Abstract
Background
Minimally invasive surgical (MIS) approaches to transforaminal lumbar interbody fusion (TLIF) have been developed as an alternative to the open approach. However, concerns remain regarding the adequacy of disc space preparation that can be achieved through a minimally invasive approach to TLIF.
Questions/purposes
The purpose of this cadaver study is to compare the adequacy of disc space preparation through MIS and open approaches to TLIF. Specifically we sought to compare the two approaches with respect to (1) the time required to perform a discectomy and the number of endplate violations; (2) the percentage of disc removed; and (3) the anatomic location where residual disc would remain after discectomy.
Methods
Forty lumbar levels (ie, L1-2 to L5-S1 in eight fresh cadaver specimens) were randomly assigned to open and MIS groups. Both surgeons were fellowship-trained spine surgeons proficient in the assigned approach used. Time required for discectomy, endplate violations, and percentage of disc removed by volume and mass were recorded for each level. A digital imaging software program (ImageJ; US National Institutes of Health, Bethesda, MD, USA) was used to measure the percent disc removed by area for the total disc and for each quadrant of the endplate.
Results
The open approach was associated with a shorter discectomy time (9 versus 12 minutes, p = 0.01) and fewer endplate violations (one versus three, p = 0.04) when compared with an MIS approach, percent disc removed by volume (80% versus 77%, p = 0.41), percent disc removed by mass (77% versus 75%, p = 0.55), and percent total disc removed by area (73% versus 71%, p = 0.63) between the open and MIS approaches, respectively. The posterior contralateral quadrant was associated with the lowest percent of disc removed compared with the other three quadrants in both open and MIS groups (50% and 60%, respectively).
Conclusions
When performed by a surgeon experienced with MIS TLIF, MIS and open approaches are similar in regard to the adequacy of disc space preparation. The least amount of disc by percentage is removed from the posterior contralateral quadrant regardless of the approach; surgeons should pay particular attention to this anatomic location during the discectomy portion of the procedure to minimize the likelihood of pseudarthrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intervertebral disc space preparation is a vital step in performing lumbar interbody fusion regardless of the approach. Inadequate removal of disc material and vertebral body endplate cartilage increases the risk of pseudarthrosis. Li et al. [9] showed that nucleus pulposis mixed with bone graft slows down the rate of bony growth, possibly through inflammatory mediators. Lowe et al. [10] asserted that total area of discectomy and endplate preparation play a role in fusion rate. Thus, the goals of disc space preparation when performing lumbar interbody fusion are to thoroughly remove the disc and endplate cartilage, expose the underlying bleeding endplate bone, and avoid gross violation of the endplate.
Initially described in the early 1980 s by Harms and Rolinger [4], transforaminal lumbar interbody fusion (TLIF) has become a popular approach to achieving interbody fusion through a posterior approach. More recently, with the advent of sophisticated retractor systems and instrumentation, minimally invasive approaches to the TLIF have become popular in an attempt to decrease surgical morbidity and length of hospital stay and hasten recovery [1, 3, 8, 12]. However, concerns remain regarding the adequacy of disc space preparation that can be achieved through a minimally invasive approach to TLIF [16]. Whether minimally invasive surgical (MIS) approaches are sufficient to perform adequate disc space preparation remains an unanswered question [11].
To the best of our knowledge, there has been no cadaveric study comparing the effectiveness of disc space preparation in TLIF between MIS and open approaches.
We therefore sought to compare the efficacy of disc space preparation in unilateral TLIF between minimally invasive and open approaches. Specifically we sought to compare the two approaches with respect to (1) the time required to perform a discectomy and the number of endplate violations; (2) the percentage of disc removed; and (3) the anatomic location where residual disc would remain after discectomy.
Materials and Methods
Forty lumbar levels (ie, L1-2 to L5-S1) from eight fresh cadaver specimens were randomly assigned to open and MIS groups using a random number generator. All cadavers contained both MIS and open levels. All approaches were unilateral and performed from the right side.
Two fellowship-trained orthopaedic spine surgeons (JAR, DGA) performed all the discectomies. One surgeon was responsible for all of the MIS disc space preparations (DGA), whereas another surgeon performed all the open disc space preparations (JAR). Both surgeons were proficient in the assigned approach and routinely used the assigned approach in their clinical practice. The MIS procedures were performed through a 21-mm diameter straight, fixed tubular retractor (Spotlight; DePuy Spine, Inc, Rayhnam, MA, USA). The open approach and disc space preparation were performed through an open incision with standard soft tissue retractors. Both procedures involved (1) osteotomy of the pars and lamina of the involved cranial vertebra performed using a ¼-inch straight osteotome with subsequent removal of the pars and inferior articular process of the cranial vertebra; (2) skeletonization of the ipsilateral pedicle of the caudal vertebra and additional laminectomy using Kerrison rongeurs; (3) annulotomy using a #15 blade scalpel; and (4) disc space preparation. Both surgeons performed manual discectomies using a combination of straight and curved curettes, double-angled curettes, endplate shavers, and pituitary rongeurs. The Kerrison rongeurs and curettes used in the MIS procedure (Spotlight; DePuy Spine, Inc) were appropriately bayonetted to allow access through the tubular retractor. All other instruments used for the approach and disc space preparation were the same for both the MIS and open procedures.
The time of discectomy and number of instrument passes were recorded for each level. The time of discectomy began with annulotomy and ended when the surgeon declared that the discectomy and endplate preparation were complete to the best of his ability. An observer for each surgeon counted the number of instrument passes using a counter. An instrument pass was defined as complete removal of the instrument from the disc space once the instrument had been placed through the annulotomy. We kept track of this number as the more times an instrument is passed into the surgical field, the higher the likelihood of endplate violation, dural tear, or nerve root injury.
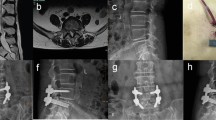
During disc space preparation, all disc and cartilaginous material that was removed from each level was collected by an assistant and measured by both mass and volume. After all levels of a given cadaver were completed, the soft tissue was dissected off of the spine and each disc space was opened and was directly inspected for evidence of gross endplate violation of either the superior or inferior endplate. We defined an endplate violation as a breech of the vertebral body endplate with exposed cancellous bone. A digital image of the superior and inferior endplate of each level was obtained using a digital camera. The remainder of the disc and cartilaginous material was then removed from the superior and inferior endplate of each level, and the mass and volume of this residual material were determined. This allowed determination of total disc per level by both mass and volume (ie, that disc removed at the time of the TLIF discectomy plus the disc removed after opening each disc and removing what remained). The percentage of disc volume and disc mass removed through the TLIF approach was calculated for each level. A digital imaging software program (ImageJ; US National Institutes of Health, Bethesda, MD, USA) was used to measure the surface area and percentage of disc removed from each endplate (Fig. 1). Percentage of disc removed by area was calculated for the total disc and for each quadrant of the endplate (ie, anterior ipsilateral, anterior contralateral, posterior ipsilateral, and posterior contralateral). Measurements of the superior endplate and the inferior endplate were averaged to obtain a single measurement for each level. Two independent observers (SDG, PS) made measurements of disc area removed in a blinded fashion.
Image demonstrating a vertebral body endplate after the discectomy. This is an example of an image that was used to determine percent of disc removal by surface area using the distal imaging software. The solid black line demonstrates the outline of the total disc area. The dotted black line outlines the demarcation between the exposed endplate (solid black arrow) and remaining disc (open arrow). A = anterior; P = posterior; I = ipsilateral; C = contralateral.
Time of discectomy, number of instrument passes, and percentage of disc removed by volume, mass, and area were compared between MIS and open approaches using Student’s t-test. Incidence of endplate violations was compared between MIS and open approaches using a chi square test. Interobserver correlation coefficient (ICC) was calculated for percentage of disc area removed between observers.
Results
The MIS procedures took longer and resulted in more endplate violations but did not require more instrument passes (Table 1). The MIS group and the open group discectomies were performed in an average of 11.5 minutes and 9.3 minutes with an SD of 2.7 and 2.6, respectively (p = 0.01). There was no difference in the number of instrument passes between the MIS and open groups (31.1 versus 33.5 passes, SD = 7.8 versus 8.9, respectively, p = 0.42). There were fewer endplate violations in the open group compared with the MIS group (one versus three, respectively, p = 0.04).
There were no differences between the approaches in terms of the amount of disc removed (Table 1). The average amount of disc removed by volume and mass for the MIS group was 12.5 cc and 13.1 g with a SD of 4.8 and 4.5, respectively. The average amount of disc removed by volume and weight for the open group was 13.4 cc and 13.9 g with an SD of 7.1 and 6.5, respectively (p = 0.63 and 0.65, respectively). The average percentage of disc removed in the discectomy of the MIS group by volume and weight was 77% and 75%, respectively, with an SD of 12% and 13%, respectively. The average percent of disc removed in the discectomy of the open group by volume and weight was 80% and 77%, respectively, with an SD of 8.4% and 8.5%, respectively (p = 0.41 and 0.55, respectively). As determined by the digital imaging software program, the average percent of disc removed by area (ie, total disc area) of the MIS and open groups was 71% and 73% with an SD of 16.0% and 15.6%, respectively (p = 0.63). The ICC for percent of disc area removed was 0.737 (95% confidence interval, 0.589–0.831).
Area of disc removed by quadrants was also determined (ie, posterior ipsilateral, posterior contralateral, anterior ipsilateral, and anterior contralateral). Contralateral and ipsilateral refer to the side of the osteotomy and approach to the disc space. There were no differences in percentage of disc removed in the posterior ipsilateral, anterior ipsilateral, and anterior contralateral quadrants between the MIS and open groups (p = 0.98, 0.11, and 0.62, respectively). With the numbers available, there was also no difference in the percentage of disc area removed in the posterior contralateral quadrant between the MIS and open groups (60% versus 50%, SD = 29% versus 26%, respectively, p = 0.056).
In the MIS group, 83%, 73%, 71%, and 60% of the disc space area was removed in the posterior ipsilateral, anterior ipsilateral, anterior contralateral, and posterior contralateral quadrants, respectively (Fig. 2). In the open group, 83%, 83%, 74%, and 50% of the disc space area was removed in the posterior ipsilateral, anterior ipsilateral, anterior contralateral, and posterior contralateral quadrants, respectively (Fig. 3). There was a lower percentage of disc removed in the posterior contralateral quadrant compared with the posterior ipsilateral quadrant in both the MIS and open groups (p < 0.001 for MIS and open groups). In the open group, there was a lower percentage of disc removed in the posterior contralateral quadrant compared with the anterior contralateral quadrant (p < 0.001). In the MIS group, with the numbers available, there was no difference in percentage of disc removed in the posterior contralateral quadrant compared with the anterior contralateral quadrant (p = 0.067). In both the MIS and open groups, there was no difference between the anterior contralateral and anterior ipsilateral quadrants (p = 0.82 and 0.061 for MIS and open, respectively). There was a lower percentage of disc removed from the anterior ipsilateral quadrant compared with the posterior ipsilateral quadrant in the MIS group (p = 0.035). There was no difference in the percentage of disc removed in the anterior ipsilateral quadrant compared with the posterior ipsilateral quadrant in the open group (p = 0.96).
Discussion
TLIF has become an increasingly popular approach to obtaining combined anterior and posterolateral lumbar fusion. Adequate disc space preparation performed through a unilateral posterolateral annulotomy is an essential component of the TLIF procedure. Adequate disc space preparation exposes the underlying bleeding bony endplates and provides adequate surface area across which an anterior intervertebral body fusion can form. The traditional open approach to TLIF involves bilateral elevation and retraction of the paraspinal muscles. This provides adequate exposure through which a unilateral facetectomy, annulotomy, and disc space preparation can be performed. MIS approaches to the TLIF have been developed with the goals of decreasing surgical morbidity, decreasing hospital stay, and hastening recovery [1, 3, 8, 12]. However, concerns remain about the adequacy of the disc space preparation in a minimally invasive approach to the TLIF [16]. To our knowledge, no prior studies have studied the adequacy of disc space preparation through the MIS TLIF approach. We therefore performed a cadaver study to compare the open with the MIS approach to TLIF and found that the MIS approach took longer and resulted in more endplate perforations but achieved a similarly complete discectomy to the open approach.
This study had a number of limitations. First, one surgeon (DGA) performed the entire MIS leg of the study, whereas another surgeon (JAR) performed the entire open leg of the study. The involvement of just two surgeons, each performing a single leg of the study, introduces a potential confounding variable in level of experience and comfort with his respective procedure. Second, this study is limited by the fact that it is an in vitro cadaveric study. Because there is no risk of actual nerve root damage, we may have inadvertently been more aggressive in performing the disc space preparation. Thus, the results of this study may overestimate the amount of disc removed in an in vivo setting. Furthermore, this study does not address the clinical significance of disc space preparation in regard to fusion rate or clinical outcome and does not suggest that TLIF is superior in anyway to other approaches to interbody fusion, because data do exist that call into question the clinical benefit of the TLIF procedure over other methods of lumbar fusion [5]. Numerous aspects of the TLIF procedure that may affect clinical and radiographic outcomes such as cage placement, bone grafting, and instrumentation were not addressed as part of this study. Furthermore, there are numerous variations of the MIS approach to TLIF, and the results of this particular study are applicable only to the unilateral MIS approach performed through a tubular retractor according to the methods described.
We found that the MIS approach took slightly longer and resulted in more violations of the endplate but did not require more instrument passes. It is unclear what clinical relevance the increased disc space preparation time in the MIS approach would have. Although some previous studies have found no significant difference in operative time between MIS and open approaches [8, 17], others have found that MIS TLIF is associated with a longer operative time [13]. Few studies have examined endplate violations and instrument passes in MIS and open TLIF, although concerns over adequate exposure in the MIS approach make these measures valuable information. In our study, it is unclear whether the increased number of endplate violations was resulting from inadequate visualization of the field or whether a more aggressive discectomy was performed in the in vitro setting than would otherwise be performed in an in vivo setting.
In addition, the current study found that both MIS and open approaches were similar in their adequacy of disc space preparation in regard to volume of disc, mass of disc, and percent of disc removed by surface area. Javernick et al. [6] studied disc space preparation through an open TLIF approach in patients undergoing one- or two-level TLIF. These authors reported that 69% of the total disc volume was removed from a unilateral approach. A postoperative CT scan was used to determine that 80% of the disc by surface area was removed using a bilateral approach. This study was limited in that it was an in vivo study, thus limiting the analysis that could be performed on the endplates after disc space preparation. In 2011, Pumberger et al. [14] performed an in vitro, human cadaveric study comparing manual versus powered discectomy (ie, using a handheld, battery-powered discectomy device) in a unilateral TLIF approach. These authors reported a 36.3% and 46.8% area of discectomy and endplate preparation for the manual and powered discectomies, respectively (p = 0.025). The least amount of disc removal using both techniques was in the posterior, contralateral quadrant. This and other recent studies compare manual discectomy with discectomy using various automated devices for the TLIF procedure but do not compare manual discectomy performed through the open and MIS TLIF approaches [2, 7, 14].
We also found that the posterior contralateral quadrant was the most difficult quadrant of the disc to remove in a unilateral TLIF in both MIS and open approaches. Pumberger et al., in two separate cadaveric studies, also found that the posterior contralateral quadrant was the most difficult disc quadrant to prepare in a unilateral TLIF [14, 15]. Although there was no difference in disc removed from the anterior ipsilateral quadrant compared with the posterior ipsilateral quadrant in the open approach, the MIS approach was slightly less effective at removing disc from the anterior ipsilateral quadrant compared with the posterior ipsilateral quadrant. This difference may relate to the visualization and access through the tubular retractor, which may limit access to the anterior ipsilateral quadrant.
This study found in a cadaver model that the unilateral MIS approach to TLIF, performed through a tubular retractor, provides similar disc space preparation when compared with the traditional open approach. The least amount of disc by percentage is removed from the posterior contralateral quadrant regardless of the approach. Although this study shows similar disc space preparation using both approaches, differences that may exist in clinical and radiographic outcomes between these approaches need to be further studied.
References
Archavlis E, Carvi y Nievas M. Comparison of minimally invasive fusion and instrumentation versus open surgery for severe stenotic spondylolisthesis with high-grade facet joint osteoarthritis. Eur Spine J. 2013;22:1731–1740.
Freedman BA, Rhee JM, Jackson KL. Preparing the lumbar intervertebral disk space for interbody procedures: a comparison between the traditional method and a new automated method. J Spinal Disord Tech. 2012;25:E1–6.
Gandhi SD, Anderson DG. Minimally invasive surgery for the lumbar spine. J Neurosurg Sci. 2012;56:27–34.
Harms J, Rolinger H. [A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl)]. Z Orthop Ihre Grenzgeb. 1982;120:343–347.
Hoy K, Bunger C, Niederman B, Helmig P, Hansen ES, Li H, Andersen T. Transforaminal lumbar interbody fusion (TLIF) versus posterolateral instrumented fusion (PLF) in degenerative lumbar disorders: a randomized clinical trial with 2-year follow-up. Eur Spine J. 2013;22:2022–2029.
Javernick MA, Kuklo TR, Polly DW Jr. Transforaminal lumbar interbody fusion: unilateral versus bilateral disk removal–an in vivo study. Am J Orthop (Belle Mead NJ). 2003;32:344–348; discussion 348.
Le Huec JC, Assaker R. Comparison of powered Spine Shaver and conventional discectomy for TLIF: a randomized cadaver specimens study. J Spinal Disord Tech. 2012;25:249–253.
Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J. 2012;21:2265–2270.
Li H, Zou X, Laursen M, Egund N, Lind M, Bunger C. The influence of intervertebral disc tissue on anterior spinal interbody fusion: an experimental study on pigs. Eur Spine J. 2002;11:476–481.
Lowe TG, Hashim S, Wilson LA, O’Brien MF, Smith DA, Diekmann MJ, Trommeter J. A biomechanical study of regional endplate strength and cage morphology as it relates to structural interbody support. Spine (Phila Pa 1976). 2004;29:2389–2394.
Ozgur BM, Yoo K, Rodriguez G, Taylor WR. Minimally-invasive technique for transforaminal lumbar interbody fusion (TLIF). Eur Spine J. 2005;14:887–894.
Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, McGirt MJ. Minimally invasive versus open transforaminal lumbar interbody fusion (TLIF) for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg. 2013 Jan 12 [Epub ahead of print].
Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 2009;34:1385–1389.
Pumberger M, Gogia J, Hughes AP, Kotwal SY, Girardi FP, Sama AA. Conventional manual discectomy versus powered discectomy for interbody fusion in the lumbar spine: cadaveric testing in forty levels. J Spinal Disord Tech. 2011;24:E71–74.
Pumberger M, Hughes AP, Girardi FP, Gogia J, Kotwal SY, Thaler C, Sama AA. Influence of surgical experience on the efficiency of discectomy in TLIF: a cadaveric testing in 40 levels. J Spinal Disord Tech. 2012;25:E254–258.
Reitman CA, Anderson DG, Fischgrund J. Surgery for degenerative spondylolisthesis: open versus minimally invasive surgery. Clin Orthop Relat Res. 2013;471:3082–3087.
Seng C, Siddiqui MA, Wong KP, Zhang K, Yeo W, Tan SB, Yue WM. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976). 2013;38:2049–2055.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors certifies that he (JAR, ARV, ASH, TJA, DGA) has received benefits during the study period, in the form of an institutional research grant, an amount of USD 10,000 to USD 100,000, from DePuy Spine Inc (Raynham, MA, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Thomas Jefferson University Hospital, Philadelphia, PA, USA.
About this article
Cite this article
Rihn, J.A., Gandhi, S.D., Sheehan, P. et al. Disc Space Preparation in Transforaminal Lumbar Interbody Fusion: A Comparison of Minimally Invasive and Open Approaches. Clin Orthop Relat Res 472, 1800–1805 (2014). https://doi.org/10.1007/s11999-014-3479-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3479-z