, Pallottino A, Pires e Albuquerque R, Franklin CE, Labronici PJ. Operative treatment of transverse acetabular fractures: is it really necessary to fix both columns? Int J Med Sci. 2009;6:192–199.
Grover P, Albert C, Wang M, Harris GF. Mechanical characterization of fourth generation composite humerus. Proc Inst Mech Eng H. 2011;225:1169–1176.
Heiner AD. Structural properties of fourth-generation composite femurs and tibias. J Biomech. 2008;41:3282–3284.
Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;297:28–32.
Khajavi K, Lee AT, Lindsey DP, Leucht P, Bellino MJ, Giori NJ. Single column locking plate fixation is inadequate in two column acetabular fractures. A biomechanical analysis. J Orthop Surg Res. 2010;5:30.
Letournel E, Judet R. Fractures of the Acetabulum. 2nd ed. Berlin, Germany: Springer Verlag; 1993.
Olson SA, Kadrmas MW, Hernandez JD, Glisson RR, West JL. Augmentation of posterior wall acetabular fracture fixation using calcium-phosphate cement: a biomechanical analysis. J Orthop Trauma. 2007;21:608–616.
Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004;18:175–178.
Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–270.
Sawaguchi T, Brown TD, Rubash HE, Mears DC. Stability of acetabular fractures after internal fixation. A cadaveric study. Acta Orthop Scand. 1984;55:601–605.
Shazar N, Brumback RJ, Novak VP, Belkoff SM. Biomechanical evaluation of transverse acetabular fracture fixation. Clin Orthop Relat Res. 1998;352:215–222.
Zdero R, Elfallah K, Olsen M, Schemitsch EH. Cortical screw purchase in synthetic and human femurs. J Biomech Eng. 2009;131:094503.
Zdero R, Olsen M, Bougherara H, Schemitsch EH. Cancellous bone screw purchase: a comparison of synthetic femurs, human femurs, and finite element analysis. Proc Inst Mech Eng H. 2008;222:1175–1183.
Acknowledgments
We acknowledge Scott Marberry MD, Kaitlyn Christmas BS, and Max Hoggard BS, for assistance with specimen preparation and instrumentation as well as biomechanical testing and data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
The institution of one or more of the authors (BGS) has received, during the study period, funding from Stryker Trauma (Kiel, Germany). One of the authors certifies that he (HCS) has received or may receive payments or benefits, during the study period, an amount of USD 10,000 to USD 100,000 from Stryker Trauma.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research ® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
This work was performed at the Foundation for Orthopaedic Research & Education, Tampa, FL, USA.
About this article
Cite this article
Kistler, B.J., Smithson, I.R., Cooper, S.A. et al. Are Quadrilateral Surface Buttress Plates Comparable to Traditional Forms of Transverse Acetabular Fracture Fixation?. Clin Orthop Relat Res 472, 3353–3361 (2014). https://doi.org/10.1007/s11999-014-3800-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3800-x