Abstract
Background
The Charlson Comorbidity Index (CCI) originally was developed to predict mortality within 1 year of hospital admission in patients without trauma. As it includes factors associated with medical and surgical complexities, it also may be useful as a predictive tool for hospital readmission after orthopaedic surgery, but to our knowledge, this has not been studied.
Questions/purposes
We asked whether an increased score on the CCI was associated with (1) readmission, (2) an increased risk of surgical site infection or other adverse events, (3) transfusion risk, or (4) mortality after orthopaedic surgery.
Methods
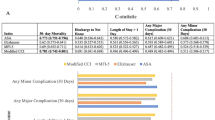
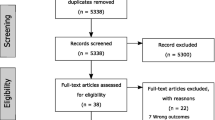
A total of 30,129 orthopaedic surgeries performed between 2008 and 2011 without any orthopaedic surgery in the preceding 30 days were analyzed. International Classification of Diseases, 9th Revision codes were used to identify diagnoses, procedures, surgery-related adverse events, surgical site infection, and comorbidities as listed in the updated and reweighted CCI. A total of 913 patients (3.0%) were readmitted within 30 days after discharge; in 393 (1.4%) patients adverse events occurred; 417 patients (1.4%) had a surgical site infection develop; 211 (0.7%) needed transfusions, and 56 (0.2%) died within 30 days after surgery. Ordinary least squares regression analyses were used to determine whether the CCI was associated with these outcomes.
Results
The CCI accounted for 10% of the variation in readmissions. Every point increase in CCI score added an additional 0.45% risk in readmission for patients undergoing arthroplasty, 0.63% for patients undergoing trauma surgery, and 0.9% risk for patients undergoing spine surgery (all p < 0.01). The CCI was not associated with surgical site infection or other adverse events, but accounted for 8% of the variation in transfusion rate and 10% of the variation in mortality within 30 days of surgery.
Conclusions
The CCI can be used to estimate the risk of readmission after arthroplasty, hand and upper extremity surgery, spine surgery, and trauma surgery. It also can be used to estimate the risk of transfusion after arthroplasty, spine, trauma, and oncologic orthopaedic surgery and the risk of mortality after shoulder, trauma, and oncologic orthopaedic surgery.
Level of Evidence
Level IV, prognostic study. See the Instructions for Authors for a complete description of levels of evidence
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hospital readmissions are used as an indicator of quality of care [3, 5, 24]. Readmissions are costly [13], and recent legislation introduced financial penalties for high risk-adjusted 30-day readmission for certain diagnoses by establishing the Hospital Readmissions Reduction Program [6, 16, 19]. One center developed an intervention program to reduce readmissions after orthopaedic surgery [14].
There is a relationship between comorbidities and readmissions after orthopaedic trauma surgery [23, 35]. In orthopaedic surgery, comorbidities have been identified as predictors of mortality after arthroplasty, trauma surgery, and oncologic surgery [4, 9, 18, 20, 21, 25, 27, 36]. Complications after ankle fractures, spinal metastasis surgery, and knee or hip arthroplasty also are associated with comorbidities [2, 12, 31–34] as are infections after orthopaedic trauma, spine surgery, knee or hip arthroplasty [8, 17, 22, 36], and transfusion after knee or shoulder arthroplasty [12, 29].
The Charlson Comorbidity Index (CCI) [7] and its recent modification [26] are comorbidity-based measures developed to predict mortality within 1 year of hospital admission in patients without trauma. The updated CCI scores 12 comorbidities with various weightings giving a maximum score of 24 [26]. A higher CCI indicates a higher risk of death within 1 year. The CCI also has been evaluated as a predictor for outcomes after orthopaedic trauma surgery, postoperative adverse events after general surgery, and readmission for geriatric and general medicine patients [2, 9, 17, 30, 32–34, 37].
We sought to answer the following: Is an increased score on the CCI associated with (1) readmission, (2) surgical site infection or other adverse events, (3) transfusion risk, or (4) mortality after orthopaedic surgery?
Patients and Methods
The Research Patient Data Registry is a centralized clinical data registry covering a patient base of greater than 4.0 million insured and uninsured patients from Massachusetts General Hospital and Brigham Women’s Hospital, Boston. It comprises diagnoses, medications, laboratory scores, procedures codes, demographic information (sex, age, race, marital status) and visit entries. We used the Research Patient Data Registry to identify patients having orthopaedic surgery. A total of 30,126 orthopaedic surgeries met the following inclusion criteria: (1) surgery performed between 2008 and 2011, and (2) no prior orthopaedic surgery within 30 days of the operation. The included surgeries were performed with an equal distribution of males and females, with the majority of the patients being between 40 and 59 years old (Table 1).
The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) was used to code diagnoses and procedures. Surgeries were excluded if data were missing for diagnosis codes (194 cases) or procedure codes (1270 cases). Surgery-related adverse events and infections (Appendix 1) and comorbidities as listed in the updated and reweighted CCI [26] (Appendix 2) also were classified using ICD-9 codes.
Statistical Analysis
Baseline characteristics of study patients were summarized with frequencies and percentages for categorical variables and as mean ± SD for continuous variables. Factors significantly associated with readmission, adverse event, surgical site infection, transfusion, and mortality were assessed in bivariate analysis using Student’s t-tests and chi-square tests (Table 2). Variables entered in these analyses were indicators for the ICD-9 procedure group, the surgeon, the patient’s age group, sex, race and marital status, the timing of the operation, duration of operation, length of hospital stay, and orthopaedic subspecialty performing surgery (arthroplasty, foot and ankle, hand, shoulder, spine, sports, pediatrics, trauma, and oncology). For analysis of postoperative surgery-related adverse events and infections within 30 days of surgery, we excluded operations that were performed for surgery-related adverse events or infection within 30 days of another operation. Ordinary least squares regression analyses then were used to determine factors associated with readmission, adverse event, surgical site infection, transfusion, and mortality within 30 days of discharge, from the CCI and the other explanatory variables, which were significantly related to our dependent variables in the bivariate analyses. We decided against using logistic regressions for computational reasons. The coefficient of the ordinary least squares regression indicates the direction of one unit increase of the response variable in relation to explanatory variable. The R-square means the percentage of the variance of the explanatory variable is accounted by the response variables in the model.
Results
Readmission
A total of 913 of 30,129 patients (3.0%) were readmitted within 30 days after discharge.
The CCI accounted for 10% of the variation in readmissions. Every point increase in CCI score adds an additional 0.45% risk in readmission for patients undergoing arthroplasty, 0.63% for patients undergoing trauma surgery, 0.90% risk for patients undergoing spine surgery (all p < 0.001), and −0.27% for patients undergoing hand and upper extremity surgery (p = 0.092) (Table 3). As a reference every year increase in age adds an additional 0.03% risk in readmission for all patients.
Surgical Site Infections and Other Surgery-related Adverse Events
Surgical site infections and other surgery-related adverse events within 30 days of surgery occurred in 393 of 28,604 (1.4%) (Table 4) and 417 of 29,678 (1.4%) (Table 5) patients, respectively. An increase in the CCI was not associated with changes in the likelihood of these events for all surgery types.
Blood Transfusion
Blood transfusion was prescribed after 211 of 30,129 (0.7%) orthopaedic surgeries. With every point increase in CCI score, the risk of transfusion was increased by 0.11% after arthroplasty (p = 0.044), 0.69% after spine surgery, 0.45% after trauma surgery, and 0.34% after oncologic surgery (all p < 0.001). The CCI explained 7.5% of the variation in blood transfusion after orthopaedic surgery (Table 6).
Mortality
Fifty-six of 30,129 patients (0.19%) died within 30 days after discharge. For every point increase in CCI score, mortality increased 0.25% after shoulder surgery, 0.24% after trauma surgery, and 0.33% after oncologic surgery. The CCI explained 9.9% of the variation in mortality after orthopaedic surgery (Table 7).
Discussion
The ability to anticipate complications of treatment is essential to the effective practice of surgery. With the economic penalties associated with readmission after surgery with the Hospital Readmissions Reduction Program [6, 16, 19], there now are financial and professional incentives to improve our ability to anticipate complications of treatment. The CCI has been used as a predictor for adverse events [2, 9, 17, 30, 32–34, 37]. Our study addressed the association of comorbidities as measured by the CCI on readmission and adverse outcomes after orthopaedic surgeries. We evaluated the correlation between CCI and risk of readmission, surgical site infection, other adverse events, risk of transfusion, and mortality after orthopaedic surgery.
This study should be interpreted in light of several limitations. The data are from one registry representing a few years at two major teaching hospitals in the same area and therefore may not be generalizable. Our analyses on readmission did account for length of stay, although the relation of readmission and hospital stay has been questioned [11, 28]. We used ICD-9 codes to calculate the CCI (Appendix 2) and detect adverse events and surgical site infections (Appendix 1). ICD-9 codes may be inaccurate or incomplete in a large database, but the rate of errors seems acceptably low. The main drawback of using the CCI as a predictor of readmission or the other outcomes analyzed is that different conditions or combinations of conditions may lead to an equal index score. This blunt scoring system hinders the development of risk management protocols which should focus on specific conditions or interactions. In addition, we could not account for the severity of injury or complexity of surgery, both of which may influence surgery outcomes.
Readmission after surgery was associated with CCI for spine and trauma surgeries and arthroplasties but explained only a small amount of the variation in readmission. This is consistent with studies of medical patients [30, 37]. A retrospective study of readmission of general medicine patients admitted from the emergency department revealed a hazard ratio of 1.42 (95% CI, 1.07–1.89) for patients with a Charlson score of 2 to 4 and a hazard ratio of 1.93 (95% CI, 1.37–2.73) for patients with a Charlson score higher than 4 [30]. A prospective study on geriatric patients revealed that 3.1% of the variation in readmission in their study-population was explained by the CCI [37].
In our study, the CCI was not related to repeat surgery for adverse events or surgical site infection. In other words, adverse events judged to be related to the surgery based on expert review were not related to the CCI. Prior studies that included medical adverse events found associations with the CCI. One 10-year study of patients undergoing primary THA revealed increased CCI score as a predictor of infection, dislocation, revision, perioperative fracture, neurologic injury, and thromboembolic events [33]. In another study, the risk of deep venous thrombosis or pulmonary embolism (DVT/PE) after surgery for ankle fracture was increased in patients with higher CCI scores [32]. An analysis of thromboembolic adverse events after THA and TKA exposed higher CCI score as a risk factor (odds ratio, 1.2; 95% CI, 1.1–1.4) for DVT/PE in patients undergoing TKAs but not for patients undergoing THAs [31, 34]. One retrospective study analyzing patients after oncologic orthopaedic surgery found the CCI was a predictor of medical complications (eg, pneumonia, respiratory failure) [2]. Higher CCI scores were found to significantly increase the risk of infection at 10 years after spine surgery (hazard ratio, 2.48; 95% CI, 1.93–3.19) [17]. Some comorbidities, in particular diabetes, have an important influence on infections after orthopaedic trauma surgery [8, 22].
CCI was associated with increased use of transfusion in patients undergoing arthroplasty, spine, trauma, or oncologic orthopaedic treatment in our study. Some studies of transfusion after orthopaedic surgery do not involve comorbidities in their risk analyses [1, 15], despite that some comorbidities (especially cardiovascular) commonly lead to increased need for transfusion. A prospective study of geriatric patients with primary hip or knee arthroplasty revealed coronary artery disease as a predictor of transfusion. The association between transfusion after shoulder arthroplasty and the number of comorbidities has been inconsistent [10, 12, 29].
In our study, the CCI was associated with a higher risk of death within 30 days of discharge for patients with trauma, undergoing shoulder surgery, or receiving oncologic treatment. The association of the CCI with mortality after trauma is consistent with prior studies in which higher in-hospital mortality was found in patients with hip fractures with higher CCI scores [9, 25].
This data set indicates that comorbidities as measured by the CCI have a significant influence on readmission, transfusion, and mortality after orthopaedic surgery, more so for certain subspecialties, but are not useful as a predictor of surgical site infection or surgery-related adverse events. To determine if these findings are generalizable, multicenter studies could be useful, although our conclusions are drawn from a robust data registry providing considerable power. However, since multiple comorbidities or combinations have the same weight, the CCI may not be helpful in developing risk management protocols focused on specific conditions or interactions, for which a more precise tool is needed. Using Current Procedural Terminology codes and other methods, more detailed analyses for common procedures in each orthopaedic subspecialty could be made, for example, by addressing different kinds of arthroplasty or severity of injury.
References
Ahmed I, Chan JK, Jenkins P, Brenkel I, Walmsley P. Estimating the transfusion risk following total knee arthroplasty. Orthopedics. 2012;35:e1465–1471.
Arrigo RT, Kalanithi P, Cheng I, Alamin T, Carragee EJ, Mindea SA, Boakye M, Park J. Charlson score is a robust predictor of 30-day complications following spinal metastasis surgery. Spine (Phila Pa 1976). 2011;36:E1274–1280.
Ashton CM, Kuykendall DH, Johnson ML, Wray NP, Wu L. The association between the quality of inpatient care and early readmission. Ann Intern Med. 1995;122:415–421.
Aynardi M, Jacovides CL, Huang R, Mortazavi SM, Parvizi J. Risk factors for early mortality following modern total hip arthroplasty. J Arthroplasty. 2013;28:517–520.
Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Arch Intern Med. 2000;160:1074–1081.
Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013;173:695–698.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma. 1999;13:369–372.
Gabbe BJ, Magtengaard K, Hannaford AP, Cameron PA. Is the Charlson Comorbidity Index useful for predicting trauma outcomes? Acad Emerg Med. 2005;12:318–321.
Hardy JC, Hung M, Snow BJ, Martin CL, Tashjian RZ, Burks RT, Greis PE. Blood transfusion associated with shoulder arthroplasty. J Shoulder Elbow Surg. 2013; 22:233–239
Hendren S, Morris AM, Zhang W, Dimick J. Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum. 2011;54:1362–1367.
Higuera CA, Elsharkawy K, Klika AK, Brocone M, Barsoum WK. 2010 Mid-America Orthopaedic Association Physician in Training Award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. 2011;469:1391–1400.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–2148.
Jordan CJ, Goldstein RY, Michels RF, Hutzler L, Slover JD, Bosco JA 3rd. Comprehensive program reduces hospital readmission rates after total joint arthroplasty. Am J Orthop (Belle Mead NJ). 2012;41:E147–151.
Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A. Predicting the need for blood transfusion in patients with hip fractures. Int Orthop. 2013;37:693–700.
Kocher RP, Adashi EY. Hospital readmissions and the Affordable Care Act: paying for coordinated quality care. JAMA. 2011;306:1794–1795.
Kurtz SM, Lau E, Ong KL, Carreon L, Watson H, Albert T, Glassman S. Infection risk for primary and revision instrumented lumbar spine fusion in the Medicare population. J Neurosurg Spine. 2012;17:342–347.
Mantilla CB, Wass CT, Goodrich KA, Johanns CJ, Kool ML, Zhu X, Corredor JA, Warner DO, Joyner MJ, Berry DJ, Schroeder DR, Sprung J. Risk for perioperative myocardial infarction and mortality in patients undergoing hip or knee arthroplasty: the role of anemia. Transfusion. 2011;51:82–91.
McCarthy D, Johnson MB, Audet AM. Recasting readmissions by placing the hospital role in community context. JAMA. 2013;309:351–352.
Memtsoudis SG, Ma Y, Chiu YL, Walz JM, Voswinckel R, Mazumdar M. Perioperative mortality in patients with pulmonary hypertension undergoing major joint replacement. Anesth Analg. 2010;111:1110–1116.
Memtsoudis SG, Pumberger M, Ma Y, Chiu YL, Fritsch G, Gerner P, Poultsides L, Valle AG. Epidemiology and risk factors for perioperative mortality after total hip and knee arthroplasty. J Orthop Res. 2012;30:1811–1821.
Miller AG, Margules A, Raikin SM. Risk factors for wound complications after ankle fracture surgery. J. Bone Joint Surg Am. 2012;94:2047–2052.
Moore L, Thomas Stelfox H, Turgeon AF, Nathens AB, Sage NL, Emond M, Bourgeois G, Lapointe J, Gagné M. Rates, patterns, and determinants of unplanned readmission after traumatic injury: a multicentre cohort study. Ann Surg. 2013 Mar 8. [Epub ahead of print]
Navaneethan U, Gutierrez NG, Jegadeesan R, Venkatesh PG, Butt M, Sanaka MR, Vargo JJ, Parsi MA. Delay in performing ERCP and adverse events increase the 30-day readmission risk in patients with acute cholangitis. Gastrointest Endosc. 2013;78:81–90.
Neuhaus V, King J, Hageman MG, Ring DC. Charlson comorbidity indices and in-hospital deaths in patients with hip fractures. Clin Orthop Relat Res. 2013;471:1712–1719.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, Januel JM, Sundararajan V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173:676–682.
Sanders RD, Bottle A, Jameson SS, Mozid A, Aylin P, Edger L, Ma D, Reed MR, Walters M, Lees KR, Maze M. Independent preoperative predictors of outcomes in orthopedic and vascular surgery: the influence of time interval between an acute coronary syndrome or stroke and the operation. Ann Surg. 2012;255:901–907.
Schneider EB, Hyder O, Brooke BS, Efron J, Cameron JL, Edil BH, Schulick RD, Choti MA, Wolfgang CL, Pawlik TM. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214:390–398; discussion 398–399.
Schumer RA, Chae JS, Markert RJ, Sprott D, Crosby LA. Predicting transfusion in shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:91–96.
Shu CC, Lin YF, Hsu NC, Ko WJ. Risk factors for 30-day readmission in general medical patients admitted from the emergency department: a single centre study. Intern Med J. 2012;42:677–682.
Singh JA, Jensen MR, Harmsen WS, Gabriel SE, Lewallen DG. Cardiac and thromboembolic complications and mortality in patients undergoing total hip and total knee arthroplasty. Ann Rheum Dis. 2011;70:2082–2088.
SooHoo NF, Eagan M, Krenek L, Zingmond DS. Incidence and factors predicting pulmonary embolism and deep venous thrombosis following surgical treatment of ankle fractures. Foot Ankle Surg. 2011;17:259–262.
Soohoo NF, Farng E, Lieberman JR, Chambers L, Zingmond DS. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–2371.
SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88:480–485.
Teixeira A, Trinquart L, Raphael M, Bastianic T, Chatellier G, Holstein J. Outcomes in older patients after surgical treatment for hip fracture: a new approach to characterise the link between readmissions and the surgical stay. Age Ageing. 2009;38:584–589.
Viens NA, Hug KT, Marchant MH, Cook C, Vail TP, Bolognesi MP. Role of diabetes type in perioperative outcomes after hip and knee arthroplasty in the United States. J Surg Orthop Adv. 2012;21:253–260.
Zekry D, Loures Valle BH, Graf C, Michel JP, Gold G, Krause KH, Herrmann FR. Prospective comparison of 6 comorbidity indices as predictors of 1-year post-hospital discharge institutionalization, readmission, and mortality in elderly individuals. J Am Med Dir Assoc. 2012;13:272–278.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Appendices
Appendix 1. ICD-9 codes for variables used in this study*
Diagnosis | Corresponding ICD-9 codes |
|---|---|
Surgical site infection | |
Other specified local infections of skin and subcutaneous tissue | 686.8 |
Unspecified local infection of skin and subcutaneous tissue | 686.9 |
Unspecified infection of bone, site unspecified | 730.90 |
Unspecified infection of bone, shoulder region | 730.91 |
Unspecified infection of bone, upper arm | 730.92 |
Unspecified infection of bone, forearm | 730.93 |
Unspecified infection of bone, hand | 730.94 |
Unspecified infection of bone, pelvic region and thigh | 730.95 |
Unspecified infection of bone, lower leg | 730.96 |
Unspecified infection of bone, ankle and foot | 730.97 |
Unspecified infection of bone, other specified sites | 730.98 |
Unspecified infection of bone, multiple sites | 730.99 |
Infection and inflammatory reaction due to unspecified device, implant, and graft | 996.60 |
Infection and inflammatory reaction due to internal joint prosthesis | 996.66 |
Infection and inflammatory reaction due to other internal orthopedic device, implant, and graft | 996.67 |
Infection and inflammatory reaction due to other internal prosthetic device, implant, and graft | 996.69 |
Infected postoperative seroma | 998.51 |
Other postoperative infection | 998.59 |
Posttraumatic wound infection not elsewhere classified | 958.3 |
Surgical adverse event | |
Unspecified mechanical complication of internal orthopedic device, implant, and graft | 996.40 |
Other mechanical complication of prosthetic joint implant | 996.47 |
Other mechanical complication of other internal orthopedic device, implant, and graft | 996.49 |
Other complications due to internal joint prosthesis | 996.77 |
Other complications due to other internal orthopedic device, implant, and graft | 996.78 |
Other complications due to other internal prosthetic device, implant, and graft | 996.79 |
Complications of unspecified reattached extremity | 996.90 |
Complications of reattached hand | 996.92 |
Complications of reattached finger(s) | 996.93 |
Complications of reattached upper extremity, other and unspecified | 996.94 |
Complication of reattached foot and toe(s) | 996.95 |
Complication of other specified reattached body part | 996.99 |
Unspecified complication of amputation stump | 997.60 |
Other amputation stump complication | 997.69 |
Surgical operation with implant of artificial internal device causing abnormal patient reaction, or later complication, without mention of misadventure at time of operation | E878.1 |
Amputation of limb(s) causing abnormal patient reaction, or later complication, without mention of misadventure at time of operation | E878.5 |
Other specified surgical operations and procedures causing abnormal patient reaction, or later complication, without mention of misadventure at time of operation | E878.8 |
Unspecified surgical operations and procedures causing abnormal patient reaction, or later complication, without mention of misadventure at time of operation | E878.9 |
Appendix 2. Comorbidities as listed in the updated CCI with corresponding ICD 9 codes as used in this study*
Diagnosis | Corresponding ICD9 codes |
|---|---|
Congestive heart failure | 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.4–425.9, 428.x |
Dementia | 290.x, 294.1, 331.2 |
Chronic pulmonary disease | 416.8, 416.9, 490.x–505.x, 506.4, 508.1, 508.8 |
Rheumatologic disease | 446.5, 710.0–710.4, 714.0–714.2, 714.8, 725.x |
Mild liver disease | 070.22, 070.23, 070.32, 070.33, 070.44, 070.54, 070.6, 070.9, 570.x, 571.x, 573.3, 573.4, 573.8, 573.9, V42.7 |
Diabetes with chronic complications | 250.4–250.7 |
Hemiplegia or paraplegia | 334.1, 342.x, 343.x, 344.0, 344.6, 344.9 |
Renal disease | 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 582.x, 583.0–583.7, 585.x, 586.x, 588.0, V42.0, V45.1, V56x |
Any malignancy, including leukemia and lymphoma | 140.x–172.x, 174.x–195.8, 200.x–208.x, 238.6 |
Moderate or severe liver disease | 456.0–456.2, 572.2–572.8 |
Metastatic solid tumor | 196.x–199.x |
HIV/AIDS | 042.x–044.x |
About this article
Cite this article
Voskuijl, T., Hageman, M. & Ring, D. Higher Charlson Comorbidity Index Scores are Associated With Readmission After Orthopaedic Surgery. Clin Orthop Relat Res 472, 1638–1644 (2014). https://doi.org/10.1007/s11999-013-3394-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-013-3394-8