Abstract
Background
Rotator cuff repair is a successful treatment in terms of patient satisfaction and pain relief regardless of the repair method. Although arthroscopic repair is commonly thought to be less painful than open or miniopen repair, studies disagree on this point.
Questions/purposes
We wished to compare the results of patient-reported postoperative pain after open versus arthroscopic rotator cuff repair and to identify any predictors of various pain outcomes in these groups.
Methods
One-hundred two patients (52 with open repair, 50 with arthroscopic repair) participated. Preoperatively, patients reported pain levels and self-perceived pain tolerance, and they underwent a test for an objective measurement of pain tolerance. Intraoperative variables included surgery duration and size of the tear. Postoperatively, patients maintained a pain log for 6 weeks, reporting daily pain (VAS) and narcotic consumption. Outcome variables included days to zero pain, the presence of residual pain, weekly pain levels, and cumulative 6-week pain level. Age, sex, tear size, pain tolerance, surgery duration, and self-reported preoperative pain were analyzed as possible predictors of postoperative pain. This study was powered (β = 0.2 and α = 0.05) to detect a difference of 10% in the VAS and postoperative analgesic use with a requirement of 50 patients in each arm.
Results
Days to zero pain (mean, 28.8 days, 95% CI, 24.8–32.8 days versus 27.6 days, 95% CI, 23.3–31.9 days for open versus arthroscopic, respectively; p = 0.69) were not different between the open and arthroscopic repair groups. There were differences of questionable clinical relevance and borderline statistical significance favoring arthroscopic intervention in the second postoperative week (2.3 versus 3.2 of 10 on the VAS; p = 0.045). Otherwise, no differences were seen between the two groups in terms of residual pain, cumulative pain, or medication use. Consistent predictors of postoperative pain affecting multiple outcome measures included severe preoperative pain, smaller tear size, and female sex.
Conclusions
There were no differences of clinically relevant size between arthroscopic and open rotator cuff surgery in this comparative series. Therefore, the choice of arthroscopic rotator cuff repair should not be based on decreased postoperative pain.
Level of Evidence
Level II, therapeutic study. See the Instructions or Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Beginning in the late 1980s, surgeons began to perform rotator cuff repairs arthroscopically because of the potential benefits of smaller incisions, less trauma to the deltoid, ability to address concomitant disorders, better patient acceptance, and less postoperative pain [8, 18]. Early experience revealed that, despite these potential benefits, postoperative rerupture rates were greater with arthroscopic repair compared with open repair [7, 37]. During the last two to three decades, however, the popularity of arthroscopic cuff repair has increased as surgical technique and technology have improved and patient-reported outcome scores and objective outcomes, such as retear rates, have approached those for open techniques, especially with smaller tears [12, 14, 19, 22, 25].
Almost all clinical outcome measures for patients undergoing open or arthroscopic rotator cuff repair incorporate some determination of pain at final followup. Although arthroscopic repair is thought to be less painful than open or miniopen repair, studies disagree on this point [3, 13, 14, 17, 26, 32]. One of these studies reported decreased pain with the miniopen compared with arthroscopic repair in the fourth postoperative week [14]. However, that study had a small sample size (n = 17 in arthroscopic and miniopen groups) and patients rated their pain on a weekly rather than daily basis. Another study was unable to detect a difference in postoperative pain (decreased in the arthroscopic group) until 6 months after surgery [13]. Pain with either approach within 6 weeks can be severe and likely has a substantial effect on patient satisfaction.
Anecdotally, our practice receives a large number of patient calls on the evening of and day after outpatient arthroscopic cuff repairs. Because of this, we hypothesized that early (6 weeks) postoperative pain after open or arthroscopic rotator cuff repair would not differ.
The purposes of our study, therefore, were to compare postoperative pain during the first 6 weeks after open versus arthroscopic rotator cuff repair, specifically evaluating (1) duration of postoperative pain; (2) residual pain at the end of followup; (3) average weekly pain and analgesic use; and (4) cumulative pain and analgesic use. Our secondary aim was to identify factors that are predictive of pain using these parameters.
Patients and Methods
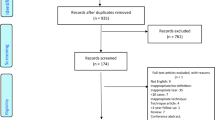
Before enrollment of patients, approval was obtained from the institutional review board. Potential patients were scheduled to undergo an open or arthroscopic rotator cuff repair with an acromioplasty. All open repairs were performed by one senior author (JMF) and all arthroscopic repairs were done by another (GRW). Patients presenting with a concomitant shoulder disorder, prior rotator cuff repair, history of hypersensitivity to or abuse of narcotics, fibromyalgia, or patients collecting workers compensation or long-term disability were excluded. During this time, 150 patients potentially meeting the inclusion criteria underwent open rotator cuff repair while 307 patients potentially meeting the inclusion criteria underwent arthroscopic rotator cuff repair. Attempts were made to obtain consent from all patients meeting inclusion criteria. One hundred forty-five subjects consented to participation in the study and were enrolled between May 2007 and May 2010. Of these, 58 had open rotator cuff repairs and 87 had arthroscopic repairs. Of these, 52 patients who had open repairs (90%) and 50 who had arthroscopic repairs (57%) filled out their pain diaries.
Preoperative Pain Evaluation
In a pilot study regarding pain after open rotator cuff repair (data unpublished), our group found a significant relationship between a preoperative pain tolerance test, the Ouch! Test, preoperative pain level (mild, moderate, and severe), and postoperative pain measures. However, for purposes of the current study, the Ouch! Test should be considered an unvalidated outcomes instrument. The patients in the current study were tested using the Ouch! Test to identify any selection bias based on individual pain tolerance in either group. In brief, the Ouch! Test is performed with a 3-foot tube with openings at 1-foot intervals. During administration of the test, patients place their index finger in an opening at the base of the device while closing their eyes. A lead ball then is dropped on the fingernail of each index finger from the openings at heights of 1, 2, and 3 feet. After each stimulus, patients reported their pain on a scale of 0 to 10. In addition, patients were asked to report their self-perceived pain tolerance preoperatively on a scale of 0 (no tolerance) to 10 (extreme tolerance).
Surgical Technique
Open repair of the rotator cuff was performed in conjunction with an acromioplasty in all cases. All patients received general anesthesia with a scalene block. In all cases, the cuff was repaired to the greater tuberosity with 3-mm nonabsorbable sutures through bone tunnels. The deltoid was reflected from and reattached to the anterior acromion. Arthroscopic repair also was done in conjunction with the acromioplasty. Repair was performed using a double-row, suture bridge technique in all cases. Intraoperative data collection included size of the tear and duration of surgery to the nearest quarter hour. All patients were discharged with standardized instructions for home exercises including passive external rotation of 0° with the arm at the side and passive elevation to 90°. Patients were instructed in these exercises by a physical therapist in the hospital and to perform them three times a day. Oxycodone and acetaminophen 5/325 mg was prescribed for postoperative pain control on discharge. The surgeon (JMF) performing open repair has been doing open repairs exclusively. The surgeon (GRW) performing arthroscopic repair has been doing so for approximately a decade at the initiation of this study, and averages greater than 100 arthroscopic repairs per year. He performs arthroscopic repair on all patients, excluding approximately five to six revisions per year that require a patch.
Patient Characteristics
The patients who completed their diaries had a mean age of 59 years (range, 39–86 years; SD, 10.01) and included 73 men (72%). Preoperative pain level, self-perceived pain tolerance, and Ouch! Test scores were compared between open and arthroscopic groups (Table 1).
Pain Diary
Postoperatively, patients were instructed to record their pain level and oxycodone use daily. Pain levels were recorded on a VAS using a 10-cm horizontal line with “0, no pain” on the left and “10, worst pain imaginable” on the right. Patients were instructed to draw a vertical mark along the line that best represented their degree of shoulder pain relative to the two extremes. Daily analgesic use was recorded as type of analgesic and quantity of tablets. The analgesic use then was normalized using morphine-equivalency dosage, as described previously [29]. Patients were instructed not to use NSAIDs. The daily pain log was maintained by each patient for 6 weeks or until three consecutive pain-free days, whichever came first. Patients who reported three consecutive pain-free days were assigned a daily pain score of 0 for each of the remaining days.
Analysis
Outcome variables included days to pain-free, residual pain [6], average weekly pain levels and analgesic use, and cumulative pain levels and analgesic use. Days to pain-free, a continuous variable, was defined as the number of postoperative days until the first day on which a subjective pain level of 0 was recorded. Patients with pain continuing to postoperative Day 42 were reported as 42 days to pain-free. Residual pain was defined as the presence of any pain on postoperative Day 42. Likewise, a patient with a pain level of zero on postoperative Day 42 did not have residual pain. If the patient did not complete the pain log on postoperative Day 42, the most recent daily pain level was substituted. Weekly pain score averages were calculated for weeks in which at least one daily value was not 0, initiated with postoperative Day 1, and were calculated for the next 6 weeks. Weekly average narcotic use was calculated similarly and was converted to morphine equivalence as indicated previously. Cumulative pain levels and narcotic use were the summation of all average weekly pain levels and narcotic use from postoperative Day 1 to postoperative Day 42.
Furthermore, each of the parameters was analyzed for age, sex, preoperative pain level, tear size, duration of surgery, self-reported pain tolerance, objectively measured pain tolerance, and surgically treated shoulder relative to the primary arm. These variables were compared independently with the four outcome measures to determine their association with postoperative pain.
A priori sample size calculation was performed to detect the required number of patients for this analysis. This analysis provided that a sample size of 50 subjects per treatment group yields 80% power to rule out the null hypothesis that the lower limit of a two-sided 95% confidence limit of the difference in the pain medication requirements and subjective pain assessments between groups is less than 10% under the assumption that the success rate is 84% for both groups. Post hoc power analysis, using the resulting data and α = 0.05, also was performed for each outcome variable to confirm sufficient power.
Univariate analyses were performed on all potential predictors of postoperative pain. Two-tailed Student’s t-tests were performed to determine significant differences between continuous measures. Pearson’s correlation coefficient was used to assess the relationship between two continuous variables. For nonparametric continuous measures, the Mann-Whitney test was used to assess statistical significance. Differences between groups were determined to be significant with a probability less than 0.05. Chi-square tests were performed to determine the significance of differences in which both variables were dichotomous. Statistical analysis was performed using SPSS 20.0 (SPSS Inc, Chicago, IL, USA).
Results
Days to Pain-free
There was no difference in days to pain-free between patients in the open (mean, 28.8 days; 95% CI, 24.8–32.8) and arthroscopic groups (mean, 27.6 days; 95% CI, 23.3–31.9; p = 0.69; power = 5.9%). Tear size (R = −0.29; p = 0.007) was correlated with the duration of postoperative pain. In addition, age (R = −0.07; p = 0.48), duration of surgery (R = −0.05; p = 0.66), and self-perceived pain tolerance (R = −0.16; p = 0.12) had no effect on days to pain-free. Patients who reported severe preoperative pain had greater duration of postoperative pain (35 days) compared with patients without severe preoperative pain (27 days; p = 0.045). Female patients had a longer duration of postoperative pain (33 days) compared with male patients (26 days; p = 0.03). Neither preoperative pain (p = 0.22) nor sex (p = 0.93) was different as a function of surgical group.
Residual Pain
There was no difference between arthroscopic (43%; 19/44) and open (50%; 26/52) groups regarding the percentage of patients with residual pain (p = 0.51; power = 9.6%). A greater percentage of female patients (62% versus 41%; p = 0.11) had residual pain. In addition, patients with residual pain had smaller tear sizes (2.1 versus 2.6 cm; p = 0.02) and lower self-perceived pain tolerance (6.4 versus 7.6; p = 0.01). No differences were found regarding severe preoperative pain (p = 0.33) or surgical duration (p = 0.67).
Average Weekly Pain and Narcotic Use
Patients in the open repair group had greater pain than patients in the arthroscopic group at Week 2 (3.2; 95% CI, 2.5–3.8, versus 2.3, 95% CI, 1.8–2.8; p = 0.045), whereas pain between groups was similar during the other weeks (Table 1). The average pain for each group decreased from week to week through 6 weeks. Patients in the open and arthroscopic groups had similar analgesic use during all weeks recorded (Table 1).
Average weekly pain was greater during all weeks for patients with severe preoperative pain (p < 0.008). Shorter surgery duration (R = −0.22) was associated with greater postoperative pain during Week 1 (p = 0.047). In addition, smaller tear sizes correlated with greater average pain during Weeks 4 (R = −0.28; p = 0.01), 5 (R = 0.30; p = 0.005), and 6 (R = −0.28; p = 0.01). However, the tear size (p = 0.32) was not different between the two surgical groups. The Ouch! Test was positively correlated (R = 0.20; p = 0.04) with pain levels during the first postoperative week whereas pain was inversely correlated with self-perceived pain tolerance during the second (R = −0.23; p = 0.02) and third postoperative weeks (R = −0.22; p = 0.03). Female patients had greater average pain during the sixth postoperative week compared with male patients (1.6 versus 0.78; p = 0.03). Age was correlated with analgesic use during the first postoperative week (R = −0.26; p = 0.01).
Cumulative Pain Levels and Narcotic Use
There was no difference in cumulative pain levels (113.5 [95% CI, 91.5–135.5] versus 96.7 [95% CI, 76.0–117.3]; p = 0.28 power = 18.3%) or analgesic use (380.4 mg [95% CI, 249.1–511.7] versus 327.8 mg [95% CI, 239.8–415.8]; p = 0.96, power = 9.5%) between open and arthroscopic groups (Table 1). Tear size was inversely correlated (R = −0.25; p = 0.02) with cumulative pain. Age was inversely correlated (R = − 0.21; p = 0.05) with cumulative analgesic use. Cumulative pain and analgesic use were greater for patients with severe preoperative pain (p < 0.01).
Discussion
During the last decade, there has been a transition from open to arthroscopic rotator cuff repair [1, 23, 34, 35]. Arthroscopic repair has advantages, including smaller incisions and less disturbance of the normal shoulder musculature. Less postoperative pain also is thought to be an advantage of arthroscopic surgery [4, 9, 20, 32, 36], but this has not been substantiated. Because of controversy regarding pain relief, we wished to compare patients undergoing open or arthroscopic rotator cuff repair regarding (1) days to pain-free; (2) residual pain at the end of followup; (3) average weekly pain and narcotic use; and (4) cumulative pain and narcotic use. We also sought to identify factors that predict postoperative pain using these parameters.
Our study has limitations including differential loss to followup, lack of anatomic data, lack of randomization, and small sample size. First, there was a substantial difference between the percentage of patients who filled out the pain diaries in the treatment groups (90% and 57% in the open and arthroscopic groups, respectively). It is difficult to know what influence this might have had in this analysis. We do not think that patients’ compliance with the pain diary was driven by their individual pain experience but rather differences in reminders provided to them. However, these results must be weighed with this difference in followup. We did not obtain anatomic data for cuff integrity and it is possible that at least some of the repairs failed early and could have resulted in worse pain outcomes. Current repair failure rates in small tears probably are similar with arthroscopic and open repairs, but in large tears, data would favor open repairs as having a lower retear rate [2]. However, there was no difference in our study in the percentage of patients with small and large tears who underwent open or arthroscopic repair. Although our study was prospective, patients were not randomized. It is possible that surgeon selection bias could have influenced patients’ early postoperative pain experience. However, there were no differences between groups in the influential preoperative variables that we measured. Finally, our patient cohort was relatively small and homogeneous. However, a prior power analysis provided that this sample size would be sufficient for detecting a meaningful difference between the two groups. In assessing the post hoc power analysis, while the resulting power is low, the differences between the groups also were small leading to the small power sizes. Pain analysis, a subjective outcome, also has significant variability between individuals resulting in large distributions among the groups and requiring large sample sizes to detect differences. Our results may not be transferable to other patient groups that are larger and more heterogeneous. Despite these limitations, our results indicate that factors other than surgical method influence early postoperative pain and narcotic use.
We found equivalent times to pain-free for open and arthroscopic repair groups, equivalent proportions of patients in each group reporting residual pain at the end of 6 weeks, and comparable weekly pain and analgesic use. Existing studies have compared postoperative pain after arthroscopic and either open or miniopen cuff repair [3, 13, 14, 17, 26, 32], however, only one study focused on the early (6 weeks) postoperative pain experience [14]. That study had a small sample size and patients rated their pain on a weekly rather than daily basis, thus compromising the results. However, they did note decreased pain in the miniopen group after 4 weeks and decreased analgesic use in the arthroscopic group during the first week. Pain during the early postoperative period likely has a strong relationship to soft tissue and bone manipulations that occur during the surgical procedure. Our results indicate that none of the pain outcome measures we used in this study were effectively improved with arthroscopic cuff repair in comparison to open repair. These measures include duration of postoperative pain, presence of residual pain at the end of the study period (6 weeks), average weekly postoperative pain levels and analgesic use, and cumulative postoperative pain levels and analgesic use. There was a trend for increased early postoperative pain in Weeks 1 and 2 for patients who had an open compared with arthroscopic approach. However, although this difference did reach statistical significance in the second week, the differences observed in this analysis did not meet the threshold of a minimum clinically important difference previously reported for the VAS [15, 16, 31], specifically with rotator cuff repair [30]. Furthermore, this understanding applies to all endpoints of pain measurement, including analgesic use. Although there is a possible Type II error preventing detection of a statistically significant difference, the variation between procedures regarding postoperative pain in our patients is not clinically meaningful. For example, in a post hoc analysis using the open results, to statistically detect the minimum clinically important difference in decreased cumulative pain in the arthroscopic group a sample size of 60 patients (30 in each arm) is the number that would be required. Therefore, early postoperative pain does not appear to be among the real or perceived advantages of arthroscopic rotator cuff repair in comparison to open repair. Moreover, early postoperative pain experience may be based on other perioperative factors.
We found several patient-related factors that were associated with differences in patient-reported pain. Preoperative pain, self-perceived pain tolerance, female sex, and tear size were found to have a significant relationship with some of the outcome measures but no influence on the effect of surgical method. Patients with severe preoperative pain, as categorized preoperatively by the patient, had a greater number of days to pain-free, greater average weekly and cumulative postoperative pain, and increased analgesic requirements. Preoperative pain was found to be a predictor of postoperative pain in nonorthopaedic procedures [10, 11, 21]. This suggests that patients with exaggerated pain responses may be identified preoperatively and treated appropriately. One of the outcome measures that was found to be related to a patient’s self-perceived pain tolerance was the presence of residual pain 6 weeks postoperatively. This finding is in agreement with that of a previous study on needle electromyography, which showed that residual pain, but not immediate pain, correlated with self-perceived pain tolerance [28]. In addition, patients with high self-reported pain tolerance had decreased pain levels during postoperative Weeks 2 and 3. The Ouch! Test also predicted pain during the first postoperative week in this analysis. Female patients were more likely to have residual pain, increased pain during the sixth postoperative week, and a longer duration of postoperative pain compared with male patients. This is consistent with findings in another study [33]. In particular, female patients have been shown to experience greater pain than male patients after arthroscopic knee surgery [27], dental surgery [5], and thoracotomy [24]. Decreased surgery duration predisposed to increased pain during the first postoperative week. This might point to the relationship between time of surgery and surgical approach (with arthroscopic surgery being longer) and the difference in pain between these two groups. The association between decreased tear size and increased duration of pain, presence of residual pain, increased pain during the final 3 weeks, and increased cumulative pain suggests a strong association between pain and tear size that is not understood. In this cohort, 68% (63/92) of patients had a tear size smaller than 2.5 cm while 32% (29/92) had a tear size between 3 and 5 cm, with 10 patients without reported data. However, no difference in tear size between surgical approaches or patients with severe preoperative pain was appreciated.
Arthroscopic rotator cuff repair likely will continue to be popular because of real and perceived benefits, including smaller incisions, less deltoid morbidity, better ability to identify and manage concomitant disorders, and greater patient acceptance. However, pain relief during the early postoperative period may not be one of the advantages of arthroscopic repair. We found other factors, such as preoperative pain and individual pain tolerance, are more predictive of early postoperative pain than the surgical method. When counseling patients undergoing either open or arthroscopic rotator cuff repair, it is important to understand these factors and realize that pain management may be challenging with either type of repair.
References
Baker CL, Whaley AL, Baker M. Arthroscopic rotator cuff tear repair. J Surg Orthop Adv. 2003;12:175–190.
Bishop J, Klepps S, Lo IK, Bird J, Gladstone JN, Flatow EL. Cuff integrity after arthroscopic versus open rotator cuff repair: a prospective study. J Shoulder Elbow Surg. 2006;15:290–299.
Buess E, Steuber KU, Waibl B. Open versus arthroscopic rotator cuff repair: a comparative view of 96 cases. Arthroscopy. 2005;21:597–604.
Demirhan M, Esenyel CZ. [All arthroscopic treatment of rotator cuff tears][in Turkish]. Acta Orthop Traumatol Turc. 2003;37(suppl 1):93–104.
Faucett J, Gordon N, Levine J. Differences in postoperative pain severity among four ethnic groups. J Pain Symptom Manage. 1994;9:383–389.
Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJL, Gross M. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008;13:335–341.
Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–224.
Gartsman GM. Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone Joint Surg Am. 1990;72:169–180.
Gartsman GM. All arthroscopic rotator cuff repairs. Orthop Clin North Am. 2001;32:501–510, x.
Gramke HF, de Rijke JM, van Kleef M, Kessels AG, Peters ML, Sommer M, Marcus MA. Predictive factors of postoperative pain after day-case surgery. Clin J Pain. 2009;25:455–460.
Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111:657–677.
Itoi E, Tabata S. Incomplete rotator cuff tears: results of operative treatment. Clin Orthop Relat Res. 1992;284:128–135.
Kang L, Henn RF, Tashjian RZ, Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573–582, 582.e1–2.
Kasten P, Keil C, Grieser T, Raiss P, Streich N, Loew M. Prospective randomised comparison of arthroscopic versus mini-open rotator cuff repair of the supraspinatus tendon. Int Orthop. 2011;35:1663–1670.
Kelly AM. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med. 1998;5:1086–1090.
Kelly AM. The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J. 2001;18:205–207.
Köse KC, Tezen E, Cebesoy O, Karadeniz E, Guner D, Adiyaman S, Demirtas M. Mini-open versus all-arthroscopic rotator cuff repair: comparison of the operative costs and the clinical outcomes. Adv Ther. 2008;25:249–259.
Levy HJ, Uribe JW, Delaney LG. Arthroscopic assisted rotator cuff repair: preliminary results. Arthroscopy. 1990;6:55–60.
Lindley K, Jones GL. Outcomes of arthroscopic versus open rotator cuff repair: a systematic review of the literature. Am J Orthop (Belle Mead, NJ). 2010;39:592–600.
Millar NL, Wu X, Tantau R, Silverstone E, Murrell GA. Open versus two forms of arthroscopic rotator cuff repair. Clin Orthop Relat Res. 2009;467:966–978.
Mobilio N, Gremigni P, Pramstraller M, Vecchiatini R, Calura G, Catapano S. Explaining pain after lower third molar extraction by preoperative pain assessment. J Oral Maxillofac Surg. 2011;69:2731–2738.
Morse K, Davis AD, Afra R, Kaye EK, Schepsis A, Voloshin I. Arthroscopic versus mini-open rotator cuff repair: a comprehensive review and meta-analysis. Am J Sports Med. 2008;36:1824–1828.
Norberg FB, Field LD, Savoie FH 3rd. Repair of the rotator cuff: mini-open and arthroscopic repairs. Clin Sports Med. 2000;19:77–99.
Ochroch EA, Gottschalk A, Troxel AB, Farrar JT. Women suffer more short and long-term pain than men after major thoracotomy. Clin J Pain. 2006;22:491–498.
Osti L, Papalia R, Paganelli M, Denaro E, Maffulli N. Arthroscopic vs mini-open rotator cuff repair: a quality of life impairment study. Int Orthop. 2010;34:389–394.
Pearsall AW 4th, Ibrahim KA, Madanagopal SG. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res. 2007;2:24.
Rosseland LA, Stubhaug A. Gender is a confounding factor in pain trials: women report more pain than men after arthroscopic surgery. Pain. 2004;112:248–253.
Strommen JA, Daube JR. Determinants of pain in needle electromyography. Clin Neurophysiol. 2001;112:1414–1418.
Svendsen K, Borchgrevink P, Fredheim O, Hamunen K, Mellbye A, Dale O. Choosing the unit of measurement counts: the use of oral morphine equivalents in studies of opioid consumption is a useful addition to defined daily doses. Palliat Med. 2011;25:725–732.
Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18:927–932.
Todd KH. Clinical versus statistical significance in the assessment of pain relief. Ann Emerg Med. 1996;27:439–441.
Warner JJ, Tétreault P, Lehtinen J, Zurakowski D. Arthroscopic versus mini-open rotator cuff repair: a cohort comparison study. Arthroscopy. 2005;21:328–332.
Wiesenfeld-Hallin Z. Sex differences in pain perception. Gend Med. 2005;2:137–145.
Yamaguchi K, Ball CM, Galatz LM. Arthroscopic rotator cuff repair: transition from mini-open to all-arthroscopic. Clin Orthop Relat Res. 2001;390:83–94.
Yamaguchi K, Levine WN, Marra G, Galatz LM, Klepps S, Flatow EL. Transitioning to arthroscopic rotator cuff repair: the pros and cons. Instr Course Lect. 2003;52:81–92.
Yu J, Higgins LD, Moorman CT 3rd. Technique for arthroscopic rotator cuff repair. J Surg Orthop Adv. 2006;15:154–159.
Zumstein MA, Jost B, Hempel J, Hodler J, Gerber C. The clinical and structural long-term results of open repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2008;90:2423–2431.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Williams, G., Kraeutler, M.J., Zmistowski, B. et al. No Difference in Postoperative Pain After Arthroscopic versus Open Rotator Cuff Repair. Clin Orthop Relat Res 472, 2759–2765 (2014). https://doi.org/10.1007/s11999-014-3715-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3715-6